Abstract
PURPOSE
To evaluate the current (2001–2002) capacity of community-based mammography facilities to deliver screening and diagnostic services in the United States.
MATERIALS AND METHODS
Institutional review board approvals and patient consent were obtained. A mailed survey was sent to 53 eligible mammography facilities in three states (Washington, New Hampshire, and Colorado). Survey questions assessed equipment and staffing availability, as well as appointment waiting times for screening and diagnostic mammography services. Criterion-related content and construct validity were obtained first by means of a national advisory committee of academic, scientific, and clinical colleagues in mammography that reviewed literature on existing surveys and second by pilot testing a series of draft surveys among community mammography facilities not inclusive of the study facilities. The final survey results were independently double entered into a relational database with programmed data checks. The data were sent encrypted by means of file transfer protocol to a central analytical center at Group Health Cooperative. A two-sided P value with α = .05 was considered to show statistical significance in all analyses.
RESULTS
Forty-five of 53 eligible mammography facilities (85%) returned the survey. Shortages of radiologists relative to the mammographic volume were found in 44% of mammography facilities overall, with shortages of radiologists higher in not-for-profit versus for-profit facilities (60% vs 28% reported). Shortages of Mammography Quality Standards Act–qualified technologists were reported by 20% of facilities, with 46% reporting some level of difficulty in maintaining qualified technologists. Waiting times for diagnostic mammography ranged from less than 1 week to 4 weeks, with 85% performed within 1 week. Waiting times for screening mammography ranged from less than 1 week to 8 weeks, with 59% performed between 1 week and 4 weeks. Waiting times for both diagnostic and screening services were two to three times higher in high-volume compared with low-volume facilities.
CONCLUSION
Survey results show shortages of radiologists and certified mammography technologists.
In 2002, the U.S. General Accounting Office, the investigative branch of Congress, published a report on the capacity of mammography facilities to deliver screening and diagnostic services in the United States. This report demonstrated an increase in the U.S. population of women over 40 years of age who are eligible for screening and an increased utilization of screening mammography (1), but in the report it was stated that “adequate capacity to deliver mammography services exist.” Recent media reports, however, indicate that mammography facilities are closing because of several issues, including inadequate radiologist and technologist staffing (2,3). Additional concerns about medical malpractice litigation and low financial compensation may also be affecting the career choices of radiologists. Because the General Accounting Office analyzed capacity measures by using data from 1998 to 2000, the report may not be representative of the current capacity to provide mammography services.
Information regarding human resources for the field of radiology is usually anecdotal, is not mammographyspecific, and comes from academic or hospital-based settings rather than those that are community based. In addition, reports to address mammography capacity have tended to originate from industrialized countries other than the United States, such as the United Kingdom, Canada, and Australia (2–5). Here in the United States, there are few scientific data documenting either the extent to which human resource shortages in mammography exist or what effect these shortages may have on the delivery of breast cancer screening and diagnostic services.
Thus the purpose of our study was to evaluate the current (2001–2002) capacity of community-based mammography facilities to deliver screening and diagnostic services in the United States.
MATERIALS AND METHODS
Study Population
This multicenter study utilized a unique collaboration among three geographically and clinically distinct breast cancer surveillance programs composed of both community- and academic-based, as well as for-profit and not-for-profit, facilities: the Colorado Mammography Advocacy Program, which includes approximately 50% of the women in the six-county metropolitan area of Denver, Colorado; the New Hampshire Mammography Network (6), which includes over 85% of the women in the state; and a not-for-profit health plan in the Pacific Northwest, Group Health Cooperative Breast Cancer Surveillance System, which serves more than 100 000 women aged 40 years and older (7,8). These three mammography registries, which are part of the federally funded Breast Cancer Surveillance Consortium (9), differ not only in geographic location but also in how health care is delivered. Thus, they represent a broad spectrum of mammography facilities in the United States. All facilities in the three mammography registries that performed screening mammography from December 2001 to September 2002 were eligible for study. All research activities were approved by the appropriate institutional review boards, and informed consent was obtained.
