Abstract
Purpose
Prime Time, a youth development intervention, aims to reduce pregnancy risk among adolescent girls seeking clinic services who are at high risk for pregnancy. This paper examines sexual risk behaviors and hypothesized psychosocial mediators after 12 months of the Prime Time intervention.
Methods
Randomized controlled trial with 253 girls ages 13-17 years meeting specified risk criteria. Intervention participants were involved in Prime Time programming plus usual clinic services for 18 months, control participants received usual clinic services. The intervention employed a combination of case management and peer leadership programs. Participants in this interim outcomes study completed self-report surveys at baseline and 12 months following enrollment. Surveys assessed sexual risk behaviors and psychosocial factors targeted for change by Prime Time.
Results
At the 12-month interim, the intervention group reported more consistent use of condoms, hormonal contraception and dual contraceptive methods with their most recent partner than did the control group. The intervention group also reported greater stress management skills with trends towards higher levels of pro-social connectedness at school and with family. No between-group differences were noted in psychosocial measures specific to sex and contraceptive use.
Conclusions
Preventing early pregnancy among high-risk adolescents requires multifaceted, sustained approaches. An important research focus involves testing youth development interventions offered through clinic settings, where access to high-risk adolescents is plentiful and few efforts have emphasized a dual approach of building protective factors while addressing risk. Findings suggest that youth development interventions through clinic settings hold promise in reducing pregnancy risk among high-risk youth.
Introduction
Adolescent pregnancy and childbearing continue to be major social and public health issues in the U.S. Teen pregnancy and birth rates declined dramatically between 1991 and 2005 – each by about one-third [1,2]. Following this decline, the teen birth rate increased 5% between 2005 and 2007 [3]. Despite overall declines since the early 1990's, nearly one-third of young women become pregnant at least once by age 20. The U.S. continues to have the highest rates of teen pregnancy and birth among industrialized nations [4], with rates being disproportionately high among young women of color [1-3].
Adolescent childbearing has adverse outcomes for teen mothers, their children, and society. When adolescents give birth, their future prospects decline. They become less likely to finish high school and attend college and more likely to be single parents and have large families [5]. Being the child of an adolescent parent carries adverse social and health risks including delays in cognitive development, behavior problems, school failure, and increased likelihood of adolescent childbearing [5]. In 2004, teen childbearing cost U.S. taxpayers at least $9.1 billion in lost tax revenues, public assistance, health care, child welfare and criminal justice systems [5].
Among adolescents at high risk for pregnancy, research suggests that preventive interventions must be multifaceted, intensive and sustained to have substantive effects on pregnancy risk behaviors [4,6]. Indeed, intensive and sustained programs that explicitly address reproductive health and foster positive youth development have reduced pregnancy risk among vulnerable youth [4,6]. Such programs address a broad array of sexual (e.g., effective contraceptive use skills) and non-sexual determinants (e.g., pro-social attachments to family and school) of pregnancy risk behaviors.
Youth development programs tap into the power of protective factors -- within adolescents and their environments -- to counteract risk [7]. Effective youth development programs with vulnerable populations have included case management and peer leadership components [8,9]. One-on-one case management assures adequate attention to the diverse psychosocial issues confronting high-risk youth. Because peer influence is a central theme of adolescence, structuring pro-social peer influence may be critical to the success of prevention efforts, particularly when young people themselves take on leadership roles [10].
A 2009 report of the National Research Council and the Institute of Medicine noted that the health needs of contemporary adolescents increasingly involve problems resulting from risk behaviors [11]. This report concluded that to improve adolescent health services, priority must be given to integrating prevention and youth development strategies, particularly for groups most vulnerable to negative health outcomes. A major research challenge posed by the NRC/IOM report was the need for rigorous evaluation of health services utilizing a youth development framework. A critical intervention question that remains largely untested is whether adolescent health services grounded in a youth development frame can reduce risk behaviors linked to teen pregnancy.
Prime Time is a multi-component youth development intervention for adolescent girls at high risk for pregnancy. Designed for use by clinics, this intervention aims to reduce precursors of teen pregnancy including sexual risk behaviors, violence involvement and school disconnection. The intervention, involving one-on-one case management and peer leadership programming over an 18-month period, targets specific environmental, personal and behavioral mediators of pregnancy risk [12]. A Prime Time intervention trial is ongoing in school and community-based clinics in Minneapolis and Saint Paul, Minnesota. This paper examines sexual risk behaviors and hypothesized environmental, personal and behavioral mediators of these behaviors after 12 months of the Prime Time intervention.
Methods
Participants
The sample consisted of sexually active 13-17 year old girls meeting ≥1 of the following risk criteria: clinic visits involving negative pregnancy test [13] or treatment for sexually transmitted infection [14]; young age [4]; high-risk sexual and contraceptive behaviors [4]; aggressive and violent behaviors [15,4]; behaviors indicating school disconnection [4]. Behavioral risk criteria were assessed through a self-report screening tool, 20 items previously linked with sexual risk behaviors in clinic samples or identified by content experts as valid indicators of risk [16,12]. Girls who could not understand consent materials, were married, pregnant or had given birth were excluded from the study. University and participating clinics' IRBs approved all study protocols.
