Abstract
Objectives
To describe the current level of utilization of informatics systems in hospice and palliative care and to discuss two projects that highlight the role of informatics applications for hospice informal caregivers.
Data sources
Published articles, web resources, clinical practice and ongoing research initiatives.
Conclusion
There are currently few informatics interventions designed specifically for palliative and hospice care. Challenges such as interoperability, user acceptance, privacy, the digital divide and allocation of resources all affect the diffusion of informatics tools in hospice.
Implications for nursing practice
Caregiver support through use of IT is feasible and may enhance hospice care.
Keywords: informatics, hospice, palliative care, information technology, Internet
The field of biomedical and health informatics, defined as the study of the use of information technology (IT) to support and enhance health care delivery, biomedical research and education, has experienced rapid growth in recent years. Informatics applications including electronic medical records, hospital information systems, medical imaging applications and telemedicine platforms are widely used in health care settings. Initially developed with an emphasis on improving care delivery within an institution, advances in technology have shifted the design of IT based systems to a focus on patient applications that allow patients to be actively involved in the decision making process and to access their own record and other resources.
Government initiatives worldwide are currently in place to foster and expedite the adoption and diffusion of informatics applications. In the United States, for example, the federal government established an ambitious goal of providing electronic health records for all Americans that will ensure information is accessible at the time and place of care regardless of the information source.1 These records are to be designed to allow for secure and private exchange of information among health care providers when authorized by the patient. The federal government is taking several steps to realize this goal, such as an adoption of health information standards, funding increase for demonstration projects and coordination of efforts at a federal level. Furthermore, with the Health Information Technology for Economic and Clinical Health Act (HITECH) the government authorized incentive payments to clinicians and hospitals when they use Electronic Health Records (EHRs) privately and securely to achieve specified improvements in care delivery, promoting “meaningful use” of IT.1
While informatics tools are widely used in most domains of health care, their diffusion has not fully reached the field of palliative and hospice care where the focus is on providing care for the seriously ill and dying. The goal in this setting is to minimize suffering and improve patients’ quality of life at the end of life with an emphasis on palliation rather than treatment of the terminal disease. In the United States, one of four deaths is due to cancer.2 As reviewed by Murray et al.,3 while the majority of patients with cancer continue to die within institutions, those who die at home typically have identified caregivers. Communication and connection between providers, hospice/palliative care services and the home vary widely. Palliative care services may be delivered under the umbrella of a large health care facility that utilizes IT, but it is less frequent that system designers implement applications specifically for home hospice or palliative care services. For example, findings from the 2000 National Home and Hospice Care Survey in the US indicated that approximately 32% of all agencies, and about one-fifth of hospice agencies specifically (18.6%), reported using computerized medical records.4
Current Use of Informatics for End of Life Care
Studies have examined the potential of telecommunications; ways in which technology can function as a support mechanism for caregivers of hospice patients,5 an assessment of the readiness of hospice organizations to accept technological innovation,6 and the creation of a Web-based worksheet that allows for expert feedback in a community-based hospice.7 Long et al.8 explored whether computers and the Internet are used in home care and hospice agencies, conducting a survey that indicated the potential of advanced technologies remains to a great extent unexplored. Finally, several studies focused on the use of telehealth or videoconferencing technologies in hospice (telehospice) describing the concept and potential of telehospice, 9–13 pilot projects with a small numbers of subjects,14–16 ethical considerations associated with the use of telehealth technologies in hospice care,17 hospice agencies’ readiness to adopt telehealth,6 providers’ acceptance18–21 and patients’ acceptance.22,23
In spite of the limited evidence of IT use specifically in hospice, there are successful demonstrations of IT implementation in home care that highlight the potential of informatics to improve palliative and hospice care. Home-based telehealth applications (also known as telehomecare applications) are based on the utilization of telecommunication and videoconferencing technologies to enable a healthcare provider at the clinical site to communicate with patients at their home. Such an interaction via videoconferencing is called a ‘virtual visit.’ Johnston et al.24 evaluated the use and costs of remote video technology in the home care setting for congestive heart failure patients and determined that this approach achieved cost savings and improved access to home care support while producing no differences in clinical outcomes when compared to traditional home care. Similarly, a telehealth application developed at Columbia University25 for diabetic home care patients showed that the intervention led to measurable improvements in clinical status for the patients. Obviously, the evaluation of telehealth in hospice will focus on outcomes such as patient’s comfort or caregiver anxiety or cost, rather than long term clinical outcomes that are the focus of the chronic condition, telehealth interventions in home care.