Survey Development and Administration
The mammography facility survey was developed to delineate existing breast imaging services (screening and diagnostic), as well as the capacity to deliver these services at each participating facility. More specifically, survey questions were used to ascertain radiologist and Mammography Quality Standards Act (MQSA)-certified technologist–staffing levels, the volume of screening and diagnostic mammography examinations performed annually, and the length of appointment waiting times in weeks for screening and diagnostic mammography. Criterion-related content and construct validity were addressed by using two approaches. First, a national advisory committee of academic, scientific, and clinical colleagues in the fields of mammography, physics, and economics was convened to review the literature on existing surveys and to identify survey questions most relevant for use. Second, a series of draft surveys were sequentially pilot tested among community mammography facilities from regions close to but not inclusive of the study facilities. Pilot testing involved cognitive interviews either during or shortly following completion of each draft until all variables were assessed as accurately collected.
The final nine-page survey took approximately 15 minutes to complete, and all data collection activities were conducted at each of the three mammography registries. The surveys were mailed to a designated contact person at each facility, and then follow-up was conducted by using one or more of the following: second survey mailing, telephone follow-up, and/or site visits to the facilities by members of the project staff to ensure completion of data collection (E.B., S.P.T., S.H.T.). Because we recognized that different study questions might need to be completed by different facility members, respondents to each survey question were noted by using the following categories: lead technologist, other technologist, radiologist, radiology department or facility business manager, and mammography registry project office staff member (information known from frequent inter actions with facilities). Each site independently double entered data into a relational database with programmed data checks, and site coordinators resolved any data entry discrepancies. After data were checked and cleaned, they were sent encrypted by means of file transfer protocol to a central analytical center at Group Health Cooperative.
Data and Statistical Analysis
We used descriptive statistics to characterize technologist- and radiologist-related variables, including the total number of open positions for radiologists and technologists, changes in numbers of radiologists who perform mammography, and level of difficulty the facility was experiencing with personnel shortages. We used a similar approach to characterize the number of weeks patients have had to wait for screening and diagnostic mammography examinations as ascertained from the facility schedule appointments. We also analyzed technologist staffing in relation to the volume of mammography examinations performed at each site to more accurately represent the service challenges experienced at facilities. Because we could find no publications in which technologists’ times required to complete screening and diagnostic mammography were compared, estimates of mammography staffing volume for this study were based on the Medicare reimbursement formula for mammography (10). This formula included an assumption that the staffing needed to obtain a diagnostic mammogram was equivalent to that needed for two screening mammograms. A two-sided P value with α = .05 was considered to show a statistically significant difference in all analyses.
Participating facilities were further identified as urban or rural according to the zip code in which they were located, as defined in the Rural Urban Commuting Area Code classification system (11). The zip codes of all certified mammography facilities in the United States in the year 2002 were obtained from the Food and Drug Administration. These facilities were also classified as urban or rural by using the same system to allow comparison of the urban-rural distribution of surveyed facilities with that of all Food and Drug Administration–approved mammography facilities, which allowed us to assess the representativeness of our data to other geographic regions in the United States. Analyses were performed by using statistical software (SAS 8.0; SAS Institute, Cary, NC).
RESULTS
Forty-five (85%) of 53 eligible facilities responded to our survey. The lead mammography technologist at each facility gathered the majority of survey information (75%). All participating facilities provided screening mammography, while only nine (20%) provided screening mammography alone, with no other diagnostic services. Other services provided at the multi-service facilities included diagnostic mammography (76% of screening facilities, or 34 facilities), breast ultrasonography (67%, or 30 facilities), breast magnetic resonance imaging (16%, or seven facilities), breast nuclear medicine scanning (16%, or seven facilities), digital mammography (11%, or five facilities), and computer-assisted diagnosis (11%, or five facilities). Breast interventional procedures provided at facilities included cyst aspiration (53%, or 24 facilities), needle localization (51%, or 23 facilities), core biopsy (40%, or 18 facilities), fine needle aspiration (27%, or 12 facilities), and vacuum-assisted biopsy (24%, or 11 facilities). Clinical breast examination was provided routinely for women undergoing screening mammography at eight facilities (18%).