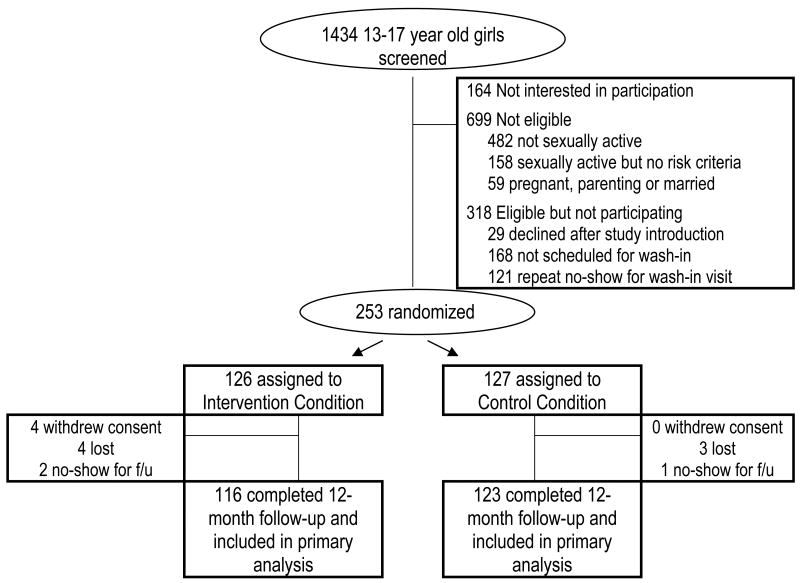
From April 2007 through October 2008, trained study staff screened 1434 girls at four school and community clinics (Figure 1). Of these, 571 sexually active girls who met ≥1 study risk criteria were invited to participate. Enrollment involved two clinic visits, a strategy to minimize attrition [17] that can be particularly problematic in high-risk, mobile youth populations [18]. At Visit#1, staff identified study-eligible girls and invited them to return for a second visit within two weeks. At Visit#2, girls signed an informed consent statement, provided baseline survey data and were randomized into study conditions. A total of 253 adolescents agreed to study participation, completed baseline data collection and randomization.
Figure 1. Flow of Prime Time Study Participants.
Lost participants were those who were unable to be contacted. No-show participants were contacted and scheduled for a follow-up survey but did not complete the survey.
Demographics and risk behavior items on the screening tool (completed at Visit#1) were used to compare participants (n=253) to eligible girls who did not enroll (n=318). Participants were similar to eligible non-participants on a number of indicators including age, race/ethnicity, public assistance, school enrollment, school mobility, skipping school, violence involvement, number of sex partners and contraceptive use in the past 6 months. Participants were more likely than eligible non-participants to be living with one parent (64% vs. 52%; [χ2(2, N=545)=19.09, p=0.015]).
The sample's baseline demographic characteristics and sexual risk indicators are summarized in Table 1. Intervention and control groups were equivalent on these descriptors.
Table 1. Baseline Characteristics of Prime Time Participants by Intervention Condition*.
| Intervention (n = 126) |
Control (n = 127) |
p-value | |
|---|---|---|---|
| Demographics | |||
| Age, mean (se) | 15.7 (0.07) | 15.49 (0.21) | 0.334 |
| 13 | 1% | 2% | |
| 14 | 14% | 22% | |
| 15 | 29% | 24% | |
| 16 | 27% | 28% | |
| 17 | 29% | 24% | |
| Race/Ethnicitya | 0.118 | ||
| American Indian/Native American | 3% | 2% | |
| Asian/Asian American/Pacific Islander | 10% | 13% | |
| Black/African/African American | 45% | 38% | |
| Hispanic /Latina | 17% | 8% | |
| White/European American | 6% | 16% | |
| Mixed/Multiple | 19% | 23% | |
| # Adults/guardians in homeb | 0.152 | ||
| No adult guardian | 4% | 2% | |
| 1 adult guardian | 46% | 44% | |
| 2 adult guardians | 38% | 46% | |
| Other arrangements | 12% | 8% | |
| # Places lived, past 6 months | 0.811 | ||
| 1 place | 58% | 61% | |
| 2 places | 25% | 23% | |
| 3 or more places | 17% | 16% | |
| Receipt of public assistance, past yearc | 0.343 | ||
| No | 43% | 51% | |
| Yes | 33% | 32% | |
| Unsure | 24% | 17% | |
| Currently enrolled in school (% yes) | 94% | 96% | 0.096 |
| Ever suspended from school (% yes) | 65% | 75% | 0.138 |
| Sexual behaviors | |||
| # Male sex partners, past 6 months, mean (se) | 1.54 (0.21) | 1.76 (0.07) | 0.289 |
| 1 | 65% | 57% | |
| 2 | 26% | 24% | |
| 3 | 2% | 9% | |
| 4 | 5% | 5% | |
| 5 or more | 2% | 5% | |
| Condom use, past 6 months (n=251) | 0.427 | ||
| Never | 14% | 9% | |
| ≤ ½ time | 32% | 33% | |
| > ½ time | 23% | 26% | |
| Every time | 31% | 32% | |
| Hormonal contraceptive use, past 6 months | |||
| No use | 36% | 45% | 0.185 |
| 1 month | 21% | 7% | |
| 2 months | 12% | 14% | |
| 3 Months | 5% | 8% | |
| 4 Months | 9% | 3% | |
| 5 Months | 1% | 6% | |
| 6 Months | 6% | 9% | |
| 7 Months | 10% | 8% | |
Data are expressed as % of participants unless otherwise noted
Mutually exclusive race categories; participants were allowed to select more than one category
Adults/guardian may include biological or adoptive parent, step-parent, foster parent, grandparent, other guardian
Public assistance includes welfare payments, M-FIP, public assistance, or food stamps
Intervention Components
Social cognitive theory [19], the resilience paradigm [7], and findings from the Prime Time pilot study [20] guided the Prime Time intervention. Intervention strategies sought change in specific environmental, personal and behavioral attributes associated with pregnancy risk [4,7,12].