The Internet provides a platform for consumers to access health information and can therefore play a role in end of life care as well. Over the years, the number of web-based patient education sites that allow patients to access information related to their condition has been increasing. Such sites, however, do not always protect visitors from misleading or inaccurate data. There are examples of successful implementation of Web-based systems that empower patients such as the home asthma telemonitoring (HAT) system26 which provides patients with continuous web-based individualized help in the daily routine of asthma self-care or a web-based system for patients who manage insulin-dependent diabetes mellitus.27 Again, this domain has not been studied extensively in the hospice setting. Willis et al,28 conducted a systematic literature review to identify current Internet-based interventions in hospice and palliative care and the evidence of their effectiveness. The authors found only six studies evaluating web-based clinical interventions for patients, caregivers and hospice/palliative care providers.
Mobile devices are widely utilized in other clinical settings and may find utility in palliative care as well. For health care practitioners, the use of mobile IT not only can bring additional resources to the point-of-care, but it can actually change the point of care itself. Within the mobile IT disease management literature, there appears to be a gradual transition from provider-centric applications to applications that include the patient within the process. Earlier research into using mobile IT devices, such as PDAs or cellular phones, emphasized the collection of data from the patient in order to facilitate clinician decision making.29 Decision support for these devices has been mainly on the clinician (receiver) side; however there are a few applications that are also providing real-time decision support to the patients.30 Interestingly, despite the movement towards patient-centric applications, most of the current application descriptions rely on an older medical model of decision making in which the patient is a receiver of instructions rather than a participant in the management process.31 In hospice care, the use of mobile devices has been studied by Kuziemsky et al.32 as a tool to enhance pain management; however, the tool is used solely by health care providers and does not involve patients.
When considering the potential of IT the digital divide becomes a challenge that needs to be addressed. The term is used to refer to the gap in computer and Internet access between population groups segmented by income, age, educational level, or other parameters. Several efforts have been made to address this divide focusing primarily on providing access to computers, the Internet, and training. While lower socioeconomic groups are increasingly gaining Internet access, it is considered likely that the digital divide will persist as new technologies become available. For example, as sophisticated multimedia services become an integral part of Internet-based applications, broadband access may become as important for accessing health care sites as narrowband access is today for obtaining Web-based health information. In that case, the digital divide can exist between two groups that both have PC hardware and Internet access, simply due to different access protocols. Furthermore, access to infrastructure is only one dimension of the digital divide, of which health literacy and appropriate web content are additional key components. These issues play a key role in the diffusion of informatics applications in hospice and palliative care especially systems that are to be used or implemented in the patients and families’ homes.
IT and the Caregiving Experience
Our own work focuses specifically on the hospice setting and ways to utilize IT to support informal caregivers, namely family, spouses, friends or others who assume the primary unpaid caregiver role, often parallel to diminished function or abilities in the patient. Recent research has underscored the importance of understanding the risks and unmet needs of informal caregivers who care for patients at the end of life.33 The presence of a caregiver in the home is required for admission to many US hospices as non-professional caregiving is crucial to providing end-of-life care for patients with terminal illness who chose to die at home. Caregivers are at greater risk for depression, deteriorating physical health, financial difficulties, and premature death.34,35 Health and psychological risks are compounded by the fact that caregivers are less likely to engage in preventive health behaviors, or otherwise attend to their own health needs, which places them at risk for exacerbation of existing chronic health problems.36
In many instances, hospice agencies struggle to provide adequate or frequent support to caregivers as they are faced with a series of challenges. The Institute of Medicine (IOM) has identified systemic deficiencies in end-of-life care37 that can be grouped into (1) legal, organizational, and economic obstacles to palliative care; and (2) the systemic lack of appropriate end-of-life care, education of health care professionals and the public, and communication between all involved parties. Caregivers rate communication as essential to the support they receive and seek regular contact with hospice providers, appreciating both face-to-face communication and the security of the phone as an “emergency back-up tool.”38 The use of information technologies can bridge geographic distance and enhance hospice services provided to informal caregivers in cases where additional face to face interactions may be costly or non-feasible.
