Abstract
Purpose of Review
Recent research related to sex and gender role influences on asthma in women is summarized. Implications for enhancing women’s self regulation and ability to manage asthma effectively are discussed.
Recent Findings
Studies in the past year have indicated that asthma is a significant burden on women and emphasized the importance of control, especially during pregnancy. The significance of hormonal variation in symptoms and severity has been noted. An association between weight and asthma has been observed. Evidence suggests that hormonal changes contribute to the asthma prevalence shift from boys to women in adolescence. One study showed positive results from focusing on sex and gender related factors in self regulation education for women. Recent findings imply that enhancing self regulation and effective management of asthma by women requires attention to sex and gender role influences in clinical counseling and intervention research.
Summary
Clinicians may help female patients with asthma by incorporating sex and gender-role related considerations into their clinical consultations. Evidence based asthma education interventions to assist women with their particular asthma management challenges are needed.
Keywords: asthma, women, self-regulation, gender
INTRODUCTION
Asthma continues to be a significant problem for large numbers of Americans, indeed, people around the world. In the United States, recent data from the CDC [1*, 2] indicate that asthma prevalence has become somewhat stable in the last two years. Three observations are important in regard to these data. First, the prevalence of asthma has stabilized at a very high level with 20 million people in the U.S. alone suffering from the condition.[2] Second, there has been no flattening of prevalence in low income and minority communities where the burden of asthma has been shown to be greatest, in fact, morbidity and health care use for asthma continue to increase in these areas.[3] Third, in adolescence, asthma changes from a disease primarily affecting boys to predominate in adult women [4**, 5**, 6, 7] and relatively little is known about how women’s sex and gender roles influence the condition and their efforts to manage it. Studies have illustrated that interventions to help children and adults with asthma can reduce symptoms and health care use, generally by helping these patients to become more self regulating regarding its management. [8**, 9, 10, 11*] Nonetheless, the particulars about how women manage and can be helped to be more self regulating have received much less attention.
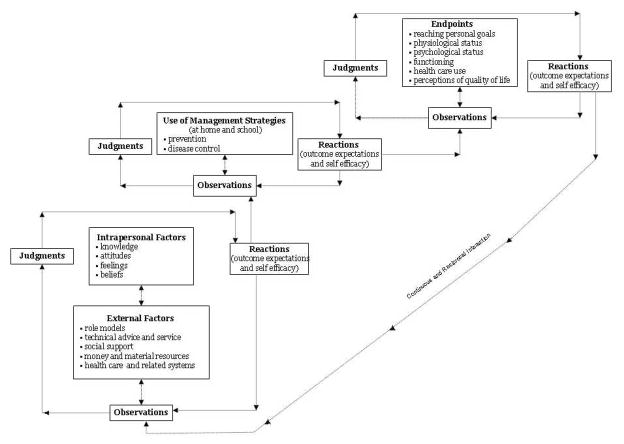
Self regulation as it relates to asthma (and other chronic conditions) entails the ability to observe, make judgments about the observations, try out change strategies to improve management, and react appropriately to the change effort [that is, conclude that one can carry out the strategy (self efficacy) and that the strategy produced the desired result (outcome expectation)]. Figure 1 presents the authors’ model of self regulation. It illustrates the many influences on the woman trying to manage including both internal and external factors. [12]
Figure 1.
The Continuous and Reciprocal Nature of Self-Regulation Processes in Disease Prevention and Management.
Clearly, physical and clinical manifestations of asthma must be understood to allow the patient to make sense of how to manage it. Effective interventions need to widen the woman’s perspective regarding these influences and build her skills of self regulation as they relate to effectively completing a range of varied and complex management tasks. Although, very few data are available to assess self regulation interventions focused on the female patient, in the past year, new work has further illuminated how a woman’s sex and gender roles play a part in the clinical presentation of asthma.
