Abstract
Although exposure to early adversity and prior experiences with depression have both been associated with lower levels of precipitating life stress in depression, it is unclear whether these stress sensitization effects are similar for all types of stress or whether they are specific to stressors that may be particularly depressogenic, such as those involving interpersonal loss. To investigate this issue, we administered structured, interview-based measures of early adversity, depression history, and recent life stress to one hundred adults who were diagnosed with inflammation disorder. As predicted, individuals who experienced early parental loss or prolonged separation (i.e., lasting one year or longer) and persons with more lifetime episodes of depression became depressed following lower levels of life stress occurring in the etiologically-central time period of three months prior to onset of depression. Importantly, however, additional analyses revealed that these effects were unique to stressors involving interpersonal loss. These data highlight potential stressor-specific effects in stress sensitization and demonstrate for the first time that individuals exposed to early parental loss or separation, and persons with greater histories of MDD, may be selectively sensitized to stressors involving interpersonal loss.
Keywords: Interpersonal loss, Parental separation, Depression recurrence, Stressful life events, Stressor characteristics, Selective sensitization, Early adversity, Inflammation
A large literature now exists documenting a strong association between major life events, such as the termination of an important relationship or job, and the subsequent onset of Major Depressive Disorder (MDD; Hammen, 2005; Kendler et al., 1999; Kessler, 1997; Monroe et al., 2009). Nevertheless, an estimated 30% of first-onset depressive episodes and 60% of all recurrent episodes appear to develop in the absence of major forms of stress (Monroe and Harkness, 2005). As a result, it has been suggested that some individuals may be especially sensitive to the depressogenic effects of stress and, consequently, develop depression in response to more minor forms of adversity. This phenomenon, which is believed to be mediated at least in part by neurobiological kindling and behavioral sensitization, has generally been referred to as stress sensitization (Kendler et al., 2000, 2001; Kessing et al., 1998, 2004; Monroe and Harkness, 2005; Post, 1992, 2007; Segal et al., 1996).
Although a complete account of factors that impact stress sensitization is not yet available, there is growing evidence that childhood adversity and prior experiences with depression may both play a role. For example, several studies have now demonstrated that individuals who experience a major early adversity, such as parental loss or physical abuse, develop depression following lower levels of life stress than do persons without such adversity (Hammen et al., 2000; Harkness et al., 2006; Kendler et al., 2004; Rudolph and Flynn, 2007; see also Dienes et al., 2006). Moreover, a number of studies have shown that individuals with more lifetime episodes of MDD exhibit lower levels of precipitating life stress than do persons with fewer lifetime episodes of the disorder (Kendler et al., 2000; Monroe et al., 2007a; Stroud et al., 2008, 2011; see also Morris et al., 2010).
Considered together, these findings provide support for the possibility that persons who have experienced early adversity or who have a history of depression may be sensitized to stress such that they have the capability of developing MDD following relatively lower levels of adversity. Rarely, however, have the effects of early adversity and depression history been examined together in the same sample. In addition, no studies to date have investigated whether stress sensitization effects are similar for all types of stress or, alternatively, whether they are specific to types of stressors that may be highly depressogenic, such as those involving interpersonal loss. Relevant to this issue is a growing body of research suggesting that interpersonal loss events are strongly associated with depression (Slavich et al., 2009, 2010a). Stressors involving interpersonal loss, for example, are the most common precipitant of depression, with 44% of depressive episodes being preceded by such stress (Farmer and McGuffin, 2003; see also Brown et al., 1995). In addition, two large epidemiologic studies have reported that risk for depression is greater following interpersonal loss (hazard ratios = 1.70 and 1.76, respectively) than for any other type of major life event (Kendler et al., 2003; Monroe et al., 1999). Given these findings, persons at risk for depression may be more sensitive to stressors involving interpersonal loss (e.g., relationship break-ups, deaths) than to other types of stressors (e.g., occupational or financial problems). Importantly, however, no studies have examined this issue of stressor specificity in the context of stress sensitization in depression.
To examine associations between early adversity and depression history with levels of pre-onset life stress in depression, we administered structured, interview-based measures of these constructs to adults who were diagnosed with MDD. We were particularly interested in early adversities that involved parental loss or prolonged separation, given previous research showing that stressors of this type are associated with elevated risk for depression in adulthood (e.g., Bifulco et al., 1987; Coffino, 2009). We then conducted two sets of analyses. First, we examined the relations of early parental loss or separation and depression history to levels of pre-onset life stress, regardless of event type (i.e., interpersonal loss and non-loss events considered together). Next, we conducted the same analyses while separating pre-onset interpersonal loss and non-loss events. Consistent with previous research, we hypothesized that individuals with a history of early parental loss or separation, and persons with more lifetime episodes of depression, would become depressed following lower levels of recent, pre-onset life stress. We hypothesized further that the relations of early parental loss or separation and depression history to levels of pre-onset stress would be particularly strong for stressors involving interpersonal loss.
1. Method
1.1 Participants and procedures
Participants were 100 adults (74 females) between the ages of 18 and 58 years old (M = 35.1, SD = 10.4). These individuals, all diagnosed with MDD, were drawn from a larger study examining the roles of life stress and cognitive vulnerability in depression (Gotlib et al., 2004a, 2004b; Monroe et al., 2007a, 2007b; Muscatell et al., 2009; Slavich et al., 2009). Most participants (58%) were single, with 34% married or living with a domestic partner and 8% divorced. Ethnicity was primarily Caucasian (52%) and Asian (40%), followed by African American (4%), Latino or Hispanic (2%), and other (2%). The sample was generally well-educated, with 56% of participants having completed college, 26% reporting graduate or professional education beyond college, and 18% reporting some college or less. Finally, the sample was varied with respect to annual income, with 15% of participants earning under $10,000, 15% earning between $10,000 and $25,000, 25% earning between $25,000 and $50,000, 17% earning between $50,000 and $75,000, and 20% earning more than $75,000 (8 participants declined to report their income).
