Abstract
A 14-year-old male, diagnosed case of type 1 diabetes mellitus since 1 year, presented with uncontrolled blood glucose levels, non-compliance with insulin therapy and recurrent admissions with diabetic ketoacidosis. His blood glucose levels were difficult to control with wide fluctuations in insulin requirement. He had absent secondary sexual characteristics and hepatomegaly. Liver biopsy showed macrovesicularsteatosis without fibrosis or inflammation. Many glycogenated nuclei were present. He was started on intensive insulin therapy, whereby he showed subsequent regression of hepatomegaly and onset of pubertal spurt.
Background
This case reflects the occurrence of a rare syndrome associated with poorly controlled type 1 diabetes mellitus (T1DM). In the present era of intensive insulin therapy, with availability of low cost and subsidised treatment, and wider outreach of nutritional programs, occurrence of mauriac syndrome may be extremely rare. However, every young patient presenting with T1DM on insulin treatment should be closely monitored for adequacy of diet and treatment.
Case presentation
A 14-year-old student, hailing from Northern India, second of the two siblings, presented to the emergency department with a history of weight loss, easy fatigability and abdominal discomfort for past 1 month. He was diagnosed to have T1DM and was on human insulin (30/70) 16 units–8 units regimen for past 1 year. He gave a history of non-compliance with insulin therapy due to financial constraints. Old records revealed admissions in emergency department for diabetic ketoacidosis (DKA) on multiple occasions. He belonged to low socioeconomic strata. His father is manual labourer and the only earning member in the family and the mother is a housewife. There was no history of diabetes mellitus in the family. On admission, he was conscious and fully oriented. He had a pulse rate of 100/min, blood pressure of 110/70 mm Hg (no postural drop) and a respiratory rate of 23/min. He was 130 cm tall and his weight was 32 kg, body mass index being 18.93 (between 5th and 85th percentile). He had a non-tender, firm, non-pulsatile liver enlargement of 6 cm below subcostal margin. Secondary sexual characters were absent, Tanner stage being 1.
Investigations
His random blood glucose level was 458 mg % with urine sugar 3+ and urine ketone small. Arterial blood gases showed pH of 7.34 and bicarbonate 18 meq/l. Liver function tests, renal function test, serum iron studies, thyroid function test, lipid profile, urine examination and routine chest skiagrams were within normal limits. Haemoglobin A1c was 8.5%.
Abdominal ultrasound showed hepatomegaly with coarse echotexture. Portal vein was normal.
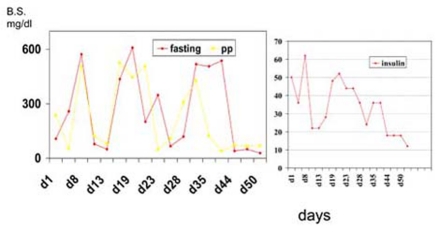
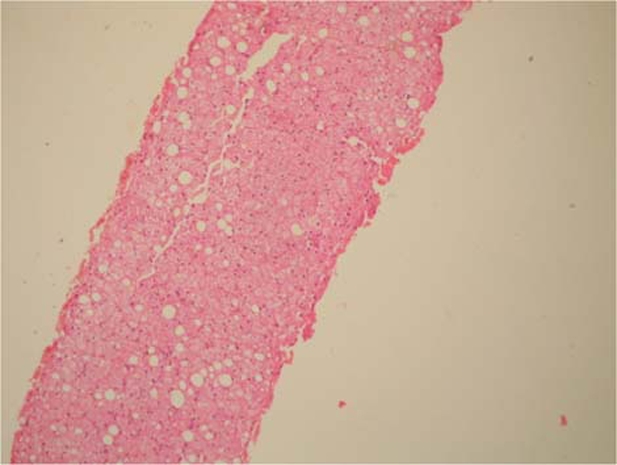
Liver biopsy was done (figures 1 and 2) which revealed macrovascularsteatosis involving 20% of hepatocytes. Hepatocytes showed ballooning. Glycogenated nuclei were present. No evidence of inflammation or fibrosis was seen; features consistent with diabetic changes.
Figure 1.
Low magnification view of liver biopsy sample showing steatosis.
Figure 2.
Higher magnification view of liver biopsy sample showing macrovesicularsteatosis and glycogenated nuclei. Note the absence of fibrosis.
Differential diagnosis
-
▶
Haemochromatosis
-
▶
Cryptogenic cirrhosis.