Shortages
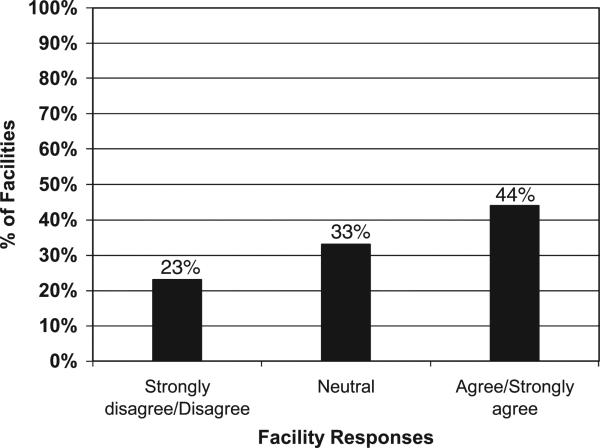
Twenty (44%) of 45 facilities reported radiologist staffing shortages (Fig 1). Compared with for-profit facilities (seven of 25 [28%]), a significant proportion of not-for-profit facilities (12 of 20 [60%]) reported being short staffed of radiolo gists (P = .01). More community-based facilities (16 of 35 [46%]) reported radiologist shortages compared with academic facilities (three of 10 [30%]); however, this difference was not statistically significant (P = .11). Data on radiologist staffing were supplied by 32 lead technologists, one business manager, six other technologists, and five radiologists. At one facility, both the lead mammography technologist and a radiologist responded to this question.
Figure 1.
Graph of responses by mammography facilities to the following: “We are currently experiencing a shortage of radiologists” (n = 45). Almost 50% of facilities are experiencing shortages for mammography image interpretation.
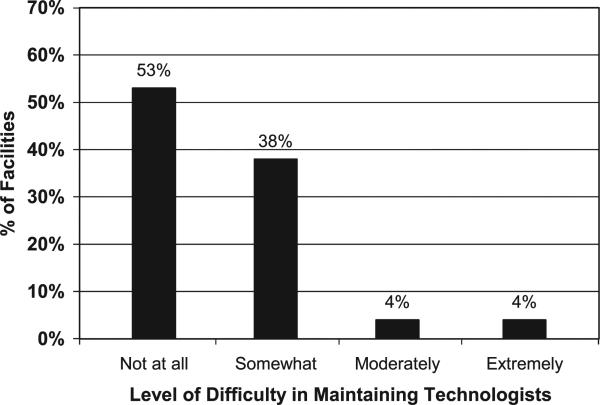
Nine facilities (20%) reported having unfilled technologist positions. Of note is that almost half of all facilities, 21 (47%) of 45, reported some level of difficulty maintaining adequate MQSA-qualified technologists (Fig 2). More for-profit facilities (14 of 25) and academic medical center–affiliated facilities (seven of 10) reported difficulty maintaining certified technologists compared with not-forprofit (seven of 20) and nonacademic facilities (14 of 35) (for profit vs not for profit, 56% vs 35%, P = .23; academic vs nonacademic, 70% vs 40%, P = .15). These findings were based on responses from the lead technologist at 41 participating facilities and from other technologists at the other four facilities. Survey results indicated that facilities with higher volume had more MQSA-certified technologists. However, findings of examination of full-time equivalent (FTE) technologist staffing per 1000 mammo-grams (diagnostic mammograms were counted as two mammograms to account for time differences between diagnostic and screening mammography) showed that facilities with lower mean technolo gist FTEs reported more difficulty maintaining MQSA-certified technologists than facilities with higher mean FTEs per 1000 mammograms (P > .05) (Table 1).
Figure 2.
Graph of reported difficulty by mammography facilities in maintaining adequate numbers of MQSA-certified technologists. Almost 50% of facilities have a problem maintaining MQSA-certified technologists.
TABLE 1.
