Abstract
Background and purpose
The purpose of this study was to quantify the biomechanical properties of specific manual therapy techniques in patients with symptomatic knee osteoarthritis.
Methods
Twenty subjects (7 female/13 male, age 54±8 years, ht 1·7±0·1 m, wt 94·2±21·8 kg) participated in this study. One physical therapist delivered joint mobilizations (tibiofemoral extension and flexion; patellofemoral medial–lateral and inferior glide) at two grades (Maitland’s grade III and grade IV). A capacitance-based pressure mat was used to capture biomechanical characteristics of force and frequency during 2 trials of 15 second mobilizations. Statistical analysis included intraclass correlation coefficient (ICC3,1) for intrarater reliability and 2×4 repeated measures analyses of variance and post-hoc comparison tests.
Results
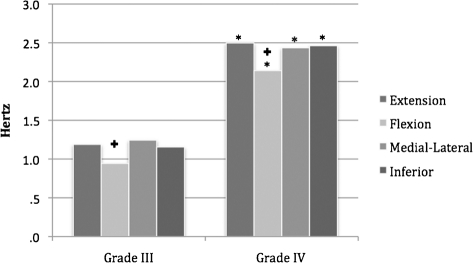
Force (Newtons) measurements (mean, max.) for grade III were: extension 45, 74; flexion 39, 61; medial–lateral glide 20, 34; inferior glide 16, 27. Force (Newtons) measurements (mean, max.) for grade IV were: extension 57, 76; flexion 47, 68; medial–lateral glide 23, 36; inferior glide 18, 35. Frequency (Hz) measurements were between 0·9 and 1·2 for grade III, and between 2·1 and 2·4 for grade IV. ICCs were above 0·90 for almost all measures.
Discussion and conclusion
Maximum force measures were between the ranges reported for cervical and lumbar mobilization at similar grades. Mean force measures were greater at grade IV than III. Oscillation frequency and peak-to-peak amplitude measures were consistent with the grade performed (i.e. greater frequency at grade IV, greater peak-to-peak amplitude at grade III). Intrarater reliability for force, peak-to-peak amplitude and oscillation frequency for knee joint mobilizations was excellent.
Keywords: Knee Joint, Mobilization, Manual therapy, Biomechanics, Joint, Orthopedic, Force, Reliability
Introduction
Osteoarthritis (OA) is the most commonly reported joint disease and the most common cause of disability in the United States.1 While knee OA is more common in older adults and the obese, sports participation and related occupational hazards have been identified as risk factors.2 The knee is the most common lower extremity joint affected by OA.1,3 Pain and stiffness in osteoarthritic joints can limit mobility and function and contribute to morbidity, loss of function, medical expenses, and lost work time in adults.1,3–5 For many years the standard treatment for symptomatic knee OA was arthroscopic debridement, but a recent systematic review concluded that this procedure provides no benefit when compared to placebo.6 Medications such as acetaminophen and non-steroidal anti-inflammatory drugs are frequently used for long-term management of OA, but they have side effects to consider as part of their risk/benefit ratio.7–10 A manual physical therapy approach which includes joint mobilization and reinforcing exercise has a growing base of evidence, including randomized clinical trials, to support its use in treating knee OA.11–13
Joint mobilization, also called nonthrust manipulation, is a form of manual physical therapy and is a tool used by a physical therapist in the treatment of many disorders of the neurological, muscular, and skeletal system, including OA.14 Many common manual mobilization techniques used by physical therapists when treating the knee joint are described by Maitland et al.15 Knee joint mobilization can be described as an oscillatory manual force applied to the tibiofemoral, proximal tibio-fibular, or patellofemoral joints, in a variety of directions and positions based on the patient’s presentation. Mobilizations to the knee may be applied with several different hand positions or grips. Physical therapists typically select 1 of 4 grades, or types of mobilization application based on the amount of resistance and magnitude of movement, which have been described by Maitland et al.15 and Grieve16 depending on the aim of treatment. Grades I and II are designated as movements before reaching joint resistance (primarily for pain modulation), and Grades III and IV are for movements into resistance (primarily to increase motion). Additionally, grades I and IV are small movements, and grades II and III are large movements.
The external forces provided by the physical therapist with these movements are seen as an important part of the mechanism of effect of these treatments, regardless of the particular explanatory model under consideration.15,17–21 Therefore, some standardization of these forces and techniques may be important. If the forces applied during knee mobilization vary largely within or between physical therapists then forces may not be consistently effective, and this may affect patient outcomes. No optimal dosage of joint mobilization has been established for the knee. A lack of standardization for these interventions can also lead to variation of outcomes in research that evaluates the effectiveness of manual therapy as an intervention. In order to fully investigate the possible effects of manual forces on treatment outcomes, the forces delivered (i.e. the dosage) must be accurately measured.
In other anatomic regions (the cervical and lumbar spines and selected peripheral joints), a growing body of literature21–23 has quantified the biomechanical parameters and reliability for joint mobilization techniques. This characterization of parameters and reliability for joint mobilization techniques may help refine teaching methods, determine safety and dosages, drive theories of mechanisms of effect, and suggest suitability for use in different populations.24–30 Biomechanical parameters describe the techniques and also provide an opportunity to examine their reliability. Existing evidence indicates overall fair to poor inter-rater reliability for force measurements during spinal mobilization or palpatory assessments, which improves for intrarater measures.24–27,29,30 The fair to poor inter-rater and intrarater reliability for manual mobilization assessments and techniques is a central issue affecting reproducibility, dosage determination, force quantification, and training methods for these techniques. Little is known about the magnitude of forces applied during knee mobilization. A necessary first step in the understanding the biomechanical properties of knee joint mobilizations is to quantify the forces involved and investigate their reliability. A review of the literature revealed no published data concerning the description of biomechanical measures of knee joint mobilization, reliability, or methods of feedback training.