SEX AND GENDER-ROLE INFLUENCES ON ASTHMA AND ITS MANAGEMENT
The studies published between 2006 and 2007 on this topic can be divided into three categories: sex and gender-role predictors of asthma; sex and gender-roles in treatment and health care use; pregnancy related factors.
Sex and gender-role predictors of asthma
Following a fairly comprehensive review of available studies, Almquist et al [5] conclude that hormonal changes and environmental exposures are possible explanations for the asthma prevalence shift to women during adolescence. They suggest that work of several investigators support this idea. Increases in asthma during adolescence among girls may be associated with their tendency to gain weight over that period of time [13]. This social environment related occurrence may contribute to the sex differences observed. Gender roles apparent in the social environment may also contribute to differences. Exposure to gas cooking, the tendency of new smokers to be girls and the potential greater affect of smoking on their health, may also result in more disease and more problems associated with it. Almquist et al [5] point out, however, that girls may over report asthma symptoms compared to boys [14] and this may be a feature of the social environment contributing to sex differences in asthma measurements
Burgess et al [15*] conducted a population based study of 8,583 individuals in a birth cohort in Tasmania surveyed first at seven years of age and again at 25. Their findings underscored the much discussed potential association of weight to asthma. In females but not males there was a correlation between adiposity at seven and adult onset asthma at 32 years of age. Further, a higher body mass index level in females with no evidence of asthma at seven years predicted the onset of asthma later in life (after 21 years of age). Jones et al [16*] give a different slant on the weight and asthma question. This team used data from the Nurses Health Study of 121,700 married women ages 30 to 55 years who are surveyed biennially. They found that short stature predicted adult onset of asthma in these women but the association was not independent of obesity. Being of shorter height and greater weight correlated with development of the disease.
Hormonal factors and weight were explored by Gomez Real et al [17**]. They found that long or irregular menstrual cycles were associated with more asthma symptoms, allergic asthma and lower forced vital capacity (FVC) in women. There was also an additive feature of body mass index to lung capacity. Symptoms, FVC and FEV1 increased with BMI until 25 kg/m2 but, thereafter, decreased with increasing BMI. The investigators concluded that women with long or irregular periods have more asthma independent of BMI. They speculated that airways pathology may have not only a hormonal component but a metabolic one. The same investigators (Gomez Real et al [18] found in the cross Europe peri-menopausal study of 8,588 women 25 to 54 years of age that use of hormone replacement therapy (HRT) increased the asthma risk in women and this risk was greater for women at lower weight than higher weight. They concluded that in peri-menopausal women, lean women on HRT were at as high a risk for asthma as overweight women not on HRT and both factors (weight and HRT) may function partly through common pathways.
Sex and Gender-roles in Asthma Treatment and Health Care Use
Lee et al [19*] reported on the TENOR study of 4,756 subjects 12 years or older with severe or difficult to treat asthma and baseline IgE between 30 to 700 ul/ml. They found that compared to males, females reported more asthma related negative health outcomes including need for steroid bursts, unscheduled office visits, missed work and reduced quality of life. The number of precipitants to asthma episodes and allergy were more common in women. However, at the same time, women had better lung function, similar treatment patterns and no differences in disease severity from men. The investigators observed, in what might be labeled an understatement, that a complex range of factors predict asthma in women.
Almquist et al [5] in their review also concluded that hospitalization between boys and girls appear to be attributable to differences in the prevalence not the severity of asthma. [20] In other words, they posited that asthma in females may be more prevalent but not more serious than in males. Similarly, Naleway et al [21] studied 1191 patients with persistent asthma in the Colorado Kaiser Permanente medical organization and found no severity differences between men and women. Further, women in this investigation were more likely to have a regular physician, use peak flow monitoring (PFM) and be in possession of an asthma action plan.
