Abstract
PURPOSE
To assess the relationship between radiologists’ perception of and experience with medical malpractice and their patient-recall rates in actual community-based clinical settings.
MATERIALS AND METHODS
All study activities were approved by the institutional review boards of the involved institutions, and patient and radiologist informed consent was obtained where necessary. This study was performed in three regions of the United States (Washington, Colorado, and New Hampshire). Radiologists who routinely interpret mammograms completed a mailed survey that included questions on demographic data, practice environment, and medical malpractice. Survey responses were linked to interpretive performance for all screening mammography examinations performed between January 1, 1996, and December 31, 2001. The odds of recall were modeled by using logistic regression analysis based on generalized estimating equations that adjust for study region.
RESULTS
Of 181 eligible radiologists, 139 (76.8%) returned the survey with full consent. The analysis included 124 radiologists who had interpreted a total of 557 143 screening mammograms. Approximately half (64 of 122 [52.4%]) of the radiologists reported a prior malpractice claim, with 18 (14.8%) reporting mammography-related claims. The majority (n = 51 [81.0%]) of the 63 radiologists who responded to a question regarding the degree of stress caused by a medical malpractice claim described the experience as very or extremely stressful. More than three of every four radiologists (ie, 94 [76.4%] of 123) expressed concern about the impact medical malpractice has on mammography practice, with over half (72 [58.5%] of 123) indicating that their concern moderately to greatly increased the number of their recommendations for breast biopsies. Radiologists’ estimates of their future malpractice risk were substantially higher than the actual historical risk. Almost one of every three radiologists (43 of 122 [35.3%]) had considered withdrawing from mammogram interpretation because of malpractice concerns. No significant association was found between recall rates and radiologists’ experiences or perceptions of medical malpractice.
CONCLUSION
U.S. radiologists are extremely concerned about medical malpractice and report that this concern affects their recall rates and biopsy recommendations. However, medical malpractice experience and concerns were not associated with recall or false-positive rates. Heightened concern of almost all radiologists may be a key reason that recall rates are higher in the United States than in other countries, but this hypothesis requires further study.
Failure or delay in breast cancer diagnosis continues to be the most prevalent and second-most expensive condition in malpractice claims lodged against physicians (1,2). Many of the claims occur because of mammographic misinterpretation or failure to communicate abnormalities seen at mammography in a timely fashion (2,3). In 2002, the average indemnity payment for breast cancer malpractice litigation was $438 000, a 45% increase since 1995 (1,2,4).
The topics of both medical malpractice and breast cancer are frequently in the news. A review of just three U.S. states for a 6-month period yielded more than 2500 different media events on the topics of mammography, breast cancer, and malpractice from just 45 news sources (eg, newspapers ranked among the top five in terms of circulation, medical journal articles, radiology trade publications, national public radio, and national and local network news) (5). Media exposure, both popular and professional, is obviously extensive. Despite this high level of media coverage, very little research has been conducted on how radiologists perceive the malpractice environment or how their perceptions or experiences with medical malpractice may be affecting their interpretative performance and patient-recall rates.
Several studies have involved comparison of mammographic performance indexes in the United States with those in other countries, and these have identified medical malpractice as a possible cause of the higher recall rates observed in the United States (6,7). We believed that studying this phenomenon in detail, although it constitutes a challenging task, should be done. We hypothesized that greater perceptive concerns and previous medical malpractice experiences would be associated with higher recall rates. Thus, the purpose of our study was to assess the relationships between radiologists’ perceptions of and experiences with medical malpractice and their patient-recall rates in actual community-based clinical practice.
MATERIALS AND METHODS
Study Population
This community-based, multicenter observational study involved collaboration among three geographically and clinically distinct mammography registries that capture mammographic encounter data for a substantial proportion of the population in their respective catchment areas. One of these registries, the Group Health Cooperative Breast Cancer Surveillance System (8,9), is associated with a nonprofit health plan in Washington. Another registry, the New Hampshire Mammography Network (10), captures data for more than 85% of the women in the state of New Hampshire. The third registry, the Colorado Mammography Project, captures data for approximately 50% of the women in the six-county metropolitan area of Denver, Colorado. These three mammography registries are members of the federally funded Breast Cancer Surveillance Consortium (11,12).
All study activities were approved by the institutional review boards of the University of Washington School of Medicine and the Group Health Cooperative (Washington), Dartmouth College (New Hampshire), and the Cooper Institute (Colorado). In the New Hampshire Mammography Network, patients sign informed consent statements, while the two other sites allow patients to exclude their data from research if they want, but their institutional review boards do not require informed consent for primarily clinical activity. All radiologists gave consent for the use of their survey data and to the linkage of their survey data to the performance data that had already been gathered for them by the Breast Cancer Surveillance Consortium.
Data Collection
A conceptual framework guided both survey instrument development and the interpretation of findings. We used a blended conceptual framework that integrated the Fishbein Theory of Reasoned Action (13), the Bandura Social Cognition Theory (14,15), and the Green Precede Model (16–18). The Theory of Reasoned Action has been used in several studies of physician behavior (19–21). The Bandura Social Cognition Theory, which has also been used to study physician behavior (22–24), asserts that individuals’ behaviors are influenced by a complex interaction between their attitudes and beliefs and their environment (14). Use of the Precede Model in studying physician behavior is also well established (25–28).
We developed the questionnaire and then field tested it with highly experienced and nationally recognized radiology, mammography, and malpractice specialists. We then revised and retested the questionnaire for its face validity among community radiologists who were not in the study cohort. The final four-page survey took less than 10 minutes to complete and included questions on demographics (eg, age, sex), clinical practice (eg, experience with mammography, experience with procedures), and perception of and experience with medical malpractice. A copy of the survey is available upon request. The self-administered survey was designed to collect information on demographics and clinical practices, as well as on perceptions of and experiences with medical malpractice.
Eligible radiologists included those interpreting mammograms at one of the three mammography registries between January 1, 2001, and December 31, 2001. Surveys were mailed in February 2002 from each registry. Written informed consent forms were returned with signatures by regular mail for two sites; at the third site (Colorado), informed consent was embedded in the cover letter, which stated that filling out and returning the survey gave consent to release the data collected in the survey. To enhance our response rate, we re-sent the survey and followed up with a telephone call to non-responders after 3 weeks; a total of three attempts were made to collect survey responses.