Participants were recruited through community advertisements and through referrals from two outpatient psychiatry clinics at Stanford University. Individuals were screened by telephone to recruit persons with a high likelihood of current MDD with a recent and distinct onset of the disorder (98% of participants had their onset of depression within 2.5 years and the average current episode length was 7.8 months). Individuals who passed this telephone screen were invited to complete an in-person diagnostic interview. To be included in the study, participants had to meet Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; American Psychiatric Association, 2000) criteria for current MDD, as assessed by the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First et al., 2002). In addition, they had to have no detectable episodes of MDD, and be relatively free of depressive symptoms, for six months prior to onset of the index episode of depression.
The diagnostic interviews were conducted by advanced graduate students who were trained to “gold standard” reliability status (see Grove et al., 1981). To assess diagnostic inter-rater reliability, an independent rater kept blind to group membership evaluated 15 SCID audiotapes selected at random from the parent project, which included individuals with depression, panic disorder, social phobia, and no psychopathology. In all 15 of the reassessed cases, the re-rating matched the original diagnosis, κ = 1.00. Although this represents excellent reliability, interviewers used the “skip out” strategy of the SCID, which may have reduced the opportunities for the independent raters to disagree with the diagnoses. Individuals were excluded if they had current comorbid panic disorder or social phobia; a lifetime history of mania, hypomania, or primary psychotic symptoms; a recent history (i.e., past 6 months) of alcohol or substance abuse or dependence; or a history of brain injury or mental retardation. Participants who met all inclusion requirements were invited for an additional session in which their exposure to life stress was assessed (see below). All participants provided written informed consent and were paid $25 per hour.
1.2 Early parental loss/separation
Detailed information regarding participants’ history of parental loss and separation was collected during the life stress assessment session. Participants were asked whether they had ever lost or been separated from their mother, father, or primary caregiver before age 17. If participants responded “yes,” they were asked to identify the age at which the loss/separation occurred, the duration of the separation (if a separation), and the specific reason for the loss/separation. Consistent with prior research (Rudolph and Flynn, 2007), participants were judged to be positive for a history of parental loss/separation if they lost a parent or primary caregiver (e.g., to death) or were separated from at least one parent (or primary caregiver) for a period lasting one year or longer. Based on these criteria, 51 individuals had no history of parental loss/separation and 49 individuals had a history of parental loss/separation involving one (n = 32, 65.3%) or both (n = 17, 34.7%) parents. Participants’ mean age at loss/separation was 8.9 years (SD = 5.3). Of the 49 parental losses/separations, 23 (46.9%) were due to marital separation or divorce, 8 (16.3%) were due to death, 5 (10.2%) were due to paternal abandonment, 4 (8.2%) were due to father’s absence because of work, 2 (4.1%) were due to mother’s absence because of work, and 7 (14.3%) were the result of prolonged parental absence due to other extenuating circumstances.
1.3 History of depression
Number of lifetime episodes of MDD was carefully assessed as part of the SCID. Interviewers systematically inquired about each depressive experience to determine if it met diagnostic criteria for MDD. The total number of lifetime depressive episodes (including the index episode) ranged from 1 (n = 18) to “too many to count” (n = 15). The majority of participants had four or fewer lifetime episodes, and there were an ample number of participants with up to five lifetime episodes within each of these categories. Beyond five lifetime episodes, the number of participants per depression history category decreased substantially. Consequently, for individuals with more than five episodes, we collapsed across depression history categories to provide a more uniform index of depression history. Individuals with six or more lifetime episodes were collapsed into three categories (6–10 episodes, 11–36 episodes, > 36 episodes or “too many to count”). The final distribution of participants across categories was: 1 lifetime episode, n = 18; 2 lifetime episodes, n = 14; 3 lifetime episodes, n = 14; 4 lifetime episodes, n = 7; 5 lifetime episodes, n = 9; 6–10 lifetime episodes, n = 12; 11–36 lifetime episodes, n = 11; and > 36 lifetime episodes, n = 15.
1.4 Stressful life events and chronic difficulties
Stressful life events and chronic difficulties that preceded onset of depression were assessed using the Life Events and Difficulties Schedule (LEDS; Brown and Harris, 1978). The LEDS has established psychometric validity and is regarded as a state-of-the-art instrument for assessing diverse types of stress (Dohrenwend, 2006; Hammen, 2005; Monroe, 2008). This system uses a two-hour semi-structured interview in which the interviewer carefully inquires about potential stressors in ten domains of functioning (e.g., health, work, education, relationships, etc.). Next, the interviewer presents the reported stressors to a panel of trained raters who judge each stressor using a 520-page manual that outlines explicit rules and criteria for rating life stress. The manual also includes 5,000 case vignettes that are used as standardized anchors in the rating process. All ratings are made independently by each rater and are then finalized following a consensus discussion that considers extensive information about the stressor and the individual’s biographical circumstances (i.e., “contextual” ratings; see Brown and Harris, 1978, 1989).
In the present study, after the LEDS interviews were completed, the interviewer presented the detailed life stress profiles to an independent panel of 3–4 expert LEDS raters. These raters were kept blind to participants’ clinical characteristics (e.g., timing of onset of depression, history of depression), as well as to their emotional response to the stressors (e.g., how often they cried), to prevent this information from influencing the life stress ratings. Inter-rater agreement ranged from κ = .72 to κ = .79 (M = .76; corrected for differences in the number of raters per event; Uebersax, 1982).