This study had three aims. First, we sought to quantify the biomechanical measures of four common knee joint mobilizations (flexion, extension, medial–lateral glide, and inferior glide) for the variables of mean force, maximum force, force–time integral (FTI), peak-to-peak amplitude, and oscillation frequency in a sample of patients with symptomatic knee OA. Second, we attempted to determine if any of these variables were different between grade III and grade IV mobilizations; and we hypothesized that grade IV mobilizations would show higher mean forces, similar maximum forces, lower oscillation frequencies and lower peak-to-peak amplitudes than the grade III mobilizations, consistent with their textbook descriptions. Last, we sought to determine the reliability of a single operator in applying joint mobilization using these grades and techniques.
Methods
Design
This was a descriptive biomechanical study using a cross-sectional observational cohort with prospective sequential enrollment. We sought to quantify the biomechanical parameters of knee joint mobilization as measured using a capacitance-based pressure platform (Pliance-x®, Novel Electronics Inc., St Paul, MN, USA) for data capture. The pressure data are captured by means of a thin flexible mat placed between the mobilizing hand and the patient’s body. The flexibility of the sensor mat allows for conformability to patient’s knee and does not alter the mobilization technique used by the physical therapist.
Setting and participants
Subjects were recruited from patients referred to physical therapy for symptomatic knee OA at Brooke Army Medical Center from January 2010 to August 2010. At the time of entrance into the study, the subjects were undergoing the standard of care treatment for their condition in physical therapy, which includes knee joint mobilization. All subjects provided written informed consent to participate, and the Institutional Review Board at Brooke Army Medical Center, San Antonio Texas, approved this study.
Inclusion and exclusion criteria
To be included in the study, the subject must have been eligible for military health care and have sufficient English language ability to understand the consent and testing procedures. Their treating physical therapist had to judge them able to tolerate both grade III and grade IV knee mobilization. Finally, they must have met clinical criteria for knee OA as described by the American College of Rheumatology.31,32 These clinical criteria are knee pain for most days of the prior month with: crepitus with active motion, morning stiffness in the knee ⩽30 minutes and age ⩾38; or crepitus and morning stiffness >30 minutes; or no crepitus and bony enlargement of the knee.32,33 Exclusion criteria included absence of knee joint pain, pain in the knee joint area referred from another region,32 diagnostic or therapeutic injections to the knee within the last 30 days, history of knee joint replacement surgery on the involved limb, or evidence of systemic rheumatic conditions affecting the knee (such as rheumatoid arthritis).
Before biomechanical data collection, each subject completed intake forms and reported age, height, body weight, duration of knee symptoms, and other demographic factors. To describe the impact of their symptoms on function, the subjects also completed the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scale. This instrument is a self-report questionnaire that asks patients to rate their pain, stiffness, and functional limitation associated with their condition.34,35 It has been determined to be a reliable, valid, and responsive instrument in evaluating knee OA.36 Subjects also completed the numeric pain rating scale (NPRS) before and immediately after testing to describe the sample and account for any effect pain might have had on the measurements (not as an outcome measure). This eleven point (0–10) NPRS has demonstrated reliability, responsiveness, and validity.37,38 A radiologist determined the radiographic severity of knee OA in each subject according to the Kellgren–Lawrence scale. The Kellgren–Lawrence scale for grading knee OA is a 5 point rating scale of 0 to 4 to describe the degree of knee OA as measured by plain radiographs.39 There is currently conflicting evidence regarding the correlation between pain complaints and radiographic measurement of OA via the Kellgren–Lawrence scale.40,41 Despite concerns about its validity, correlation to pain complaints, and its consistency between studies,42 this scale is widely used to describe the radiographic severity of knee OA.43 Similar to the WOMAC and NPRS, this scale is reported as a description of our patient sample.
Instrumentation
A capacitance-based pressure platform (Pliance-x®, Novel Electronics Inc., St Paul, MN, USA) was used as a portable biomechanical data capture package for the measurement of variables such as force and pressure distribution (Fig. 1A–D). The system consists of a flexible capacitance-based pressure measuring mat, a multi-channel analyzer, a calibration device, and a software package for the Windows computer operating system. The system works with capacitive transducers in a matrix configuration inside the mat. The sensor mat used in this study was calibrated prior to data collection.
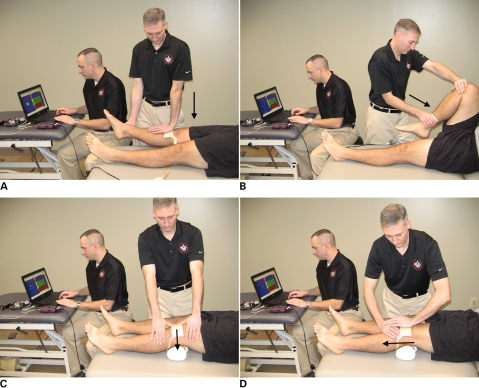
Figure 1.
(A) The extension technique, (B) the flexion technique, (C) the medial–lateral glide technique and (D) the inferior glide technique.
