Abstract
Purpose
To examine the feasibility and efficacy of a theory-driven and family-based program delivered online to promote healthy lifestyles and weights in Chinese American adolescents.
Methods
A randomized controlled study of a Web-based intervention was developed and conducted in 54 Chinese American adolescents (ages, 12–15 years) and their families. Data on anthropometry, blood pressure, dietary intake, physical activity, and knowledge and self-efficacy regarding physical activity and nutrition were collected at baseline and 2, 6, and 8 months after the baseline assessment. Data were analyzed using linear mixed modeling.
Results
The intervention resulted in significant declines in waist-to-hip ratio and diastolic blood pressure and increases in vegetable and fruit intake, level of physical activity, and knowledge about physical activity and nutrition.
Conclusions
This Web-based behavior program for Chinese American adolescents and their families appears feasible and effective in the short term. Longer term effects remain to be determined. This type of program can be adapted for other minority ethnic groups who are at high risk for overweight and obesity and have limited access to programs that promote healthy lifestyles.
Keywords: computer, Internet, overweight prevention, healthy lifestyles, family-based, randomized clinical trial, dietary intake, BMI
Introduction
Obesity is a critical public health concern facing children and adolescents of all ethnicities, including Chinese Americans [1]. Approximately 25% of Chinese American children and adolescents are overweight or obese [2]. Several physical and psychosocial health problems are associated with being overweight, including cardiovascular diseases (CVD), sleep disorders, type 2 diabetes mellitus (T2DM), low self-esteem, and social withdrawal [3, 4]. At the same body mass index (BMI), Chinese Americans are at a higher risk of CVD and T2DM developing than are non-Hispanic whites [5, 6]. Obesity in children is associated with annual costs of $14.1 billion in additional prescription drugs, emergency room care, and outpatient visits [7]. Because 80% of obese children 10 to 15 years old will become obese adults [8], prevention of overweight needs to start in childhood.
Childhood obesity prevention programs usually include strategies to improve nutritional habits and physical activity [9–11] and can be delivered either in person or online. Wantland et al. [12] conducted a meta-analysis of 22 studies and found that an Internet intervention was more successful than a non–Web-based intervention at improving knowledge and behavioral outcomes in an adult population (effect size, −.25 to .29). Although an intervention facilitated by or based on the Internet has a moderate and short-term effect in weight loss and eating behaviors in overweight adolescents [13], Williamson et al. [14] found that a 2-year Internet-based program did not improve weight loss in African American girls.
Culturally appropriate programs have been reported to promote healthy lifestyles, and improve children’s problem-solving in children [15]. In addition, a family-based approach to prevent or treat obesity is more successful at helping children maintain a healthy weight than are programs that do not involve families [16, 17]. However, to our knowledge, only one Internet-based intervention for childhood obesity prevention that included parents has been conducted in African Americans [18].
Internet-based health promotion and obesity prevention programs have the potential to reach a large number of people by reducing some barriers such as program availability, transportation concerns, and time constraints at a relatively reasonable cost compared with traditional personal consultation programs [19]. However, no Internet-based obesity prevention program for Chinese American adolescents has been reported. Thus, we developed a Web-based behavioral program (Web-Based Active Balance Childhood [Web ABC] study) that focuses on promoting healthy lifestyles (adequate dietary intake and improved physical activity) and healthy weight in Chinese American adolescents, ages 12 to 15, and their parents. The aim of this study was to examine the efficacy of the Web ABC program in promoting healthy lifestyles and healthy weight in Chinese American adolescents.
Methods
The efficacy of the Web ABC study’s program was examined by using a randomized control study design. Adolescents in the study completed questionnaires regarding their dietary intake, knowledge of nutrition and physical activity, and self-efficacy related to physical activity and healthy food choices at baseline (T0) and 2 months (T1), 6 months (T2), and 8 months (T3) after the baseline assessment. The mothers completed questionnaires regarding parents’ demographic information and levels of acculturation at baseline. Inclusion criteria for this study included: (1) adolescents who were 12 to 15 years old and were normal weight or overweight based on CDC’s recommendation; (2) self-identified ethnicity as Chinese or of Chinese origin by both subject and parent, and they must reside in the same household; (3) the adolescent had to be able to speak and read English; (4) The adolescent had to report being in good health, defined as free of an acute or life-threatening disease; and (5) parents must have been able to speak English, Mandarin, or Cantonese and read English or Chinese. Data were collected from October 2007 to May 2009.
