Abstract
DNA from two novel HPV genotypes, HPV-150 and HPV-151, isolated from hair follicles of immuno-competent individuals, was fully cloned, sequenced and characterized. The complete genomes of HPV-150 and HPV-151 are 7,436-bp and 7,386-bp in length, respectively. Both contain genes for at least six proteins, namely E6, E7, E1, E2, L2, L1, as well as a non-coding upstream regulatory region located between the L1 and E6 genes: spanning 416-bp in HPV-150 (genomic positions 7,371 to 350) and 322-bp in HPV-151 (genomic positions 7,213 to 148). HPV-150 and HPV-151 are phylogenetically placed within the Betapapillomavirus genus and are most closely related to HPV-96 and HPV-22, respectively. As in other members of this genus, the intergenic E2-L2 region is very short and does not encode for an E5 gene. Both genotypes contain typical zinc binding domains in their E6 and E7 proteins, but HPV-151 lacks the regular pRb-binding core sequence within its E7 protein. In order to assess the tissue predilection and clinical significance of the novel genotypes, quantitative type-specific real-time PCR assays were developed. The 95% detection limits of the HPV-150 and HPV-151 assays were 7.3 copies/reaction (range 5.6 to 11.4) and 3.4 copies/reaction (range 2.5 to 6.0), respectively. Testing of a representative collection of HPV-associated mucosal and cutaneous benign and malignant neoplasms and hair follicles (total of 540 samples) revealed that HPV-150 and HPV-151 are relatively rare genotypes with a cutaneous tropism. Both genotypes were found in sporadic cases of common warts and SCC and BCC of the skin as single or multiple infections usually with low viral loads. HPV-150 can establish persistent infection of hair follicles in immuno-competent individuals. A partial L1 sequence of a putative novel HPV genotype, related to HPV-150, was identified in a squamous cell carcinoma of the skin obtained from a 64-year old immuno-compromised male patient.
Introduction
Papilomaviruses (PVs) are a diverse family of small viruses with a circular double stranded DNA genome, which are etiologically linked with several skin and mucosal epithelial lesions of animals and humans. They are hierarchically classified into categories designated as genera, species and genotypes [1]. To date, full genomes of more than 200 PV genotypes have been publicly deposited, of which roughly 150 have been detected in humans and are referred to as human PVs or HPVs [1], [2]. Currently, HPVs are classified into five genera: Alpha-, Beta-, Gamma-, Mu- and Nupapillomavirus [1].
According to the 2004 guidelines for PV nomenclature, published by the Study Group of Papillomaviruses of the International Committee on Taxonomy of Viruses (ICTV), in order to be officially recognized as a unique genotype, a candidate PV isolate must differ by at least 10% of its complete gene coding for the major capsid protein (L1 gene) from all other known genotypes, and its complete genome must be sequenced and deposited in the form of clones to the Reference Centre for Papillomaviruses in Heidelberg, Germany [2]. The guidelines issued in 2010 have refrained from strict identity boundaries and have suggested instead the introduction of phylogenetic relationships as a guiding criterion [1]. Traditionally, PV genomic sequences have been obtained directly from epithelial lesions, using cloning methods, which are mainly suitable for characterization of HPV genotypes present in clinical samples in high viral copy numbers [2]. As the field of molecular biology evolved, polymerase chain reaction (PCR), rolling circle amplification, whole genome amplification and, recently, shotgun sequencing have been added to the repertoire of methods used in identification of novel PVs [3], [4]. These technologies have enabled the identification and characterization of many recently identified PVs, especially those present in minute quantities in clinical samples.
Cutaneous HPV genotypes are found within all five PV genera that contain HPVs. They are ubiquitously present in human skin and in the hair follicles of immuno-competent individuals [5]–[7], but can occasionally cause various, predominantly benign skin lesions, including cutaneous warts, e.g. common warts or verrucae vulgaris [8]. In hosts with primary immuno-deficiency or with a genetic predisposition, cutaneous HPVs - especially Betapapillomaviruses - can cause serious clinical manifestations, such as numerous benign and malignant tumors in patients with the hereditary disease epidermodysplasia verruciformis [9]. In immuno-suppressed patients, such as renal transplant recipients, infection with cutaneous HPVs can similarly lead to the development of various benign and malignant skin tumors [10]–[14]. Additionally, several Betapapillomavirus HPVs, such as HPV-22, HPV-38, HPV-92 or HPV-96, have been etiologically linked with the development of squamous cell carcinoma of the skin [15]–[18]. Several cutaneous HPVs have also been linked with actinic keratosis, Bowen's disease and non-melanoma skin cancer in connection with UV-damage in immuno-competent hosts [19], [20].
In the last decade, several studies have shown that HPV DNA can be recovered from healthy skin in humans from very early stages of life [6], [21], that skin infections with multiple HPV genotypes are very common [7], [22], [23] and that several recently identified cutaneous HPVs may not be associated with any clinical manifestations [5], [24]. In view of these facts, the clinical significance of any novel HPV genotype needs to be carefully examined.
In this study, two novel HPV genotypes: HPV-150 and HPV-151, isolated originally from eyebrow hair follicles (isolates SIBX1 and SIBX2, respectively) and initially characterized by our group in 2005 [25], were fully cloned, sequenced and characterized. In addition, two quantitative type-specific real-time PCRs were developed and a representative collection of HPV-associated benign and malignant neoplasms and hair follicles was tested in order to assess the tissue predilection and clinical significance of the novel HPV genotypes.
Materials and Methods
The original isolates of HPV-150 (SIBX1) and HPV-151 (SIBX2) were obtained from eyebrow hair follicles of two immuno-competent males, aged 28 and 25 years, respectively, during our previous study of HPV distribution in eyebrow hair follicles of patients with genital warts [25]. The original SIBX1 positive eyebrow hair follicle sample was used for cloning HPV-150 [25], and a SIBX2 positive sample of scrotal hair, obtained in 2003 from a healthy 23-year-old male individual was used for cloning of HPV-151 [7]. In both cases, DNA was isolated from clinical samples by using a High Pure PCR Template Preparation Kit (Roche Diagnostics GmbH, Mannheim, Germany), according to the manufacturer's instructions.
Whole genome amplification (WGA) of both HPV-150 and HPV-151 was performed prior to PCR amplification, by using an Illustra™ TempliPhi 100 Amplification Kit (GE Healthcare, Amersham, UK), according to the manufacturer's instructions. Following the amplification, the WGA product was diluted 200x fold with PCR-grade H2O.
Amplification, sequencing and cloning of HPV-150
Primers for the reverse long template PCR of HPV-150 were constructed manually on the basis of the previously obtained 373-bp sequence of the HPV-150 L1 gene (GenBank Acc. No AJ606880). A 7,367-bp PCR product of HPV-150 was generated using primer pair X1-longF and X1-longR (Table S1) and the Expand Long Template PCR System (Roche Applied Bioscience, Mannheim, Germany) on a PE9700 Thermo Cycler (Perkin Elmer Applied Biosystems Inc, Foster City, CA).
PCR was carried out in a 25 µl reaction volume containing 5 µl of diluted WGA product, 2.5 µl of 10× Expand Long Template buffer 2 with 27.5 mM MgCl2, 500 µM of dNTPs, 0.75 U of Expand Long Template Enzyme Mix, and 3 pmol of each primer. The thermal cycler program was set to 2 min at 94°C, followed by 40 cycles consisting of 10s at 94°C, 30 s at 53°C, and 8 min at 68°C. The final extension step was performed at 68°C for 10 min and the reaction mixtures were then cooled to 4°C.