Schatz et al [22] on the other hand, in a study of 1286 patients two to 54 years of age, found that among adults, women had a greater number of hospitalizations even accounting for higher prevalence and adjusting for previous utilization of health care and for use of inhaled corticosteroids. Data from Sinclair and Tolsema [23] echo these findings. They showed in a survey of 1200 members (35 years or older)of a medical care organization that women with asthma made more acute visits for the condition and reported more symptoms, more use of asthma relievers and greater severity of disease. Findings in a study by Day et al [24] landed somewhere in the middle of previous work. They surveyed 512 adults with asthma 20 to 50 years of age and found poor levels of asthma control in both men and women. Women, however, were more likely to have used inhaled corticosteroids and to have needed urgent care in the previous year.
Asthma in Pregnancy
In general, the National Asthma Education and Prevention Guidelines updated this year [25] indicate that asthma well controlled during pregnancy does not result in negative consequences for women. Tata et al [26*] in a study of 281,019 pregnant women in the United Kingdom Health Improvement Network data base came to a similar conclusion. Ten percent of the women they studied had asthma and there was no evidence of increased risk for adverse pregnancy outcomes or obstetric complications for these women. There was a modest risk for miscarriage. Baibergenova et al [27] also reported no adverse effects in pregnancy among the 530 women with asthma they studied, while Bakhiereva et al [28*] found no or minimal effect of asthma medicines on fetal growth for pregnant women with asthma and that perinatal complications were reduced among women with well managed disease.
Uncontrolled asthma, however, has been shown to produce some negative pregnancy results for some patients. Getahun et al [29**] examined 41,250 cases from the National Hospital Discharge Survey. They found asthma in the mother was associated with premature rupture of membranes at delivery in 5% of black but not white patients.
Characteristics of women and their pregnancies have been associated with outcomes for their children. Laerum et al [30*] found among 16,190 subjects in the European Community Respiratory Health Survey that younger maternal age at delivery was associated with more asthma and respiratory symptoms in children after adjusting for a large number of other potential influences. Shinohara et al [31*] found among 400 women studied that allergic rhinitis in the mother early in pregnancy was associated with greater risk for allergic rhinitis in the child. Enriquez et al [32**] studied women aged 15 to 44 enrolled in the Medicaid Program. Among the 140,299 pregnancies investigated, birth weight of children of women with asthma was 38 grams lower when the mother delivered with exacerbated asthma. Jaakkola et al [33] in a review of 19 studies found that pre term babies were at greater risk for asthma and in another investigation [34*] that there were no differences in risk for asthma among male or female children when their mothers smoked during pregnancy, that is, both were at greater risk for asthma.
IMPLICATIONS FOR SELF REGULATION OF ASTHMA IN WOMEN
These recent findings hold important implications for enhancing self regulation in women and building their capacity to manage asthma more effectively. Although data are not definitive, given the suggestion that women may over report their symptoms, a number of investigators have concluded that asthma and its associated burden including health care use is greater for women than men. Further, hormonal fluctuations (menstruation, menopause, pregnancy) have an impact on a woman’s asthma and by extension, how she must manage it. In addition, although questions remain unanswered concerning weight and the onset of asthma, sufficient data indicate that BMI is a factor in the condition and, therefore, in an individual’s management efforts.
How frequently are these sex and gender-role factors considered in clinical consultations and education? The CDC’s recent Morbidity and Mortality Weekly Report (September 7, 2007) [35*] provides data from a study of asthma education in the U.S. involving a random and representative sample of adolescents and adults with asthma. While 64% of respondents reported that they had been told by a health care provider how to handle an asthma attack, only 12% had received organized instruction regarding the management of asthma. Given the extent and cost of the disease in human and financial terms these data are disappointing. Further, the extent to which the small percentage of women receiving asthma education also got counseling in the sex and gender related factors associated with their disease is questionable.