Level of Difficulty Maintaining Adequate Numbers of MQSA-certified Technologists
| Technologist FTEs per 1000 Mammograms |
||
|---|---|---|
| Level of Difficulty | Number | Mean* |
| No difficulty | 22 | 1.32 |
| Any difficulty | 20 | 0.72 |
Mean FTE = number of FTEs × 1000/number of screening mammograms + (2 × number of diagnostic mammograms). Results were not statistically significant.
Appointment Waiting Times
The reported waiting time between facility contact by patients and scheduled appointments for diagnostic mammography was shorter than for screening mammography (Table 2). A majority of facilities (28 of 33 [85%]) reported that they were able to schedule diagnostic mammography within 1 week of the request. In contrast, only 13 (30%) of 44 facilities reported being able to schedule screening mammography within 1 week of contact. In fact, nearly half (21 of 44 [47%]) of the facilities had a waiting time of 2 or more weeks for screening mammography.
TABLE 2.
Reported Waiting Times for Scheduled Mammography Examinations
| Waiting Time (wk) | Screening Mammography (n = 44) | Diagnostic Mammography (n = 33) |
|---|---|---|
| <1 | 13 (30) | 28 (85) |
| 1–2 | 10 (23) | 4 (12) |
| 2–4 | 16 (36) | 1 (3) |
| 4–8 | 5 (11) | 0 (0) |
Note.—Data are numbers of facilities, and numbers in parentheses are percentages.
No statistical differences or indications of possible trends were noted in appointment waiting times between academic and nonacademic facilities or according to facility profit status (for profit vs not for profit). More specifically, the mean interval between facility contact and scheduled appointments for screening mammography was slightly shorter at academic facilities than at nonacademic facilities (11.6 vs 14.0 days), although this difference was not significant (P = .52). However, nonacademic facilities reported slightly shorter mean waiting times for diagnostic mammography compared with academic facilities (3.7 vs 6.8 days; P = .40). In the analysis of facilities according to profit status, for-profit facilities had shorter mean waiting times than not-forprofit facilities for both screening mammography (12.5 vs 14.7 days, P = .49) and diagnostic mammography (3.4 vs 4.9 days, P = .28), although these differences were also not significant.
Results of an examination of scheduling times according to annual volume of screening or diagnostic mammography examinations showed that sites performing more mammography examinations had significantly longer appointment waiting times (Table 3). Last, on the basis of the Rural Urban Community Area Code classification system, 12 (27%) of 45 study facilities were located within zip codes identified as rural and 33 (73%) were located within zip codes identified as urban. In comparison, 30% (2811 of 9359) of all U.S. mammography facilities are classified as within rural zip codes and 70% (6548 of 9359) are classified as within urban zip codes.
TABLE 3.
Mean Waiting Times according to Volume of Mammograms Obtained
| Screening Mammography |
Diagnostic Mammography |
|||
|---|---|---|---|---|
| Volume of Mammograms | No. of Facilities | Mean Waiting Time (d)* | No. of Facilities | Mean Waiting Time (d)† |
| ≤2000 | 14 | 9.8 | 9 | 1.9 |
| 2001–4500 | 13 | 11.0 | 10 | 4.4 |
| >4500 | 14 | 21.8 | 12 | 6.0 |
P = .0016.
P = .0983.
DISCUSSION
Our study findings highlight three critical issues in mammography screening today. First, at the same time that the demand for mammography in the United States was increasing, based at least in part on the revised U.S. Preventive Services Guidelines, we were also experiencing critical staffing shortages of both radiologists and MQSA-certified technologists. Nearly half of mammography facilities surveyed reported shortages of both radiologists and mammography technologists. Second, a similar percentage of facilities reported waiting times between contact and scheduled appointments of more than 2 weeks for screening mammography. Third, not unexpectedly, our results indicated a possible trend toward increasing waiting times for both screening and diagnostic mammography at sites with a larger mammographic volume. We suggest that this last finding is the result of limited personnel and, perhaps, available equipment. We will discuss each of these primary findings in turn.