Initial sequencing of the 7,367-bp HPV-150 PCR fragment was done by primer walking (primers are listed in Table S1) using the ABI Prism® 310 Genetic Analyzer System (Applied Biosystems), and Big Dye® Terminator 1.1 Cycle Sequencing Kit (Applied Biosystems), according to the manufacturer's instructions.
In order to clone the complete genome of HPV-150, two overlapping blunt-end PCR products of sizes 3,465-bp and 4,375-bp were generated using primer pairs X1F18 and X1R18; and X1F5 and X1R5, respectively (Table S1). Both blunt-end PCR products were generated using KOD Xtreme™ Hot Start DNA Polymerase (Toyobo Novagen, EMD Biosciences Inc., San Diego, CA).
PCR was carried out in a 25 µl reaction volume containing 1 µl of diluted WGA product, 12.5 µl of 2× Xtreme Buffer, 500 µM (each) of dNTPs, 0.02 U of KOD Xtreme™ Hot Start DNA Polymerase, and 0.6 pmol of each primer. The thermal cycler program was set to 2 min at 94°C, followed by 40 cycles consisting of 10 s at 94°C, 30 s at 60°C, and 3 to 6 min at 68°C. Following amplification, the reaction mixtures were cooled to 4°C.
Before cloning, PCR products were excised and purified from 1% agarose gel using a GeneJET™ Gel Extraction Kit (Fermentas, Vilnius, Lithuania). Plasmids containing overlapping PCR products of HPV-150 were prepared using a CloneJET™ PCR Cloning Kit (Fermentas), according to the manufacturer's instructions. A TransformAid™ Bacterial Transformation Kit (Fermentas) was used to transform E.coli strain JM107 with the HPV-150 clones, according to the manufacturer's instructions.
Plasmid clones isolated from the transformed overnight bacterial culture with a GeneJET™ Plasmid Miniprep Kit (Fermentas) were checked for correct HPV inserts by size analysis and sequencing with pJET1.2 sequencing primers, according to the manufacturer's instructions.
Sequencing by primer walking was carried out for both clones, confirming the full genome sequence of HPV-150. The obtained sequences were additionally confirmed by commercial sequencing of the selected clones at Macrogen Inc. (Seoul, Korea) and at Microsynth AG (Balgach, Switzerland).
All primers used in the study were designed manually and checked for Tm and secondary structures using NetPrimer (Premier Biosoft International) and TIB-Molbiol (Berlin, Germany) free web-based software. The ‘Primer Pair Specificity Checking Parameters’ function of Primer-BLAST (NCBI) was used in order to check for the specificity of the primers.
Amplification, sequencing and cloning of HPV-151
In the case of HPV-151, the primers initially constructed on the basis of the previously obtained 367-bp sequence of the HPV-151 L1 gene (GenBank Acc. No AJ606879) failed to amplify the remainder of the genome. In order to solve this problem, additional degenerate primers were designed, based on the genome of HPV-22, the genotype which was most closely related to HPV-151. An initial assessment of the primers was done by short PCR using the DreamTaq™ Green PCR Master Mix (2X) (Fermentas UAB - Thermo Fisher Scientific, Vilnius, Lithuania), following the manufacturer's instructions. The amplified DNA was examined by gel electrophoresis and several degenerate primer pairs produced PCR products of the expected size, ranging from 100 to 1,328-bp. Following sequencing of these short amplicons, several additional primers, specific for the novel genotype HPV-151, were designed (Table S1). Finally, a 6,256-bp fragment of the HPV-151 genome was amplified using the primer pair X2-L1For and X2-longR2, designed on the basis of the sequence obtained using degenerate primer pair HPV22-L1f1mix and HPV22-L1-r1mix (Table S1), and the Expand Long Template PCR System on a PE9700 Thermo Cycler.
PCR was carried out in a 25 µl reaction volume containing 1 µl of diluted WGA product, 2.5 µl of 10× Expand Long Template buffer 2 with 27.5 mM MgCl2, 500 µM of dNTPs, 0.75 U of Expand Long Template Enzyme Mix and 3 pmol of each primer. The thermal cycler program was set to 2 min at 94°C, followed by 40 cycles consisting of 10 s at 94°C, 30 s at 55°C, and 7 min at 68°C. The final extension step was performed at 68°C for 7 min and the reaction mixtures were then cooled to 4°C.
Initial sequencing of the 6,256-bp HPV-151 PCR fragment was done by primer walking with the primers listed in Table S1.
For cloning HPV-151, two overlapping blunt-end PCR products of sizes 2,785-bp and 5,481-bp were generated using primer pairs X2F17 and X2R17; and X2F3 and X2R3, respectively (Table S1) by using KOD Xtreme™ Hot Start DNA Polymerase (Toyobo Novagen, EMD Biosciences Inc.).
PCR conditions and the entire further cloning and sequencing procedure for HPV-151 were the same as described above for HPV-150.
ORF and phylogenetic analysis
All partial sequences obtained for HPV-150 and HPV-151 were assembled using ContigExpress of Vector NTI Advance™ v11.0 (Invitrogen, Carlsbad, CA). The open reading frames (ORFs) of HPV-150 and HPV-151 were determined using the ORF finder function of Vector NTI Advance™ v11.0 and were additionally confirmed by genome organization analysis and comparison with closely related HPV genotypes using the BioEdit Sequence Alignment Editor [26].
The phylogenetic relationships of HPV-150 and HPV-151 within the PV family were determined based on the L1 gene. Briefly, L1 nucleic acid sequences were converted to protein sequences and aligned using MAFFT v6.832b (http://mafft.cbrc.jp/alignment/software) [27], reverse translated using Pal2Nal (http://www.bork.embl.de/pal2nal/) [28] and filtered using Gblocks (http://molevol.cmima.csic.es/castresana/Gblocks.html) [29], [30]. Maximum likelihood phylogenetic inference was conducted using RAxML version v7.2.8 [31]–[33] alpha (PTHREADS version) on an 2x CPU 6 core AMD Opteron 2431 with 12 GB RAM DDR2-800 (kindly provided free of charge by ABAKUS plus, Kranj, Slovenia). A generalized time-reversible (GTR) model with four gamma discrete rate categories and three partitions, one per codon position, was used for the analysis. One thousand bootstrap replicates were generated to determine node support for the best tree.
HPV-150 and HPV-151 type specific real-time PCRs
Primers and a probe specific for HPV-150 were chosen within the L1 gene by using the on-line ProbeFinder software (Roche Applied Science), resulting in a PCR product of 60-bp in length. Primers RT-150-F (5′- AGGCCTTACCTTGTGCTGAA -3′, HPV-150 nucleotide positions 6,355 to 6,374) and RT-150-F (5′- TTAATTCTAAAGGAGGACATGAACC -3′, HPV-150 nucleotide positions 6,390 to 6,414), together with FAM-labeled Universal Probe #50 (Roche Applied Science) were used for HPV-150 specific real-time PCR.