The authors have conducted extensive research and evaluation of asthma education for women. In this process women have frequently reported that their clinicians have never or rarely discussed sex and gender role related issues of asthma management with them. An example is hormonal changes. The great majority of the 808 women in our recent study [36**] had not been advised to observe any connections between hormonal fluctuations such as just before or during menstruation and any changes in the extent of their asthma symptoms. Another good example is related to sexual activity. Although the topic never or rarely was a feature of the clinical consultations received by the women over the time they have been asthmatic, 19% of women reported asthma symptoms as troublesome during sexual activity. Another example is weight. Among the women we studied, weight, was significantly associated with daytime and nighttime, scheduled (and unscheduled doctor visits, and follow-up visits for an asthma episode. However, the majority of overweight and obese women in our research had not connected their overweight condition to asthma exacerbations. Further, in the review of recent articles for this paper, we could locate only one (our own) article in the peer reviewed literature that describes the results of an intervention to help women manage more effectively in light of these sex and gender-role related influences on their disease. [36**]
Figure 1 makes clear the kind of barriers to effective management that patients confront. To be good managers, women need to increase their skills in self regulation (observation, judgment, trial behavior, reaction) recognizing the potential influence of a wide range of factors on their situation and, most certainly, those related to their sex and gender-roles. In a randomized control trial of an intervention designed to enhance self regulation by emphasizing these central influences on female patients [36**] we found that significant improvements in the women’s asthma outcomes could be achieved. One year subsequent to the program, women in the treatment group reported significantly fewer nighttime symptoms. Women who participated in the intervention reported significantly fewer ED visits, unscheduled doctor visits, and scheduled doctor visits. Women in the treatment group were significantly more likely to notice hormonal changes in their asthma during their menstrual cycle and when having PMS. Additionally, over time the women in the treatment group were significantly less likely to report being bothered by asthma symptoms during sexual activities. Women in the treatment group also had a significant improvement in their quality of life, their level of asthma related self-regulation and their self-confidence to manage asthma.
CONCLUSION
Studies in the past year have confirmed the burden of asthma on female patients, the influence of hormonal factors on their symptoms, the association between weight and asthma and the importance of good control, especially during pregnancy. One study has shown positive results from focusing on sex and gender-role factors in self regulation education for women with asthma. This recent research suggests that clinicians might better serve their female patients with asthma by incorporating sex and gender-role related factors into clinical consultations. Findings also suggest that evidence based asthma education, in general, and most certainly interventions developed to assist women with their particular management challenges should be more widely available.
Acknowledgments
Thanks to Megan Laver and Minal Patel for their assistance with this manuscript.
Contributor Information
Noreen M. Clark, Myron E. Wegman Distinguished University Professor, Director, Center for Managing Chronic Disease, University of Michigan
Melissa A. Valerio, Health Behavior & Health Education, University of Michigan School of Public Health.
Z. Molly Gong, Head of Data Analysis, Center for Managing Chronic Disease, University of Michigan
References