The radiologist shortage is an important concern because delays in the interpretation of mammograms could result. Why is this shortage occurring? A survey of radiology residents regarding their attitudes toward breast imaging reveals that the majority want to spend less than 25% of their time in breast imaging (12). The high levels of malpractice litigation in breast imaging and the lower financial incentives may be possible reasons for this radiology practice preference. Another possible disincentive could be the MQSA requirements, which include both increased continuing education in mammography and the burden of tracking biopsy yield at each facility for which they interpret mammograms. Although the shortage of radiologists is decreasing (5.38 average vacancies per academic program in 2001 vs 3.91 in 2003) (13), challenges with staffing of radiologists performing mammogram interpretation were noted in our study, with more notfor-profit facilities reporting having shortages compared with for-profit facilities.
The shortage of certified mammography technologists is a concern because, again, delays in diagnosis could be associated with this shortage. Results of a recent survey by the American Hospital Association (14) showed an 18% job va cancy rate for radiologic technologists in 2001, and 63% of hospitals reported recruitment of technologists to be more difficult than in the previous year. Data from the American Registry of Radiologic Technologists (15) also indicated inadequate mammography service staffing for tracking records from 1996 to 2000 and showed a substantial decline in number of examinees for mammography certification. Our study, which focused on community-based facilities rather than just hospital-based facilities and used more recent data (2001–2002), yields results that are consistent with these reports. Thus, worrisome trends appear to be continuing. Furthermore, our results highlight the challenges of ensuring mammography services in the community: Sites reporting lower technologist FTEs per 1000 mammograms also report having difficulty maintaining MQSA-certified technologists (although this was not statistically significant). This finding suggests that the volume of mammography services at these sites may not be compatible to available technologist FTE.
What might be causing this apparent trend in shortages of radiologic technologists overall and mammography technologists specifically? Many health profession disciplines that employ women, such as nursing, are experiencing dramatic decreases of women entering these fields. Expanded career options for women, especially those that are associated with higher incomes, have been the proposed cause. Another possibility for the shortages of mammography technologists specifically may be MQSA. Perhaps MQSA's strict certification requirements for technologists, many of which are educational, occur on weekends and often are not tied to better pay and therefore have also become a disincentive for radiologic technologists to obtain certification in mammography.
Unlike the results of the majority of published studies, our results represent findings primarily at community-based facilities in three regions: Colorado, New Hampshire, and Washington. The locales of study facilities (rural vs urban) were representative of the general U.S. mammography facilities. Another strength is the timeliness of the data. With the rapidly changing status of mammography practices, these results are more representative of the current capacity for mammography services than are data used from the General Accounting Office report.
Deficiencies in human resources to provide mammography services have important clinical implications. First, as mentioned, early detection of breast cancer could be hampered if the supply of mammography technologists and radiologists cannot meet the demand established by the promotional efforts of the past 25 years and national objectives such as Healthy People 2010 (16). Second, the effect of staffing shortages on the accuracy of mammography screening ought to be more specifically studied. If the need for mammography is increasing and staffing of qualified interpreters is decreasing, more mammograms may be interpreted by an increasingly stressed discipline of mammographic interpreters, which would result in a decline in interpretative acumen.
There are some weaknesses to our study. Results from our study represent self-reported data by lead technologists, radiologists, facility business managers, or project staff at each mammography registry office. Self-reporting may not be as accurate and the variability in respondents may result in a lower level of precision. To minimize these problems, every effort was made to collect data from the most knowledgeable representative at each facility. Therefore, we believe there is only a small chance that our data were affected by these limitations.
In conclusion, while demand and patient expectations for mammography are increasing, the availability of radiologists and certified mammography technologists is decreasing. Waiting times between facility contact and scheduling of mammography examinations are often 1–2 months long, which could delay breast cancer detection. To ensure the continuation of quality mammography services for women in the United States, in addition to recruiting and maintaining qualified technologists, mammography reimbursement, tort reform, and other disincentives for mammography practice must be addressed so that facilities providing these services in the community can remain clinically and financially viable.