All survey data were encrypted and de-identified and sent to the statistical coordinating center in Seattle, Wash. Responses to the survey were linked to mammogram interpretations by each participating radiologist for all screening examinations performed between January 1, 1996, and December 31, 2001. Variables for each mammography examination included date, Breast Imaging Reporting and Data System (BI-RADS) (29) assessment and recommendation categories, patient clinical characteristics, and benign and malignant breast pathologic findings, which were obtained from state or Surveillance, Epidemiology, and End Results, or SEER, cancer registries and/or pathology laboratories.
Analytic Definitions
Standard definitions of accuracy (sensitivity, specificity) and recall rate developed by the Breast Cancer Surveillance Consortium by using BI-RADS categories (29) were used (30). Screening mammograms obtained in women aged 40 years and older were included in the analysis. A screening mammogram was considered positive if it was classified as BI-RADS category 0 (necessitating additional imaging evaluation), category 4 (depicting a suspicious abnormality), category 5 (revealing findings highly suggestive of malignancy), or category 3 with a recommendation for immediate work-up. If a woman underwent different BI-RADS assessments for each breast, the higher assessment level was used according to the following hierarchy (BI-RADS category 1 < 2 < 3 < 0 < 4 < 5). The recall rate was defined as the number of mammograms interpreted as positive divided by the total number of mammograms. A second, more stringent definition of recall rate was also used in which a positive mammogram was defined as one assigned a BI-RADS category of 4 or 5.
Statistical Analysis
Data for radiologists with more than 480 screening mammograms in the Breast Cancer Surveillance Consortium database were considered for the linked analysis (480 is the minimum average annual number of mammograms that radiologists are required to interpret in order to be accredited for breast imaging, according to U.S. Food and Drug Administration regulations [31]). Univariate analyses were used to examine the associations between individual radiologist recall rates and medical malpractice perceptions and experiences. Mean recall rates and 95% confidence intervals were computed for each physician.
Each radiologist’s score was weighted by the number of mammograms interpreted by that radiologist so that the overall findings would accurately reflect radiology practice and each mammogram would have the same weight. An unweighted analysis of radiologists would bias the results toward radiologists with fewer mammograms and would therefore not adequately characterize the overall effect. Assume we have two radiologists; one reads 250 mammograms with a sensitivity of 60%, and the other reads 750 mammograms with a sensitivity of 80%. We could compute their overall sensitivity as [(½ · 60) + (½ · 80)] · 100%, which would yield a value of 70%. However, the sensitivity of the first radiologist is probably less stable because he or she read fewer mammograms, while the sensitivity of the second radiologist is more stable because he or she read more mammograms. By taking their volume into account, we could compute their overall sensitivity as {[(250/1000) · 60] + [(750/1000) · 80]} · 100%, which would yield a value of 75%. If we do not take volume into account, we are assuming that both radiologists have equally representative measures of sensitivity, which may not be the case.
In addition, we performed an analysis at the mammogram level that accounted for the correlation of assessments within each radiologist. For each medical malpractice variable, the odds of recall were modeled by using logistic regression while adjusting for study site (Washington, Colorado, or New Hampshire). The logistic regression models were fit by using generalized estimating equations that assumed an independent working correlation matrix (the GENMOD procedure in the SAS software package [SAS Institute, Cary, NC]). For all analyses (performed by L.A.A. and W.E.B.), a two-sided P value of less than .05 was considered to indicate a statistically significant difference.
RESULTS
Response Rate
Of 181 eligible radiologists, 139 (76.8%) returned the survey with full consent, two (1.1%) returned the survey without consent, three (1.7%) declined to complete the survey, and 37 (20.4%) did not respond. Among the 139 consenting radiologists, 124 had interpreted 480 or more total screening mammograms within study sites and were included in our analyses. We found no significant differences in sex or number of years since medical school graduation between the responders and the nonresponders. We also found no significant differences in terms of performance in interpreting screening mammograms—that is, no differences in recall rate, sensitivity, or specificity—between the responders and the nonresponders.
Screening Population
The radiologists interpreted mammography results at 81 facilities in the three states. A total of 557 143 screening mammograms obtained in 308 634 women were interpreted by participating radiologists between 1996 and 2001. The age of the women ranged from 40 to 102 years (mean age, 56 years), and 187 295 of the mammograms had been obtained in women who were between the ages of 40 and 49 years. Breast cancer was diagnosed in 2840 women within 1 year of the screening mammography examination.
Radiologist Characteristics
Physician demographic and clinical practice characteristics are shown in Table 1. The age of the radiologists ranged from 35 to 79 years. The age distributions between male and female radiologists were similar, although there was a smaller percentage of women in the older-than-55 age category. The majority of the radiologists were male (77.4%), worked full time (74.0%), were not affiliated with an academic medical center (83.9%), had more than 10 years of experience in interpreting mammograms (77.2%), and spent less than 40% of their time working in breast imaging (87.7%). The reported number of mammograms interpreted in the year before the survey was administered ranged from 480 to more than 5000.
TABLE 1.
Demographic and Clinical Practice Characteristics of 124 Radiologists
| Characteristic | No. of Radiologists* |
|---|---|
| Demographic | |
| Age (y) | |
| 35–44 | 37 (29.8) |
| 45–54 | 48 (38.7) |
| ≥55 | 39 (31.5) |
| Sex | |
| Male | 96 (77.4) |
| Female | 28 (22.6) |
| Practice | |
| Work full time | |
| Yes | 91 (74.0) |
| No | 32 (26.0) |
| Affiliation with academic medical center | |
| Yes, primary faculty | 7 (5.6) |
| Yes, adjunct or affiliate faculty | 13 (10.5) |
| No | 104 (83.9) |
| General experience in breast imaging | |
| Fellowship training in breast imaging | |
| Yes | 6 (4.9) |
| No | 117 (95.1) |
| Years of experience in mammographic interpretation | |
| 1–4 | 9 (7.3) |
| 5–9 | 19 (15.4) |
| 10–19 | 57 (46.3) |
| ≥20 | 38 (30.9) |
| Percentage of time spent working in breast imaging | |
| <20 | 55 (45.1) |
| 20–39 | 52 (42.6) |
| 40–59 | 7 (5.7) |
| 60–79 | 3 (2.5) |
| 80–100 | 5 (4.1) |
| Work reported for previous year | |
| Total no. of mammograms interpreted | |
| <1000 | 31 (25.2) |
| 1001–2000 | 46 (37.4) |
| >2000 | 46 (37.4) |
| Percentage of mammograms that were screening mammograms | |
| ≤25 | 5 (4.1) |
| 26–50 | 5 (4.1) |
| 51–75 | 52 (42.3) |
| 76–100 | 61 (49.6) |
| No. of fine-needle aspirations performed | |
| 0 | 85 (72.6) |
| 1–50 | 27 (23.1) |
| 51–100 | 4 (3.4) |
| >100 | 1 (0.9) |
| No. of breast biopsies performed | |
| 0 | 34 (28.3) |
| 1–50 | 48 (40.0) |
| 51–100 | 20 (16.7) |
| >100 | 18 (15.0) |
| No. of breast US examinations interpreted† | |
| 0 | 3 (2.5) |
| 1–50 | 18 (14.9) |
| 51–100 | 26 (21.5) |
| >100 | 74 (61.2) |
Data in parentheses are percentages. Numbers of radiologists included for each descriptor may vary owing to missing data.