Data collection procedures
After completion of the consent process and the demographic forms, each subject lay supine on a standard physical therapy treatment table. A board-certified, fellowship-trained physical therapist (male, ht: 1·83 m, wt: 74·84 kg) with 12 years of clinical experience at the time of the study (author NWG) applied the joint mobilization techniques in this study. Each subject received four mobilization techniques applied to the symptomatic knee at both grade III and grade IV (a total of eight technique-grade combinations for two trials each with a total of 16 bouts per subject). Before mobilizing the knee, a brief manual examination was performed and the physical therapist assessed the pain and resistance through the range of each movement. This served to condition the joint to movement, demonstrate the movement to the patient and assess tolerance, and is part of the typical clinical examination process. The order of the techniques delivered was counterbalanced across all subjects with a master spreadsheet. The physical therapist performed one trial of mobilization followed by a 60 second rest and then a second trial of the same mobilization technique at the same grade. During each trial of mobilization, 15 seconds of data were captured. A 1-minute rest was followed by the next technique-grade combination. Once two trials of each technique-grade combination were applied and the data were captured and verified, the NPRS was collected and the subject’s participation was complete. Each testing session lasted between 45 minutes and 1 hour per subject.
The independent variables were mobilization grade, with two levels (grade III, grade IV) and mobilization technique, with four levels (extension, flexion, medial–lateral glide, and inferior glide). We used grade III (large movement into resistance) and grade IV (small movement into resistance) mobilizations. Mobilization techniques are depicted in Fig. 1A–D. A screen capture of the force readout for the Pliance system for a sample of grade III and grade IV mobilizations can be found in Figure 5. The mat was placed directly on the skin overlying the anterior superior tibia for the extension technique, on the distal tibiofibular area for the flexion technique, and the medial or superior patella for the medial–lateral and inferior glide techniques. In all cases the mat was placed between the hand providing the mobilizing force and the subject (Fig. 1A–D).
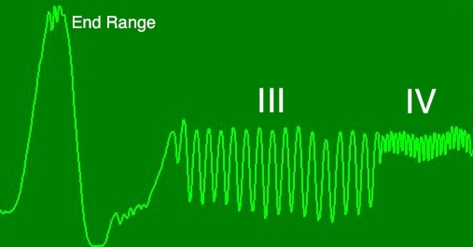
Figure 5.
A screen capture of the Pliance system output of force over time. The vertical axis is force and the horizontal axis is time. This example demonstrates the force at end range and then a series of Grade III followed by Grade IV mobilizations in mid range.
The dependent variables captured were mean force, maximum force, FTI, peak-to-peak amplitude, and oscillation frequency. Mean force was the average force measurement across all active sensors on the mat during the trial, and was measured in Newtons (N). Maximum force was the highest force value from any sensor on the mat during the trial, and was also measured in Newtons. Force–time integral is the product of the force over time, and can be considered as a measure of the total dosage of force applied. A simple illustration of FTI is the application of 10 N of force over 5 seconds, which would result in an FTI measurement of 50 – the same reached with 25 N applied over 2 seconds. In a graphical depiction of the force over time, the FTI is also the area under the force curve. Force–time integral is reported in Newton–seconds (N*s). Peak-to-peak amplitude was the difference between the highest and lowest force measurement during each trial, and was reported in Newtons (N). Oscillation frequency was the number of peaks in the oscillatory pattern of mobilization during the 15-second data capture, and was reported in oscillations per second or Hertz.
Data analysis
Descriptive statistics were calculated for subjects’ age, gender, height, weight, body mass index, WOMAC score, NPRS score, Kellgren–Lawrence osteoarthritis severity score, and use of medications to manage knee pain. Descriptive statistics were also calculated to quantify the biomechanical dependent variables of mean force, maximum force, FTI, peak-to-peak amplitude, and oscillation frequency. Kolmogorov-Smirnoff tests were performed on all dependent variables to test the normality assumption for parametric statistical analysis.
The intraclass correlation coefficient (ICC3,1) was calculated for each dependent variable using trial 1 and trial 2 of every technique-grade combination (eight combinations per subject) to assess intrarater reliability. Although no clear standards exist, ICC values above 0·75 are generally considered good reliability; and for clinical ratings measures at or above 0·90 have been suggested as a target to ensure reasonable validity.44 Standard error of measurement (SEM) was calculated as a measure of response stability.
All dependent variables (mean force, maximum force, FTI, peak-to-peak amplitude, and oscillation frequency) were also analyzed using a 2×4 (grade×technique) repeated measures analysis of variance with significance level at 0·05 and post-hoc comparisons with Sidak correction. Mauchly’s Test of Sphericity was performed and the Greenhouse–Geisser correction was used for any comparisons found to violate the sphericity assumption.
A 2-tailed paired t-test with significance level of 0·05 was used to compare the mean NPRS pain scale before data collection and the mean NPRS pain score after data collection.
Data were processed with the Novel Database Medical software (Novel Electronics Corporation, St. Paul, MN, USA) and exported to Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) and SPSS for Windows version 16.0 (SPSS Inc., Chicago, IL, USA) for analysis.
Results
Twenty-two patients were screened and two were excluded due to recent intra-articular steroid injections; the remaining 20 patients consented to and completed the study. Characteristics of study subjects are described in Table 1. An a priori power analysis was performed using G*Power software (Heinrich-Heine University, Dusseldorf, Germany). At a 0·05 alpha level and using an effect size for the grade III to grade IV difference by Snodgrass et al.,45 we needed to recruit at least 16 subjects to obtain 80% power. We collected 20 subjects due to the exploratory nature of the equipment and methods.
Table 1. Subject demographic data.
| Age (y) | 54 (8·0), 40–66 |
| Gender | 7 female, 13 male |
| Height (m) | 1·7 (0·1), 1·5–1·9 |
| Weight (kg) | 94·2 (21·8), 58·9–145·1 |
| BMI (kg/m2) | 31·5 (5·5), 21·6–39·3 |
| Duration of symptoms (mos) | 112·2 (126·9), 0·8–420 |
| WOMAC score (0–240) | 83·6 (46·6), 0–181 |
| NPRS (0–10) | 2·9 (1·9), 0–7 |
| Kellgren–Lawrence score (0–4) |
Note: Presented as ‘mean (SD), range’ unless otherwise noted. Abbreviations: y = years, m = meters, kg = kilograms, BMI = Body Mass Index, mos = months, WOMAC = Western Ontario and McMaster Osteoarthritis Index, NPRS = Numeric Pain Rating Scale.