The primary outcomes of interest were participants’ levels of overall and stressor-specific (i.e., interpersonal loss vs. non-loss) pre-onset stress. These variables were based on the long-term threat (i.e., severity) and focus of each event. In accordance with the LEDS system, each event was rated on a 5-point severity scale (1 = marked, 2a = high moderate, 2b = low moderate, 3 = some, 4 = little/none). With respect to focus, events that occurred to the participant were categorized as subject or joint focused, and those that occurred to another person in the participant’s social network were categorized as other focused. Based on these dimensions, and consistent with prior research (Harkness et al., 2006), four stress levels were derived: Level 4 = events rated 4 (little/none) on threat; Level 3 = events rated 3 (some) on threat; Level 2 = events rated 2b (low moderate) and 2a (high moderate) on threat, which were other focused; and Level 1 = events rated 1 (marked) and 2a (high moderate) on threat, which were subject or joint focused. As per prior work (Harkness et al., 2006), these levels were then reverse coded, summed together, and divided by the total number of events reported to form an average pre-onset life stress score for each participant (M = 1.8, SD = 1.0). Because stressors occurring relatively close in time to onset of depression have the greatest likelihood of being etiologically relevant (Brown and Harris, 1989; Harkness et al., 2006), the final pre-onset life stress index was restricted to life events that occurred within 3 months of onset of depression.
To derive separate life stress scores for interpersonal loss and non-loss events, each stressor that occurred within 3 months of onset of depression was categorized as either interpersonal loss or non-loss by a team of two LEDS raters. Events were categorized as interpersonal loss if they involved the death of a close friend or loved one (e.g., parent, partner, sibling, close family member, or confidant), or the dissolution or termination of a key relationship (e.g., with any of these individuals). All other events (i.e., those not involving interpersonal loss) were judged to be non-loss events. Inter-rater agreement for these determinations ranged from κ = .84 to κ = .91 (M = .88). Pre-onset interpersonal loss and non-loss stress scores were then computed by summing together and then averaging the contextual long-term threat ratings for the interpersonal loss events (M = 1.5, SD = 1.5) and non-loss events (M = 1.3, SD = 0.9) that each participant experienced.
Finally, although our primary hypotheses focused on differing levels of pre-onset acute life stress, sensitivity to acute stress may be influenced by exposure to chronic stress, which has been found to be related to both early adversity and depression history status (Brown and Harris, 1986; Cicchetti and Toth, 2005; Harkness et al., 2006). Consequently, we also assessed levels of pre-onset chronic stress. These stressors were rated on a 6-point scale in accord with the LEDS system (1 = high marked, 2 = low marked, 3 = high moderate, 4 = low moderate, 5 = mild, 6 = very mild). Severity scores were subsequently reversed coded so that higher values represented greater levels of threat. The scores were then summed and divided by the total number of difficulties reported to compute each participant’s chronic difficulty stress score (M = 1.1, SD = 1.3). Chronic difficulties were required to be present for at least 4 weeks of the 3-month pre-onset time period, although the average chronic difficulty length was 34.1 months. Difficulties directly attributable to a depressive episode (e.g., ongoing sleep problems) were excluded.
1.5 Data analyses
Preliminary univariate analyses were conducted on all demographic and study variables. Separate hierarchical regression analyses were then conducted to predict levels of pre-onset overall stress, interpersonal loss stress, and non-loss stress. For each model, level of pre-onset chronic difficulty stress was entered first (to adjust for its potential contribution to sensitization), parental loss/separation was entered second (because of its temporal precedence relative to depression history), and depression history was entered third. The cross-product interaction term of Parental Loss/Separation × Depression History was entered into the equation last to rule out a possible interaction between these factors (Cohen and Cohen, 1983). Finally, these analyses were rerun without chronic difficulty stress to ensure that significant results could not be due to having adjusted for pre-onset chronic difficulties.
2. Results
2.1 Preliminary analyses
Age, sex, marital status, ethnicity, and income were unrelated to the main outcomes variables (i.e., participants’ levels of pre-onset overall, interpersonal loss, and non-loss stress). Early parental loss/separation was unrelated to level of pre-onset chronic difficulty stress, F(1, 98) = 0.01, p = .919, R2 = .001. Participants with a history of parental loss/separation tended to have more lifetime episodes of depression (M = 4.7, SD = 2.4) than did those without a history of parental loss/separation (M = 4.0, SD = 2.5), although this difference was not statistically significant, t(98) = −1.39, p = .168, d = 0.28. Participants with more lifetime episodes of depression exhibited lower levels of pre-onset overall stress (r = −.30, p = .002) and interpersonal loss stress (r = −.41, p = .001), but higher levels of pre-onset chronic difficulty stress (r = .34, p = .001), underscoring the importance of adjusting for chronic difficulties in tests of our primary hypotheses (Monroe et al., 2007a). Finally, although neither acute interpersonal loss nor non-loss stress were related to pre-onset chronic difficulty stress (r = −.08, p = .428, and r = .14, p = .157, respectively), as expected, levels of overall acute stress were positively correlated with both pre-onset interpersonal loss stress (r = .61, p = .001) and non-loss stress (r = .59, p = .001).
2.2 Primary analyses
Hierarchical regression models testing the relations of early parental loss/separation and depression history to average levels of pre-onset acute and chronic life stress are presented in Table 1. Pre-onset chronic difficulty stress was unrelated to levels of recent overall acute stress (p = .474), interpersonal loss stress (p = .428), and non-loss stress (p = .157). Consistent with previous studies on stress sensitization in depression, early parental loss/separation and greater depression history were both significantly associated with lower levels of overall pre-onset life stress (p = .030 and p = .001, respectively), demonstrating that persons with early parental loss/separation and greater depression history became depressed following relatively lower levels of stress.