Primers and a probe specific for HPV-151 were chosen within the L1 gene by using the on-line ProbeFinder software (Roche Applied Science), resulting in a PCR product of 60-bp in length. FAM-labeled Universal Probe #127 (Roche Applied Science) was used together with primers RT-151-F (5′- ATCAGCAACAGATGGAGCAA -3′, HPV-151 nucleotide positions 5,838 to 5,857) and RT-151-R (5′- GCTCTATACTGGTTCCCTGACAC -3′, HPV-151 nucleotide positions 5,875 to 5,897) for HPV-151 specific real-time PCR.
The plasmid reference clones of HPV-150 and HPV-151, containing the L1 sequence, were used to optimize the real-time PCR conditions. Plasmid DNA concentration was quantified using a NanoDrop ND-1000 spectrophotometer (Nanodrop Technologies, Oxfordshire, UK) and the number of plasmid copies/µl was calculated using the equation of Whelan et al. [34].
The optimized real-time PCR reaction mixture for both type-specific real-time PCRs contained 10 µl of LightCycler® Probes Master 2x conc. (Roche Applied Science), 0.2 µM of each primer, 0.05 µM of Universal Probe #50 or #127 (Roche Applied Science), 1U of LightCycler® Uracil-N-Glycosylase (Roche Applied Science), sample DNA and water up to a final volume of 20 µl. The assays were performed on a LightCycler® 480 (Roche) under the following conditions: Uracil-N-Glycosylase activation at 40°C and pre-incubation at 95°C for 10 min each, followed by 45 cycles of 95°C for 10 s (denaturation) and 59°C for 30 s (annealing) and 72°C for 1 s (extension). Acquisition of the fluorescence signal was performed in single mode during the annealing step of each cycle. The final cooling step consisted of a 10 s hold at 40°C. The conditions of the real-time PCR for HPV-150 and HPV-151 were intentionally identical, since this allowed simultaneous testing of samples on the LightCycler® 480 (Roche).
To evaluate the linearity of the assays, triplicate ten-fold serial dilutions of the reference plasmids of HPV-150 and HPV-151 were prepared in 1.5 ml DNA LoBind tubes (Eppendorf, Hamburg, Germany) using a water solution with carrier RNA (1 µg/ml). The limits of detection of the assays were determined by testing 15 replicates of the reference plasmid dilutions corresponding to an input of 25, 13, 6, 3, 1.5, 0.8 and 0.4 copies per reaction.
The specificity and cross-reactivity of the assays were tested using 107 to 108 copies of synthetic partial L1 sequences (inserted into plasmid pUC57, by Genscript, Piscataway, USA) of the following Betapapillomaviruses: HPV-9, HPV-15, HPV-17, HPV-22, HPV-23, HPV-37, HPV-38, HPV-80, HPV-100, HPV-111, HPV-113, HPV-120, HPV-122, HPV-92 and HPV-96.
Clinical samples
The tissue predilection and clinical significance of HPV-150 and HPV-151 were assessed on a representative collection of HPV-associated benign and malignant neoplasms and hair follicles. The DNA was isolated from a total of 540 samples obtained from the same number of patients, including tissue samples of histologically confirmed genital warts (71), laryngeal papillomas (78), cervical squamous cell carcinomas (100), common warts (101), squamous cell carcinoma (SCC) of the skin (52), basal cell carcinoma (BCC) of the skin (49) and hair follicles (89), as described previously [7], [25], [35]-[38]. The quality of isolated DNA and absence of PCR inhibitors were checked by amplification of a 110-bp fragment of human beta-globin, as described previously [36]. The number of human cells per µl of clinical sample in samples positive for HPV-150 or HPV-151 was calculated from the beta-globin concentration, as described previously [17], and used to determine the ratio between the number of viral genomes and human cells. All positive results of the HPV-150 and HPV-151 real-time PCRs were confirmed by sequencing.
The presence of additional HPV genotypes in HPV-150 and/or HPV-151 positive samples was determined using two commercial line-probe assays: INNO-LiPA HPV Genotyping Extra (Innogenetics, Gent, Belgium), which allows identification of 28 different Alphapapillomavirus genotypes; RHA skin (beta) HPV (Diassay B.V., Rijswijk, The Netherlands), which allows identification of 26 different Betapapillomavirus genotypes, and additionally by consensus GP5+/6+ in-house PCR and sequencing of PCR products [39].
Ethics Statement
None of the 540 clinical samples tested were collected solely for the purpose of this study. All samples included in the study were collected in compliance with the Helsinki Declaration. Samples of cervical cancer, hair follicles, genital warts and common warts were collected prospectively in our previous studies. These studies were approved by the Ethics Committee of the Ministry of Health of the Republic of Slovenia (consent references 34/11/06, 83/11/09, 174/05/09, 97/11/09 and 100/12/09) and written informed consent was obtained from each patient. Samples of laryngeal papillomas, squamous cell carcinoma and basal cell carcinoma of the skin were retrieved from the tissue collection of paraffin-embedded samples of the Institute of Pathology, Faculty of Medicine, University of Ljubljana. Approval from the Institutional Review Board of the Institute of Pathology, Faculty of Medicine, University of Ljubljana was obtained prior to starting work on samples included in this study. In accordance with the national legislation of the Republic of Slovenia, no informed consent is needed for research on archival clinical samples. In order to protect the identity of the patient, all archival clinical samples used in the study were coded and tested anonymously. The only available data were patient gender, age and immune status (if collected during the original study).
Results and Discussion
Partial L1 sequences of HPV-150 (SIBX1; 373-bp) and HPV-151 (SIBX2, 367-bp) were deposited in GenBank in March 2005 under Acc. Nos. AJ606880 and AJ606879, respectively. The four reference clones, covering the full genomes of HPV-150 and HPV-151, were deposited in March 2010 in the Reference Centre for Papillomaviruses, Heidelberg, Germany, where their sequences were independently confirmed and the two genotypes were officially named in April 2010.
The genome of HPV-150 has a total length of 7,436-bp, with a GC ratio of 39.70%, and is deposited in GenBank under Acc. No. FN677755. The genome of HPV-151 has a total length of 7,386-bp, with a GC ratio of 39.79%, and is deposited in GenBank under Acc. No. FN677756.
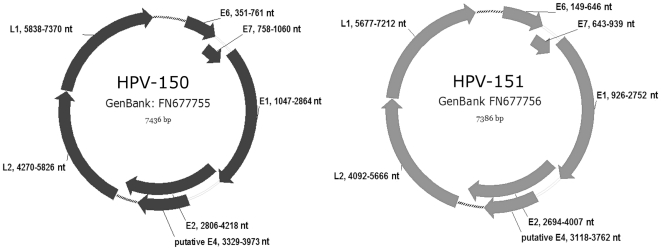
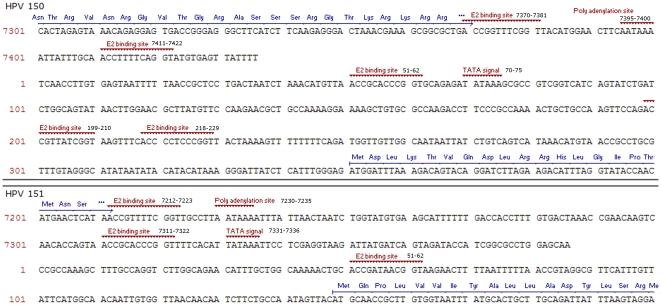
ORF analysis and sequence alignment comparisons showed both HPV-150 and HPV-151 to have the typical genomic organization of HPVs and to contain at least six viral genes: E6, E7, E1, E2, L2 and L1, as well as possibly a gene for the E4 protein (Figure 1). In addition to the mentioned ORFs, the genomes of both new genotypes contain a non-coding upstream regulatory region (URR) or long control region (LCR) located between the L1 and E6 genes, spanning 416-bp in HPV-150 (genomic positions 7,371 to 350) and 322-bp in HPV-151 (genomic positions 7,213 to 148) (Figure 2). The LCRs of both HPV-150 and HPV-151 lack the conserved M29 and M33 motifs [40] which are typical for members of Betapapillomavirus species 1 [41] but are absent in other Betapapillomavirus species [42]. As in other members of Betapapillomaviruses, the intergenic region located between E2 and L2 genes is very short (51-bp in HPV-150 (genomic positions 4,219 to 4,269) and 84-bp in HPV-151 (genomic positions 4,008 to 4,091)) and does not encode for an E5 gene.