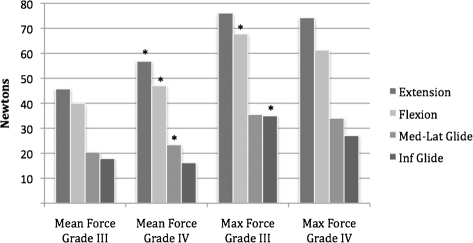
Mean force demonstrated a significant interaction effect for grade×technique (F = 8·3, df = 3, P<0·001), along with significant main effects of grade (F = 21·5, df = 1, P<0·001) and technique (F = 93·9, df = 3, P<0·001). Interactions were ordinal concerning the tibiofemoral versus patellofemoral comparison. Between techniques, the mean force measurements were significantly greater for the tibiofemoral compared to the patellofemoral joint at both grades (P<0·001), with extension greater than flexion at grade IV (P = 0·011) and medial–lateral greater than inferior at grade IV only (P = 0·007). Between grades, mean force was significantly greater at grade IV for extension, flexion, and medial–lateral glide compared to grade III (P = 0·029 or less), as shown in Fig. 2. Mean force measurements for the tibiofemoral techniques were between 39·9 and 56·8 N and between 16·2 and 23·3 N for the patellofemoral techniques (Table 2).
Figure 2.
Mean and maximum force measurements. * = Significant difference between grade III and IV.
Table 2. Force and frequency measurements.
| Mean force |
Max. force |
Peak to peak amplitude |
Force–time integral |
Oscillation frequency |
||
| Technique | Grade | N | N | N | N*s | Hz |
| Extension | III | 45·7 (13·7) | 76·1 (19·8) | 71·3 (21·4) | 726·2 (218·6) | 1·1 (0·2) |
| IV | 56·8 (15·2) | 74·2 (19·5) | 32·8 (9·8) | 900·9 (243·7) | 2·4 (0·2) | |
| Flexion | III | 39·9 (11·2) | 67·7 (15·8) | 53·4 (19·6) | 632·7 (174·4) | 0·9 (0·2) |
| IV | 47·0 (15·0) | 61·2 (16·6) | 25·7 (6·9) | 744·0 (238·0) | 2·1 (0·3) | |
| Medial–lateral Glide | III | 20·4 (7·5) | 35·5 (9·7) | 34·8 (9·2) | 324·3 (120·7) | 1·2 (0·2) |
| IV | 23·3 (7·4) | 34·0 (8·2) | 22·6 (7·0) | 370·9 (118·3) | 2·4 (0·3) | |
| Inferior Glide | III | 17·8 (7·5) | 34·9 (12·3) | 37·5 (13·2) | 283·3 (120·5) | 1·1 (0·1) |
| IV | 16·2 (7·5) | 27·0 (9·5) | 20·6 (5·5) | 256·7 (119·2) | 2·4 (0·2) |
Note: Presented as mean (SD) for all measures. N = Newtons, N*s = Newton–seconds, Hz = Hertz.
Maximum force demonstrated a significant interaction effect for grade×technique (F = 2·8, df = 3, P = 0·049), along with significant main effects of grade (F = 13·3, df = 1, P = 0·002) and technique (F = 106·7, df = 3, P<0·001). Interactions were ordinal concerning the tibiofemoral versus patellofemoral comparison. Between techniques the maximum force measurements showed tibiofemoral measures significantly greater than patellofemoral measures at both grades (P<0·001), extension significantly greater than flexion at grade IV (P = 0·004), and medial–lateral significantly greater than inferior at grade IV (P = 0·021), as shown in Fig. 2. Maximum force measurements for the tibiofemoral techniques were between 61·2 and 76·1 N; and between 27·0 and 35·5 N for the patellofemoral techniques (Table 2).
Force–time integral demonstrated a significant interaction effect for grade×technique (F = 8·1, df = 3, P<0·001), along with significant main effects of grade (F = 21·4, df = 1, P<0·001) and technique (F = 93·9, df = 3, P<0·001). Interactions were ordinal concerning the tibiofemoral versus patellofemoral comparison. Tibiofemoral measures of FTI were significantly greater than the patellofemoral measures (P<0·001). The FTI measurements were significantly greater for the extension than the flexion technique at grade IV, and medial–lateral glide was significantly greater than inferior glide at grade IV (P = 0·011 and 0·006 respectively). Force–time integral measures were significantly higher at grade IV than grade III for all techniques except inferior glide (P = 0·031 or less). Force–time integral measurements for the tibiofemoral techniques were between 632·7 and 900·9 N*s and between 256·7 and 370·9 N*s for the patellofemoral techniques (Table 2).
Peak-to-peak amplitude demonstrated a significant interaction effect for grade×technique (F = 29·4, df = 3, P<0·001), along with significant main effects for grade (F = 118·5, df = 1, P<0·001) and technique (F = 43·7, df = 3, P<0·001). Interactions were ordinal concerning the tibiofemoral versus patellofemoral comparison. Between techniques, the peak-to-peak amplitude measurements for tibiofemoral techniques were greater than the patellofemoral techniques at grade III (P = 0·002 or less). At grade IV, extension was greatest (P = 0·011 or less), flexion was greater than inferior glide (P = 0·041), and not different than medial–lateral glide (P = 0·585), and the patellofemoral techniques were not significantly different from each other (P = 0·769). Peak-to-peak amplitude measurements were greater for grade III than for grade IV for all techniques (P<0·001). The peak-to-peak amplitudes for the tibiofemoral techniques were between 25·7 and 71·3 N; and between 20·6 and 37·4 N for the patellofemoral techniques (Table 2).