Table 1.
Hierarchical regression models for parental loss/separation and depression history predicting average levels of pre-onset life stress by stressor type
| Type of stress and predictor | β | Multiple R |
R2 | ΔR2 | ΔF (dfs) | p |
|---|---|---|---|---|---|---|
| Overall stress | ||||||
| Step 1: Difficulty stress | .072 | .072 | .005 | .005 | 0.52 (1, 98) | .474 |
| Step 2: Parental loss/separation | −.218 | .229 | .053 | .047 | 4.85 (1, 97) | .030 |
| Step 3: Depression history | −.346 | .395 | .156 | .103 | 11.75 (1, 96) | .001 |
| Step 4: Parental loss/separation × Depression history interaction | .169 | .401 | .161 | .005 | 0.59 (1, 95) | .445 |
| Interpersonal loss stress | ||||||
| Step 1: Difficulty stress | −.080 | .080 | .006 | .006 | 0.63 (1, 98) | .428 |
| Step 2: Parental loss/separation | −.226 | .240 | .058 | .051 | 5.28 (1, 97) | .024 |
| Step 3: Depression history | −.403 | .444 | .197 | .140 | 16.69 (1, 96) | .001 |
| Step 4: Parental loss/separation × Depression history interaction | .318 | .464 | .216 | .018 | 2.23 (1, 95) | .139 |
| Non-loss stress | ||||||
| Step 1: Difficulty stress | .142 | .142 | .020 | .020 | 2.03 (1, 98) | .157 |
| Step 2: Parental loss/separation | −.040 | .148 | .022 | .002 | 0.16 (1, 97) | .690 |
| Step 3: Depression history | −.097 | .173 | .030 | .008 | 0.81 (1, 96) | .371 |
| Step 4: Parental loss/separation × Depression history interaction | .017 | .174 | .030 | .000 | 0.01 (1, 95) | .942 |
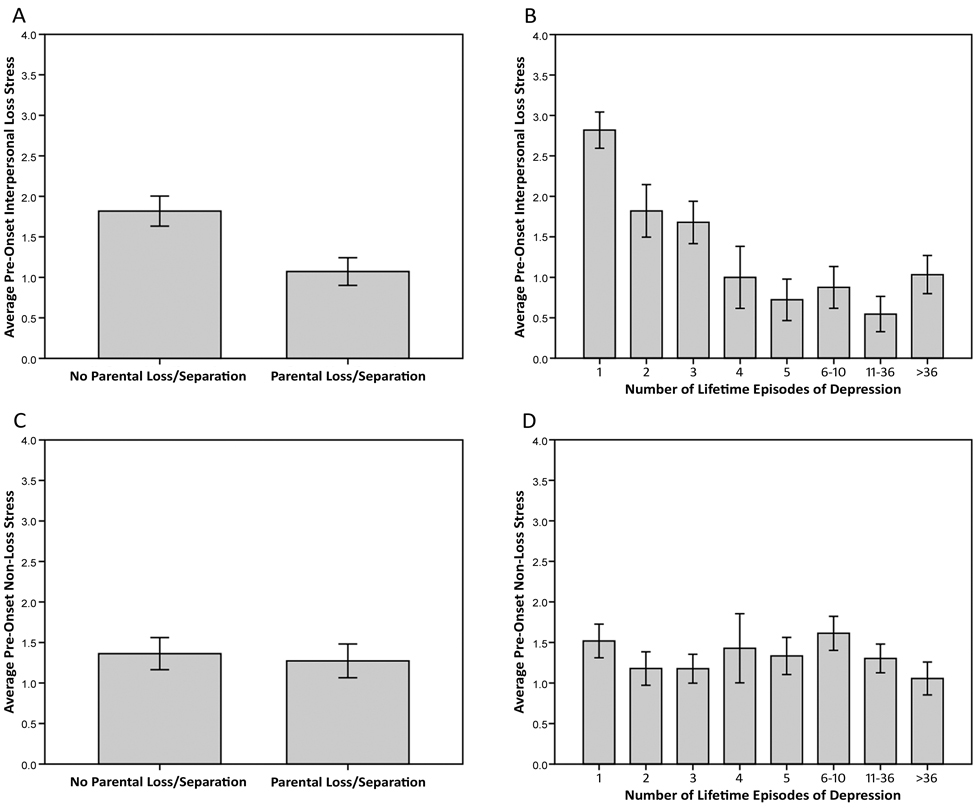
As we described above, we also examined whether these effects differed by type of stress (i.e., interpersonal loss vs. non-loss stress). Consistent with hypotheses, early parental loss/separation and greater depression history were both significantly associated with lower levels of pre-onset interpersonal loss stress (p = .024 and p = .001, respectively). As shown in Figure 1a, for example, participants exposed to early parental loss or prolonged separation became depressed following interpersonal loss events that were approximately half as severe as those experienced by individuals who were not exposed to early parental loss or separation. In addition, as depicted in Figure 1b, the severity level of a precipitating interpersonal loss event decreased by an average of .25 points for each additional depressive episode experienced. In contrast to these effects, early parental loss/separation and depression history were both unrelated to levels of pre-onset non-loss stress (p = .690 and p = .371, respectively; see Figure 1c and Figure 1d). Finally, the interaction of parental loss/separation and depression history was not significant for all analyses (all ps > .14).
Fig. 1.
Relations of early parental loss/separation and depression history to levels of pre-onset interpersonal loss and non-loss stress, expressed as mean ± SEM. Individuals exposed to early parental loss or prolonged separation (i.e., lasting one year or longer) and persons with more lifetime episodes of depression became depressed following lower levels of interpersonal loss stress occurring in the etiologically-central time period of three months prior to onset of depression (see A & B). This effect was robust when adjusting for levels of pre-onset chronic difficulty stress. In contrast, early parental loss/separation and depression history were unrelated to levels of pre-onset non-loss stress (see C & D) (n = 100).