A growing number of researcher teams are exploring strategies to enhance traditional hospice care through the use of web-based technologies. Although the field is in its infancy, early results appear promising. Many hospice caregivers and patients access information about their illnesses online.39 Often spending the majority of time in the home, both patients and caregivers seek remote mutual support from others who are coping with a terminal illness, often enjoying the anonymity provided by the Internet.40,41 Lind and Karlsson41 found that both hospice providers and service recipients benefited from Web-based services in that patients reported a high level of access to providers, while providers received information from patients in a timely manner.
Focus on the Caregiver
Kinsella and colleagues42 categorized caregiver burden into an objective form represented by tangible costs, physical care demands and disruptions to daily routines, and a subjective form represented by the caregiver’s own appraisal of the impact of caring, emotions aroused by caregiving and coping resources. Factors that affect the caregiving experience included personality, stressor appraisal, use of coping strategies, the availability and adequacy of social support, family functioning and competing commitments.42 Based on this conceptual foundation, a comprehensive model of stress and coping indicating the mediating factors in the process of caregiving was developed by Pearlin, Mullan, Semple and Skaff 43 and has been further developed by Meyers and Gray.44
Our work of integrating technology for hospice caregivers, based on previous work cited above is a theoretical model labeled ACT (Assessing Caregivers for Team Interventions). ACT (Figure 1) incorporates ongoing assessment of the background context, primary, secondary and intrapsychic stressors as well outcomes of the caregiving experience and subsequently, the design and delivery of appropriate interventions to be delivered by the hospice team (ensuring a holistic approach to addressing the multifaceted challenges of the caregiving experience).45 ACT can therefore act as one of the mediators affecting the overall caregiver experience and improve outcomes such as satisfaction with hospice care, reduced anxiety and improved overall quality of care.45 Next, we describe two projects based on the ACT model that use informatics tools to deliver supportive services to hospice informal caregivers.
Figure 1.
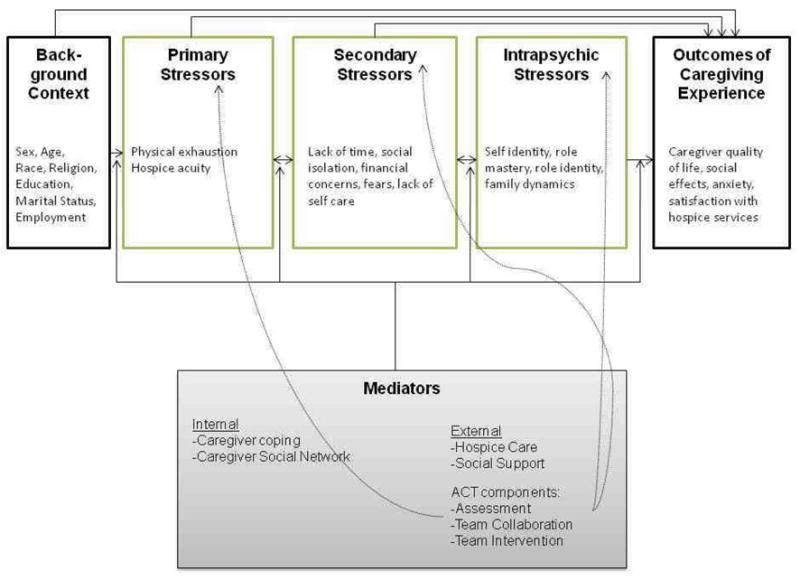
The Assessing Caregivers for Team interventions model 45 illustrating caregiver needs, mediators, hospice interventions and outcomes. (Reprinted with permission)
A Video Platform to Invite Caregivers to Interdisciplinary Hospice Teams:The ACTIVE Intervention
Patient and family participation in hospice interdisciplinary team (IDT) meetings is consistent with the hospice philosophy of care that recognizes the family caregiver along cwith the patient as the dyad that receives services and drives decision making.46 Yet, significant barriers exist to fully involving patients and their family members in IDT meetings. In our preliminary work, 47 we found that less than half of hospices surveyed ever had a caregiver attend their meeting and in no case was caregiver attendance a standard of care. The barriers identified for this lack of attendance included the frail condition of the patient and the time and distance required for travel to meet at the hospice office.7
The ACTIVE (Assessing Caregivers for Team Intervention through Videophone Encounters) intervention was designed to overcome these barriers by allowing patients and/or their informal caregivers to participate in meetings from their own homes using commercially available videophone technology (Figure 2). By eliminating logistical barriers, ACTIVE was designed to provide the context for patient and family participation in hospice IDT meetings.48 Staff installed a videophone unit in the homes of participating families, connecting them to the hospice office using a standard telephone line. The hospice office was equipped with compatible videophone