- 1*.Moorman JE, Rudd RA, Johnson CA, King M, Minor P, Bailey C, et al. National surveillance for asthma--United States, 1980–2004. MMWR Surveill Summ. 2007 Oct 19;56(8):1–54. This article highlights asthma surveillance data from the Centers for Disease Control, indicating that prevalence rates have increased alongside asthma encounters with regard to healthcare utilization over the past two decades. Recently, trends have stabilized. [PubMed] [Google Scholar]
- 2.Center for Disease Control and Prevention. National Center for Health Statistics. Atlanta, Georgia: 2007. [accessed 07 Nov 2007]. http://www.cdc.gov/nchs/ [Google Scholar]
- 3.Stingone JA, Claudio L. Disparities in the use of urgent health care services among asthmatic children. Ann Allergy Asthma Immunol. 2006 Aug;97(2):244–250. doi: 10.1016/S1081-1206(10)60021-X. [DOI] [PubMed] [Google Scholar]
- 4**.Carey MA, Card JW, Voltz JW, Arbes SJ, Jr, Germolec DR, Korach KS, et al. It’s all about sex: gender, lung development and lung disease. Trends Endocrinol Metab. 2007 Oct;18(8):308–313. doi: 10.1016/j.tem.2007.08.003. This review highlights the influence of gender and sex hormones on lung development. Increasing age and the role of female sex hormones have been shown to explain the increasing incidence of asthma in women. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5**.Almquist C, Worm M, Leynaert B. Impact of gender on asthma in childhood and adolescence: a GA(2)LEN review. Allergy. 2007 Sep 5; doi: 10.1111/j.1398-9995.2007.01524.x. This review discusses developmental shifts in the prevalence of asthma in males and females. These trends have significant implication for clinical practice and diagnosis. [DOI] [PubMed] [Google Scholar]
- 6.Trawick DR, Holm C, Wirth J. Influence of gender on rates of hospitalization, hospital course, and hypercapnea in high-risk patients admitted for asthma: a 10-year retrospective study at Yale-New Haven Hospital. Chest. 2001 Jan;119(1):115–119. doi: 10.1378/chest.119.1.115. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) Asthma prevalence and control characteristics by race/ethnicity--United States, 2002. MMWR Morb Mortal Wkly Rep. 2004 Feb;27;53(7):145–148. [PubMed] [Google Scholar]
- 8**.Tapp S, Lasserson TJ, Rowe B. Education interventions for adults who attend the emergency room for acute asthma. Cochrane Database Syst Rev. 2007 Jul 18;3(3):CD003000. doi: 10.1002/14651858.CD003000.pub2. This review describes the effects of educational interventions on asthma exacerbated emergency room visits. Educational interventions in the emergency department reduce subsequent hospital admission for asthma. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gibson PG, Ram FS, Powell H. Asthma education. Respir Med. 2003 Sep;97(9):1036–1044. doi: 10.1016/s0954-6111(03)00134-3. [DOI] [PubMed] [Google Scholar]
- 10.Guevara JP. Self-management education of children with asthma: a meta-analysis. LDI Issue Brief. 2003 Nov-Dec;9(3):1–4. [PubMed] [Google Scholar]
- 11*.Ngamvitroj A, Kang DH. Effects of self-efficacy, social support and knowledge on adherence to PEFR self-monitoring among adults with asthma: a prospective repeated measures study. Int J Nurs Stud. 2007 Aug;44(6):882–892. doi: 10.1016/j.ijnurstu.2006.03.001. This study looked at the effects of self-monitoring on self-efficacy in reducing asthma symptoms in adults. Because of a small sample size, the influence of self-efficacy on self-monitoring was not seen to improve asthma symptoms. [DOI] [PubMed] [Google Scholar]
- 12.Clark NM, Gong M, Kaciroti N. A model of self-regulation for control of chronic disease. Health Educ Behav. 2001 Dec;28(6):769–782. doi: 10.1177/109019810102800608. [DOI] [PubMed] [Google Scholar]
- 13.Hancox RJ, Milne BJ, Poulton R, Taylor DR, Greene JM, McLachlan CR, et al. Sex differences in the relation between body mass index and asthma and atopy in a birth cohort. Am J Respir Crit Care Med. 2005 Mar;Jan;171(5):440–445. doi: 10.1164/rccm.200405-623OC. [DOI] [PubMed] [Google Scholar]