These analyses were rerun without adjusting for pre-onset chronic difficulties, and this did not alter the results. Specifically, early parental loss/separation and greater depression history continued to be significantly associated with lower levels of pre-onset overall stress (β = −.218, t = −2.21, p = .029, and β = −.279, t = −2.91, p = .004, respectively). In addition, early parental loss/separation and greater depression history continued to be significantly associated with lower levels of interpersonal loss stress (β = −.226, t = −2.29, p = .024, and β = −.383, t = −4.16, p = .001, respectively). Finally, parental loss/separation and depression history continued to be unrelated to levels of pre-onset non-loss stress (β = −.042, t = −0.41, p = .681, and β = −.035, t = −0.34, p = .730, respectively). Therefore, the relations of early parental loss/separation and depression history to levels of pre-onset overall and interpersonal loss stress are not dependent on having adjusted for pre-onset chronic difficulties.
3. Discussion
A relatively large body of research demonstrates that individuals with a history of a major early adversity and persons with more lifetime episodes of depression develop MDD following lower levels of life stress compared to their less-vulnerable counterparts (Monroe and Harkness, 2005; Stroud et al., 2008, 2011). The present data replicate this effect, but suggest for the first time that these associations may be unique to stressors involving interpersonal loss. Specifically, in a relatively large sample of adults who were clinically diagnosed with MDD and then administered interview-based measures of early adversity, depression history, and recent life stress, we found evidence that early parental loss/separation and more lifetime episodes of depression were associated with lower levels of interpersonal loss stress occurring over the etiologically-central time period of three months prior to onset of depression. Importantly, however, individuals did not differ on levels of non-loss stress. From these findings, we conclude that individuals who are exposed to early parental loss or separation, and persons with greater histories of depression, may be selectively sensitized to stressors involving interpersonal loss insofar as they become depressed following lower levels of interpersonal loss (but not non-loss) stress.
Because individuals who experience early adversity and persons with a history of depression have a greater likelihood of experiencing chronic stress in their lives (Cicchetti and Toth, 2005; Harkness et al., 2006; Monroe et al., 2007a), we adjusted for levels of pre-onset chronic stress in tests of our primary hypotheses. Including chronic stress in these models, however, did not alter the results. In addition, when we reran the primary regression models without adjusting for pre-onset chronic difficulties, the effects of early parental loss/separation and depression history on levels of pre-onset life stress were unchanged. The significant results reported here, therefore, are not due to having adjusted for levels of pre-onset chronic difficulty stress.
Different types of psychosocial stress have largely been treated as functionally equivalent in contemporary research on life stress and depression (cf. Brown et al., 1995; Kendler et al., 2003; Slavich et al., 2009). Although parsimonious, conceptualizing stress in this way obscures potentially important information that could help researchers and clinicians understand who is vulnerable for depression when exposed to different types of adversity (Monroe & Slavich, 2007). Knowing that certain individuals may become depressed following relatively low levels of interpersonal loss may help inform the next generation of integrative models of risk for depression that take into account the effects that different types of stress have on the disorder (e.g., Backs-Dermott et al., 2010). This information could also be used to inform the development of targeted intervention strategies that are aimed at reducing risk for depression among persons who have experienced a major early interpersonal loss or who have a history of MDD (Muñoz et al., 2010; Smit et al., 2004).
Although we did not examine the mechanisms by which lower-level stressors promote depression, several mediators are possible. Consistent with cognitive models of risk for depression, for example, individuals who experience early parental loss or separation may develop negative cognitive schemas that include themes of inferiority, loss, and rejection (Beck, 1967, 2008; Bowlby, 1969; Segal et al., 1996; Young, 1999). When activated, these schemas direct attention to—and enhance memory for—schema-congruent information, and they negatively skew the interpretation of neutral or ambiguous information. Activated schemas also give rise to specific negative thoughts (e.g., “I’m unlovable, “Other people are unavailable,” “I’ll always be alone”) and related self-conscious emotions (e.g., shame, guilt, humiliation). Insofar as depressogenic cognitive schemas are preferentially activated by stressors that are reminiscent of the original adversity (see Beck, 1967, 2008), individuals who experience parental loss or separation in childhood may be especially sensitive to interpersonal loss and, therefore, more likely to develop depression following lower levels of interpersonal loss stress later in life. Similarly, if depressogenic cognitive schemas often involve loss (i.e., because interpersonal loss is the most common precipitant of depression; Farmer and McGuffin, 2003), and if these schemas become more easily activated over successive recurrences of depression (Beck, 1967, 2008), then negative schematic processing may also underlie the heightened sensitivity to interpersonal loss that is exhibited by persons with greater lifetime histories of depression (see also Wichers et al., 2009, 2010).
There also exists a broader set of questions regarding the biological processes that mediate the link between life stress and depression. Relevant to this issue is a growing body of animal and human research showing that social stressors upregulate components of the immune system involved in inflammation (Avitsur et al., 2009; Segerstrom & Miller, 2004; Steptoe et al., 2007). Although this response can be adaptive, pro-inflammatory cytokines, which mediate inflammatory responses to stress, are powerful and can act on the central nervous system to induce a constellation of behaviors called sickness behaviors (Miller et al., 2009; Wolkowitz et al., 2010). Sickness behaviors facilitate an organism’s recuperation and recovery from illness or injury, and they include specific depressotypic symptoms such as anhedonia, fatigue, psychomotor retardation, cognitive dysfunction, irritability, altered sleep, increased pain sensitivity, and social-behavioral withdrawal (Dantzer et al., 2008; Yirmiya et al., 2000). Interestingly, although many individuals mount an inflammatory response to acute social stress, the magnitude of this response is greatest for people who are neurally sensitive to social rejection (Slavich et al., 2010b). In sum, then, social stressors may evoke depression (at least in part) by upregulating inflammatory activity, and this response may be potentiated for persons who are sensitive to rejection (Slavich et al., 2010a).