Case managers experienced working with urban teens from diverse cultural backgrounds led all intervention programming. Details regarding case managers' backgrounds, training and supervision are found elsewhere [21]. Each intervention component is summarized below.
Case Management
The overall goal of Prime Time case management was to establish a trusting, consistent relationship in which an adolescent and case manager could work together to address environmental, personal and behavioral attributes targeted by this intervention. Case managers attempted monthly visits with each intervention participant over the 18-month intervention period. Participants received $10 for each monthly visit. One-on-one visits focused on core topics of emotional skills, healthy relationships, responsible sexual behaviors, and positive family, school and community involvement. As a client-centered approach, the capacities, interests, and needs of individual participants determined topics and strategies employed during any particular case management visit. With each participant actively involved in case management, all core topics were addressed over each 6-month interval.
Peer Leadership Components
Designed to complement one-on-one case management, youth leadership groups provided hands-on skill-building experiences. The sequence of peer educator training followed by service learning programming was designed to foster development of pro-social interaction skills and supportive peer relationships among a vulnerable group of teens, many of whom had experienced disruptions in the development of supportive peer relationships [22]. Peer educator training activities addressed basic skills to function constructively in a group. Service learning group activities expanded on skills for group involvement
Peer Educator Training and Employment: Just in Time
The purpose of Just In Time was to provide opportunities for positive peer, school and community involvement by engaging participants as peer health educators. Just In Time peer educator training used a standardized 15-session curriculum addressing communication skills, stress management skills, conflict resolution skills, expectations and skills for healthy relationships, understanding social influences on sexual behaviors, sexual decision-making and contraceptive use skills. Through weekly homework activities, participants explored Just In Time topics with an adult family member. Beginning with their first training session, girls were instructed to reach and teach others in their lives. A peer educator contact was defined as at least a 15-minute conversation on a topic covered in training. Girls received $5 for each documented contact, for up to 50 contacts during the training.
After completing the Just In Time training curriculum, girls engaged in a group teaching practicum with an existing group of students. During this 7-session practicum, groups chose a topic from the Just In Time curriculum to teach, developed a lesson plan, practiced their teaching skills, taught a group session, reflected and adjusted their lesson plan, and taught a second group session.
Service Learning: It's Our Time
The purpose of It's Our Time was to expand participants' social-emotional skills and their real-world experience in civic engagement and leadership. It's Our Time groups followed a standardized curriculum that included core elements of service learning: preparation, action, reflection and celebration [23]. An initial It's Our Time unit focused on building group cohesion and identifying participants' leadership skills. During a second unit, participants explored community needs, assets, and potential service projects. Groups implemented their service projects during the third unit. Each implementation session included a group reflection activity highlighting the impact of service on recipients and relating service experiences to girls' leadership skills and civic engagement. In a final session, groups celebrated their It's Our Time accomplishments.
It's Our Time sessions included homework assignments such as journaling about service experiences. Girls were given small rewards ($2-3 value) for completing assignments.
Evaluation
All study participants completed an A-CASI survey at baseline and 12 months following enrollment. Trained research staff conducted evaluation visits, orienting teens to the A-CASI survey with non-sensitive practice items. Participants were paid $25 for completing each survey.
Participants
Of 253 participants at baseline, 94.5% (n=239) completed a 12-month follow-up survey. Fourteen were lost to follow-up at the 12 months, 10 of whom were in the intervention condition. There were no significant differences in baseline indicators (age, ethnicity, public assistance, contraceptive use, number of sex partners) between intervention and control groups completing the 12-month survey. An attrition analysis identified very few significant differences in baseline characteristics between those lost to follow-up and those completing the 12-month assessment. Compared to the 12-month sample, girls lost to follow-up were less likely to be enrolled in school at baseline (86% vs. 95%; p<0.01) and less likely to have used emergency contraception with their most recent sex partner (no use vs. mean use=0.23 times; p<0.01).
Measures
The participant survey assessed sexual risk behaviors and psychosocial factors targeted for change by Prime Time.
Two primary outcome measures were the focus of this analysis: contraceptive use consistency with a participant's most recent sex partner, and number of sex partners in the past six months. Previous research has established the reliability of these measures among sexually active adolescent girls [24].