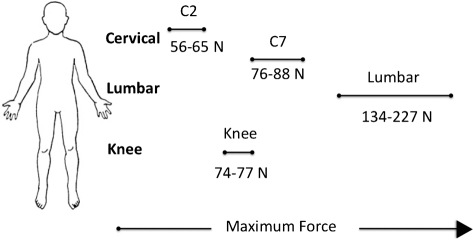
Figure 4.
Force comparisons of maximum force means for grade III and IV joint mobilizations (PA glides C2, C7 and lumbar, and knee tibiofemoral joint).22,45–49,51
For oscillation frequency, the grade×technique comparison was not significant (F = 1·0, df = 3, P = 0·379) but we observed a main effect for grade (F = 284·5, df = 1, P<0·001) and for technique (F = 18·0, df = 3, P<0·001) (Fig. 3). Grade III oscillation frequency measurements were less than grade IV for all techniques (P<0·001), and the flexion technique showed lower oscillation frequency measurements than all other techniques (P = 0·001 or less) at both grades except for grade IV, where flexion and medial–lateral glide were not different (P = 0·087), as shown in Fig. 3. Oscillation frequency measurements were between 0·94 and 1·24 Hz (oscillations per second) for the grade III techniques and between 2·14 and 2·49 Hz for the grade IV techniques (Table 2).
Figure 3.
Oscillation frequency measurements. * = Significant difference between grade III and IV; + = Significant difference from other techniques.
Intrarater reliability
Intrarater reliability using ICC3,1 for the mean force, maximum force, and FTI measured between 0·88 and 0·96, except for the medial–lateral glide technique at grade IV that was 0·75 (Table 3). SEM values were between 1·68 and 5·75 N for mean and maximum force, and between 24·66 and 78·94 N*s for FTI (Table 4). ICC3,1 for peak-to-peak amplitude measured between 0·88 and 0·96 (Table 3). Values for the SEM for peak-to-peak amplitude were between 1·71 and 5·24 N (Table 4). ICC3,1 for the oscillation frequency measurements were nearly all at or above 0·90, measuring between 0·86 and 0·98 (Table 3). Values for the SEM for oscillation frequency were between 0·03 and 0·10 Hertz (Table 4).
Table 3. Reliability measures using ICC3,1 with 95% confidence intervals.
| Technique | Grade | Mean force | Maximum force | Peak to peakamplitude | Force–time integral | Oscillation frequency |
| Extension | III | 0·95 (0·88 to 0·98) | 0·94 (0·86 to 0·98) | 0·94 (0·85 to 0·98) | 0·95 (0·88 to 0·98) | 0·96 (0·91 to 0·99) |
| IV | 0·92 (0·81 to 0·97) | 0·94 (0·86 to 0·98) | 0·96 (0·91 to 0·99) | 0·92 (0·81 to 0·97) | 0·86 (0·67 to 0·94) | |
| Flexion | III | 0·94 (0·85 to 0·98) | 0·93 (0·84 to 0·97) | 0·95 (0·88 to 0·98) | 0·98 (0·94 to 0·99) | 0·98 (0·94 to 0·99) |
| IV | 0·89 (0·75 to 0·96) | 0·93 (0·82 to 0·97) | 0·88 (0·73 to 0·95) | 0·89 (0·75 to 0·96) | 0·89 (0·75 to 0·96) | |
| Medial–lateral glide | III | 0·95 (0·89 to 0·98) | 0·96 (0·89 to 0·98) | 0·95 (0·88 to 0·98) | 0·95 (0·88 to 0·98) | 0·93 (0·83 to 0·97) |
| IV | 0·75 (0·47 to 0·89) | 0·75 (0·48 to 0·90) | 0·94 (0·85 to 0·98) | 0·75 (0·48 to 0·90) | 0·93 (0·84 to 0·97) | |
| Inferior glide | III | 0·95 (0·89 to 0·98) | 0·94 (0·85 to 0·98) | 0·96 (0·91 to 0·99) | 0·95 (0·88 to 0·98) | 0·92 (0·81 to 0·97) |
| IV | 0·93 (0·83 to 0·97) | 0·93 (0·82 to 0·97) | 0·89 (0·75 to 0·96) | 0·93 (0·83 to 0·97) | 0·91 (0·79 to 0·96) |
Table 4. Standard errors of measurement for force & frequency measures for each applied technique.
| Mean force |
Maximum force |
Peak to peak amplitude |
Force–time integral |
Oscillation frequency |
||
| Technique | Grade | N | N | N | N*s | Hz |
| Extension | III | 3·06 | 4·85 | 5·24 | 48·88 | 0·04 |
| IV | 4·30 | 3·90 | 1·96 | 68·93 | 0·07 | |
| Flexion | III | 2·74 | 3·53 | 4·38 | 24·66 | 0·03 |
| IV | 4·97 | 5·75 | 2·39 | 78·94 | 0·10 | |
| Medial–lateral glide | III | 1·68 | 2·17 | 2·06 | 26·99 | 0·05 |
| IV | 3·70 | 2·01 | 1·71 | 59·15 | 0·08 | |
| Inferior glide | III | 1·68 | 2·46 | 2·64 | 26·94 | 0·03 |
| IV | 1·98 | 3·15 | 1·82 | 31·54 | 0·06 |
Note: N = Newtons, N*s = Newton-seconds, Hz = Hertz.