3.1 Strengths and limitations
Strengths of the present study include a sample that was well-characterized with respect to depression history and current depression status (e.g., the sample was carefully screened to include only individuals with current MDD with a relatively recent and distinct onset of the disorder). As a result, all participants were clinically depressed at the time of the study; importantly, however, they had no detectable episodes of MDD for six months prior to the index episode. Another strength of this study is the use of the LEDS system, which involved an expert interviewer and an independent team of trained raters who judged the contextual threat and specific timing of each stressor that was reported. This enabled us to ensure that all of the life events analyzed occurred in the critical period of three months prior to onset of depression. The LEDS system was also helpful because it permitted us to distinguish between interpersonal loss and non-loss life events, which is difficult (if not impossible) to do with less sophisticated measures of stress (Dohrenwend, 2006; Monroe, 2008).
We should also note a number of limitations of this study. First, because we used a cross-sectional design, we cannot determine the causal nature of the associations among the constructs we assessed. Future research should use a prospective, longitudinal design to examine issues of causality. Second, our assessment of life stress was based on the retrospective reports of depressed individuals. Although our stress variables were derived from the judgments of a team of expert raters who utilized a set of extensive rules and criteria to rate the stressors that were reported, it is nevertheless possible that respondent biases influenced our ratings of life stress. Third, because we had limited information about forms of early adversity other than early parental loss and separation, we were not able to examine the effects that other types of early adversity may have had on individuals’ sensitivity to recent life stress. Fourth, we did not examine non-demographic factors that may moderate the effects of early parental loss and depression history. However, several are possible, including social support, treatment exposure, and psychosocial resources (e.g., optimism, mastery, self-esteem; Taylor & Seeman, 1999). Considering that men and women differ in rates of both depression (Nolen-Hoeksema, 2001) and pre-onset life events (Harkness et al., 2010), gender differences in selective sensitization may also exist. However, we were not able to comprehensively test for such differences given that the present sample contained relatively few men. Future research along each of these lines could be fruitful. Finally, the present data do not speak to the mechanisms by which low-level stressors promote depression. Additional research examining social stress-induced changes in cognitive, emotional, and biological processes is required to address this important issue.
3.2 Concluding comments
In sum, the present data demonstrate that individuals exposed to early parental loss or separation and persons with greater histories of depression become depressed following relatively lower levels of psychosocial stress. Importantly, however, these associations appear to be unique to stressors involving interpersonal loss, an effect we call selective sensitization. Additional research is needed to elucidate the cognitive, emotional, and neurobiological mechanisms that underlie stress sensitization, and to examine the variety of factors that may moderate these effects. Research is also needed to identify the specific characteristics that make interpersonal loss events highly depressogenic (Monroe and Slavich, 2007; Slavich et al., 2009, 2010a).
Acknowledgments
We thank Lauren Anas, Erica Aronson, Kathryn Dingman, and Danielle Keenan-Miller for conducting the life stress interviews; Corrie Doyle, Julien Guillaumot, Keely Muscatell, Tiffany Thornton, and Leandro Torres for participating in the life stress ratings; Faith Brozovich for assisting with data management; and Margaret Kemeny and Keely Muscatell for commenting on a previous version of this report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fourth edition – text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Avitsur R, Powell N, Padgett DA, Sheridan JF. Social interactions, stress, and immunity. Immunology and Allergy Clinics of North America. 2009;29:285–293. doi: 10.1016/j.iac.2009.02.006. [DOI] [PubMed] [Google Scholar]
- Backs-Dermott BJ, Dobson KS, Jones SL. An evaluation of an integrated model of relapse in depression. Journal of Affective Disorders. 2010;124:60–67. doi: 10.1016/j.jad.2009.11.015. [DOI] [PubMed] [Google Scholar]
- Beck AT. Depression: Clinical, experimental, and theoretical aspects. New York: Harper and Row; 1967. [Google Scholar]
- Beck AT. The evolution of the cognitive model of depression and its neurobiological correlates. American Journal of Psychiatry. 2008;165:969–977. doi: 10.1176/appi.ajp.2008.08050721. [DOI] [PubMed] [Google Scholar]
- Bifulco AT, Brown GW, Harris TO. Childhood loss of parent, lack of adequate parental care and adult depression: a replication. Journal of Affective Disorders. 1987;12:115–128. doi: 10.1016/0165-0327(87)90003-6. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: Vol. 1. Attachment. New York: Basic Books; 1969. [Google Scholar]
- Brown GW, Harris TO. Social origins of depression: a study of psychiatric disorder in women. New York: Free Press; 1978. [Google Scholar]
- Brown GW, Harris TO. Establishing causal links: The Bedford College studies of depression. In: Katschnig H, editor. Life events and psychiatric disorders: controversial issues. Cambridge, England: Cambridge University Press; 1986. pp. 107–187. [Google Scholar]
- Brown GW, Harris TO. Depression. In: Brown GW, Harris TO, editors. Life events and illness. London: Guilford Press; 1989. pp. 49–93. [Google Scholar]