Treatment
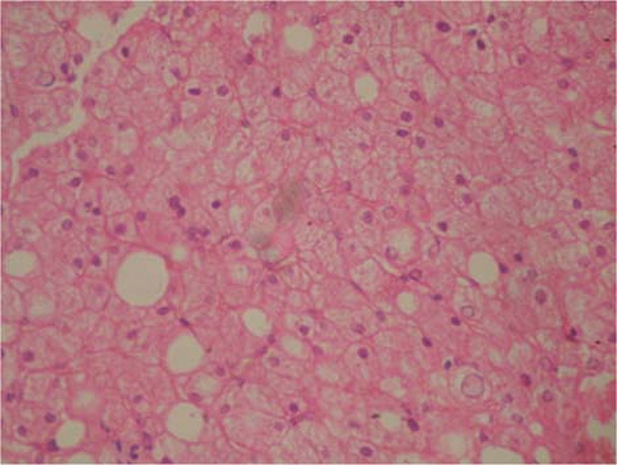
He was started on intensive insulin therapy. His treatment was monitored frequently. Fluctuations in the insulin requirement and blood glucose levels (figure 3) with brisk hypoglycaemic responses to increases in insulin dosage were noted.
Figure 3.
Graphs showing fluctuations in the blood glucose levels and insulin requirement during treatment.
By day 50 of admission, his sugar levels and insulin dosage were regularised.
Outcome and follow-up
He was discharged on insulin therapy with advice on home glucose monitoring and diabetic diet. With frequent reviews and intensive insulin therapy coupled with balanced adequate diet, he showed improvement with regression of liver enlargement and signs of puberty during the follow-up, which was over 8 months.
Discussion
Mauriac syndrome, a rare complication associated with T1DM, is attributed to poor insulin compliance and glycaemic control along with inadequate diet.1 Originally described as a triad of dwarfism, obesity and hepatomegaly,2 mauriac syndrome has variously been reported to have raised serum transaminases, malnutrition, growth failure and cushingoid features.1 3 The cause of growth failure in mauriac syndrome is not known; presumably it is related to the poor metabolic control of diabetes.3 Low levels of insulin like growth factor 1 have been implicated, which was attributed to low-dose insulin over a long time and delayed puberty.4 Patients with mauriac syndrome can have normal body mass index.5 These patients often have history of recurrent admissions with DKA or asymptomatic hyperglycaemia reflecting poor glycaemic control and low insulin levels. The same was evident in our patient. Joint contractures, osteopaenia, hyperlipidaemia with hypertriglyceridaemia and diabetic microvascular complications such as retinopathy and albuminuria, may be seen in such individuals.4 5 These were absent in our patient may be due to early presentation.
Since the syndrome has, at its root, poorly controlled diabetes, most of its manifestations may revert/be arrested with timely intervention with intensive insulin therapy and adequate nutritious diet.6 Our patient had hepatomegaly with biopsy demonstrating steatosis as well as glycogen deposition consistent with liver involvement in mauriac syndrome, although such findings can vary in presentation.7
Learning points.
-
▶
Occurrence of mauriac syndrome may be extremely rare, but possible especially in the developing countries and in patients belonging to lower socioeconomic strata.
-
▶
Ultrasound examination and liver biopsy is prudent in cases with unexplained hepatomegaly.
-
▶
Every young/adolescent patient presenting with T1DM on insulin treatment should be closely monitored with home glucose monitoring for adequacy of treatment and diet.
-
▶
Regular monitoring for growth failure and diabetes related complications should be mandatory.
-
▶
With close monitoring, a rare but disabling syndrome can be averted in this subset of population.
Acknowledgments
The authors thank Dr Amrapurkar A, Professor, Department of Pathology, BYL Nair Charitable Hospital and TN Medical College, Mumbai, for processing and reporting the liver biopsy specimen.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Mahesh S, Karp RJ, Castells S, et al. Mauriac syndrome in a 3-year-old boy. Endocr Pract 2007;13:63–6 [DOI] [PubMed] [Google Scholar]
- 2.Mauriac P. Grosventre, hepatomegalie, troubles de la croissance chez les enfantsdiabetques, traits depuisplusieursanbnees par l’insuline. Gaz Hebd Sci Med Bordeux 1930;51:402 [Google Scholar]
- 3.Kim MS, Quintos JB. Mauriac syndrome: growth failure and type 1 diabetes mellitus. Pediatr Endocrinol Rev 2008;5 Suppl 4:989–93 [PubMed] [Google Scholar]
- 4.Simsek E. Insulin-like growth factor (IGF-I) in Mauriac syndrome or diabetic dwarfism. Turk J Med Sci 2002;32:421–4 [Google Scholar]
- 5.Norouzy A, Lawrence I. Mauriac syndrome: a case report. Endocrine Abstracts 2008;15:93 [Google Scholar]
- 6.Kim SY, Shin CH, Ha S, et al. A case of Mauriac syndrome. J Korean Pediatr Soc 1996:39:1020–4 [Google Scholar]
- 7.Lorenz G. Bioptical liver changes in Mauriac syndrome. Zentralbl Allg Pathol 1981;125:364–8 [PubMed] [Google Scholar]