Figure 1. Genomic organization of HPV-150 and HPV-151 showing genomic positions of viral genes E6, E7, E1, E2, L1, L2, and the non-coding regions located between L1 and E6 (LCR); and E2 and L2 (dotted line).
Figure 2. Characteristic features of the long control region (LCR) of HPV-150 and HPV-151, showing genomic locations of E2 binding sites (ACC-N5-7-GGT), polyadenilation sites (AATAAA), and TATA signals (TATAAA or TATA(A/T)A(A/T).
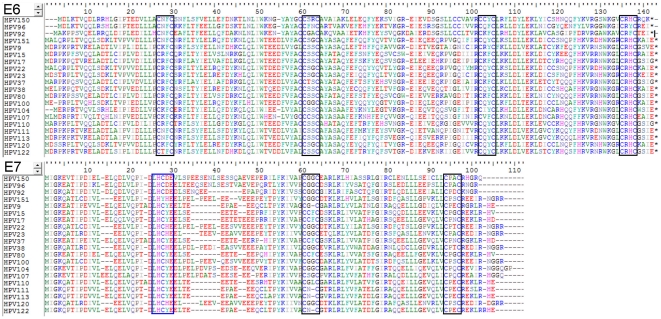
HPV-150 and HPV-151 contain two regular zinc binding domains (CxxC(x)29CxxC) within their E6 protein, at amino-acid positions 24 and 98; and 27 and 101, respectively (Figure 3). Both genotypes also contain one regular zinc binding domain (CxxC(x)29CxxC) within their E7 protein, at amino-acid positions 50 and 53, respectively. However only HPV-150 also contains the regular pRb-binding core sequence (LxCxE) at amino-acid position 24 of E7 (Figure 3). Unlike other members of Betapapillomavirus species 2, HPV-151 does not contain the regular pRb-binding core sequence (LxCxE) within its E7 protein (Figure 3).
Figure 3. Amino acid alignment of HPV-150 and HPV-151 E6 and E7 proteins with corresponding proteins of closely related genotypes from Betapapillomavirus species 2, 4 and 5.
The locations of zinc-binding domains (CxxC(x)29CxxC) are indicated by black boxes, and the location of the pRb-binding core sequence (LxCxE) is indicated with a blue box.
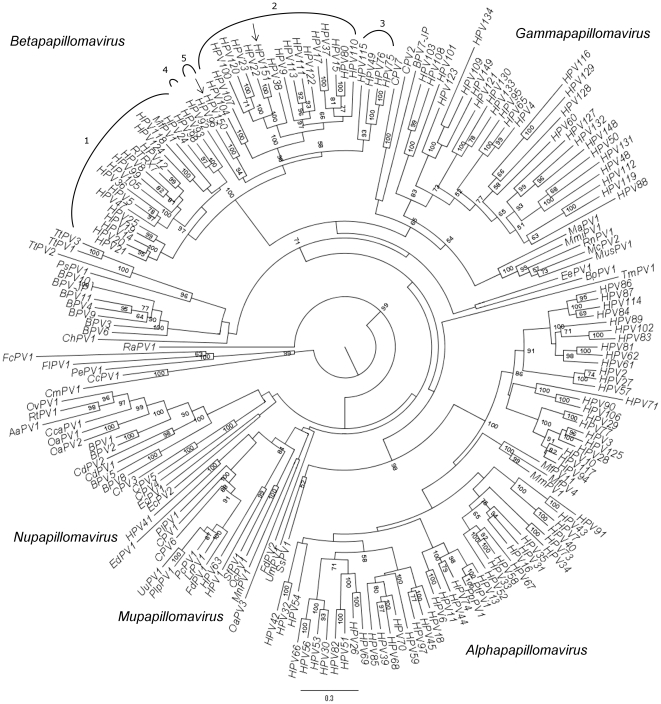
Phylogenetic analyses using the L1 gene sequences of a representative selection of 200 PVs place both HPV-150 and HPV-151 within the Betapapillomavirus genus (Figure 4). As shown in Figure 4, the closest relative of HPV-150 is HPV-96 (79.59% nucleotide (nt) identity in the L1 gene; distance in substitutions per site for L1; 0.264440 and 0.103792 for nt and for amino-acid (aa), respectively). HPV-96 belongs to Betapapillomavirus species 5 and was originally isolated from a SCC of the skin [18]. The next phylogenetically closest genotype to HPV-150 and HPV-96 is HPV-92, which belongs to Betapapillomavirus species 4, and was originally isolated from a BCC of the skin [16]. Since these three genotypes seem to have evolved through intra-host duplication [43] and two of them show at least some carcinogenic potential, the ancestral genotype from which these genotypes were derived may have itself been an oncogenic HPV genotype.
Figure 4. A consensus phylogenetic tree of 200 PV based on nucleotide sequences of the L1 gene.
Numbers at nodes show maximum likelihood bootstrap support (%) above 50. Betapapillomavirus species numbers are indicated above the corresponding genotypes.
As shown in Figure 4, HPV-151 appears to be phylogenetically nested within Betapapillomavirus species 2, with HPV-22 being its closest relative (86.98% nt identity for the L1 gene; 0.164208 and 0.084639 distance in substitutions per site for L1 nt and aa, respectively). HPV-22 was originally isolated from chest macules [15]. Currently, Betapapillomavirus species 2 encompasses 17 HPV genotypes isolated from humans, making it one of the largest species among PVs. The generation of such viral diversity has probably occurred through intra-host duplication events, which may reflect multiple ways of succeeding in adaptation to the human host [43]. An example of this capacity to establish infection in multiple ways can be seen from the fact that particular genotypes of Betapapillomavirus species 2 have been found in lesions ranging from macules and other benign skin lesions, to actinic keratosis, BCC and SCC of the skin, and even head and neck and esophageal carcinoma, as in the case of HPV-100 [44].
In order to assess the biological and clinical importance of the novel HPV genotypes, two quantitative HPV-150 and HPV-151 type-specific PCR assays were developed. The standard curves of both assays showed an excellent correlation coefficient (R2 = 1.00) between the Ct (threshold) and the log of starting viral copy number across at least seven orders of magnitude. The 95% limits of detection determined by Probit analysis using the PASW Statistics 18 program (SPSS GmbH Software, Munich, Germany) were 7.3 copies/reaction (range 5.6 to 11.4) and 3.4 copies/reaction (range 2.5 to 6.0), for the HPV-150 and HPV-151 assays, respectively. For HPV-150 assay, the intra- and inter-assay coefficient of variation (CV (%) = (st.dev/mean Ct)×100) were 0.55 and 1.43 for 100 copies per reaction, respectively, and 1.73 and 1.81 for 10 copies per reaction, respectively, and corresponding values for HPV-151 assay were 0.81 and 1.54 for 100 copies per reaction, respectively, and 1.02 and 1.98 for 10 copies per reaction, respectively. Both assays showed no cross-reactivity with any of the tested non-targeted HPV genotypes.