technology that could be viewed on a large television screen, thereby permitting numerous members of the hospice IDT to view the participant simultaneously. The intervention was designed primarily for family caregivers; patients could participate as their health condition(s) allowed.48 Results indicated that ACTIVE enhanced team functioning in terms of context, structure, processes, and outcomes. Participants discussed challenges and offered corresponding recommendations to make the intervention more efficient and effective. Data supported ACTIVE as a way for hospice providers to more fully realize their goal of maximum patient and family participation in care planning.48 Caregivers readily asked questions while virtually attending the meeting, especially of the hospice medical director. Those questions primarily involved issues of pain management.49 Caregivers’ perceptions of pain medication management and quality of life improved in Phase 2 (when the video intervention was introduced) as compared to caregivers in Phase 1 (where traditional hospice services were observed).50 The caregivers in the intervention phase had significantly fewer perceptions of pain management that were regarded as barriers.50 Both caregivers and hospice staff members reported ACTIVE as valuable, both reporting that the intervention created trust in the relationship as the “voices and faces” were more real during the meetings.44
Figure 2.

The videophone used for the study operates over regular phone lines and plugs into the phone already in use in the household, thus, reducing the need for training prior to operation. Both parties have to consent by pressing the “Video” button for a video-call to be established; if one or both parties choose not to enable the video feature, they can use their regular phone for audio interactions.
Note: Higher resolution of this figure is in a separate file (#6A)
Using Videophones to Deliver Problem Solving Therapy to Hospice Caregivers
Videophones are a feasible method for the delivery of problem-solving therapy (PST) to informal hospice caregivers.51 Because audio-only communication is poor at capturing nonverbal behaviors, it may not be as efficient as a mechanism for comprehensive assessment of the caregiver and patient situation, followed by delivery of a cognitive-behavioral intervention. In our pilot study we used the same commercially available, low cost videophone technology as in previous work. Informal hospice caregivers were randomly assigned to receive PST from researchers using videophones, instead of communicating in face-to-face sessions. Outcome measures included caregiver anxiety, quality of life and problem-solving abilities, technical quality of video-sessions and satisfaction of participants (including both subjects and researchers). The overall technical quality of the video-calls was very good. Caregivers reported a slightly higher quality of life post-intervention than at baseline.51 Caregivers reported lower levels of anxiety post-intervention than at baseline. The subjects were generally satisfied with the videophones during their exit interviews suggesting this as a cost-effective way to deliver cognitive behavioral interventions without investment in travel,
Conclusion
There is an emerging body of literature that showcases the potential of informatics applications for patients and caregivers in hospice. While IT has not been utilized in the hospice setting to the same extent as in other clinical domains, studies suggest the potential of videoconferencing, Web applications and mobile tools to support clinicians as well as patients and their families. As is the case with any health information system, end-user satisfaction is key to successful system implementation. Health care is an information-intensive industry, yet stakeholders may resist information technology as it may change roles and responsibilities.52 Hospice end-users represent different professional disciplines, patients, family members and informal caregivers. Testing of new hospice IT requires that the user groups be involved in all stages of the system development.