- Brown GW, Harris TO, Hepworth C. Loss, humiliation and entrapment among women developing depression: a patient and non-patient comparison. Psychological Medicine. 1995;25:7–21. doi: 10.1017/s003329170002804x. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. Child maltreatment. Annual Review of Clinical Psychology. 2005;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- Coffino B. The role of childhood parent figure loss in the etiology of adult depression: findings from a prospective longitudinal study. Attachment and Human Development. 2009;11:445–470. doi: 10.1080/14616730903135993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multivariate regression/correlation analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1983. [Google Scholar]
- Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nature Reviews Neuroscience. 2008;9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dienes KA, Hammen C, Henry RM, Cohen AN, Daley SE. The stress sensitization hypothesis: understanding the course of bipolar disorder. Journal of Affective Disorders. 2006;95:43–49. doi: 10.1016/j.jad.2006.04.009. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP. Inventorying stressful life events as risk factors for psychopathology: toward resolution of the problem of intracategory variability. Psychological Bulletin. 2006;132:477–495. doi: 10.1037/0033-2909.132.3.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer AE, McGuffin P. Humiliation, loss and other types of life events and difficulties: a comparison of depressed subjects, healthy controls and their siblings. Psychological Medicine. 2003;33:1169–1175. doi: 10.1017/s0033291703008419. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer MB, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders, research version, non-patient edition (SCID-I/NP) New York: Biometrics Research Department, New York State Psychiatric Institute; 2002. [Google Scholar]
- Gotlib IH, Kasch KL, Traill S, Joormann J, Arnow BA, Johnson SL. Coherence and specificity of information-processing biases in depression and social phobia. Journal of Abnormal Psychology. 2004a;113:386–398. doi: 10.1037/0021-843X.113.3.386. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Krasnoperova E, Yue DN, Joormann J. Attentional biases for negative interpersonal stimuli in clinical depression. Journal of Abnormal Psychology. 2004b;113:127–135. doi: 10.1037/0021-843X.113.1.121. [DOI] [PubMed] [Google Scholar]
- Grove WM, Andreasen NC, McDonald-Scott P, Keller MB, Shapiro RW. Reliability studies of psychiatric diagnosis: theory and practice. Archives of General Psychiatry. 1981;38:408–413. doi: 10.1001/archpsyc.1981.01780290042004. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hammen C, Henry R, Daley SE. Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology. 2000;68:782–787. [PubMed] [Google Scholar]
- Harkness KL, Alavi N, Monroe SM, Slavich GM, Gotlib IH, Bagby RM. Gender differences in life events prior to onset of major depressive disorder: the moderating effect of age. Journal of Abnormal Psychology. 2010;119:791–803. doi: 10.1037/a0020629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness KL, Bruce AE, Lumley MN. The role of childhood abuse and neglect in the sensitization to stressful life events in adolescent depression. Journal of Abnormal Psychology. 2006;115:730–741. doi: 10.1037/0021-843X.115.4.730. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Archives of General Psychiatry. 2003;60:789–796. doi: 10.1001/archpsyc.60.8.789. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. The causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry. 1999;156:837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn JW, Prescott CA. Childhood sexual abuse, stressful life events and risk for major depression in women. Psychological Medicine. 2004;34:1475–1482. doi: 10.1017/s003329170400265x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, Gardner CO. Stressful life events and previous episodes in the etiology of major depression in women: an evaluation of the “kindling” hypothesis. American Journal of Psychiatry. 2000;157:1243–1251. doi: 10.1176/appi.ajp.157.8.1243. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, Gardner CO. Genetic risk, number of previous depressive episodes, and stressful life events in predicting onset of major depression. American Journal of Psychiatry. 2001;158:582–586. doi: 10.1176/appi.ajp.158.4.582. [DOI] [PubMed] [Google Scholar]
- Kessing LV, Andersen PK, Mortensen PB, Bolwig TG. Recurrence in affective disorder. I. Case register study. British Journal of Psychiatry. 1998;172:23–28. doi: 10.1192/bjp.172.1.23. [DOI] [PubMed] [Google Scholar]
- Kessing LV, Hansen MG, Andersen PK, Angst J. The predictive effect of episodes on the risk of recurrence in depressive and bipolar disorders – a life-long perspective. Acta Psychiatrica Scandinavica. 2004;109:339–344. doi: 10.1046/j.1600-0447.2003.00266.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The effects of stressful life events on depression. Annual Review of Psychology. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biological Psychiatry. 2009;65:732–741. doi: 10.1016/j.biopsych.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM. Modern approaches to conceptualizing and measuring human life stress. Annual Review of Clinical Psychology. 2008;4:33–52. doi: 10.1146/annurev.clinpsy.4.022007.141207. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Harkness KL. Life stress, the “kindling” hypothesis, and the recurrence of depression: considerations from a life stress perspective. Psychological Review. 2005;112:417–445. doi: 10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Rohde P, Seeley JR, Lewinsohn PM. Life events and depression in adolescence: relationship loss as a prospective risk factor for first onset of major depressive disorder. Journal of Abnormal Psychology. 1999;108:606–614. doi: 10.1037//0021-843x.108.4.606. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Slavich GM. Psychological stressors, overview. In: Fink G, editor. Encyclopedia of stress, second edition (Vol. 3) Oxford: Academic Press; 2007. pp. 278–284. [Google Scholar]