Contraceptive use consistency, most recent partner
Participants identified which of the past six months they had sex and in which of these months they used a hormonal method (birth control pills, injection, patch, ring), dual methods (hormonal method plus condoms) or condoms every/most times they had sex with their most recent male partner. For measures of condom, hormonal and dual method use consistency, we tallied the number of months a participant reported using condoms every/most times they had sex, a hormonal method, or dual methods, respectively (range: 0-7 months, including current month).
Number of male sex partners
Participants indicated the number of males with whom they had vaginal sex in the past six months.
Psychosocial outcomes, environmental, personal and behavioral attributes repeatedly associated with adolescent sexual and contraceptive behaviors [4] and thus targeted for change by the intervention, were also examined. These variables and their measurement properties are presented in Table 2.
Table 2. Measurement Information for Psychosocial Variables.
| Construct | # of Items | Sample Item | Response Format, Measure Coding | Internal Consistency |
|---|---|---|---|---|
| Environmental Attributes | ||||
| Social Connectedness | ||||
| Family connectedness | 5 | My family cares about me. | 4-point response (0 = not at all to 3 = a lot) | α=0.90 |
| School connectedness | 3 | I feel like I belong at my school. | 4-point response (0 = never or seldom to 3 = very often) | α=0.63 |
| Teacher connectedness | 6 | My teachers respect me. | 4-point response (0 = none to 3 = a lot) | α=0.87 |
| Perceived Norms re Contraception | ||||
| Perceived partner desire to use contraceptiona | 1 | How did [most recent partner] feel about using condoms or other birth control when the two of you had sex? | 5-point response (0 = He did not want us to use to 4 = He always wanted us to use) | NA |
| Measure dichotomized, contrasting girls who reported their partner always wanted to use contraception with others | ||||
| Personal Attributes | ||||
| Sexual Attitudes & Beliefs | ||||
| Desire to use contraception with partnera | 1 | How did you feel about using condoms or other birth control when you had sex with [most recent partner]? | 4-point response (0 = I did not want us to use to 3 = I always wanted us to use) | NA |
| Measure dichotomized, contrasting girls who always wanted to use contraception with others | ||||
| Beliefs supporting birth control use | 5 | Using birth control makes me feel responsible. | 4-point response (0 = strongly disagree to 3 = strongly agree) | α=0.82 |
| Perceived pregnancy consequences | 6 | Getting pregnant would force me to grow up too fast. | 4-point response (0 = strongly disagree to 3 = strongly agree) | α=0.77 |
| Behavioral Attributes | ||||
| Social-Emotional Intelligence | ||||
| Stress management skillsb | 8 | When I get angry, I act without thinking. | 4-point response (0 = never or seldom to 3 = very often) | α=0.86 |
| Interpersonal skillsb | 7 | I am able to respect others. | 4-point response (0 = never or seldom to 3 = very often) | α=0.81 |
| Intrapersonal skillsb | 6 | It is easy to tell people how I feel. | 4-point response (0 = never or seldom to 3 = very often) | α=0.79 |
| Sexual Self-Efficacy & Skills | ||||
| Communication about sexual risk | 7 | When did you and [most recent partner] talk about how to keep from getting pregnant? | 3-point response (0 = we never talked about this; 1 = we talked about this after we had sex; 2 = we talked about it before we had sex) | α=0.74 |
| Sex refusal self-efficacy | 4 | Imagine that you met someone at a party who wants to have sex with you. Even though you are very attracted to each other, you don't think you are ready to have sex. How sure are you that you could keep from having sex? | 4-point response (0 = not sure to 3 = really sure) | α=0.81 |
| Condom use self-efficacy | 5 | It would be easy to tell [most recent partner] that I wanted to use a condom | 4-point response (0 = strongly disagree to 3 = strongly agree) | α=0.67 |
Dichotomous version of measure used in analyses.
From Bar-On Emotional Quotient Inventory: Youth Version [40].
Statistical Analyses
Analyses utilized an intent-to-treat design in which participants were analyzed in their original assigned study condition. To summarize major characteristics of the sample, baseline descriptive statistics are presented by study condition. Differences between intervention and control groups were assessed using t-tests for continuous variables and chi-square analyses for categorical variables. Bivariate analyses were conducted in STATA Version 9.2 using “svy” commands to adjust for clustering of participants within clinics.
Interim effectiveness of the intervention was evaluated from baseline to 12 months using generalized estimating equation (GEE) regression models in SAS Version 9.2. GEE models allow for flexibility in modeling variables that are non-normally distributed (i.e., using logistic, Poisson and negative binomial regression), adjusting standard errors for intercorrelations between participants from the same clinic [25,26,27]. Intracluster coefficients for outcome variables ranged from 0.00-0.05.
Each 12-month outcome variable was regressed upon study condition (intervention vs. control) and the corresponding baseline measure of that outcome (with the exception of perceived partner desire to use contraception). Models of partner-specific outcomes controlled for a dichotomous indicator of whether or not the most recent sex partner at 12 months was the same male as reported at baseline. Log-linear count models of consistent condom, hormone, and dual method use included an “offset” variable to adjust for the varying lengths of exposure to pregnancy risk, in this case, number of months of being sexually active with one's most recent partner [28]. Results of the GEE models are presented including valid sample sizes for each model, adjusted odds ratios for dichotomous and count outcomes, adjusted mean differences for outcomes treated as normally distributed, corresponding p-values, and 95% confidence intervals around the adjusted estimates. It is important to note that GEE models are “marginal” or “population averaged models” [26]. Thus, model estimates should be interpreted as odds or means applicable to an “average” participant in this population of high-risk adolescent girls.