If IT is to play a role in hospice and palliative care, more research is needed to explore the appropriate ways of designing and implementing information systems in this domain and to determine the technology’s impact on patient clinical outcomes and the caregiving experience. An interdisciplinary approach will ensure that we move beyond silos of expertise and design systems driven not by the technological advances but rather by the needs of the stakeholders.
Acknowledgments
Supported in part by the National Institutes of Health (NIH) National Institute on Nursing R21NR010744 (Demiris PI) and R01NR011472 (Parker Oliver PI).
Footnotes
Manuscript work completed at the University of Washington, University of Missouri and the University of North Texas
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–4. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Siegel R, Xu J, Ward E. Cancer Statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 3.Murray MA, Fiset V, Young S, Kryworuchko J. Where the dying live: a systematic review of determinants of place of end-of-life cancer care. Oncol Nurs Forum. 2009;36(1):69–77. doi: 10.1188/09.ONF.69-77. [DOI] [PubMed] [Google Scholar]
- 4.Pearson WS, Bercovitz AR. Use of computerized medical records in home health and hospice agencies: United States, 2000. Vital and Health Statistics Series. 2006;13 (161):1–14. [PubMed] [Google Scholar]
- 5.Demiris G, Parker Oliver D, Courtney KL, Porock D. Use of technology as a support mechanism for caregivers of hospice patients. J Palliat Care. 2005;21:303–309. [PubMed] [Google Scholar]
- 6.Oliver DR, Demiris G. An assessment of the readiness of hospice organizations to accept technological innovation. J Telemedicine and Telecare. 2004;10:170–174. doi: 10.1258/135763304323070832. [DOI] [PubMed] [Google Scholar]
- 7.Ogle K, Thompson ME, Noel MM. The Web-based worksheet: an opportunity for prompt, consistent, and expert feedback in a community-based hospice experience. J Palliat Med. 2002;5:756–757. doi: 10.1089/109662102320880642. [DOI] [PubMed] [Google Scholar]
- 8.Long CO, Greenberg EA, Ismeurt RL, Smith G. Computer and Internet use by home care and hospice agencies. Home Healthcare Nurse. 2000;18:666–671. doi: 10.1097/00004045-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Wesley D. High-tech hospice. Am J Hospice Care. 1989;6:17–18. doi: 10.1177/104990918900600520. [DOI] [PubMed] [Google Scholar]
- 10.Waters RJ, Eder-Van Hook J. Hospice’s high touch approach enhanced by telecommunication. Caring. 2005;24:70–71. [PubMed] [Google Scholar]
- 11.Kinsella A. Telehospice and its use in home hospice care delivery today. Caring. 2005;24:54–57. [PubMed] [Google Scholar]
- 12.Kinsella A. Telehealth in hospice care, or telehospice: a new frontier of telehealth service delivery. J Palliat Med. 2005;8:711–712. doi: 10.1089/jpm.2005.8.711. [DOI] [PubMed] [Google Scholar]
- 13.Williams J, Bassett M. Telemanagement in hospice-a new frontier. Caring. 2006;25:22–24. [PubMed] [Google Scholar]
- 14.Saysell E, Routley C. Telemedicine in community-based palliative care: evaluation of a videolink teleconference project. Int J Palliat Nurs. 2003;9:489–495. doi: 10.12968/ijpn.2003.9.11.11874. [DOI] [PubMed] [Google Scholar]
- 15.Lynch J, Weaver L, Hall P, Langlois S, Stunt M, Schroder C, Bouvette M. Using telehealth technology to support CME in end-of-life care for community physicians in Ontario. Telemed J e-Health. 2004;10:103–107. doi: 10.1089/153056204773644643. [DOI] [PubMed] [Google Scholar]
- 16.Oliver D, Demiris G, Day M, Courtney KL, Porock D. Telehospice support for elder caregivers of hospice patients: two case studies. J Palliat Med. 2006;9:264–267. doi: 10.1089/jpm.2006.9.264. [DOI] [PubMed] [Google Scholar]