Study procedure
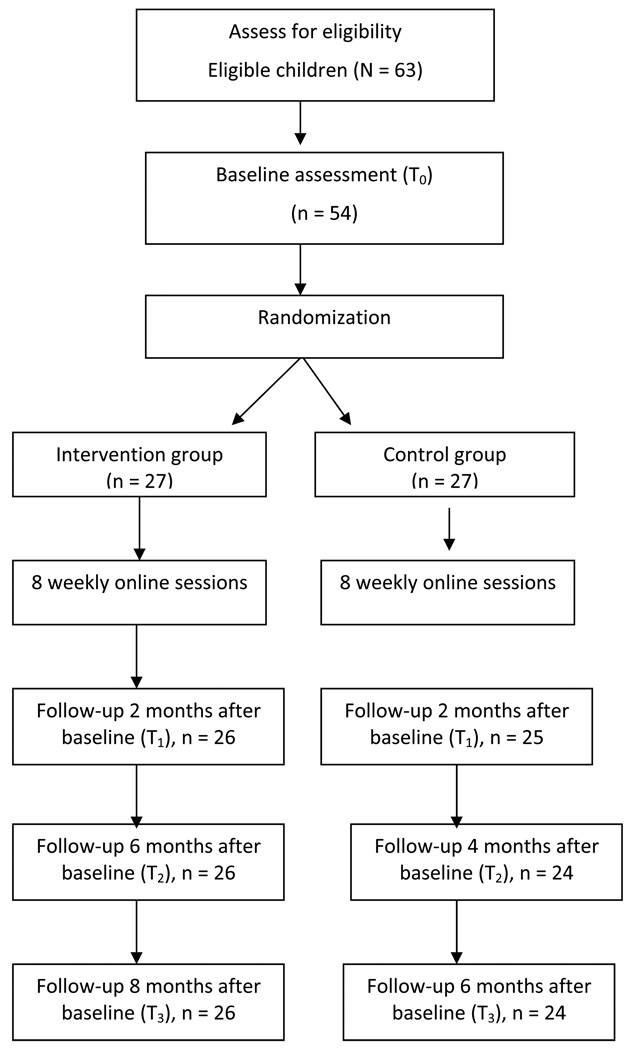
The University of California, San Francisco Committee on Human Research approved the study. Convenience sampling was used to recruit participants from community programs in the San Francisco Bay area. Each site coordinator helped identify potential eligible participants and introduced them to research assistants. Research assistants described the study to adolescents and gave them a letter of introduction to take home to their parents. Parents and adolescents provided their names and contact information to the research team within 2 weeks of receiving the forms if they were interested in participating in the study. Research assistant conducted eligibility assessments based on inclusion and exclusion criteria at a meeting with both parents and adolescents. Both parents and adolescents signed the written inform consents. After obtaining informed consent, subjects were randomly assigned to the intervention group or the control group on the basis of a computer-generated random number assignment (Figure 1). A lesson on Internet navigation and login procedures was demonstrated on a laptop, and a written guide was given to participants. Parents and adolescents each had a separate username and password assigned to them, allowing them to have access to the study’s Web site (intervention or control Web sites). Subjects were able to complete study surveys in parts but were asked to complete the remaining surveys within 1 week. Participants can logon to the website and complete the online assessment from any place that has internet access (i.e., home, school or library). Personal data collection for weight, height, blood pressure, and circumferences were done within the same week of online data collection by a trained research assistant. Because mothers are typically the primary caregiver, they were asked to complete all surveys online at the same as the adolescents. After the completing the questionnaires online, subjects had access to lessons assigned to them. In this study, subjects received weekly session activities online for 8 weeks (Table 1), and parents received three online sessions within the same 8 weeks.
Figure 1.
Study procedure.
Table 1.