US = ultrasonographic.
Radiologist Experience and Concerns about Medical Malpractice
The radiologists’ self-reported medical malpractice experience and concerns, with associated recall rates, are shown in Table 2. Approximately half of the radiologists (64 of 122 [52.5%]) reported a prior medical malpractice claim, with 18 (14.8%) of 122 reporting mammography-related claims. Among these 18 radiologists, a total of 24 prior mammography-related claims were noted (13 radiologists cited one prior claim, four radiologists cited two prior claims, and one radiologist cited three prior claims). The reason for the claim was alleged misinterpretation of a mammogram for 20 claims, alleged misinterpretation of the results of a breast US examination for one claim, another clinician (not a radiologist) missing a lesion on a radiograph for one claim, and “unknown” in two. The majority of claims were either withdrawn (n = 11) or settled out of court (n = 9). The status of one claim was unknown, and three claims were going to trial (one trial was completed, and two were in progress) at the time of the survey. Approximately half of the claims (12 of 22 [55%]) were initiated between 1996 and 2001. Female radiologists tended to report fewer claims; however, this difference was not statistically significant. Both radiologists who were older, and those who had more years in clinical practice were significantly more likely to report a prior medical malpractice claim (P < .001 for both).
TABLE 2.
Medical Malpractice Experience and Concerns and Associated Rates of Recall and Recommendation of Surgical Evaluation or Biopsy Reported by 124 Radiologists
| Parameter | Total No. of Radiologists* | Recall Rate (%)†‡ | Rate of Recommendation of Surgical Evaluation Biopsy†§ |
|---|---|---|---|
| Personal malpractice history | |||
| Ever have a medical malpractice claim filed against you? | |||
| No | 58 (47.5) | 11.2 (10.2, 12.2) | 0.41 (0.3, 0.5) |
| Yes, non–mammography-related claim | 46 (37.7) | 8.9 (7.7, 10.1) | 0.48 (0.3, 0.6) |
| Yes, mammography-related claim | 18 (14.8) | 10.1 (8.2, 12.0) | 0.51 (0.2, 0.9) |
| If you had a past claim, how stressful was it? | |||
| Not at all or slightly | 3 (5) | 5.8|| | 0.22|| |
| Moderately | 9 (14) | 11.7 (8.1, 15.4) | 0.83 (0.4, 1.3) |
| Very | 21 (33) | 9.4 (7.9, 10.8) | 0.29 (0.2, 0.4) |
| Extremely | 30 (48) | 8.6 (7.1, 10.1) | 0.54 (0.3, 0.8) |
| Who pays your medical malpractice insurance? | |||
| Facility | 111 (89.5) | 10.2 (9.5, 11.0) | 0.43 (0.3, 0.5) |
| Myself | 12 (9.7) | 8.8 (5.7, 12.0) | 0.83 (0.4, 1.3) |
| Other | 1 (0.8) | NC | NC |
| Perceived impact on practice | |||
| I am concerned about the impact malpractice is having on my practice of mammography | |||
| Strongly disagree | 0 | NC | NC |
| Disagree | 9 (7.3) | 12.3 (8.4, 16.2) | 0.61 (0.1, 1.1) |
| Neutral | 20 (16.3) | 9.1 (7.2, 11.0) | 0.40 (0.1, 0.7) |
| Agree | 47 (38.2) | 10.4 (9.3, 11.5) | 0.40 (0.3, 0.5) |
| Strongly agree | 47 (38.2) | 10.0 (8.8, 11.3) | 0.50 (0.3, 0.7) |
| How have malpractice concerns influenced your recommendation of diagnostic mammograms and/or US? | |||
| Greatly decreased | 0 | NC | NC |
| Moderately decreased | 0 | NC | NC |
| Not changed | 34 (27.6) | 10.4 (9.1, 11.7) | 0.38 (0.2, 0.5) |
| Moderately increased | 73 (59.3) | 9.9 (8.9, 10.9) | 0.45 (0.4, 0.6) |
| Greatly increased | 16 (13.0) | 11.0 (8.9, 13.1) | 0.64 (0.1, 1.1) |
| How have malpractice concerns influenced the number of breast biopsies you recommend? | |||
| Greatly decreased | 0 | NC | NC |
| Moderately decreased | 0 | NC | NC |
| Not changed | 51 (41.5) | 10.3 (9.1, 11.5) | 0.34 (0.2, 0.5) |
| Moderately increased | 61 (49.6) | 10.1 (9.1, 11.1) | 0.51 (0.4, 0.7) |
| Greatly increased | 11 (8.9) | 10.1 (7.1, 13.1) | 0.66 (0.2, 1.2) |
| Malpractice impact on manpower | |||
| How often do you consider withdrawing from mammography because of concerns about malpractice? | |||
| Not at all | 60 (49.2) | 10.3 (9.3, 11.3) | 0.47 (0.3, 0.6) |
| Yearly | 29 (23.8) | 9.5 (8.0, 11.0) | 0.30 (0.2, 0.4) |
| Monthly | 13 (10.7) | 11.7 (9.0, 14.3) | 0.18 (0.1, 0.3) |
| Weekly | 12 (9.8) | 11.3 (8.7, 14.0) | 1.14 (0.4, 1.9) |
| Daily | 8 (6.6) | 8.1 (4.6, 11.6) | 0.57 (0.1, 1.0) |
| How often do you consider withdrawing from general radiology because of concerns about malpractice? | |||
| Not at all | 79 (64.8) | 10.0 (9.2, 10.9) | 0.42 (0.3, 0.5) |
| Yearly | 31 (25.4) | 10.2 (8.6, 11.8) | 0.55 (0.3, 0.8) |
| Monthly | 9 (7.4) | 11.4 (7.8, 15.0) | 0.36 (0.0, 0.7) |
| Weekly | 1 (0.8) | NC | NC |
| Daily | 2 (1.6) | 12.4|| | 0.75|| |
| Estimate of future malpractice risk | |||
| Perceived probability of malpractice suit in next 5 years if continue to interpret mammograms (%) | |||
| 0–19 | 31 (25.6) | 10.2 (8.6, 11.8) | 0.58 (0.4, 0.8) |
| 20–39 | 33 (27.3) | 10.0 (8.3, 11.7) | 0.28 (0.1, 0.4) |
| 40–59 | 23 (19.0) | 9.6 (8.4, 10.9) | 0.51 (0.3, 0.7) |
| 60–79 | 13 (10.7) | 11.3 (9.0, 13.6) | 0.46 (0.2, 0.7) |
| 80–100 | 21 (17.4) | 10.0 (8.2, 11.7) | 0.49 (0.1, 0.9) |
Data in parentheses are percentages. Numbers of radiologists included for each descriptor may vary owing to missing data. One radiologist with a past malpractice claim did not state how stressful the claim was.