- 14.Venn A, Lewis S, Cooper M, Hill J, Britton J. Questionnaire study of effect of sex and age on the prevalence of wheeze and asthma in adolescence. BMJ. 1998 Jun;27;316(7149):1945–1946. doi: 10.1136/bmj.316.7149.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15*.Burgess JA, Walters EH, Byrnes GB, Jenkins MA, Abramson MJ, Hopper JL, et al. Childhood adiposity predicts adult-onset current asthma in females: a 25-yr prospective study. Eur Respir J. 2007;29(4):668–675. doi: 10.1183/09031936.00080906. This study examined the relationship between childhood adiposity and the incidence of asthma during adulthood. This observation may have implications for predicting asthma. [DOI] [PubMed] [Google Scholar]
- 16*.Jones DP, Camargo CA, Speizer FE, Barr RG. Prospective study of short stature and newly diagnosed asthma in women. Journal of Asthma. 2007;44(4):291–295. doi: 10.1080/02770900701344116. The relationship between short stature and asthma in women was examined. This observation may have implications for identifying predictive factors in diagnosing asthma in women. [DOI] [PubMed] [Google Scholar]
- 17**.Gomez Real F, Svanes C, Omenaas ER, Anto JM, Plana E, Janson C, et al. Menstual irregularity and asthma and lung function. J Allergy Clin Immunol. 2007 Sept;120(3):557–56. doi: 10.1016/j.jaci.2007.04.041. Study examining the relationship between irregular menstruation and lung function in women. This observation has significant implications for identifying risk factors for asthma in women. [DOI] [PubMed] [Google Scholar]
- 18.Gomez Real F, Svanes C, Bjornsson EH, Franklin KA, Gislason D, Gislason T, et al. Hormone replacement therapy, body mass index and asthma in perimenopausal women: a cross sectional survey. Thorax. 2006 Jan;61(1):34–40. doi: 10.1136/thx.2005.040881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19*.Lee JH, Haselkorn T, Chipps BE, Miller DP, Wenzel SE. Gender differences in IgE-Mediated allergic asthma in the epidemiology and natural history of asthma: Outcomes and Treatment Regimens (TENOR) Study. Journal of Asthma. 2006;43(3):179–184. doi: 10.1080/02770900600566405. [DOI] [PubMed] [Google Scholar]
- 20.Chen Y, Dales R, Stewart P, Johansen H, Scott G, Taylor G. Hospital readmissions for asthma in children and young adults in Canada. Pediatr Pulmonol. 2003 Jul;36(1):22–26. doi: 10.1002/ppul.10307. [DOI] [PubMed] [Google Scholar]
- 21.Naleway AL, Vollmer WM, Frazier EA, O’Connor E, Magid DJ. Gender differences in asthma management and quality of life. J Asthma. 2006 Sep;43(7):549–552. doi: 10.1080/02770900600858992. [DOI] [PubMed] [Google Scholar]
- 22.Schatz M, Clark S, Camargo CA. Sex Differences in the Presentation and Course of Asthma Hospitalizations. Chest. 2006 Jan;129(1):50–55. doi: 10.1378/chest.129.1.50. [DOI] [PubMed] [Google Scholar]
- 23.Sinclair AH, Tolsma DD. Gender differences in asthma experience and disease care in a managed care organization. J Asthma. 2006 Jun–Jul;43(5):363–367. doi: 10.1080/02770900600705334. [DOI] [PubMed] [Google Scholar]
- 24.Day A, Ernst P, Glick L, Zimmerman S, Chapman KR. Women and asthma: lessons from a gender analysis of the asthma in Canada survey. J Asthma. 2006 Mar;43(2):169–173. doi: 10.1080/02770900500499061. [DOI] [PubMed] [Google Scholar]
- 25.National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. 2007 August;28:3. [Google Scholar]
- 26*.Tata LJ, Lewis SA, McKeever TM, Smith CJ, Doyle P, Smeeth L, et al. A comprehensive analysis of adverse obstetric and pediatric complications in women with asthma. Am J Respir Crit Care Med. 2007 May 15;175(10):991–997. doi: 10.1164/rccm.200611-1641OC. Researchers looked at the association between asthma and its affect on pregnancy complications. They found that asthma does increase complications during pregnancy and precautions should be taken within clinical practice. [DOI] [PubMed] [Google Scholar]
- 27.Baibergenova A, Thabane L, Akhtar-Danesh N, Levine M, Gafni A. Is fetal gender associated with emergency department visits for asthma during pregnancy? J Asthma. 2006 May;43(4):293–299. doi: 10.1080/02770900600622984. [DOI] [PubMed] [Google Scholar]