Program themes for adolescents
| Week | Intervention | Control |
|---|---|---|
| 1 | Understand how the body works and how to recognize and cope with feelings | Understand the importance of health in adolescents |
| 2 | Apply adequate problem solving techniques and coping skills | Apply appropriate techniques for identifying food and drug allergies |
| 3 | Use various relaxation techniques and develop healthy coping skills | Use adequate protection from burns |
| 4 | Nutrition 101: Understand food and health | Understand basic skin care for adolescents |
| 5 | Nutrition 102: Make smart food choices | Make smart choices in dental care |
| 6 | Understand the importance of an adequate activity level | Understand the consequences of smoking and drinking |
| 7 | Being cool and active: various fun activities for youth and families | Being cool: stay away from drugs and alcohol |
| 8 | Being yourself and using fun ways to improve your health and maintain a healthy lifestyle | Being yourself and staying healthy |
Overview of the Web ABC study intervention
The intervention is based on the Transtheoretical Model–Stages of Change [20] and the social cognitive theory [21]. This intervention was designed to be individually tailored to the behavioral stage of the adolescent. For instance, if the adolescent is in the Preparation stage in physical activity area, he/she will receive information on ways of being active and various types of fun activities he/she can do. Adolescents and their parents were also taught to set realistic and achievable goals in the area that they are ready to make a change and were provided with the necessary skills to achieve mastery and enhance self efficacy in maintaining a healthy lifestyle.
The Web-based program consists of activities to enhance adolescents’ self-efficacy and facilitated their understanding and use of problem-solving skills related to nutrition, physical activity, and coping. Information related to nutrition (e.g., Food Pyramid, the Big Three, Portion Size, and Meal Planning developed by the American Dietetic Association)] and healthy lifestyles (e.g., HeartPower developed by the American Heart Association) was modified and used as the curriculum for the intervention. Adolescents also used an interactive dietary preparation software program (The Wok) tailored to common Chinese foods that was developed by Joslin Diabetes Center. Participants could develop a dish and checked on the nutritional information on The Wok program. In addition, participants learned to set up a realistic goal and plan each week to help improve their behaviors including food intake and physical activity. Information presented over the Internet included text, graphics, comics, and voice over. Participants could logon to the program from home, library or community center.
Physical activity was also included in the program, with the goal being to increase adolescents’ energy expenditure. Subjects were encouraged to engage in different types of noncompetitive activities (e.g., dance, brisk walking), learn types of activities that they can do during recess and at home, and learn alternatives to watching television. Each subject also received a pedometer and completed an online activity diary to monitor their activity levels. Adolescents could enter the average number of steps they took and the average number of servings of fruits and vegetables they had consumed on a daily basis on the Web site. These numbers were converted to two graphics that indicated the subject’s progress. All information presented to the adolescents was in English. Each lesson lasted about 15 minutes.
Internet sessions for parents
To increase healthy environment in the family, we designed three sessions aimed to coach parents the skills to help with their adolescent in improving healthy lifestyle and healthy weight. Since most parents were busy and have limited time, three short sessions (15 minutes each) seems to be feasible and acceptable for parents. A family component (three Internet sessions) that is adolescent-specific provides reinforcement and social support at home for the education received during the study. The Internet sessions include sets of exercises to increase parents’ knowledge and skills regarding healthy food preparation, discussion of issues related to dealing with adolescents’ eating habits and problems, and tips about fun family/adolescent activities to improve dietary intake and physical activity. Parents were encouraged to involve their adolescents in shopping and meal preparation. Each lesson lasted about 15 minutes.
Control group
Participants in the control group also logged on to the Web site by using a pre-assigned username and password. Every week for 8 weeks, adolescents received general health information and not tailored, adapted from the American Academy of Pediatrics, the CDC, and the American Heart Association, related to nutrition, dental care, safety, common dermatology care, and risk-taking behaviors using similar format as the intervention group (text, graphics, comics, and voice over) (Table 1). Parents also received three Internet sessions related to general information on the topics taught in the control group. Information presented to adolescents was in English, and to parents was in English and Chinese. Each lessons lasted about 15 minutes.
After completion of each of the in person data collection, parents and subjects received a $10 gift certificate. Upon completion of the study, they received a $20 gift certificate. Adolescents each wore an actigraph monitor to measure their physical activity and had their blood pressure and waist and hip circumferences measured at all the assessments. All adolescents had their weight and height measured at T0 and T3 because we did not expect weight change will occur in 8 months.