Data in parentheses are 95% confidence intervals (given as percentages for recall rate). NC = not calculated (rates were not calculated when n = 1).
Recall rate was defined as the number of screening mammograms assigned a BI-RADS category of 0, 4, 5, or 3 with immediate work-up recommended divided by the total number of screening mammograms weighted by the number of screening mammograms obtained between 1996 and 2001.
Rate of recommendation of surgical evaluation or biopsy was defined as the number of screening mammograms assigned a BI-RADS category of 4 or 5 divided by the total number of screening mammograms weighted by the number of screening mammograms obtained between 1996 and 2001.
95% confidence intervals were not calculated when n ≤ 5.
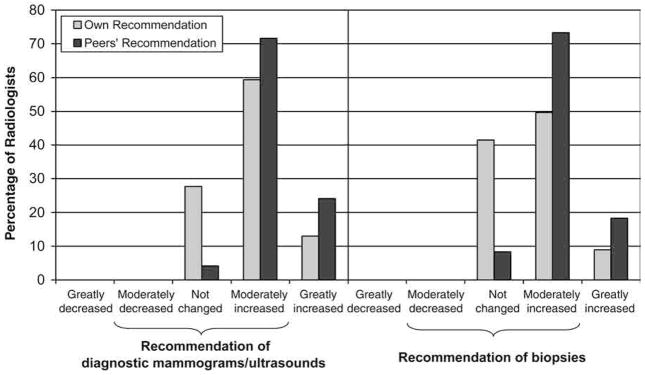
The majority of those sued (81.0%) reported the experience to be very or extremely stressful. Two response categories (“not at all stressful” and “slightly stressful”) were merged because only three of 63 radiologists (<5%) used these categories. About three of four radiologists (94 of 123 [76.4%]) either agreed or strongly agreed that they are concerned about the impact medical malpractice is having on their practice of mammography. A majority (72.4%) of radiologists believed that their concern about malpractice claims moderately or greatly increased the number of their recommendations for diagnostic mammography and/or US, while no radiologists responded that malpractice concerns decreased the number of their recommendations. More than half (58.5%) of the surveyed radiologists also believed that their concern about medical malpractice moderately or greatly increased the number of their recommendations for breast biopsies, while no radiologist reported a decrease in the number of his or her recommendations for breast biopsies because of malpractice concerns. Radiologists believed that their peers’ recommendations are more influenced by malpractice concern than their own recommendations (Fig 1).
Figure 1.
Bar graph shows that radiologists believed that their peers’ recommendations were more influenced by malpractice concern than were their own recommendations.
Recall rates for the individual radiologists ranged from 1.8% to 26.2% (Fig 2). Almost no statistically significant associations were noted between recall rates and the variables related to malpractice concerns and experience (Table 2). However, there was evidence that radiologists who reported prior non–mammography-related claims had a lower recall rate (8.9% vs 11.2%, P < .014) than those who had never had a claim (Fig 2). When we evaluated the data from the patients’ perspective, there was again evidence that screening mammograms read by radiologists with one or more prior non–mammography-related claims were less likely to be considered positive than screening mammograms read by radiologists without prior claims (P = .05) (Table 3).
Figure 2.
Graph shows no statistically significant associations between radiologist patient-recall rates and reports of prior medical malpractice claims. Each data point represents one radiologist, and error bars represent 95% confidence intervals.
TABLE 3.