Results
Intervention Engagement
Twelve months into the intervention, participation in case management was high, with 84.9% of girls in the intervention condition participating in ≥3 case management visits during their first year. The median number of case management visits was 9. Twelve months after study enrollment, 60.3% of participants had completed ≥3 peer educator training sessions, while 25.4% had gone on to complete ≥3 service learning sessions. Of girls actively involved in case management (i.e., ≥3 visits), 71% had completed ≥3 peer educator training sessions. Among girls involved in peer educator training, the median number of training sessions attended by 12 months was 16.5 and the median number of peer educator contacts made was 47.5. Among girls involved with service learning groups, the median number of sessions attended was 9.
Twelve Month Interim Outcomes
Table 3 presents interim findings from intent-to-treat analyses. Examining sexual behaviors, intervention participants were more likely to report consistent condom use with their most recent partner than were control participants (adjusted means, intervention, 0.96 of 7 months vs. control, 0.66 of 7 months; adjusted OR:1.45; 95% CI:1.26-1.67; p=.00). Intervention participants also reported more consistent hormonal use (adjusted means, intervention, 4.27 of 7 months vs. control, 2.91 of 7 months; adjusted OR:1.46; 95% CI:1.13-1.89; p=.00) and more consistent dual method use (adjusted means, intervention, 0.83 of 7 months vs. control, 0.53 of 7 months; adjusted OR:1.58; 95% CI:1.03-2.43; p=.04). No between-group differences were observed in number of sex partners in the past six months.
Table 3. Effects of Prime Time Intervention on Behavioral and Psychosocial Outcomes at 12 Months Adjusted for Baseline Values.
| Variable | Sample Size | Intervention % or Mean Score | Control % or Mean Score | Mean Difference or OR (95% CI)+ | P-Value |
|---|---|---|---|---|---|
| Sexual Behavior Outcomes | |||||
| Condom use consistency ++, a | 207 | 0.96 | 0.66 | AOR=1.45 (1.26, 1.67) | 0.00 |
| Hormonal use consistency ++, b | 206 | 4.27 | 2.91 | AOR=1.46 (1.13, 1.89) | 0.00 |
| Dual method use consistency++,b | 205 | 0.83 | 0.53 | AOR=1.58 (1.03, 2.43) | 0.01 |
| # of male sex partners, past 6 months +++, c | 236 | 1.55 | 1.44 | AOR=1.08 (0.89, 1.31) | 0.44 |
| Psychosocial Outcomes | |||||
| Environmental Attributes | |||||
| Social Connectedness | |||||
| Family connectedness +++, d | 237 | 2.04 | 1.93 | 0.12 (-0.01, 0.26) | 0.08 |
| School connectedness +++, d | 221 | 2.15 | 1.99 | 0.16 (-0.01, 0.33) | 0.06 |
| Teacher connectedness +++, d | 221 | 2.25 | 2.16 | 0.09 (-0.05, 0.23) | 0.24 |
| Perceived Norms re Contraception | |||||
| Perceived partner desire to use contraception∷,e | 216 | 50.09% | 40.07% | AOR=1.5 (0.88, 2.56) | 0.13 |
| Personal Attributes | |||||
| Sexual Attitudes & Beliefs | |||||
| Desire to use contraception with partner +++,∷,f | 204 | 64.48% | 53.59% | AOR=1.62 (0.81, 3.27) | 0.17 |
| Beliefs supporting birth control use +++, g | 214 | 2.20 | 2.16 | 0.04 (-0.10, 0.18) | 0.54 |
| Perceived pregnancy consequences +++, g | 220 | 1.81 | 1.77 | 0.04 (-0.07, 0.15) | 0.48 |
| Behavioral Attributes | |||||
| Social-Emotional Intelligence | |||||
| Stress management skills +++, d | 222 | 1.79 | 1.69 | 0.11 (0.05, 0.23) | 0.00 |
| Interpersonal skills +++, d | 222 | 2.15 | 2.14 | 0.01 (-0.01, 0.04) | 0.26 |
| Intrapersonal skills +++, d | 222 | 1.49 | 1.50 | -0.01(-0.21, 0.18) | 0.91 |
| Sexual Self-Efficacy & Skills | |||||
| Sexual risk communication with partner++, h | 212 | 1.21 | 1.20 | 0.01 (-0.13, 0.15) | 0.95 |
| Sex refusal self-efficacy +++, d | 229 | 2.49 | 2.34 | 0.15 (-0.04, 0.33) | 0.12 |
| Condom use self-efficacy ++, d | 209 | 2.18 | 2.09 | 0.09 (-0.2, 0.39) | 0.57 |
Difference between intervention and control groups.
Regression model adjusted for baseline measure of outcome, change in most recent sex partner from baseline to 12-month assessment, within-clinic clustering.
Regression model adjusted for baseline measure of outcome, within-clinic clustering.