Parental measures
Family information
Parents completed a 12-item questionnaire that asks about parent(s)’ and children’s ages, parents’ weights and heights, parents’ occupation(s), family income, and parents’ levels of education. The questionnaire was written at a third-grade reading level and took approximately 5 minutes to complete.
Acculturation: Suinn-Lew Asian Self-Identity Acculturation Scale (SL-ASIA)
This scale is a 21-item multiple-choice questionnaire that contains items related to language, identity, friendships, behaviors, general and geographic background, and attitudes. The SL-ASIA has moderate to good validity and reliability for Chinese Americans (Cronbach alpha 0.79–.91) [22].
Children’s measures
BMI
BMI was calculated by dividing body mass in kilograms by height in meters squared (kg/m2). BMI has acceptable ranges of sensitivities and specificity. Sensitivity ranged from 29% to 88% and specificity ranged from 94% to 100% in children [23].
Waist-to-hip ratio
The waist-to-hip ratio was derived from the waist and hip circumferences. Waist circumference was measured midway between the lowest rib and the superior border of the iliac crest. Hip circumference was measured at the maximal protrusion of the buttocks. The circumferences were measured to the nearest 0.1 cm.
Blood pressure
Systolic blood pressure and diastolic blood pressure (DBP) were measured to the nearest 2 mm Hg by using a mercury sphygmomanometer with a cuff size appropriate for children (Baumanometer, W. A. Baum Co, Copiague, New York), twice in the adolescent’s right arm, with the adolescent seated after 10 minutes of rest.
Actigraph
The Manufacturing Technologies, Inc, dual-mode actigraph (model 7164) was used to provide valid assessments of physical activity in adolescents [24, 25]. It has high correlations with oxygen consumption (r = 0.78) [24] and direct observations (r = 0.66–0.87) in children [24, 26]. In this study, a 30-second sampling epoch was used. Each monitor was positioned above the iliac crest of the right hip. Adolescents were instructed to wear the actigraph for 7 days. The outcome variables were average counts in moderate and vigorous physical activity. The cutoff point for moderate is 3581 counts per minute and vigorous activity is the count ≥ 6130 counts per minute.
Three-day food diary
Adolescents recorded all foods and beverages and serving sizes consumed for 3 days in a row. A 3-day food diary contains an instruction sheet, a sample completed day’s food-record sheet, and eight blank white dietary record forms. Adolescents were instructed to record food and drink grouped into the following categories: breakfast, snack, lunch, snack, dinner, and snack. Kappa coefficients and percentage agreement for interobserver reliability ranged from 0.43 to 0.91 [27, 28].
Physical activity knowledge
We developed a five-item questionnaire to assess subject’s knowledge about physical activity. Items were adapted from recommendations from the US Department of Agriculture [29] and the AHA [30] regarding MyPyramid, and children’s health. Sample questions included the following: How much aerobic activity is required for a healthy heart? How many hours a day should an adolescent watch television or play video games? The internal consistency in this study was 0.78.
Dietary knowledge
A 14-item survey on dietary knowledge also was part of the Health Behavior Questionnaire developed for the CATCH study [31]. Adolescents were asked to identify which food was “better for your health.” Samples of choices included “whole wheat or white bread” and “frozen corn or canned corn.” This survey had a reported internal consistency ranging from 0.76 to 0.78 [31].
Child dietary self-efficacy
A 15-item self-report questionnaire was used to measure subjects’ self-confidence in their ability to choose foods low in fat and sugar [31]. The questionnaire begin with “How sure are you…?” Items were scored on a Likert scale, with options of “not sure,” “a little sure,” or “very sure.” The internal consistency ranged from 0.82 to 0.87 [31, 32].
Physical activity self-efficacy
This subscale of the Health Behavior Questionnaire was used to measure adolescents’ self-confidence in their ability to participate in various age-appropriate physical activities [31, 32]. The subscale included five items in which subjects were asked if they were “not sure,” “a little sure,” or “very sure” that they could do such things as “keep up a steady pace without stopping for 15 to 20 minutes.” Internal consistency ranged from 0.67 to 0.69 [31, 32].