A Woman’s Odds of Recall for Diagnostic Evaluation after Screening Mammography according to Radiologist Medical Malpractice Experience and Perceptions
| Parameter | Odds of Recall* | Odds of Recommendation for Surgical Evaluation or Biopsy† |
|---|---|---|
| Personal malpractice history | ||
| Ever have a medical malpractice claim filed against you? | ||
| No | 1.00 | 1.00 |
| Yes, non–mammography-related or unspecified claim | 0.81 (0.68, 0.96) | 1.16 (0.78, 1.74) |
| Yes, mammography-related claim | 0.90 (0.75, 1.07) | 1.27 (0.71, 2.25) |
| If you had a past claim, how stressful was it? | ||
| Not at all or slightly | 1.00 | 1.00 |
| Moderately | 1.58 (0.65, 3.85) | 2.13 (0.85, 5.34) |
| Very | 1.35 (0.58, 3.13) | 1.52 (0.67, 3.46) |
| Extremely | 1.14 (0.49, 2.69) | 1.86 (0.78, 4.45) |
| Who pays your medical malpractice insurance? | ||
| Facility | 1.08 (0.77, 1.50) | 0.82 (0.43, 1.57) |
| Myself | 0.91 (0.64, 1.28) | 1.53 (0.89, 2.61) |
| Other | 0.48 (0.42, 0.55)‡ | 0.37 (0.25, 0.56)‡ |
| Perceived impact on practice | ||
| I am concerned about the impact malpractice is having on my practice of mammography | ||
| Strongly disagree | … | … |
| Disagree | 1.36 (0.95, 1.96) | 1.16 (0.58, 2.33) |
| Neutral | 1.00 | 1.00 |
| Agree | 1.22 (0.99, 1.50) | 0.71 (0.44, 1.13) |
| Strongly agree | 1.12 (0.89, 1.39) | 0.85 (0.49, 1.46) |
| How have malpractice concerns influenced your recommendation of diagnostic mammograms and/or US? | ||
| Greatly decreased | … | … |
| Moderately decreased | … | … |
| Not changed | 1.00 | 1.00 |
| Moderately increased | 0.97 (0.81, 1.15) | 0.91 (0.58, 1.43) |
| Greatly increased | 0.94 (0.73, 1.20) | 1.19 (0.53, 2.68) |
| How have malpractice concerns influenced the number of breast biopsies you recommend? | ||
| Greatly decreased | … | … |
| Moderately decreased | … | … |
| Not changed | 1.00 | 1.00 |
| Moderately increased | 0.97 (0.82, 1.14) | 1.13 (0.72, 1.76) |
| Greatly increased | 0.87 (0.63, 1.20) | 1.11 (0.50, 2.43) |
| Malpractice impact on manpower | ||
| How often do you consider withdrawing from mammography because of concerns about malpractice? | ||
| Not at all | 1.00 | 1.00 |
| Yearly | 0.92 (0.77, 1.10) | 0.68 (0.50, 0.91)‡ |
| Monthly | 1.13 (0.93, 1.39) | 0.33 (0.16, 0.66)‡ |
| Weekly | 1.02 (0.83, 1.27) | 2.40 (1.63, 3.54)‡ |
| Daily | 0.74 (0.50, 1.08) | 0.95 (0.46, 1.98) |
| How often do you consider withdrawing from general radiology because of concerns about malpractice? | ||
| Not at all | 1.00 | 1.00 |
| Yearly | 0.96 (0.80, 1.14) | 1.21 (0.75, 1.96) |
| Monthly | 1.07 (0.77, 1.48) | 0.61 (0.20, 1.82) |
| Weekly | 0.57 (0.51, 0.65)‡ | 2.41 (1.94, 2.99)‡ |
| Daily | 1.04 (0.94, 1.16) | 1.86 (1.34, 2.59)‡ |
| Estimate of future malpractice risk | ||
| Perceived probability of malpractice suit in next 5 years if continue to interpret mammograms (%) | ||
| 0–19 | 1.00 | 1.00 |
| 20–39 | 0.92 (0.72, 1.17) | 0.76 (0.47, 1.21) |
| 40–59 | 0.87 (0.71, 1.08) | 0.86 (0.54, 1.38) |
| 60–79 | 0.99 (0.78, 1.27) | 0.73 (0.37, 1.45) |
| 80–100 | 0.86 (0.68, 1.09) | 1.12 (0.57, 2.20) |
Note.—Data are based on 557 143 mammograms obtained in 308 634 women and are odds ratios, with 95% confidence intervals in parentheses. Both odds of recall and odds of recommendation for surgical evaluation or biopsy were adjusted by site.
Recall rate was defined as the number of screening mammograms assigned a BI-RADS category of 0, 4, or 5 divided by the total number of screening mammograms weighted by the number of screening mammograms obtained between 1996 and 2001.
Rate of recommendation of surgical evaluation or biopsy was defined as the number of screening mammograms assigned a BI-RADS category of 4 or 5 divided by the total number of screening mammograms weighted by the number of screening mammograms obtained between 1996 and 2001.
A statistically significant difference (P < .05).
There was also no significant difference in the odds of recall when adjustments were made for sex of radiologist and site compared with the odds when adjustments were made for site alone or when just one mammography examination per woman was selected (data not shown). Additional adjustment of recall rates for woman-level characteristics (age group by decade, BI-RADS breast density rating, whether or not a previous mammogram had been performed) and geographic site (Colorado, Washington, New Hampshire) (data not shown) did not change the pattern of results for the malpractice variables; this reflects a lack of confounding by case mix. Only 18 radiologists who interpreted mammograms during 1996–2001 reported mammography-related malpractice claims on the survey, and the legal process for these claims often occurred over a long time; therefore, we were not able to discern a direct effect of individual claims on the recall rate.
Radiologists’ Desire to Leave the Field of Mammography
Almost one of three radiologists (33 of 122 [27.0%]) reported considering withdrawing from interpreting mammograms at least on a monthly basis, and 16.4% (20 of 122) reported considering withdrawing on a weekly or daily basis because of concerns about medical malpractice (Table 2). Of the eight radiologists who considered withdrawing from mammography on a daily basis because of concerns about malpractice, all reported a prior medical malpractice claim, almost all of which were not mammography related. Among those wanting to leave mammography on a daily, weekly, or monthly basis, there was no difference by age category (35–44 years, 45–54 years, or 55 or more years). Radiologists more frequently considered withdrawing from mammography than from the practice of general radiology.
Radiologists’ Perceptions of Future Malpractice Risk
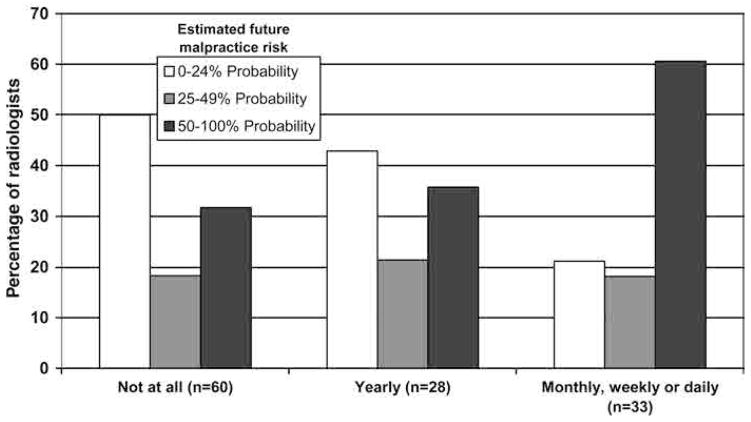
The majority of radiologists (97 of 121 [80.2%]) estimated a probability of 10% or higher that they would be sued in the next 5 years if they were to interpret mammograms full time, with 47.9% (58 of 121) estimating the probability as 30% or higher. In actuality, among radiologists who had been practicing for at least 5 years, only 8.9% (11 of 124) reported that a mammography-related claim was filed against them between 1997 and 2001. The majority of radiologists with a previous mammography-related malpractice suit thought that their probability of being sued in the next 5 years was 50% or higher. The majority of radiologists (20 of 33 [61%]) who considered leaving mammography on a monthly, weekly, or daily basis thought that their probability of being sued in the next 5 years was 50% or higher (Fig 3).