Logistic regression used with this dichotomous outcome.
Count of using a condom every/most of the time ranged from 0 -7 months. Variable adjusted for number of months participant had sex with most recent partner.
Count ranged from 0-7 months. Variable adjusted for number of months participant had sex with most recent partner.
Values ranged from 0-10 partners in the past 6 months.
Scores ranged from 0 (low) to 3 (high).
Percent reporting most recent sex partner always wanted to use contraception.
Percent reporting always wanting to use contraception with most recent sex partner.
Scores ranged from 0 (none) to 3 (many).
Scores ranged from 0 (no communication about sexual risk with most recent sex partner), 1 (communication with partner after having sex), 2 (communication with partner before having sex).
Also in Table 3 are interim intervention effects on psychosocial mediators. Intervention participants reported significantly greater stress management skills than did control participants (p=.00). Intervention participants reported trends towards higher levels of family connectedness (p=.08) and school connectedness (p=.06). No between-group differences were found in measures of perceived norms, attitudes and beliefs, partner communication skills and self-efficacy specific to sex and contraceptive use.
Discussion
Interim outcomes after 12 months of Prime Time provide evidence supporting clinics' use of multi-component, youth development interventions to reduce sexual risk behaviors among adolescent girls at high risk for early pregnancy. Findings demonstrate that a large proportion of a vulnerable group of adolescent girls seeking clinic services will engage in youth development programming, with more than four in five intervention participants (84.5%) actively involved in case management and approximately two-thirds (60.3%) involved in peer educator training by the 12-month interim point. This level of intervention involvement appears to have yielded desired changes in sexual risk behaviors. After 12 months, the intervention group reported more consistent use of condoms, hormonal and dual contraceptive methods with their most recent partner than did the control group. The intervention group also reported greater stress management skills with trends towards higher levels of positive connectedness at school and with family. Sexuality-specific psychosocial outcomes, including perceived partner norms regarding contraception, sexual attitudes and beliefs, sexual communication skills and self-efficacy, were less likely to be affected at this interim point.
Early results suggest that Prime Time is more effective in promoting consistent contraceptive use than in reducing girls' number of sex partners over a six month interval. At enrollment, inconsistent use of condoms and other effective contraceptive methods was commonplace among study participants. Having multiple sex partners was less normative, with 66% of participants reporting one sex partner and 20% reporting two sex partners in the six months preceding enrollment. Thus in this sample, there was more room for sexual risk reduction through improving contraceptive consistency than through reducing the number of sex partners. Other sexual health interventions have evaluated changes in casual and main partners. Among adolescent girls in a brief office intervention, Shrier and colleagues reported significant reductions in causal partners but not in main partners [29]. Future analysis of data from this study will examine intervention effects in relation to partner types (e.g., main, casual).
Of the psychosocial outcomes examined at this 12-month interim, the intervention appears to have impacted general social-emotional skills and pro-social connectedness. At 12 months, teens in the intervention group reported significant improvements in stress management skills with trends towards improvements in family and school connectedness. Given that substantial numbers of our participants are from disadvantaged social contexts (e.g., low-income, violent neighborhoods), they may lack social and institutional supports available to adolescents from more advantaged contexts. Provision of these supports through case management and peer leadership opportunities appeared to result in the uptake of pro-social skills and beliefs. Especially for adolescents from disadvantaged contexts, building pro-social skills, opportunities and supports may be critical to supporting health-promoting behaviors such as contraceptive use [6,30]. Previous research has demonstrated links between adolescents' stress management skills and condom use [31,32]. Other studies link high levels of family and school connectedness with condom and contraceptive use [33,34]. At this 12-month interim, the intervention appears to have had minimal systematic effects on cognitions and skills specific to sex and contraceptive use. Intervention effects on these psychosocial outcomes will be re-assessed at 18-months, when the majority of the intervention group has completed our peer educator training component which emphasizes attitudes, beliefs and skills specific to sexual behaviors and contraceptive use.
Several methodological limitations should be noted. First, data were collected using self-report surveys that are subject to response bias. Using self-report instruments is standard practice for intervention trials addressing sexual risk behaviors; prior research supports the reliability and validity of adolescents' reports of sexual and contraceptive behaviors [35] specifically among sexually active females [24] and particularly with the use of A-CASI methods [36]. Second, our findings may not be generalizable to adolescent girls at high risk for pregnancy who do not utilize clinic services.
This study also has several methodologic strengths. First, the finding that participants and eligible non-participants were similar on a range of indicators suggests that findings may be generalizable to a population of adolescent girls seeking clinic services who are at high risk for pregnancy. Second, minimal loss to follow-up at the 12-month interim along with only isolated differences between girls in the 12-month sample and those lost to follow-up increases our confidence in the validity of findings [37]. Third, use of partner-specific contraceptive measures is a recommended strategy for maximizing participants' recall [38], especially with methods such as condom use that depend on a male partner [24]. Finally, considering the intervention's impact on theoretically important psychosocial mediators of sexual behaviors is an important step in identifying how the intervention functions.