Knee pain before and after testing procedure
Resting knee pain before and after testing was recorded to account for any possible effect of pain on the measures. However, no significant difference between the pre- and post-testing NPRS was demonstrated (t = 1·76, P = 0·094). Mean pain rating (mean±SD) before testing was 2·9±1·9 and after testing was 2·4±2·3, with a mean difference of 0·5±0·3.
Discussion
The key findings were the biomechanical description of the techniques with our dependent variables, the observed differences between grades of mobilization in biomechanical measures consistent with their textbook description (greater peak to peak amplitude and lower oscillation frequency for the grade III mobilizations compared to grade IV mobilizations) and the overall excellent intrarater reliability.
These results can be put into perspective by comparing the quantitative data from knee joint mobilizations in this study to biomechanical studies characterizing the forces for spinal22,46 and other peripheral joint21,23 mobilizations. Although direct comparisons are not possible due to the differences in instrumentation (e.g. use of a force plate, instrumented table, or flexible mat) and differences in dependent measures, some general comparisons put the mean and maximum force measured in knee mobilization at the upper range of those reported for cervical spine posterior to anterior (PA) mobilization,47 and the lower range of those reported for lumbar PA mobilization46,48 (Fig. 4). Mean and maximum force were greater for the tibiofemoral techniques than the patellofemoral techniques, consistent with the relative difference in size and biomechanical motion between the two joints – as well as the difference in application of the techniques themselves. Overall, mean and maximum force measurements where highest for extension, and both tibiofemoral techniques showed greater forces than the patellofemoral techniques. In general, mean force measures were greater at grade IV versus grade III and no consistent differences between grades were observed in terms of maximum force (Fig. 2). We selected grade III and IV mobilizations since they were felt to be the most commonly used in clinical practice. Maitland et al.15 defines a grade III mobilization as a large amplitude movement performed into resistance or up to the limit of the available range. A grade IV mobilization is a small amplitude movement performed into resistance or up to the limit of the available range. A grade IV mobilization is not necessarily any further into the resistance than a grade III mobilization (only the peak to peak amplitude should be different) and our maximum force results largely reflect this concept. The force readout from the Pliance device for a sample of grade III and grade IV mobilizations illustrates this (Fig. 5).
Force–time integral results have not been reported in other studies. This variable may represent a way to characterize ‘dosage’ since it measures force over the mobilization time. We found greater FTI measurements with grade IV mobilizations, possibly owing to a greater portion of the treatment time providing higher forces. A ‘higher dosage’ might be expected with a grade IV mobilization since a grade III mobilization will oscillate into lower ranges of resistance due to the large amplitude.
The peak-to-peak amplitude was found to be greater for the grade III than the grade IV techniques, consistent with the descriptive model of these grades according to Maitland et al.15 and consistent with previous work on joint mobilization by other authors.47
The oscillation frequency for the mobilizations was approximately 1 Hz (1 oscillation per second) for grade III and approximately 2·5 Hz (2·5 oscillations per second) for grade IV. This fits the general model of oscillation frequency described by Maitland et al.15 of between 0·5 and 3 oscillations per second and demonstrates agreement with the conceptual model of joint mobilization. The flexion technique had significantly lower oscillation frequency both at grade III and grade IV than the other techniques. These slower speeds may be due to the larger range of movement involved in the performance of the technique, which would naturally result in lower oscillation frequencies.
In summary we observed differences between grade III and grade IV mobilizations consistent with our hypotheses. Mean force was generally greater at grade IV, and maximum force showed no consistent differences between the two grades. There were also differences in oscillation frequency and peak-to-peak amplitude of the oscillations during the joint mobilizations. As expected, and consistent with the work of Snodgrass et al.,47 grade III mobilizations demonstrated larger peak-to-peak amplitude when compared to grade IV mobilizations. Consistent with the conceptual joint mobilization model, we also found greater oscillation frequency at grade IV than grade III.
Intrarater reliability with ICC3,1 was excellent, with most measures at or above 0·90. Several studies reporting biomechanical parameters of joint mobilization such as force or oscillation frequency have not included reliability calculations.46,48,49 However, recent work in the cervical spine29,45,47,50 included both similar biomechanical parameters and reliability calculations and provides an opportunity to put our results in context. Though there are differences in raters, calculations and instrumentation, our reliability was equal to or greater than that reported in the cervical spine.47
There are several clinical conclusions that might be drawn from our results. The first is that the forces measured during knee joint mobilization are fairly small, supporting the overall safety profile of physical therapy interventions and the established data favoring this manual therapy approach over exercise alone in previously published randomized trials.11,12 Secondly, the parameters measured fit generally into the textbook description of these techniques by Maitland et al.15 While research data can sometimes challenge the underlying clinical constructs used in patient care, these data seem to support a close relationship between the theory and practice of manual therapy in this situation. Also, this study describes the instrumentation and methodology to further investigate inter and intrarater reliability and normative force data of manual techniques not only at the knee, but at other locations in the body, which can be used both for feedback and teaching as well as further description of manual therapy practice.
Limitations and generalizability
In comparison to the subjects in randomized trials11,12 demonstrating the effectiveness of this approach, this subject sample had a greater proportion of males and was on average 8 years younger. The sample used here may or may not be reflective of the larger population with symptomatic knee OA who might benefit from physical therapy. In other studies of joint mobilization, subject and clinician demographic characteristics (such as gender) have influenced the forces provided. Due to the small sample with one clinician providing the mobilization, our results are best interpreted as pilot data instead of normative data.
Using a board-certified, fellowship-trained physical therapist as the only rater limits the generalizability of the findings as well. The excellent reliability and clear differences between grade III/IV and between tibiofemoral/patellofemoral techniques may not generalize to all physical therapists or other manual medicine clinicians with less formal training in manual therapy or fewer years of experience.