- 17.Demiris G, Oliver D, Courtney KL. Ethical considerations for the utilization of tele-health technologies in home and hospice care by the nursing profession. Nurs Admin Q. 2006;30:56–66. doi: 10.1097/00006216-200601000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Cook DJ, Doolittle GC, Whitten PS. Administrator and provider perceptions of the factors relating to programme effectiveness in implementing telemedicine to provide end-of-life care. J Telemed Telecare. 2001;7 (Suppl 2):17–19. doi: 10.1258/1357633011937335. [DOI] [PubMed] [Google Scholar]
- 19.Demiris G, Oliver D, Fleming D, Edison K. Hospice staff attitudes towards telehospice. Am J Hospice Palliat Care. 2004;21:343–347. doi: 10.1177/104990910402100507. [DOI] [PubMed] [Google Scholar]
- 20.Whitten PS, Mackert M. Addressing telehealth’s foremost barrier: provider as initial gatekeeper. Int J Tech Assess Health Care. 2005;21:517–521. doi: 10.1017/S0266462305050725. [DOI] [PubMed] [Google Scholar]
- 21.Whitten P, Doolittle G, Mackert M. Providers’ acceptance of telehospice. J Palliati Med. 2005;8:730–735. doi: 10.1089/jpm.2005.8.730. [DOI] [PubMed] [Google Scholar]
- 22.Whitten PS, Doolittle G, Mackert M. Telehospice in Michigan: use and patient acceptance. Am J Hospice Palliat Care. 2004;21:191–195. doi: 10.1177/104990910402100307. [DOI] [PubMed] [Google Scholar]
- 23.Parker Oliver D, Demiris G, Porock D. The usability of videophones for seniors and hospice providers: a brief report of two studies. Computers in Biology and Medicine. 2005;35:782–790. doi: 10.1016/j.compbiomed.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 24.Johnston B, Wheeler L, Deuser J, Sousa KH. Outcomes of the Kaiser Permanent Tele-Home Health Research Project. Arch Family Med. 2000;9:40–45. doi: 10.1001/archfami.9.1.40. [DOI] [PubMed] [Google Scholar]
- 25.Shea S, Weinstock RS, Starren J, Teresi J, Palmas W, Field L, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus. J Am Med Informatics Assoc. 2006;13:40–51. doi: 10.1197/jamia.M1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Finkelstein J, O’Connoer G, Friedmann RH. Development and implementation of the home asthma telemonitoring (HAT) system to facilitate asthma self-care. MedInfo. 2001;10:810–814. [PubMed] [Google Scholar]
- 27.Riva A, Bellazzi R, Stefanelli M. A Web-based system for the intelligent management of diabetic patients. MD Computing. 1997;14:360–364. [PubMed] [Google Scholar]
- 28.Willis L, Demiris G, Parker Oliver D. Internet Use by Hospice Families and Providers: A Systematic Review. J Medl Systems. 2007;31(2):97–101. doi: 10.1007/s10916-006-9033-0. [DOI] [PubMed] [Google Scholar]
- 29.Mohan A, Picard R. Health0: a new health and lifestyle management paradigm. Studies in Health Technology and Informatics. 2004;108:43–48. [PubMed] [Google Scholar]
- 30.Jung D, Hinze A. A mobile alerting system for the support of patients with chronic conditions. First Euro Conference on Mobile Government; Brighton, UK. 2005. [Google Scholar]
- 31.Stead W, Lorenzi N. Health Informatics: Linking Investment to Value. J Am Med Informatics Assoc. 1999;6:341–348. doi: 10.1136/jamia.1999.0060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuziemsky CE, Downing GM, Black FM, Lau F. A grounded theory guided approach to palliative care systems design. Int J Med Informatics. 2007;76 (Suppl 1):141–148. doi: 10.1016/j.ijmedinf.2006.05.034. [DOI] [PubMed] [Google Scholar]
- 33.Pinquart M, Sorensen S. Differences between caregivers and noncaregivers in psychological health: a meta-analysis. Psychol Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- 34.Dean M. A Law That Would Care for Carers. Lancet. 1995;345(8957):1101. doi: 10.1016/s0140-6736(95)90827-7. [DOI] [PubMed] [Google Scholar]
- 35.Sherwood PR, Given CW, Given B, von Eye A. Caregiver burden and depressive symptoms: Analysis of common outcomes in caregivers of elderly patients. J Aging Health. 2005;17:125–147. doi: 10.1177/0898264304274179. [DOI] [PubMed] [Google Scholar]