Among adolescents at high risk for pregnancy, research indicates that multifaceted, sustained youth development interventions can have substantive effects on pregnancy risk [4,6]. The National Research Council and the Institute of Medicine concluded that incorporating youth development strategies is fundamental to improving health services, especially for adolescents most vulnerable to poor health outcomes such as early pregnancy [11]. Greater emphasis on youth development strategies will require substantial modifications to traditional models of adolescent health service staffing, delivery and payment [11]. In this era of health care reform, evidence about the efficacy of preventive services grounded in a youth development frame is critical to guiding these changes in health services organization. The current study is one of the first randomized trials of a youth development intervention designed specifically for adolescents seeking clinic services, with most programming occurring outside of clinics' physical space. Long-term outcomes associated with Prime Time involvement are to be determined, future dose-response analysis will examine the contributions of each intervention component to changes in outcome behaviors, and formal mediation analysis [39] will provide further insight into whether social-emotional skills and social connectedness served as important mediators of sexual risk behaviors. However, these interim findings suggest that a theoretically-driven intervention that addresses diverse psychosocial issues confronting high-risk youth while providing skills, opportunities, and supports for youth leadership can promote safer sexual behaviors. As such, these findings indicate the potential fruitfulness of adolescent health services grounded in a youth development framework.
Acknowledgments
This project is supported with funds from the National Institute of Nursing Research (5R01-NR008778) and from the Centers for Disease Control and Prevention (U48-DP001939 and T01-DP000112). The views presented do not necessarily reflect those of the funders. The Prime Time study would not have been possible without the cooperation and contributions of the young women, clinics and research staff involved with this project. We also thank Jenna Baumgartner for her excellent editorial assistance with manuscript preparation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2006. Natl Vital Stat Rep. 2009;57:1–103. [PubMed] [Google Scholar]
- 2.Ventura S, Amba J, Mosher W, et al. Estimated pregnancy rates by outcome for the United States: 1990-2004. Natl Vital Stat Rep. 2008;56:1–25. [PubMed] [Google Scholar]
- 3.Hamilton BE, Martin J, Ventura S. Births: Preliminary data for 2007. Natl Vital Stat Rep. 2009;57:12. [PubMed] [Google Scholar]
- 4.Kirby D. Emerging Answers 2007: Research Findings on Programs to Reduce Teen Pregnancy and Sexually Transmitted Diseases. Washington, DC: National Campaign to Prevent Teen Pregnancy; 2007. [Google Scholar]
- 5.Hoffman S. By the Numbers: The Public Costs of Teen Childbearing. Washington, DC: National Campaign to Prevent Teen Pregnancy; 2006. [Google Scholar]
- 6.Philliber S, Kaye JW, Herrling S, et al. Preventing pregnancy and improving health care access among teenagers: an evaluation of the Children's Aid Society-Carrera program. Perspect Sex Reprod Health. 2002;34:244–251. [PubMed] [Google Scholar]
- 7.Resnick MD. Protective factors, resiliency and healthy youth development. Adolesc Med State Art Rev. 2000;11:157–164. [PubMed] [Google Scholar]
- 8.Tuttle J, Bidwell-Cerone S, Campbell-Heider N, et al. Teen Club: a nursing intervention for reducing risk-taking behavior and improving well-being in female African American adolescents. J Pediatr Health Care. 2000;14:103–108. [PubMed] [Google Scholar]
- 9.Rosenfeld SL, Keenan PM, Fox DJ, et al. Youth perceptions of comprehensive adolescent health services through the Boston HAPPENS program. J Pediatr Health Care. 2000;14:60–67. [PubMed] [Google Scholar]
- 10.Komro K, Perry C, Murray D, et al. Peer-planned social activities for preventing alcohol use among young adolescents. J Sch Health. 1996;66:328–334. doi: 10.1111/j.1746-1561.1996.tb03413.x. [DOI] [PubMed] [Google Scholar]
- 11.National Research Council and Institute of Medicine Adolescent Health Services: Missing Opportunities. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 12.Sieving R, Resnick M, Garwick A, et al. A clinic-based, youth development approach to teen pregnancy prevention. Am J Health Behav. doi: 10.5993/ajhb.35.3.8. in press. [DOI] [PubMed] [Google Scholar]
- 13.Zabin LS, Sedivy V, Emerson MR. Subsequent risk of childbearing among adolescents with a negative pregnancy test. Fam Plann Perspect. 1994;26:212–217. [Google Scholar]
- 14.Orr DP, Johnston K, Brizendine E, et al. Subsequent sexually transmitted infection in urban adolescents and young adults. Arch Pediatr Adolesc Med. 2001;155:947–953. doi: 10.1001/archpedi.155.8.947. [DOI] [PubMed] [Google Scholar]
- 15.Silverman JG, Raj A, Clements K. Dating violence against adolescent girls and associated substance use, unhealthy weight control, sexual risk behavior, pregnancy, and suicidality. JAMA. 2001;286:572–579. doi: 10.1001/jama.286.5.572. [DOI] [PubMed] [Google Scholar]