Using the developed type-specific PCRs, a representative collection of HPV-associated benign and malignant neoplasms and hair follicles was tested for the presence of HPV-150 and HPV-151. The sample collection was chosen to represent various sites of HPV infection (mucosal/cutaneous) and possible outcomes of HPV infection (benign/malignant lesions)(Table 1). The panel of samples thus included the most important HPV-associated malignant neoplasms of mucosal (cervical squamous cell carcinoma) and cutaneous (SCC and BCC of skin) origin, and the most important HPV-associated benign neoplasms of mucosal (genital warts, laryngeal papillomas) and cutaneous (common warts) origin. In addition, we tested hair follicles, which are commonly used as the best approximate to skin biopsies, to examine the prevalence of Betapapillomaviruses in healthy skin [45], [46] and are known to be a main reservoir of commensal HPV genotypes in immuno-competent individuals [5]–[7].
Table 1. Clinical samples tested for the presence of HPV-150 and HPV-151.
| Tissue type | Sample type | No. of samples tested | No. (%) of HPV-150 positive samples | No. (%) of HPV-151 positive samples |
| Mucosal | ||||
| Genital warts | 71 | 0 | 0 | |
| Laryngeal papillomas | 78 | 0 | 0 | |
| Cervical cancer | 100 | 0 | 0 | |
| Cutaneous | ||||
| Common warts | 101 | 4 (4.0) | 4 (4.0) | |
| Squamous cell carcinoma of the skin | 52 | 3 (5.8) | 1 (1.9) | |
| Basal cell carcinoma of the skin | 49 | 1 (2.0) | 3 (6.1) | |
| Hair follicles | ||||
| 89 | 3 (3.4) | 2 (2.2) | ||
| Total | 540 | 11 (2.0) | 10 (1.9) | |
As shown in Table 1, none of the 249 mucosal tissue samples tested were positive for HPV-150 and HPV-151, indicating little, if any, mucosal tropism of both novel HPV genotypes.
Of the 101 samples of common warts tested, four samples (4.0%) contained HPV-150, indicating the cutaneous tropism of this genotype (Table 1). Of HPV-150 positive common warts, three samples contained at least one additional HPV genotype (samples 1, 2 and 4, Table 2): HPV-27 from Alphapapillomavirus species 4, a well known genotype capable of causing common warts; HPV-5 and HPV-14, cutaneotropic members of Betapapillomavirus species 1; and HPV-15 belonging to Betapapillomavirus species 2 – all three later being genotypes associated with the development of cutaneous tumors in immuno-suppressed patients or patients with epidermodysplasia verruciformis. Due to the presence of more than one HPV genotype in these lesions, the development of common warts could not be conclusively attributed to HPV-150. In contrast, in the fourth HPV-150 positive common wart (sample 3, Table 2), HPV-150 was the only HPV genotype detected, despite the use of several HPV genotyping assays, targeting a range of Alphapapillomavirus and Betapapillomavirus genotypes, indicating a possible causative role of HPV-150 in the development of this particular common wart. Although the HPV-150 viral load was relatively low (1/31 viral genomes/No. human cells) our finding is in agreement with recent studies which showed that viral load of Betapapillomaviruses associated with cutaneous warts is substantially lower than that of Alphapapillomaviruses (HPV-3, HPV-27, HPV-57) associated with similar lesions (1/2 to 1/10 000 viral genomes/No. human cells) [47]. However, further research is needed in order to reach any final conclusions on the ability of HPV-150 to cause common warts in absence of other factors.
Table 2. Characteristics of HPV-150 positive samples and patients.
| Sample type | Sample ID | Histology result | Age | Gender | Viral genomes/No. of human cells | Presence of other HPV genotypes |
| cutaneous | 1 | Common wart | 15 | Male | 1/15 | HPV-27 |
| cutaneous | 2 | Common wart | 81 | Female | 1/212 | HPV-5, HPV-14, HPV-15 |
| cutaneous | 3 | Common wart | 90 | Male | 1/31 | None |
| cutaneous | 4 | Common wart | 16 | Male | 1/12 | HPV-5 |
| cutaneous | 5 | Squamous cell carcinoma of the skin | 82 | Male | 1/57950 | None |
| cutaneous | 6 | Squamous cell carcinoma of the skin | 80 | Male | 1/9508 | HPV-151, HPV-37 |
| cutaneous | 7 | Squamous cell carcinoma of the skin | 86 | Male | 1/140 | HPV-8, HPV-75 |
| cutaneous | 8 | Basal cell carcinoma of the skin | 81 | Female | 1/22638 | HPV-151 |
| hair follicle | 9 | / | 29 | Male | Nd | HPV-6, HPV-8, HPV-9, HPV-17, HPV-21 |
| hair follicle | 10 | / | 27 | Male | Nd | None |
| hair follicle | 11 | / | 52 | Female | Nd | HPV-8, HPV-14, HPV-38, HPV-93 |
Nd – Not determined.
As shown in Table 1, HPV-150 was detected in four (4.0%) of the 101 samples of malignant skin tumors tested, further supporting cutaneous tropism of HPV-150. Similarly to the common warts, several additional cutaneous genotypes from Betapapillomavirus genus were present in three out of four HPV-150 positive samples of malignant skin tumors included in the study (samples 6–8, Table 2), greatly complicating the interpretation of our findings. The interpretation of our results is additionally complicated by the difference in viral loads observed between an abortive HPV infection leading to malignant transformation of the skin, which typically involves Betapapillomavirus genotypes present in minute quantities [13], [18], [48]–[50] and on the other side the productive HPV infection of the skin resulting in benign tumors, such as common warts, which usually harbor viruses in higher concentration [47]. Such differences make it near impossible to distinguish causative or ‘driver’ HPV genotypes from commensal or ‘passenger’ HPV genotypes, also present on the lesion and/or the surrounding skin [48]. Thus, although the HPV-150 was the only HPV genotype detected in a single case of SCC of the skin (sample 5, Table 2), due to its presence in very low quantity (1/57,950 viral genomes/No. human cells), further studies are needed in order to establish if HPV-150 is a causative or commensal genotype in sporadic cases of the SCC of the skin.
As shown in Table 1, HPV-150 was also found in three (3.4%) out of 89 hair follicle samples tested (Table 1), finally confirming cutaneous tropism of HPV-150.
Long term persistent HPV infection is a key requirement for the development of HPV-related anogenital cancers, but its role is less clear in the case of HPV-related skin cancer [13], [20], [48]-[50]. In order to determine whether HPV-150 can establish persistent infection, seven hair follicle samples collected over the course of one year from one of the HPV-150 positive individuals were tested using HPV-150 type-specific PCR. In this immuno-competent 22-year-old male, HPV-150 was detected in all seven hair follicles tested, confirming its potential for persistent infection. However, similarly to the majority of other Betapapillomavirus infections in immuno-competent individuals [22]-[24], no obvious epithelial lesions were recorded as a result of the persistence of HPV-150 in our patient during 12 months of follow-up.