Figure 3.
Bar graph shows that the majority (61%) of radiologists who consider leaving mammography on a monthly, weekly, or daily basis thought that their probability of being sued in the next 5 years was 50% or higher. Numbers below x-axis, which indicates how often a radiologist considered leaving mammography practice, are numbers of radiologists.
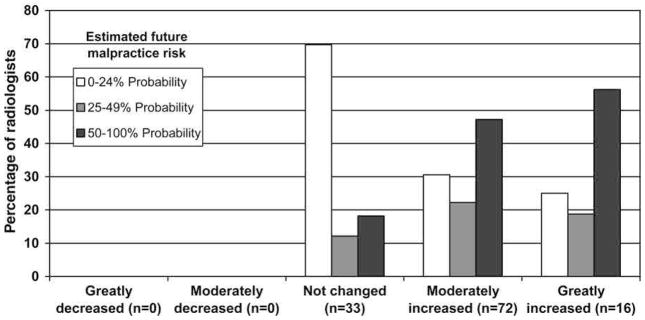
Radiologists with the highest perception of future malpractice risk also reported higher levels of influence of malpractice on their recommendations. For example, among radiologists who believed that their concerns about malpractice greatly increased the number of their recommendations for diagnostic mammography and/or US, the majority (nine of 16 [56%]) thought that their probability of being sued in the next 5 years was 50% or greater (Fig 4). Similar trends were noted between estimated future malpractice risk and perceived influence on radiologist recommendation of breast biopsies. We did not observe significant trends when we looked at the estimated probability of a future malpractice suit and the annual volume of mammographic interpretations.
Figure 4.
Bar graph shows that, of radiologists who believed that their concerns about malpractice greatly increased the number of their recommendations for diagnostic mammography and/or US, the majority (56%) thought that their probability of being sued in the next 5 years was 50% or greater. Numbers below x-axis, which indicates how radiologists characterized the influence of malpractice on the number of their recommendations for diagnostic mammography and/or US, are numbers of radiologists.
DISCUSSION
In this multisite community-based study, the majority of radiologists perceived that medical malpractice concerns affected their interpretation of mammograms. Approximately three of four radiologists believed that concern about malpractice increased the number of their recommendations for diagnostic mammography and/or US, and one of two radiologists believed that these concerns increased the number of his or her breast biopsy recommendations. Approximately one of three radiologists considered withdrawing from interpreting mammograms because of concerns about medical malpractice.
In other areas of medicine, physicians believe that medical malpractice concerns influence their clinical practice, including causing them to refer more patients to other physicians and increasing the use of tests and procedures (32–41). Interestingly, in our study, no direct association was noted between radiologists’ reported concern about medical malpractice and their recall rates in actual practice. Two opposite hypotheses are possible: One potential explanation for this finding is that fear of malpractice does not actually influence practice and that physicians have overestimated the effect malpractice concerns have on their own clinical practice (42,43). Another possible explanation (42,44,45) is that the malpractice environment and concerns about malpractice may have affected the practice patterns of all physicians, regardless of their level of malpractice claim exposure. Even the radiologists who had not reported a claim or who responded that they were not practicing defensively might unconsciously be practicing defensively. We suspect this later explanation may be the case in mammography because the recall rate has been increasing over time in the United States (46) as malpractice concerns have risen.
In addition, U.S. radiologists appear to interpret a higher percentage of mammograms as abnormal than do radiologists from other countries where malpractice is less of a concern (6,47). Handwritten survey comments by radiologists who had had a prior malpractice claim described life as miserable during the year of discovery and depositions and conveyed a sense that we, in the present investigation, had identified the main problem in breast imaging today.
The majority of radiologists surveyed in our study estimated a very high probability of a future malpractice claim. Interestingly, their predictions of future malpractice risk were substantially higher than the actual historical risk noted. If the current rate of claims continues to rise consistently over time, it is possible that these radiologists’ perceptions are correct. However, we suspect that these radiologists have highly overestimated the probability of being sued in the next 5 years. Physician perception of the risk of being sued has been heightened for many years (48). Interestingly, we see significant trends in that radiologists with heightened perceptions of future malpractice risk also more often think that malpractice influences their diagnostic recommendations and how often they consider withdrawing from the field of mammography. Education of the true risk of malpractice may allay their fears and possibly influence their mammography practice in a positive direction, reducing the false-positive rate.
The majority of women in the United States with abnormal screening mammograms do not have breast cancer but instead have false-positive examination results. It has been estimated that approximately 50% of women who undergo annual screening mammography over a decade will have at least one false-positive examination result (46). These false-positive examination results can lead to unnecessary diagnostic evaluations, with resultant high costs and possible morbidity (eg, infection after biopsy, scars), as well as provoke anxiety in women as they undergo follow-up evaluations (46). The trade-off between missing a cancer and calling too many women back for diagnostic evaluation is a challenging balance that may currently be influenced by malpractice concerns.
There were some potential limitations to this study. The surveyed radiologists were not a random sample of all U.S. radiologists but a representative sample of those interpreting mammograms in three distinct locations. It is therefore possible that these radiologists may not be completely representative of U.S. radiologists who practice mammography. This study also did not include states with the highest medical malpractice activity; indeed, we included two states with damage caps. In addition, data regarding malpractice were obtained by means of self-report, were for a short time period for some new radiologists, and were not verified; therefore, underreporting of malpractice experience was possible, and the number of radiologists reporting claims related to mammography was small.
Strengths of our study included a response rate of 76.8%, which is higher than national standards for physician surveys (49). No difference was noted between responders and nonresponders in terms of sex, number of years since medical school graduation, accuracy, and recall rates. This study in three geographic regions included community-based radiologists, not just academic radiologists, and involved a link between self-reported behavior and interpretive data from actual clinical practice.
One question this research raises is whether the heightened level of malpractice concern of practicing U.S. radiologists may lead to future workforce problems. This is of special concern because the predictions of future malpractice risk reported by radiologists may substantially overestimate the actual risk. Radiologists may refuse to interpret screening mammograms (as suggested by our data) or decide not to enter the field of mammography (as noted in a recent survey of radiology residents [50]). Demand for radiologists who can interpret mammograms will only increase in the future as more women seek screening and the population ages. Screening capacity could be affected by such a shortage, which may ultimately affect performance.