Data analysis
Descriptive statistics were calculated for demographic characteristics and study variables. We used t tests to examine any differences in variables between intervention and control groups at the baseline. Average login rate was computed as percentage of sessions the subject logged on and completion of activities over the total eight sessions. Linear mixed-effects models that included functions of time and group effects in the repeated data were used to examine change across the four data collection times between groups. The mixed model approach is a method of modeling population parameters as fixed effects while simultaneously modeling individual subject parameters as random effects. We used t tests to examine the efficacy of the intervention on three follow-up times (T0 to T1, T0 to T2, T0 to T3). All analyses were performed in SPSS 17.0.
Power analysis
A minimum of 27 participants per group provides power of 0.80 at an alpha of 0.05 to detect a moderate difference in BMI between the two groups between baseline and 8-month follow-up (mean BMI difference 0.8 between the groups).
Results
Descriptive data
Initially, 63 adolescents and their families agreed to participate in the study; however, 9 children and their families never logged on to the Web site, leaving a total of 54 families. Twenty-seven subjects were each assigned to either the intervention or control group. The mean age of the adolescents was 12.52 (SD, 3.15) years. The intervention group had 16 boys (59%) and the control group had 13 boys (48%) (X2 = 0.67, p = .59). Ten subjects (37%) in the intervention group and 9 (33.3%) in the control group were overweight or obese (X2 = 0.08, p = .99). The mean maternal age was 41.65 (SD, 3.49) years, and the mean number of years of education was 13.3 (SD, 5.00) years. The mean acculturation score was 2.13 (SD, 0.51), suggesting a low acculturation. Approximately 47% of families had an annual household income greater than $60,000 and 40% of the families had an annual household income less than $40,000. The average weekly logon rate was 71.8% (5.74 sessions) for the intervention group and 71.3% (5.7 sessions) for the control group. There was no difference in baseline variables and logon rate between the groups.
Outcomes analyses
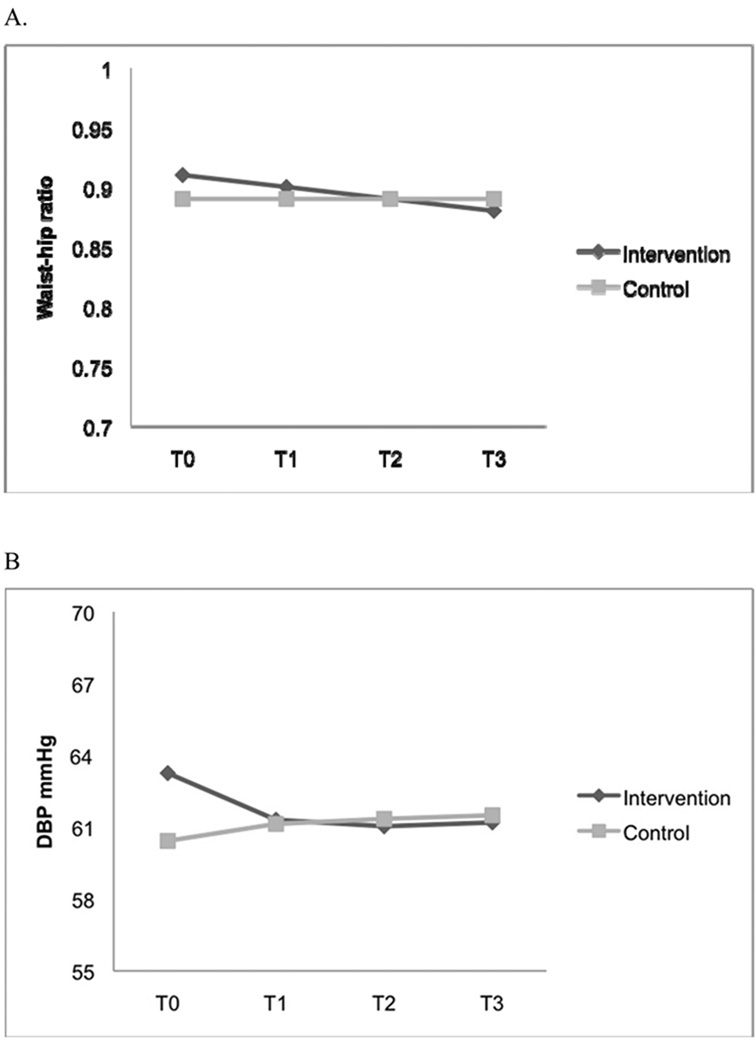
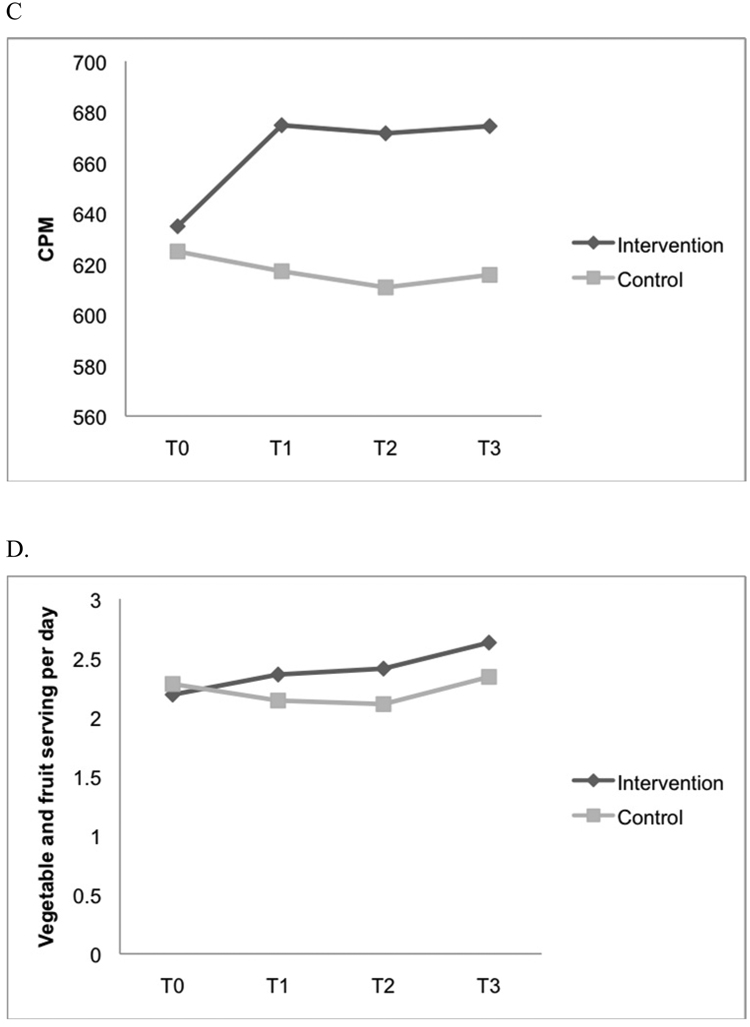
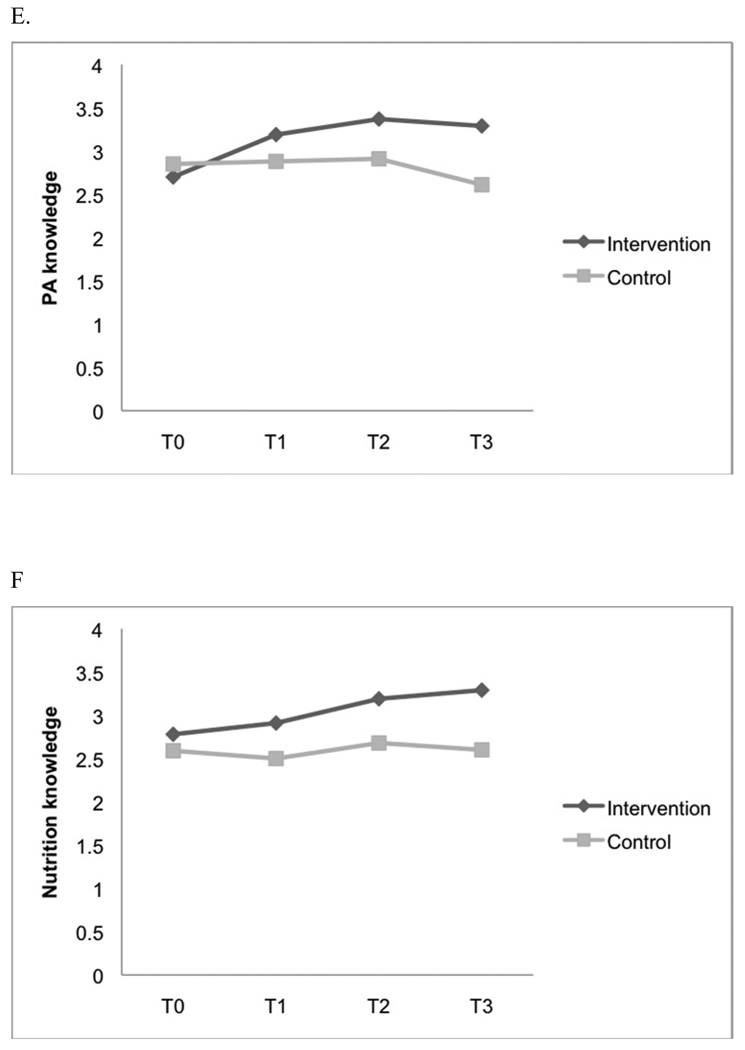
Fifty children and their families (93%) completed baseline and all follow-up measures. No significant differences were found in baseline variables between adolescents who provided follow-up data and adolescents who were lost to follow-up. Table 2 presents follow-up data on outcome variables for the intervention and control groups. Results from the mixed-model analysis indicated that significantly more adolescents in the intervention group than the control group had decreased their waist-to-hip ratio (Effect size= −.01, p = .02) and DBP (Effect size= −1.12, p = .02) while they had increased physical activity as measured by the actigraph (Effect size= 12.46, p = .01), increased vegetable and fruit intake (Effect size= .14, p = .001), and increased knowledge related to physical activity (Effect size= .16, p = .008) and nutrition (Effect size= .18, p = .001) (see Table 3 and Figure 2 for a summary of the mixed-model analysis).
Table 2.
Means and standard deviations for all outcome variables
| Variable | Intervention | Control | ||||||