Of the 101 samples of common warts tested, four samples (4.0%) contained HPV-151, indicating its cutaneous tropism (Table 1). Of HPV-151 positive common warts, two samples contained at least one additional Betapapillomavirus genotype (samples 12 and 14, Table 3): HPV-9, the type species of Betapapillomavirus species 2; HPV-19, HPV-36 and HPV-93 of Betapapillomavirus species 1; and HPV-49 of Betapapillomavirus species 3. Since all listed genotypes have cutaneous tropism and are etiologically associated with the development of cutaneous tumors in immuno-suppressed patients or patients with epidermodysplasia verruciformis, these two common warts could not conclusively be attributed etiologically to HPV-151. In contrast, two HPV-151 positive common wart samples (samples 13 and 15, Table 3) did not contain any additional HPV genotypes, indicating a possible causative role of HPV-151 in the development of these two common warts. Both samples had viral loads (1/493 and 1/103 viral genomes/No. human cells, respectively) of magnitude characteristic for Betapapillomavirus genotypes in common warts [47], however the final contribution of HPV-151 to the development of these lesions requires further studies.
Table 3. Characteristics of HPV-151 positive samples and patients.
| Sample type | Sample ID | Histology result | Age | Gender | Viral genomes/No. of human cells | Presence of other HPV genotypes |
| cutaneous | 12 | Common wart | 67 | Male | 1/19 | HPV-9, HPV-93 |
| cutaneous | 13 | Common wart | 76 | Male | 1/439 | None |
| cutaneous | 14 | Common wart | 55 | Female | 1/168 | HPV-19, HPV-36, HPV-49 |
| cutaneous | 15 | Common wart | 74 | Female | 1/103 | None |
| cutaneous | 6 | Squamous cell carcinoma of the skin | 80 | Male | 1/1994 | HPV-150, HPV-37 |
| cutaneous | 16 | Basal cell carcinoma of the skin | 84 | Female | 1/691 | None |
| cutaneous | 17 | Basal cell carcinoma of the skin | 84 | Female | 1/39 | HPV-21, HPV-36, HPV-24 |
| cutaneous | 8 | Basal cell carcinoma of the skin | 81 | Female | 1/113 | HPV-150 |
| hair follicle | 18 | / | 26 | Male | Nd | HPV-5, HPV-19, HPV-21, HPV-22, HPV-24, HPV-38, HPV-93 |
| hair follicle | 19 | / | 33 | Male | Nd | HPV-23, HPV-93 |
Nd – Not determined.
As shown in Tables 1 and 3, HPV-151 was detected in four (4.0%) of the 101 malignant skin tumor samples and in three (3.4%) of 89 hair follicle samples tested, finally confirming the cutaneous tropism of this novel HPV genotype. In the majority of the HPV-151 positive samples, several other HPV genotypes were identified (Table 3).
In the single HPV-151 positive BCC, where no other HPV genotypes were present (sample 16, Table 3), the viral load was relatively low (1/691 viral genomes/No. of human cells). Such minute viral load is consistent with values described previously for other Betapapillomaviruses in non-melanoma skin cancer [18], [48], [49], and given the advanced age of the patient (84 years) it is possible that HPV-151 contributed at least partially to the development of the BCC in question. However, further studies are required in order to finally establish the causative role of HPV-151 in the development of BCC of the skin.
Interestingly, one sample of BCC of the skin (sample 8, Tables 2 and 3) contained both novel HPV genotypes: HPV-150 and HPV-151, but not other HPV genotypes. Similarly, one sample of SCC of the skin (sample 6, Tables 2 and 3) contained both HPV-150 and HPV-151 in addition to HPV-37. In both skin cancers, the viral loads per number of human cells were substantially higher for HPV-151 than for HPV-150, but the significance (if any) of these findings remains to be determined.
In addition to full characterization of two novel HPV genotypes, a putative novel HPV genotype, phylogenetically related to HPV-150, was identified in a tissue sample of SCC of the skin obtained from a 64-year old male immuno-compromised patient, together with HPV-9, the type species genotype of Betapapillomavirus species 2. The 354-bp sequence of L1 gene of this putative novel HPV genotype (isolate SI-HPV-Beta5; GenBank Acc. No. FR822732) showed 90.68% nt identity with the corresponding part of the L1 sequence of HPV-150 but its other characteristics remain to be determined in future studies.
Conclusions
The cloning and full characterization of two novel Betapapillomaviruses HPV-150 and HPV-151, as well as the partial identification of a putative novel HPV genotype closely related to HPV-150 (isolate SI-HPV-Beta5), improves our knowledge of the diversity of Betapapillomaviruses infecting humans. HPV-150 and HPV-151 belong phylogenetically within the Betapapillomavirus genus and are most closely related to HPV-96 and HPV-22, respectively. Both novel genotypes are relatively rare, most likely lack mucosal tropism and have clear cutaneous tropism. HPV-150 can establish persistent infection of hair follicles in immuno-competent individuals. HPV-150 and HPV-151 have been found in sporadic cases of common warts, SCC and BCC of the skin preferably in elderly immuno-competent individuals, as both single and multiple infections with viral loads ranging from 1/12 to 1/57,950 viral genomes/No. of human cells.
Supporting Information
Primers used for initial amplification, primer walking and preparation of HPV-150 and HPV-151 reference clones. Nt – Nucleotide position. N – Random nucleotide. Cw – Clock-wise. Ccw – Counter clock-wise.