- 16.Duke N, Sieving R, Pettingell S, et al. Associations between health screening questions and sexual risk behaviors in adolescent female clinic patients: identifying a brief question format to yield critical information. Clin Pediatr. 2008;47:564–572. doi: 10.1177/0009922808314904. [DOI] [PubMed] [Google Scholar]
- 17.Henneken C. Epidemiology in Medicine. Boston, MA: Little Brown and Company; 1987. [Google Scholar]
- 18.Sussman S, Dent C, Stacy A. Project Towards No Drug Use: a review of the findings and future directions. Am J Health Behav. 2002;26:354–365. doi: 10.5993/ajhb.26.5.4. [DOI] [PubMed] [Google Scholar]
- 19.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice–Hall; 1986. [Google Scholar]
- 20.Sieving R, Bernat D, Resnick M, et al. A clinic-based youth development program to reduce sexual risk behaviors among adolescent girls: the Prime Time pilot study. Health Promotion Practice. doi: 10.1177/1524839910386011. in press. [DOI] [PubMed] [Google Scholar]
- 21.Tanner A, Secor-Turner M, Garwick A, et al. Engaging vulnerable adolescents in the prime time program to reduce unintended pregnancy: perspectives of case managers. J Pediatr Health Care. doi: 10.1016/j.pedhc.2010.10.003. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Caines K, Sieving R, Resnick M. Realities, rituals, and rhythms: mentoring relationships with high-risk sexually active girls. J Adolesc Health. 2004;34:150–151. [Google Scholar]
- 23.Kirby D, Lezin N, Afriye R, et al. Preventing Teen Pregnancy: Youth Development and After-School Programs. Scotts Valley, CA: ETR Associates; 2003. [Google Scholar]
- 24.Sieving R, Hellerstedt W, Fee R, et al. Reliability of self-reported contraceptive use and sexual behaviors among adolescent girls. J Sex Res. 2005;42:159–67. doi: 10.1080/00224490509552269. [DOI] [PubMed] [Google Scholar]
- 25.Ballinger G. Using generalized estimating equations for longitudinal data analysis. Org Res Methods. 2004;7:127–150. [Google Scholar]
- 26.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 27.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 28.Hutchinson KM, Holtman MC. Focus on research methods: analysis of count data using poisson regression. Res Nurs Health. 2005;28:408–418. doi: 10.1002/nur.20093. [DOI] [PubMed] [Google Scholar]
- 29.Shrier L, Ancheta R, Goodman E, et al. Randomized controlled trial of a safer sex intervention for high-risk adolescent girls. Arch Pediatr Adolesc Med. 2001;155:73–79. doi: 10.1001/archpedi.155.1.73. [DOI] [PubMed] [Google Scholar]
- 30.Pittman KJ, Irby M, Tolman J, et al. Preventing Problems, Promoting Development, Encouraging Engagement: Competing Priorities or Inseparable Goals? Washington, DC: Forum for Youth Investment; 2003. [Google Scholar]
- 31.DiClemente RJ, Lodico M, Grinstead OA, et al. African-American adolescents residing in high-risk urban environments do use condoms: correlates and predictors of condom use among adolescents in public housing developments. Pediatrics. 1996;98:269–278. [PubMed] [Google Scholar]
- 32.Lando E, Sieving R, McMorris B, et al. Associations between social emotional intelligence and adolescent girls' sexual risk behaviors. J Adolesc Health. 2010;46:S7. [Google Scholar]
- 33.Markham CM, Tortolero SR, Escobar-Chaves SL, et al. Family connectedness and sexual risk taking among youth attending alternative high schools. Perspect Sex Reprod Health. 2003;35:174–179. doi: 10.1363/psrh.35.174.03. [DOI] [PubMed] [Google Scholar]
- 34.Jaccard J, Dittus PJ, Gordon VV. Maternal correlates of adolescent sexual and contraceptive behavior. Fam Plann Perspect. 1996;28:159–165. [PubMed] [Google Scholar]
- 35.Brener N, Kann L, McManus T, et al. Reliability of the 1999 youth risk behavior survey questionnaire. J Adolesc Health. 2002;31:336–42. doi: 10.1016/s1054-139x(02)00339-7. [DOI] [PubMed] [Google Scholar]
- 36.Turner C, Ku L, Rogers S, et al. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280:867–73. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 37.Davis L, Broome M, Cox R. Maximizing retention in community-based clinical trials. J Nurs Scholarsh. 2002;34:47–53. doi: 10.1111/j.1547-5069.2002.00047.x. [DOI] [PubMed] [Google Scholar]
- 38.Catania J, Chitwood D, Gibson D, et al. Methodologic problems in AIDS research: influences on measurement error and participation bias in studies of sexual behavior. Psychological Bulletin. 1990;108:339–362. doi: 10.1037/0033-2909.108.3.339. [DOI] [PubMed] [Google Scholar]
- 39.MacKinnon DP. Analysis of mediating variables in prevention and intervention research. In: Cazares A, Beatty LA, editors. Scientific Methods for Prevention Intervention Research. National Institute on Drug Abuse Research Monographs. Vol. 139. Department of Health and Human Services; Washington, DC: 1994. pp. 127–153. Publication No. 94-3631. Supplement of Documents, US Government Printing Office. [PubMed] [Google Scholar]
- 40.Bar-On R. The Bar-On model of emotional-social intelligence. Psicothema. 2006;18(Supl):13–25. [PubMed] [Google Scholar]