- 28*.Bakhireva LN, Schatz M, Chambers CD. Effect of maternal asthma and gestational asthma therapy on fetal growth. Journal of Asthma. 2007;44:71–76. doi: 10.1080/02770900601180313. This review looked at the effects of various asthma treatments on fetal growth. Oral corticosteroids pose some documented increased risk for adverse consequences of fetal growth. [DOI] [PubMed] [Google Scholar]
- 29**.Getahaun D, Ananth CV, Oyelese Y, Peltier MR, Smulian JC, Vinzileos AM. Acute and chronic respiratory diseases in pregnancy: Associations with spontaneous premature rupture of membranes. J Matern Fetal Neonatal Med. 2007 September;20(9):669–675. doi: 10.1080/14767050701516063. This study sought to look at the association between respiratory diseases and the premature rupturing of membranes in a sample of pregnant women. Premature rupture of membranes was found among pregnant women with respiratory diseases, specifically asthma and chronic bronchitis, and the association was seen more in blacks than whites. [DOI] [PubMed] [Google Scholar]
- 30*.Laerum BN, Svanes C, Wentzel-Larsen T, Gulsvik A, Toren K, Norrman E, et al. Young maternal age at delivery is associated with asthma in adult offspring. Respir Med. 2007 Jul;101(7):1431–1438. doi: 10.1016/j.rmed.2007.01.020. The association between maternal age and the affects of asthma on offspring was studied. Asthma became less common among adult offspring as maternal age increased, and suggest that certain biological factors may be influencing maternal aging. [DOI] [PubMed] [Google Scholar]
- 31*.Shinohara M, Wakiguchi H, Saito H, Matsumoto K. Symptoms of allergic rhinitis in women during early pregnancy are associated with higher prevalence of allergic rhinitis in their offspring. Allergol Int. 2007 Sep 1;56(4) doi: 10.2332/allergolint.O-06-471. This study looked to see if allergen exposure during pregnancy had increased incidence of allergic pathology in offspring. A strong association was seen with explanation of mediation through epigenetic mechanisms. [DOI] [PubMed] [Google Scholar]
- 32**.Enriquez R, Griffin MR, Carroll KN, Wu P, Cooper WO, Gebretsadik T, et al. Effect of maternal asthma and asthma control on pregnancy and perinatal outcomes. J Allergy Clin Immunol. 2007 Sep;120(3):625–630. doi: 10.1016/j.jaci.2007.05.044. This study found that asthma exacerbates associated anomalies during pregnancy. Ethnic differences were seen, with higher risks shown among black women. These findings have implications for improved monitoring of asthma among pregnant women. [DOI] [PubMed] [Google Scholar]
- 33.Jaakola JK, Ahmed P, Ireomninom A, Goepfert P, Laiou E, Quansah R, et al. Preterm delivery and asthma: A systematic review and meta-analysis. J Allergy Clin Immunol. 2006 October;118(4):823–830. doi: 10.1016/j.jaci.2006.06.043. [DOI] [PubMed] [Google Scholar]
- 34*.Jaakkola JJ, Gissler M. Are girls more susceptible to the effects of prenatal exposure to tobacco smoke on asthma? Epidemiology. 2007 Sep 18;5:573–576. doi: 10.1097/EDE.0b013e31812001d2. Differences among genders for risk of asthma due to exposure to tobacco smoke was studied. Both males and female were at equal risk. [DOI] [PubMed] [Google Scholar]
- 35*.Centers for Disease Control and Prevention (CDC) Asthma self-management education among youths and adults--United States, 2003. MMWR. 2007 Sep 7;56(35):912–915. This review highlights the effectiveness of asthma self-management programs. The report concludes that much of the youth and adult population are lacking the education to effectively self-manage their asthma. [PubMed] [Google Scholar]
- 36**.Clark NM, Gong ZM, Wang SJ, Lin X, Bria WF, Johnson TR. A randomized trial of a self-regulation intervention for women with asthma. Chest. 2007 Jul;132(1):88–97. doi: 10.1378/chest.06-2539. This study looked at the effectiveness of a telephone counseling intervention for self-managing asthma among women. This is one of the few studies looking at self-regulation intervention for women with asthma. [DOI] [PubMed] [Google Scholar]