|---|---|---|---|---|---|---|---|---|
| T0 | T1* | T2* | T3* | T0 | T1* | T2* | T3* | |
| Body mass index** | 20.79 (3.12) | 20.76 (3.08) | 20.25 (3.21) | 20.21 (3.13) | ||||
| Waist-to-hip ratio | 0.91 (0.04) | 0.90 (0.04) | 0.89 (0.04) | 0.88 (0.04) | 0.89 (0.04) | 0.89 (0.04) | 0.89 (0.04) | 0.89 (0.04) |
| Systolic blood pressure | 102.02 (5.9) | 101.92 (6.05) | 101.76 (4.52) | 101.12 (5.72) | 101.13 (4.55) | 100.59 (5.86) | 100.26 (5.40) | 100.0 (6.12) |
| Diastolic blood pressure | 63.26 (8.19) | 61.31 (8.39) | 61.04 (8.41) | 61.20 (8.08) | 60.43 (9.98) | 61.14 (11.44) | 61.35 (9.94) | 61.50 (9.84) |
| Actigraphy results, count per minute | 634.85 (107.07) | 674.72 (76.51) | 671.54 (79.25) | 674.37 (76.52) | 624.89 (110.72) | 617.1 (96.12) | 610.75 (105.47) | 615.67 (106.77) |
| Fat, % | 29.34 (2.42) | 28.37 (2.44) | 28.09 (2.27) | 27.99 (2.04) | 28.34 (2.91) | 27.95 (2.88) | 27.72 (3.29) | 27.78 (2.57) |
| Vegetables and fruit, servings per day | 2.19 (0.48) | 2.36 (0.64) | 2.41 (0.64) | 2.63 (0.71) | 2.28 (0.61) | 2.14 (0.66) | 2.11 (0.55) | 2.34 (0.66) |
| Physical activity knowledge | 2.70 (0.78) | 3.19 (0.68) | 3.37 (0.69) | 3.29 (0.82) | 2.85 (0.82) | 2.88 (0.83) | 2.91 (0.67) | 2.61 (0.71) |
| Nutrition knowledge | 2.74 (0.81) | 2.92 (0.74) | 2.77 (0.71) | 3.04 (0.71) | 2.59 (0.89) | 2.65 (0.94) | 2.82 (0.80) | 2.76 (0.78) |
| Physical activity self-efficacy | 2.55 (0.46) | 2.81 (0.24) | 2.72 (0.23) | 2.72 (0.27) | 2.49 (0.45) | 2.51 (0.34) | 2.39 (0.25) | 2.44 (0.24) |
| Nutrition self-efficacy | 2.59 (0.29) | 2.63 (0.28) | 2.63 (0.26) | 2.59 (0.27) | 2.54 (0.32) | 2.54 (0.30) | 2.36 (0.27) | 2.52 (0.29) |
T1 was 2 months, T2 was 6 months, and T3 was 8 months after the baseline assessment.