(DOC)
Acknowledgments
Both viruses were isolated from hair follicles collected by Assistant Professor Marko Potočnik, Department of Dermatovenereology, University Medical Center, Ljubljana. We are grateful to Ethel-Michelle de Villiers for confirmatory analysis of the clones at the Reference Centre for Papillomaviruses, Heidelberg, Germany. We thank Branko Pirš, MD, Department of Dermatovenereology, University Medical Center, Ljubljana, for providing the tissue sample in which SI-HPV-Beta5 putative novel HPV was first identified. We would also like to thank Marko Potočnik, Branko Pirš, Nina Jančar, Eda Vrtačnik Bokal, Pavle Košorok and Vesna Tlaker Žunter for the collection of clinical samples, Nina Gale for the histological assessment, and Kristina Fujs-Komloš, Mateja Jelen and Robert Krošelj for excellent laboratory support. We are much indebted to Sergej Rožman for allowing us to use their computing facilities for phylogenetic analyses, and Miha Starič for assistance with remote access and data transfer.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: A.K. is funded by the Young Researcher Training Program of the Slovenian Research Agency and the Ministry of Health and B.J.K. is funded through grant Z3-0220-0381-08. I.G.B. is funded by the Spanish MICINN (Ramón y Cajal Program, and CGL2010-16713). No additional external funding was received for this study. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
References
- 1.Bernard H-U, Burk RD, Chen Z, van Doorslaer K, zur Hausen H, et al. Classification of papillomaviruses (PVs) based on 189 PV types and proposal of taxonomic amendments. Virology. 2010;401:70–79. doi: 10.1016/j.virol.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Villiers E-M, Fauquet C, Broker TR, Bernard H-U, zur Hausen H. Classification of papillomaviruses. Virology. 2004;324:17–27. doi: 10.1016/j.virol.2004.03.033. [DOI] [PubMed] [Google Scholar]
- 3.Rector A, Tachezy R, Van Ranst M. A sequence-independent strategy for detection and cloning of circular DNA virus genomes by using multiply primed rolling-circle amplification. J Virol. 2004;78:4993–4998. doi: 10.1128/JVI.78.10.4993-4998.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li L, Barry P, Yeh E, Glaser C, Schnurr D, et al. Identification of a novel human gammapapillomavirus species. J Gen Virol. 2009;90:2413–2417. doi: 10.1099/vir.0.012344-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Antonsson A, Forslund O, Ekberg H, Sterner G, Hansson BG. The ubiquity and impressive genomic diversity of human skin papillomaviruses suggest a commensalic nature of these viruses. J Virol. 2000;74:11636–11641. doi: 10.1128/jvi.74.24.11636-11641.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Antonsson A, Karanfilovska S, Lindqvist PG, Hansson BG. General acquisition of human papillomavirus infections of skin occurs in early infancy. J Clin Microbiol. 2003;41:2509–2514. doi: 10.1128/JCM.41.6.2509-2514.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Potočnik M, Kocjan BJ, Seme K, Luzar B, Babič DZ, et al. Beta-papillomaviruses in anogenital hairs plucked from healthy individuals. J Med Virol. 2006;78:1673–1678. doi: 10.1002/jmv.20753. [DOI] [PubMed] [Google Scholar]
- 8.Jabłońska S, Majewski S, Obalek S, Orth G. Cutaneous warts. Clin Dermatol. 1997;15:309–319. doi: 10.1016/s0738-081x(96)00170-8. [DOI] [PubMed] [Google Scholar]
- 9.Jablonska S, Majewski S. Epidermodysplasia verruciformis: immunological and clinical aspects. Curr Top Microbiol Immunol. 1994;186:157–175. doi: 10.1007/978-3-642-78487-3_9. [DOI] [PubMed] [Google Scholar]
- 10.Shamanin V, Glover M, Rausch C, Proby C, Leigh IM, et al. Specific types of human papillomavirus found in benign proliferations and carcinomas of the skin in immunosuppressed patients. Cancer Res. 1994;54:4610–4613. [PubMed] [Google Scholar]
- 11.de Jong-Tieben LM, Berkhout RJ, Smits HL, Bouwes Bavinck JN, Vermeer BJ, et al. High frequency of detection of epidermodysplasia verruciformis-associated human papillomavirus DNA in biopsies from malignant and premalignant skin lesions from renal transplant recipients. J Invest Dermatol. 1995;105:367–371. doi: 10.1111/1523-1747.ep12320803. [DOI] [PubMed] [Google Scholar]
- 12.de Villiers EM, Lavergne D, McLaren K, Benton EC. Prevailing papillomavirus types in non-melanoma carcinomas of the skin in renal allograft recipients. Int J Cancer. 1997;73:356–361. doi: 10.1002/(sici)1097-0215(19971104)73:3<356::aid-ijc9>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 13.Berkhout RJM, Bouwes Bavinck JN, ter Schegget J. Persistence of human papillomavirus DNA in benign and (pre)malignant skin lesions from renal transplant recipients. J Clin Microbiol. 2000;38:2087–2096. doi: 10.1128/jcm.38.6.2087-2096.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karagas MR, Nelson HH, Sehr P, Waterboer T, Stukel TA, et al. Human papillomavirus infection and incidence of squamous cell and basal cell carcinomas of the skin. J Natl Cancer Inst. 2006;98:389–395. doi: 10.1093/jnci/djj092. [DOI] [PubMed] [Google Scholar]
- 15.Kremsdorf D, Favre M, Jablonska S, Obalek S, Rueda LA, et al. Molecular cloning and characterization of the genomes of nine newly recognized human papillomavirus types associated with epidermodysplasia verruciformis. J Virol. 1984;52:1013–1018. doi: 10.1128/jvi.52.3.1013-1018.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Forslund O, Antonsson A, Higgins G, Ly H, Delius H, et al. Nucleotide sequence and phylogenetic classification of candidate human papilloma virus type 92. Virology. 2003;312:255–260. doi: 10.1016/s0042-6822(03)00391-x. [DOI] [PubMed] [Google Scholar]
- 17.Hazard K, Eliasson L, Dillner J, Forslund O. Subtype HPV38b[FA125] demonstrates heterogeneity of human papillomavirus type 38. Int J Cancer. 2006;119:1073–1077. doi: 10.1002/ijc.21920. [DOI] [PubMed] [Google Scholar]
- 18.Vasiljević N, Hazard K, Eliasson L, Ly H, Hunziker A, et al. Characterization of two novel cutaneous human papillomaviruses, HPV93 and HPV96. J Gen Virol. 2007;88:1479–1483. doi: 10.1099/vir.0.82679-0. [DOI] [PubMed] [Google Scholar]
- 19.Nindl I, Gottschling M, Stockfleth E. Human papillomaviruses and non-melanoma skin cancer: basic virology and clinical manifestations. Dis Markers. 2007;23:247–259. doi: 10.1155/2007/942650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boukamp P. Non-melanoma skin cancer: what drives tumor development and progression? Carcinogenesis. 2005;26:1657–1667. doi: 10.1093/carcin/bgi123. [DOI] [PubMed] [Google Scholar]
- 21.Castellsague X, Drudis T, Canadas M, Gonce A, Ros R, et al. Human papillomavirus (HPV) infection in pregnant women and mother-to-child transmission of genital HPV genotypes: a prospective study in Spain. BMC Infectious Diseases. 2009;9:74. doi: 10.1186/1471-2334-9-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hazard K, Karlsson A, Andersson K, Ekberg H, Dillner J, et al. Cutaneous human papillomaviruses persist on healthy skin. J Invest Dermatol. 2007;127:116–119. doi: 10.1038/sj.jid.5700570. [DOI] [PubMed] [Google Scholar]
- 23.Plasmeijer EI, Green AC, de Koning MNC, O'Rourke P, Quint WGV, et al. Transmission of betapapillomaviruses between domestic partners in an Australian community. J Clin Virol. 2010;47:216–218. doi: 10.1016/j.jcv.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 24.Antonsson A, Erfurt C, Hazard K, Holmgren V, Simon M, et al. Prevalence and type spectrum of human papillomaviruses in healthy skin samples collected in three continents. J Gen Virol. 2003;84:1881–1886. doi: 10.1099/vir.0.18836-0. [DOI] [PubMed] [Google Scholar]
- 25.Kocjan BJ, Poljak M, Seme K, Potočnik M, Fujs K, et al. Distribution of human papillomavirus genotypes in plucked eyebrow hairs from Slovenian males with genital warts. Infect Genet Evol. 2005;5:255–259. doi: 10.1016/j.meegid.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 26.Hall TA. BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucleic Acids Symposium Series. 1999;41:95–98. [Google Scholar]
- 27.Katoh K, Misawa K, Kuma K-ichi, Miyata T. MAFFT: a novel method for rapid multiple sequence alignment based on fast Fourier transform. Nucleic Acids Res. 2002;30:3059–3066. doi: 10.1093/nar/gkf436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suyama M, Torrents D, Bork P. PAL2NAL: robust conversion of protein sequence alignments into the corresponding codon alignments. Nucleic Acids Res. 2006;34:W609–612. doi: 10.1093/nar/gkl315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Talavera G, Castresana J. Improvement of phylogenies after removing divergent and ambiguously aligned blocks from protein sequence alignments. Syst Biol. 2007;56:564–577. doi: 10.1080/10635150701472164. [DOI] [PubMed] [Google Scholar]
- 30.Castresana J. Selection of conserved blocks from multiple alignments for their use in phylogenetic analysis. Mol Biol Evol 17: 540 2000;-552 doi: 10.1093/oxfordjournals.molbev.a026334. [DOI] [PubMed] [Google Scholar]
- 31.Stamatakis A. RAxML-VI-HPC: maximum likelihood-based phylogenetic analyses with thousands of taxa and mixed models. Bioinformatics. 2006;22:2688–2690. doi: 10.1093/bioinformatics/btl446. [DOI] [PubMed] [Google Scholar]
- 32.Ott M, Zola J, Stamatakis A, Aluru S. Large-scale maximum likelihood-based phylogenetic analysis on the IBM BlueGene/L. Supercomputing, 2007. 2007. pp. 1–11. SC’07.Proceedings of the 2007 ACM/IEEE Conference on.