Acknowledgments
This work was primarily conducted while S.H.T. was at Group Health Cooperative, although final writing was done while he was at the National Cancer Institute. While NCI funded this work, all opinions are those of the authors and do not imply agreement or endorsement by the federal government or the National Cancer Institute. We also thank the members of our National Advisory Committee.
Abbreviations
- FTE
full-time equivalent
- MQSA
Mammography Quality Standards Act
Footnotes
Authors stated no financial relationship to disclose.
References
- 1.U.S. General Accounting Office . Mammography: capacity generally exists to deliver services. General Accounting Office; Washington, DC: U.S.: 2002. pp. 1–20. [Google Scholar]
- 2.Martinez B. Mammography centers shut down as reimbursement feud rages on. Wall Street Journal. 2000 October 30;:A1. [Google Scholar]
- 3.Gorman C. Need a mammogram? it could take a while. Time. 2001;157:78, 81. [PubMed] [Google Scholar]
- 4.Jones DN. Australian radiology workforce report. Australas Radiol 2002. 2002;46:231–248. doi: 10.1046/j.1440-1673.2002.01051.x. [DOI] [PubMed] [Google Scholar]
- 5.Sibbald B. Staffing crisis looms, radiologists warn. CMAJ. 1999;161:1433. [PMC free article] [PubMed] [Google Scholar]
- 6.Carney PA, Poplack SP, Wells WA, Littenberg B. The New Hampshire Mammography Network: the development and design of a population-based registry. AJR Am J Roentgenol. 1996;167:367–372. doi: 10.2214/ajr.167.2.8686606. [DOI] [PubMed] [Google Scholar]
- 7.Carter AP, Thompson RS, Bourdeau RV, Andenes J, Mustin H, Straley H. A clinically effective breast cancer screening program can be cost-effective, too. Prev Med. 1987;16:19–34. doi: 10.1016/0091-7435(87)90003-x. [DOI] [PubMed] [Google Scholar]
- 8.Taplin SH, Mandelson MT, Anderman C, et al. Mammography diffusion and trends in late-stage breast cancer: evaluating outcomes in a population. Cancer Epidemiol Biomarkers Prev. 1997;6:625–631. [PubMed] [Google Scholar]
- 9.Ballard-Barbash R, Taplin SH, Yankaskas BC, et al. Breast Cancer Surveillance Consortium: a national mammography screening and outcomes database. AJR Am J Roentgenol. 1997;169:1001–1008. doi: 10.2214/ajr.169.4.9308451. [DOI] [PubMed] [Google Scholar]
- 10.Feig SA. Economic challenges in breast imaging. a survivor's guide to success. Radiol Clin North Am. 2000;38:843–852. doi: 10.1016/s0033-8389(05)70204-9. [DOI] [PubMed] [Google Scholar]
- 11.WWAMI Rural Health Research Center [February 11, 2004];The use of RUCAs in health care. Available at: www.fammed.washington.edu/wwamirhrc/. Updated December 2003.
- 12.Bassett LW, Monsees BS, Smith RA, et al. Survey of radiology residents: breast imaging training and attitudes. Radiology. 2003;227:862–869. doi: 10.1148/radiol.2273020046. [DOI] [PubMed] [Google Scholar]
- 13.Sunshine JH, Maynard CD, Paros JT, Forman HP. Update on the diagnostic radiologist shortage. AJR Am J Roentgenol. 2004;182:301–305. doi: 10.2214/ajr.182.2.1820301. [DOI] [PubMed] [Google Scholar]
- 14.American Hospital Association. Work-force survey 2001. American Hospital Association; Washington, DC: 2001. [Google Scholar]
- 15.American Registry of Radiologic Technologists . Annual report of examinations: results of the 2001 examinations in radiology, nuclear medicine technology, and radiation therapy. American Registry of Radiologic Technologists; St Paul, Minn: 2001. pp. 1–11. [Google Scholar]
- 16.U.S. Department of Health and Human Services . Healthy people 2010: understanding and improving health. 2nd ed U.S. Department of Health and Human Services; Washington, DC: 2000. [Google Scholar]