Acknowledgments
This work was primarily conducted while Dr Taplin was at Group Health Cooperative, although final writing was done while he was at the National Cancer Institute. We appreciate the dedication of participating radiologists and project support staff and the insight provided throughout this project by Alan Gelfand, PhD.
Abbreviation
- BI-RADS
Breast Imaging Reporting and Data System
Footnotes
Supported by Public Health Service grant HS-10591 (J.G.E.) from the Agency for Healthcare Research and Quality and the National Cancer Institute and surveillance grants U01 CA63731 (S.H.T.), 1 U01 CA86082-01 (P.A.C.), 5 U01 CA63736-09 (G.R.C.), and 5 U01 CA86076 (W.E.B.) from NIH and the Department of Health and Human Services and the National Cancer Institute.
Authors stated no financial relationship to disclose.
Author contributions:
Guarantor of integrity of entire study, J.G.E.; study concepts and design, all authors; literature research, J.S.F., P.A.C., J.G.E.; data acquisition, J.S.F.; data analysis/interpretation, R.E.H., G.R.C., L.A.A., S.H.T., W.E.B., J.G.E.; statistical analysis, L.A.A., W.E.B.; manuscript preparation, J.S.F.; manuscript definition of intellectual content, editing, revision/review, and final version approval, all authors
References
- 1.Physician Insurers Association of America. Breast cancer study. 3. Washington, DC: Physician Insurers Association of America; 2002. [Google Scholar]
- 2.Berlin L. Breast cancer, mammography, and malpractice litigation: the controversies continue. AJR Am J Roentgenol. 2003;180:1229–1237. doi: 10.2214/ajr.180.5.1801229. [DOI] [PubMed] [Google Scholar]
- 3.Kopans DB. Mammography screening is saving thousands of lives, but will it survive medical malpractice? [editorial] Radiology. 2004;230:20–24. doi: 10.1148/radiol.2301030619. [DOI] [PubMed] [Google Scholar]
- 4.Records SF. Female breast cancer is most prevalent cause of malpractice claims. J Okla State Med Assoc. 1995;88:311–312. [PubMed] [Google Scholar]
- 5.LexisNexis [database online] Dayton, Ohio: LexisNexis Academic; 2005. [Accessed December 1, 2003]. http://web.lexis-nexis.com/universe/ [Google Scholar]
- 6.Smith-Bindman R, Chu PW, Miglioretti DL, et al. Comparison of screening mammography in the United States and the United Kingdom. JAMA. 2003;290:2129–2137. doi: 10.1001/jama.290.16.2129. [DOI] [PubMed] [Google Scholar]
- 7.Ulcickas Yood M, McCarthy BD, Lee NC, Jacobsen G, Johnson CC. Patterns and characteristics of repeat mammography among women 50 years and older. Cancer Epidemiol Biomarkers Prev. 1999;8:595–599. [PubMed] [Google Scholar]
- 8.Carter AP, Thompson RS, Bourdeau RV, Andenes J, Mustin H, Straley H. A clinically effective breast cancer screening program can be cost-effective, too. Prev Med. 1987;16:19–34. doi: 10.1016/0091-7435(87)90003-x. [DOI] [PubMed] [Google Scholar]
- 9.Taplin SH, Mandelson MT, Anderman C, et al. Mammography diffusion and trends in late-stage breast cancer: evaluating outcomes in a population. Cancer Epidemiol Biomarkers Prev. 1997;6:625–631. [PubMed] [Google Scholar]
- 10.Carney P, Poplack S, Wells W, Littenberg B. Development and design of a population-based mammography registry: the New Hampshire Mammography Network. AJR Am J Roentgenol. 1996;167:367–372. doi: 10.2214/ajr.167.2.8686606. [DOI] [PubMed] [Google Scholar]
- 11.Ballard-Barbash R, Taplin SH, Yankaskas BC, et al. A national mammography screening and outcomes database. AJR Am J Roentgenol. 1997;169:1001–1008. doi: 10.2214/ajr.169.4.9308451. [DOI] [PubMed] [Google Scholar]
- 12. [Accessed May 4, 2005];Breast Cancer Surveillance Consortium Web site. http://breastscreening.cancer/gov/
- 13.Fishbein M. Factors influencing health behaviors: an analysis based on a theory of reasoned action. In: Landry F, editor. Health risk estimation, risk reduction and health promotion. Ottawa, Canada: CPHA; 1983. pp. 203–214. [Google Scholar]
- 14.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 15.Bandura A. Models of human nature and causality. In: Bandura A, editor. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. p. 23. [Google Scholar]
- 16.Green LW. How physicians improve patients’ participation and maintenance in self-care. West J Med. 1987;147:346–349. [PMC free article] [PubMed] [Google Scholar]
- 17.Green LW, Eriksen MP, Schor EL. Preventive practices by physicians: behavioral determinants and potential interventions. Am J Prev Med. 1988;4(suppl 4):101–107. [PubMed] [Google Scholar]
- 18.Green LW, Kreuter MW. Health promotion today and a framework for planning. Mountain View, Calif: Mayfield; 1991. Health promotion planning: an educational and environmental approach; p. 24. [Google Scholar]
- 19.Millstein SG. Utility of the theories of reasoned action and planned behavior for predicting physician behavior: a prospective analysis. Health Psychol. 1996;15:398–402. doi: 10.1037//0278-6133.15.5.398. [DOI] [PubMed] [Google Scholar]
- 20.Taylor VM, Montano DE, Koepsell T. Use of screening mammography by general internists. Cancer Detect Prev. 1994;18:455–462. [PubMed] [Google Scholar]
- 21.Gaither CA, Bagozzi RP, Ascione FJ, Kirking DM. The determinants of physician attitudes and subjective norms toward drug information sources: modification and test of the theory of reasoned action. Pharm Res. 1997;14:1298–1308. doi: 10.1023/a:1012143915886. [DOI] [PubMed] [Google Scholar]