- 33.Stamatakis A, Hoover P, Rougemont J. A rapid bootstrap algorithm for the RAxML Web servers. Syst Biol. 2008;57:758–771. doi: 10.1080/10635150802429642. [DOI] [PubMed] [Google Scholar]
- 34.Whelan JA, Russell NB, Whelan MA. A method for the absolute quantification of cDNA using real-time PCR. J Immunol Methods. 2003;278:261–269. doi: 10.1016/s0022-1759(03)00223-0. [DOI] [PubMed] [Google Scholar]
- 35.Potočnik M, Kocjan BJ, Seme K, Poljak M. Distribution of human papillomavirus (HPV) genotypes in genital warts from males in Slovenia. Acta Dermatovenerol Alp Panonica Adriat. 2007;16:91–96,98. [PubMed] [Google Scholar]
- 36.Jančar N, Kocjan BJ, Poljak M, Lunar MM, Bokal EV. Distribution of human papillomavirus genotypes in women with cervical cancer in Slovenia. Eur J Obstet Gynecol Reprod Biol. 2009;145:184–188. doi: 10.1016/j.ejogrb.2009.04.030. [DOI] [PubMed] [Google Scholar]
- 37.Kocjan BJ, Poljak M, Cimerman M, Gale N, Potočnik M, et al. Prevaccination genomic diversity of human papillomavirus genotype 6 (HPV 6). Virology. 2009;391:274–283. doi: 10.1016/j.virol.2009.06.030. [DOI] [PubMed] [Google Scholar]
- 38.Kocjan BJ, Seme K, Cimerman M, Kovanda A, Potočnik M, et al. Genomic diversity of human papillomavirus (HPV) genotype 38. J Med Virol. 2009;81:288–295. doi: 10.1002/jmv.21392. [DOI] [PubMed] [Google Scholar]
- 39.de Roda Husman AM, Walboomers JM, van den Brule AJ, Meijer CJ, Snijders PJ. The use of general primers GP5 and GP6 elongated at their 3′ ends with adjacent highly conserved sequences improves human papillomavirus detection by PCR. J Gen Virol. 1995;76:1057–1062. doi: 10.1099/0022-1317-76-4-1057. [DOI] [PubMed] [Google Scholar]
- 40.Krubke J, Kraus J, Delius H, Chow L, Broker T, et al. Genetic relationship among human papillomaviruses associated with benign and malignant tumours of patients with epidermodysplasia verruciformis. J Gen Virol. 1987;68:3091–3103. doi: 10.1099/0022-1317-68-12-3091. [DOI] [PubMed] [Google Scholar]
- 41.Lazarczyk M, Cassonnet P, Pons C, Jacob Y, Favre M. The EVER proteins as a natural barrier against papillomaviruses: a new insight into the pathogenesis of human papillomavirus infections. Microbiol. Mol Biol Rev. 2009;73:348–370. doi: 10.1128/MMBR.00033-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ensser A, Pfister H. Epidermodysplasia verruciformis associated human papilomaviruses present a subgenus-specific organization of the regulatory genome region. Nucl Acid Res. 1990;18:3919–3922. doi: 10.1093/nar/18.13.3919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gottschling M, Göker M, Stamatakis A, Bininda-Emonds ORP, Nindl I, et al. Quantifying the phylodynamic forces driving papillomavirus evolution. Mol Biol Evol . 2011. Available: http://mbe.oxfordjournals.org/content/early/2011/01/31/molbev.msr030.abstract. [DOI] [PubMed]
- 44.de Villiers E-M, Gunst K. Characterization of seven novel human papillomavirus types isolated from cutaneous tissue, but also present in mucosal lesions. Jof Gen Virol. 2009;90:1999–2004. doi: 10.1099/vir.0.011478-0. [DOI] [PubMed] [Google Scholar]
- 45.Boxman IL, Berkhout RJ, Mulder LH, Wolkers MC, Bouwes Bavinck JN, et al. Detection of human papillomavirus DNA in plucked hairs from renal transplant recipients and healthy volunteers. J Invest Dermatol. 1997;108:712–715. doi: 10.1111/1523-1747.ep12292090. [DOI] [PubMed] [Google Scholar]
- 46.Boxman IL, Russell A, Mulder LH, Bavinck JN, Schegget JT, et al. Case-control study in a subtropical Australian population to assess the relation between non-melanoma skin cancer and epidermodysplasia verruciformis human papillomavirus DNA in plucked eyebrow hairs. The Nambour Skin Cancer Prevention Study Group. Int J Cancer. 2000;86:118–121. doi: 10.1002/(sici)1097-0215(20000401)86:1<118::aid-ijc18>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 47.Köhler A, Meyer T, Stockfleth E, Nindl I. High viral load of human wart-associated papillomaviruses (PV) but not beta-PV in cutaneous warts independent of immunosuppression. Br J Dermatol. 2009;161:528–535. doi: 10.1111/j.1365-2133.2009.09297.x. [DOI] [PubMed] [Google Scholar]
- 48.Orth G. Human papillomaviruses associated with epidermodysplasia verruciformis in non-melanoma skin cancers: guilty or innocent? J Invest Dermatol. 2005;125:xii–xiii. doi: 10.1111/j.0022-202X.2005.23811.x. [DOI] [PubMed] [Google Scholar]
- 49.Weissenborn SJ, Nindl I, Purdie K, Harwood C, Proby C, et al. Human papillomavirus-DNA loads in actinic keratoses exceed those in non-melanoma skin cancers. J Invest Dermatol. 2005;125:93–97. doi: 10.1111/j.0022-202X.2005.23733.x. [DOI] [PubMed] [Google Scholar]
- 50.Purdie KJ, Surentheran T, Sterling JC, Bell L, McGregor JM, et al. Human papillomavirus gene expression in cutaneous squamous cell carcinomas from immunosuppressed and immunocompetent individuals. J Invest Dermatol. 2005;125:98–107. doi: 10.1111/j.0022-202X.2005.23635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Primers used for initial amplification, primer walking and preparation of HPV-150 and HPV-151 reference clones. Nt – Nucleotide position. N – Random nucleotide. Cw – Clock-wise. Ccw – Counter clock-wise.
(DOC)