- Monroe SM, Slavich GM, Georgiades K. The social environment and life stress in depression. In: Gotlib IH, Hammen CL, editors. Handbook of depression, second edition. New York: Guilford Press; 2009. pp. 340–360. [Google Scholar]
- Monroe SM, Slavich GM, Torres LD, Gotlib IH. Major life events and major chronic difficulties are differentially associated with history of major depression. Journal of Abnormal Psychology. 2007a;116:116–124. doi: 10.1037/0021-843X.116.1.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM, Slavich GM, Torres LD, Gotlib IH. Severe life events predict specific patterns of change in cognitive biases in major depression. Psychological Medicine. 2007b;37:863–871. doi: 10.1017/S0033291707000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris MC, Ciesla JA, Garber J. A prospective study of stress autonomy versus stress sensitization in adolescents at varied risk for depression. Journal of Abnormal Psychology. 2010;119:341–354. doi: 10.1037/a0019036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz RF, Cuijpers P, Smit F, Barrera AZ, Leykin Y. Prevention of major depression. Annual Review of Clinical Psychology. 2010;6:181–212. doi: 10.1146/annurev-clinpsy-033109-132040. [DOI] [PubMed] [Google Scholar]
- Muscatell KA, Slavich GM, Monroe SM, Gotlib IH. Stressful life events, chronic difficulties, and the symptoms of clinical depression. Journal of Nervous and Mental Disease. 2009;197:154–160. doi: 10.1097/NMD.0b013e318199f77b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in depression. Current Directions in Psychological Science. 2001;10:173–176. [Google Scholar]
- Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. American Journal of Psychiatry. 1992;149:999–1010. doi: 10.1176/ajp.149.8.999. [DOI] [PubMed] [Google Scholar]
- Post RM. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. Neuroscience and Biobehavioral Reviews. 2007;31:858–873. doi: 10.1016/j.neubiorev.2007.04.003. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Flynn M. Childhood adversity and youth depression: influence of gender and pubertal status. Development and Psychopathology. 2007;19:497–521. doi: 10.1017/S0954579407070241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams JM, Teasdale JD, Gemar M. A cognitive science perspective on kindling and episode sensitization in recurrent affective disorders. Psychological Medicine. 1996;26:371–380. doi: 10.1017/s0033291700034760. [DOI] [PubMed] [Google Scholar]
- Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychological Bulletin. 2004;130:601–630. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, O’Donovan A, Epel ES, Kemeny ME. Black sheep get the blues: a psychobiological model of social rejection and depression. Neuroscience and Biobehavioral Reviews. 2010a;35:39–45. doi: 10.1016/j.neubiorev.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, Thornton T, Torres LD, Monroe SM, Gotlib IH. Targeted rejection predicts hastened onset of major depression. Journal of Social and Clinical Psychology. 2009;28:223–243. doi: 10.1521/jscp.2009.28.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, Way BM, Eisenberger NI, Taylor SE. Neural sensitivity to social rejection is associated with inflammatory responses to social stress. Proceedings of the National Academy of Sciences of the United States of America. 2010b;107:14817–14822. doi: 10.1073/pnas.1009164107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit F, Beekman A, Cuijpers P, de Graaf R, Vollebergh W. Selecting key variables for depression prevention: results from a population-based prospective epidemiological study. Journal of Affective Disorders. 2004;81:241–249. doi: 10.1016/j.jad.2003.08.007. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Hamer M, Chida Y. The effects of acute psychological stress on circulating inflammatory factors in humans: a review and meta-analysis. Brain, Behavior, and Immunity. 2007;21:901–912. doi: 10.1016/j.bbi.2007.03.011. [DOI] [PubMed] [Google Scholar]
- Stroud CB, Davila J, Hammen C, Vrshek-Schallhorn S. Severe and nonsevere events in first onsets versus recurrences of depression: evidence for stress sensitization. Journal of Abnormal Psychology. 2011;120:142–154. doi: 10.1037/a0021659. [DOI] [PubMed] [Google Scholar]
- Stroud CB, Davila J, Moyer A. The relationship between stress and depression in first onsets versus recurrences: a meta-analytic review. Journal of Abnormal Psychology. 2008;117:206–213. doi: 10.1037/0021-843X.117.1.206. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Seeman TE. Psychosocial resources and the SES-health relationship. Annals of the New York Academy of Sciences. 1999;896:210–225. doi: 10.1111/j.1749-6632.1999.tb08117.x. [DOI] [PubMed] [Google Scholar]
- Uebersax JS. A generalized kappa coefficient. Educational and Psychological Measurement. 1982;42:181–183. [Google Scholar]
- Wichers M, Peeters F, Geschwind N, Jacobs N, Simons CJ, Derom C, Thiery E, Delespaul PH, van Os J. Unveiling patterns of affective responses in daily life may improve outcome prediction in depression: a momentary assessment study. Journal of Affective Disorders. 2010;124:191–195. doi: 10.1016/j.jad.2009.11.010. [DOI] [PubMed] [Google Scholar]
- Wichers M, Schrijvers D, Geschwind N, Jacobs N, Myin-Germeys I, Thiery E, Derom C, Sabbe B, Peeters F, Delespaul P, van Os J. Mechanisms of gene-environment interactions in depression: evidence that genes potentiate multiple sources of adversity. Psychological Medicine. 2009;39:1077–1086. doi: 10.1017/S0033291708004388. [DOI] [PubMed] [Google Scholar]
- Wolkowitz OM, Epel ES, Reus VI, Mellon SH. Depression gets old fast: do stress and depression accelerate cell aging? Depression and Anxiety. 2010;27:327–338. doi: 10.1002/da.20686. [DOI] [PubMed] [Google Scholar]
- Yirmiya R, Pollak Y, Morag M, Reichenberg A, Barak O, Avitsur R, Shavit Y, Ovadia H, Weidenfeld J, Morag A, Newman ME, Pollmacher T. Illness, cytokines, and depression. Annals of the New York Academy of Sciences. 2000;917:478–487. doi: 10.1111/j.1749-6632.2000.tb05412.x. [DOI] [PubMed] [Google Scholar]
- Young JE. Cognitive therapy for personality disorders: a schema-focused approach. Sarasota, FL: Professional Resource Press; 1999. [Google Scholar]