- 36.Schultz R, Newsom J, Mittelmark M, et al. Health Effects of Caregiving: the Caregiver Health Effects Study. An ancillary study of the Cardiovascular Health Effects Study. Ann Behav Med. 1997;19:110–116. doi: 10.1007/BF02883327. [DOI] [PubMed] [Google Scholar]
- 37.Field Marilyn J, Cassel Christine K., editors. Institute of Medicine. Approaching Death: Improving Care at the End of Life. National Academy Press; Washington: 1997. [PubMed] [Google Scholar]
- 38.Payne S, Smith P, Dean S. Identifying the concerns of informal carers in palliative care. Palliat Med. 1999;13:37–44. doi: 10.1191/026921699673763725. [DOI] [PubMed] [Google Scholar]
- 39.Pereira J, Bruera E, Macmillan K, Kavanaugh S. Palliative care patients and their families on the internet: Motivation and impact. J Palliat Care. 2000;16:13–19. [PubMed] [Google Scholar]
- 40.Coleman J, Olsen S, Sauter P, Baker D, Hodgin M, Stanfield C, Emerling A, Hruban R, Nolan M. The effect of a frequently asked questions module on a pancreatic web site patient/family chat room. Cancer Nurs. 2005;28:460–468. doi: 10.1097/00002820-200511000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Lind L, Karlsson D. A system for symptom management in advanced palliative home healthcare using digital pens. Medical Informatics and the Internet in Medicine. 2004;29:199–210. doi: 10.1080/14639230400005966. [DOI] [PubMed] [Google Scholar]
- 42.Kinsella G, Cooper B, Picton C, Murtagh D. A Review of measurement of caregiver and family burden in palliative care. J Palliat Care. 1998;14:37–45. [PubMed] [Google Scholar]
- 43.Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 44.Meyers JL, Gray LN. The relationships between family primary caregiver characteristics and satisfaction with hospice care, quality of life, and burden. Oncol Nurs Forum. 2001;28:73–82. [PubMed] [Google Scholar]
- 45.Demiris G, Parker Oliver D, Wittenberg-Lyles E. Assessing Caregivers for Team Interventions (ACT): A New Paradigm for Comprehensive Hospice Quality Care. AmJ Hospice Palliat Med. 2009;26(2):128–134. doi: 10.1177/1049909108328697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Anspaugh DJ. The hospice: advocate for the dying. Health Educ. 1978;9(6):3–4. [PubMed] [Google Scholar]
- 47.Parker Oliver D, Porock D, Demiris G, Courtney K. Patient and family involvement in hospice interdisciplinary teams. J Palliat Care. 2005;21(4):270–276. [PubMed] [Google Scholar]
- 48.Oliver DP, Washington KT, Wittenberg-Lyles E, Demiris G, Porock D. ‘They’re part of the team’: participant evaluation of the ACTIVE intervention. Palliat Med. 2009;23(6):549–55. doi: 10.1177/0269216309105725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wittenberg Lyles E, Parker Oliver D, Demiris G, Washington K, Regehr K, Wilder H. Question asking by family caregivers in hospice interdisciplinary team meetings. Res Gerontol Nurs. 2010;3(2):82–88. doi: 10.3928/19404921-20090731-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Parker Oliver D, Demiris G, Wittenberg-Lyles E, Porock D, Collier J, Arthur A. Caregiver participation in hospice interdisciplinary team meetings via videophone technology: A pilot study to improve pain management. Am J Hosp Palliat Care. 2010;27(7):465–73. doi: 10.1177/1049909110362402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Demiris G, Oliver DP, Wittenberg-Lyles E, Washington K. Use of videophones to deliver a cognitive-behavioural therapy to hospice caregivers. J Telemed Telecare. doi: 10.1258/jtt.2010.100503. in Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stead W, Lorenzi N. Health Informatics: Linking Investment to Value. J Am Med Informatics Assoc. 1999;6:341–348. doi: 10.1136/jamia.1999.0060341. [DOI] [PMC free article] [PubMed] [Google Scholar]