The measuring instrumentation is another source of potential limitations. The flexible mat in the system was designed more for pressure measurement than force characterization over time. The capacitance-based sensors in the mat are designed to measure forces perpendicular to the sensor – as such they do not account for all of the forces applied during the mobilization. However, the impact of this limitation is expected to be negligible as the manual therapy techniques that were used involved placing most forces perpendicular to the mat.
Conclusions
Scant evidence exists to describe key biomechanical parameters of knee joint mobilization, especially in a clinically relevant sample of symptomatic subjects with knee OA. Measurement of mean force, maximum force, FTI, peak-to-peak amplitude, and oscillation frequency revealed differences between grade III and grade IV mobilizations and between tibiofemoral and patellofemoral techniques that were consistent with the textbook description15 of the techniques and the underlying manual therapy constructs. Force magnitudes were between those currently reported for cervical and lumbar mobilization. Intrarater reliability of a single, experienced physical therapist for each of the measures was excellent overall. This study provides a proof of concept and initial data for the further exploration and description of joint mobilization techniques using these methods.
Acknowledgments
The authors would like to acknowledge the assistance of Ms Maria Pasquale MS of Novel Electronics USA for her technical assistance, Dr Liem Mansfield MD for radiological interpretation of knee radiographs, Dr Timothy Allison PhD for assistance with aspects of data processing and nomenclature, and Dr Daniel Rhon DPT, DSc and Dr Norman Ayotte PT, DSc for their essential early work on this concept.
The opinions and content of this paper reflect the authors' personal opinions and work and do not reflect the official policy or position of the United States Army, the Department of Defense, or the United States Government.
References
- 1.Helmick CG, Felson DT, Lawrence RC, Gabriel S, Hirsch R, Kwoh CK, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum 2008;58:15–25 [DOI] [PubMed] [Google Scholar]
- 2.Aluoch MA, Wao HO. Risk factors for occupational osteoarthritis: a literature review. AAOHN J 2009;57:283–90; quiz 91–2 [PubMed] [Google Scholar]
- 3.Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum 2008;59:1207–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 2008;58:26–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Rheum Dis Clin North Am 2008;34:515–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Laupattarakasem W, Laopaiboon M, Laupattarakasem P, Sumananont C. Arthroscopic debridement for knee osteoarthritis. Cochrane Database Syst Rev 2008;(1):CD005118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Psaty BM, Furberg CD. COX-2 inhibitors–lessons in drug safety. N Engl J Med 2005;352:1133–5 [DOI] [PubMed] [Google Scholar]
- 8.Wittenberg RH, Schell E, Krehan G, Maeumbaed R, Runge H, Schluter P, et al. First-dose analgesic effect of the cyclo-oxygenase-2 selective inhibitor lumiracoxib in osteoarthritis of the knee: a randomized, double-blind, placebo-controlled comparison with celecoxib [NCT00267215]. Arthritis Res Ther 2006;8:R35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Towheed TE, Maxwell L, Judd MG, Catton M, Hochberg MC, Wells G. Acetaminophen for osteoarthritis. Cochrane Database Syst Rev 2006;(1):CD004257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nussmeier NA, Whelton AA, Brown MT, Langford RM, Hoeft A, Parlow JL, et al. Complications of the COX-2 inhibitors parecoxib and valdecoxib after cardiac surgery. N Engl J Med 2005;352:1081–91 [DOI] [PubMed] [Google Scholar]
- 11.Deyle GD, Allison SC, Matekel RL, Ryder MG, Stang JM, Gohdes DD, et al. Physical therapy treatment effectiveness for osteoarthritis of the knee: a randomized comparison of supervised clinical exercise and manual therapy procedures versus a home exercise program. Phys Ther 2005;85:1301–17 [PubMed] [Google Scholar]
- 12.Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, Allison SC. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Ann Intern Med 2000;132:173–81 [DOI] [PubMed] [Google Scholar]
- 13.Ottawa panel evidence-based clinical practice guidelines for therapeutic exercises and manual therapy in the management of osteoarthritis. Phys Ther 2005;85:907–71 [PubMed] [Google Scholar]
- 14.American Physical Therapy Association Guide to Physical Therapist Practice. Second Edition. American Physical Therapy Association. Phys Ther 2001;81:9–746 [PubMed] [Google Scholar]
- 15.Maitland G D, Hengeveld E, Banks K, ed, editors. Maitland’s peripheral manipulation. 4th ed. Oxford: Butterworth-Heinemann; 2005 [Google Scholar]
- 16.Grieve G. Mobilisation of the spine. 5th ed. Edinburgh: Churchill Livingstone; 1991 [Google Scholar]
- 17.Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther 2009;14:531–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bialosky JE, George SZ, Bishop MD. How spinal manipulative therapy works: why ask why? J Orthop Sports Phys Ther 2008;38:293–5 [DOI] [PubMed] [Google Scholar]
- 19.Sluka KA, Skyba DA, Radhakrishnan R, Leeper BJ, Wright A. Joint mobilization reduces hyperalgesia associated with chronic muscle and joint inflammation in rats. J Pain 2006;7:602–7 [DOI] [PubMed] [Google Scholar]