- 22.Dietrich AJ, O’Connor GT, Keller A, Carney PA, Levy D, Whaley FS. Cancer: improving early detection and prevention—a community practice randomised trial. BMJ. 1992;304:687–691. doi: 10.1136/bmj.304.6828.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mann KV. Educating medical students: lessons from research in continuing education. Acad Med. 1994;69:41–47. doi: 10.1097/00001888-199401000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Mullen PD, Holcomb JD. Selected predictors of health promotion counseling by three groups of allied health professionals. Am J Prev Med. 1990;6:153–160. [PubMed] [Google Scholar]
- 25.Davis DA, Thomson MA, Oxman AD, Haynes RB. Evidence for the effectiveness of CME: a review of 50 randomized controlled trials. JAMA. 1992;268:1111–1117. [PubMed] [Google Scholar]
- 26.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–705. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 27.Oxman AD, Thomson MA, Davis DA, Haynes RB. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. CMAJ. 1995;153:1423–1431. [PMC free article] [PubMed] [Google Scholar]
- 28.Moss SM, Michel M, Patnick J, Johns L, Blanks R, Chamberlain J. Results from the NHS breast screening programme 1990–1993. J Med Screen. 1995;2:186–190. doi: 10.1177/096914139500200403. [DOI] [PubMed] [Google Scholar]
- 29.American College of Radiology. Breast imaging reporting and data system (BI-RADS) Reston, Va: American College of Radiology; 1993. [Google Scholar]
- 30.Ernster VL, Ballard-Barbash R, Barlow WE, et al. Detection of ductal carcinoma in situ in women undergoing screening mammography. J Natl Cancer Inst. 2002;94:1546–1554. doi: 10.1093/jnci/94.20.1546. [DOI] [PubMed] [Google Scholar]
- 31.Federal Register. Vol. 58. 1993. Mammography facilities: requirements for accrediting bodies and quality standards and certification requirements—interim rules; pp. 67557–67572. (codified at 21 CFR §900) [Google Scholar]
- 32.Klingman D, Localio AR, Sugarman J, et al. Measuring defensive medicine using clinical scenario surveys. J Health Polit Policy Law. 1996;21:185–217. doi: 10.1215/03616878-21-2-185. [DOI] [PubMed] [Google Scholar]
- 33.Bovbjerg RR, Dubay LC, Kenney GM, Norton SA. Defensive medicine and tort reform: new evidence in an old bottle. J Health Polit Policy Law. 1996;21:267–88. doi: 10.1215/03616878-21-2-267. [DOI] [PubMed] [Google Scholar]
- 34.Glassman PA, Rolph JE, Petersen LP, Bradley MA, Kravitz RL. Physicians’ personal malpractice experiences are not related to defensive clinical practices. J Health Polit Policy Law. 1996;21:219–241. doi: 10.1215/03616878-21-2-219. [DOI] [PubMed] [Google Scholar]
- 35.Jacobson PD, Rosenquist CJ. The use of low-osmolar contrast agents: technological change and defensive medicine. J Health Polit Policy Law. 1996;21:243–266. doi: 10.1215/03616878-21-2-243. [DOI] [PubMed] [Google Scholar]
- 36.Voss JD. Prostate cancer, screening, and prostate-specific antigen: promise or peril? J Gen Intern Med. 1994;9:468–474. doi: 10.1007/BF02599070. [DOI] [PubMed] [Google Scholar]
- 37.American College of Obstetricians and Gynecologists. Professional liability insurance and its effect: report of a survey of ACOG’s membership. Washington, DC: American College of Obstetricians and Gynecologists; 1985. [Google Scholar]
- 38.California Medical Association. Socioeconomic report: professional liability issues in obstetrical practice. San Francisco, Calif: California Medical Association, Bureau of Research and Planning; July/August, 1985. [Google Scholar]
- 39.California Medical Association. Socioeconomic report: professional liability issues in obstetrical practice (part 2) San Francisco, Calif: California Medical Association, Bureau of Research and Planning; October/November, 1985. [Google Scholar]
- 40.Weisman CS, Morlock LL, Teitelbaum MA, Klassen AC, Celentano DD. Practice changes in response to the malpractice litigation climate: results of a Maryland physician survey. Med Care. 1989;27:16–24. doi: 10.1097/00005650-198901000-00002. [DOI] [PubMed] [Google Scholar]
- 41.Zuckerman S. Medical malpractice: claims, legal costs, and the practice of defensive medicine. Health Aff (Millwood) 1984;3:128–133. doi: 10.1377/hlthaff.3.3.128. [DOI] [PubMed] [Google Scholar]
- 42.Baldwin LM, Hart LG, Lloyd M, Fordyce M, Rosenblatt RA. Defensive medicine and obstetrics. JAMA. 1995;274:1606–1610. [PubMed] [Google Scholar]
- 43.Thomas K. Defensive medicine and medical malpractice. Hosp Technol Ser. 1994;13(10):12–13. [PubMed] [Google Scholar]
- 44.Shapiro RS, Simpson DE, Lawrence SL, Talsky AM, Sobocinski KA, Schiedermayer DL. A survey of sued and nonsued physicians and suing patients. Arch Intern Med. 1989;149:2190–2196. [PubMed] [Google Scholar]
- 45.Charles SC, Wilbert JR, Franke KJ. Sued and nonsued physicians’ self-reported reactions to malpractice litigation. Am J Psychiatry. 1985;142:437–440. doi: 10.1176/ajp.142.4.437. [DOI] [PubMed] [Google Scholar]
- 46.Elmore JG, Barton MB, Moceri VM, Polk S, Arena PJ, Fletcher SW. Ten-year risk of false positive screening mammograms and clinical breast examinations. N Engl J Med. 1998;338:1089–1096. doi: 10.1056/NEJM199804163381601. [DOI] [PubMed] [Google Scholar]
- 47.Elmore JG, Nakano CY, Koepsell TD, Desnick LM, D’Orsi CJ, Ransohoff DF. International variation in screening mammography interpretations in community-based programs. J Natl Cancer Inst. 2003;95:1384–1393. doi: 10.1093/jnci/djg048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lawthers AG, Localio AR, Laird NM, Lipsitz S, Hebert L, Brennan TA. Physicians’ perceptions of the risk of being sued. J Health Polit Policy Law. 1992;17:463–482. doi: 10.1215/03616878-17-3-463. [DOI] [PubMed] [Google Scholar]
- 49.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 50.Bassett LW, Monsees BS, Smith RA, et al. Survey of radiology residents: breast imaging training and attitudes. Radiology. 2003;227:862–869. doi: 10.1148/radiol.2273020046. [DOI] [PubMed] [Google Scholar]