- 20.Triano JJ. Biomechanics of spinal manipulative therapy. Spine J 2001;1:121–30 [DOI] [PubMed] [Google Scholar]
- 21.McLean S, Naish R, Reed L, Urry S, Vicenzino B. A pilot study of the manual force levels required to produce manipulation induced hypoalgesia. Clin Biomech (Bristol, Avon) 2002;17:304–8 [DOI] [PubMed] [Google Scholar]
- 22.Snodgrass SJ, Rivett DA, Robertson VJ. Manual forces applied during posterior-to-anterior spinal mobilization: a review of the evidence. J Manipulative Physiol Ther 2006;29:316–29 [DOI] [PubMed] [Google Scholar]
- 23.de Souza MV, Venturini C, Teixeira LM, Chagas MH, de Resende MA. Force-displacement relationship during anteroposterior mobilization of the ankle joint. J Manipulative Physiol Ther 2008;31:285–92 [DOI] [PubMed] [Google Scholar]
- 24.Chiradejnant A, Maher CG, Latimer J. Objective manual assessment of lumbar posteroanterior stiffness is now possible. J Manipulative Physiol Ther 2003;26:34–9 [DOI] [PubMed] [Google Scholar]
- 25.Maher C, Adams R. Reliability of pain and stiffness assessments in clinical manual lumbar spine examination. Phys Ther 1994;74:801–9; discussion 9–11 [DOI] [PubMed] [Google Scholar]
- 26.Mootz RD, Keating JC, Jr, Kontz HP, Milus TB, Jacobs GE. Intra- and interobserver reliability of passive motion palpation of the lumbar spine. J Manipulative Physiol Ther 1989;12:440–5 [PubMed] [Google Scholar]
- 27.Binkley J, Stratford PW, Gill C. Interrater reliability of lumbar accessory motion mobility testing. Phys Ther 1995;75:786–92; discussion 93–5 [DOI] [PubMed] [Google Scholar]
- 28.Staes FF, Banks KJ, De Smet L, Daniels KJ, Carels P. Reliability of accessory motion testing at the carpal joints. Man Ther 2009;14:292–8 [DOI] [PubMed] [Google Scholar]
- 29.Snodgrass SJ, Rivett DA, Robertson VJ, Stojanovski E. Real-time feedback improves accuracy of manually applied forces during cervical spine mobilisation. Man Ther 2010;15:19–25 [DOI] [PubMed] [Google Scholar]
- 30.Latimer J, Lee M, Adams RD. The effects of high and low loading forces on measured values of lumbar stiffness. J Manipulative Physiol Ther 1998;21:157–63 [PubMed] [Google Scholar]
- 31.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 1986;29:1039–49 [DOI] [PubMed] [Google Scholar]
- 32.Altman RD. Criteria for classification of clinical osteoarthritis. J Rheumatol Suppl 1991;27:10–2 [PubMed] [Google Scholar]
- 33.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 1986;29:1039–49 [DOI] [PubMed] [Google Scholar]
- 34.Veenhof C, Bijlsma JW, van den Ende CH, van Dijk GM, Pisters MF, Dekker J. Psychometric evaluation of osteoarthritis questionnaires: a systematic review of the literature. Arthritis Rheum 2006;55:480–92 [DOI] [PubMed] [Google Scholar]
- 35.Sun Y, Sturmer T, Gunther KP, Brenner H. Reliability and validity of clinical outcome measurements of osteoarthritis of the hip and knee–a review of the literature. Clin Rheumatol 1997;16:185–98 [DOI] [PubMed] [Google Scholar]
- 36.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833–40 [PubMed] [Google Scholar]
- 37.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain 1994;58:387–92 [DOI] [PubMed] [Google Scholar]
- 38.Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain 1999;83:157–62 [DOI] [PubMed] [Google Scholar]
- 39.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Neogi T, Felson D, Niu J, Nevitt M, Lewis CE, Aliabadi P, et al. Association between radiographic features of knee osteoarthritis and pain: results from two cohort studies. BMJ 2009;339:b2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wright AA, Cook C, Abbott JH. Variables associated with the progression of hip osteoarthritis: a systematic review. Arthritis Rheum 2009;61:925–36 [DOI] [PubMed] [Google Scholar]
- 42.Schiphof D, Boers M, Bierma-Zeinstra SM. Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis 2008;67:1034–6 [DOI] [PubMed] [Google Scholar]
- 43.Menkes CJ. Radiographic criteria for classification of osteoarthritis. J Rheumatol Suppl 1991;27:13–5 [PubMed] [Google Scholar]
- 44.Portney L, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed. Upper Saddle River, NJ: Pearson Education; 2009 [Google Scholar]
- 45.Snodgrass SJ, Rivett DA, Robertson VJ. Manual forces applied during cervical mobilization. J Manipulative Physiol Ther 2007;30:17–25 [DOI] [PubMed] [Google Scholar]
- 46.Harms MC, Innes SM, Bader DL. Forces measured during spinal manipulative procedures in two age groups. Rheumatology (Oxford) 1999;38:267–74 [DOI] [PubMed] [Google Scholar]
- 47.Snodgrass SJ, Rivett DA, Robertson VJ, Stojanovski E. Forces applied to the cervical spine during posteroanterior mobilization. J Manipulative Physiol Ther 2009;32:72–83 [DOI] [PubMed] [Google Scholar]
- 48.Chiradejnant A, Latimer J, Maher CG. Forces applied during manual therapy to patients with low back pain. J Manipulative Physiol Ther 2002;25:362–9 [DOI] [PubMed] [Google Scholar]
- 49.Harms MC, Bader DL. Variability of forces applied by experienced therapists during spinal mobilization. Clin Biomech (Bristol, Avon) 1997;12:393–9 [DOI] [PubMed] [Google Scholar]
- 50.Snodgrass SJ, Rivett DA, Robertson VJ, Stojanovski E. Cervical spine mobilisation forces applied by physiotherapy students. Physiotherapy 2010;96:120–9 [DOI] [PubMed] [Google Scholar]
- 51.Snodgrass SJ, Rivett DA, Robertson VJ, Stojanovski E. A comparison of cervical spine mobilization forces applied by experienced and novice physiotherapists. J Orthop Sports Phys Ther 2010;40:392–401 [DOI] [PubMed] [Google Scholar]