Calculated as weight in kilograms divided by height in meters squared.
Table 3.
Summary of mixed model analyses
| Outcomes | Parameter | Effect estimate | 95% confidence interval | p* |
|---|---|---|---|---|
| Body mass index | Time | −0.01 | −0.04, 0.01 | .28 |
| Group | −5.15 | −5.45, −4.85 | .001 | |
| Time × Group | 0.01 | −0.03, 0.04 | .84 | |
| Waist-to-hip ratio | Time | −0.001 | −0.01, 0.001 | .93 |
| Group | 0.01 | −0.01, 0.03 | .34 | |
| Time × Group | −0.01 | −0.01, −0.001 | .02 | |
| Systolic blood pressure | Time | −0.52 | −1.12, 0.10 | .10 |
| Group | 1.19 | −1.65, 1.02 | .41 | |
| Time × Group | 0.17 | −0.66, 1.01 | .69 | |
| Diastolic blood pressure | Time | 0.21 | −0.46, 0.88 | .54 |
| Group | 2.55 | −2.32, 7.73 | .30 | |
| Time × Group | −1.12 | −2.02, 0.21 | .02 | |
| Actigraphy results, count per minute | Time | −2.35 | −6.61, 1.91 | .27 |
| Group | −59.56 | −89.66, −29.45 | .001 | |
| Time × Group | 12.46 | 6.62, 18.41 | .001 | |
| Fat, % | Time | −0.16 | −0.34, 0.02 | .07 |
| Group | 1.02 | −0.03, 2.07 | .06 | |
| Time × Group | −0.24 | −0.49, 0.01 | .06 | |
| Vegetables and fruit, servings per day | Time | 0.01 | −0.05, 0.06 | .84 |
| Group | −0.06 | −0.35, 0.22 | .67 | |
| Time × Group | 0.14 | 0.06, 0.22 | .001 | |
| Physical activity knowledge | Time** | 0.05 | −0.04, 0.13 | .29 |
| Group | 0.01 | −0.33, 0.36 | .94 | |
| Time × Group | 0.16 | 0.04, 0.29 | .008 | |
| Nutrition knowledge | Time | 0.04 | −0.02 0.11 | .20 |
| Group | 0.15 | −0.27, 0.57 | .47 | |
| Time × Group | 0.18 | 0.08, 0.29 | .001 | |
| Physical activity self-efficacy | Time | −0.02 | −0.06, 0.01 | .16 |
| Group | 0.10 | −0.05, 0.25 | .17 | |
| Time × Group | 0.032 | −0.06, 0.12 | .49 | |
| Nutrition self-efficacy | Time | −0.006 | −0.01, 0.006 | .62 |
| Group | 0.08 | −0.08, 0.23 | .34 | |
| Time × Group | 0.004 | −0.009, 0.017 | .55 |
Significant p values are boldfaced.
Figure 2.
Significant changes in (A) waist-to-hip ratio, (B) diastolic blood pressure, (C) actigraphy results, (D) vegetable and fruit intake, (E) physical activity knowledge, and (F) nutrition knowledge.
Follow-up t tests on significant outcome variables revealed that DBP, physical activity, vegetable and fruit intake, and knowledge related to physical activity and nutrition differed significantly between T0 and T1, T0 and T2, and T0 and T3 in the intervention group (p < .05). Waist-to-hip ratio also differed significantly (p < .05) between T0 and T2 and between T0 and T3 in the intervention group. No outcome variables differed significantly in the control group.
Discussion
The results suggest that an Internet-facilitated, family-based, and theory-driven program for prevention of childhood obesity can decrease waist-to-hip ratio and DBP while improving physical activity, vegetable and fruit intake, and knowledge about food intake and physical activity over a course of 8 months in Chinese American adolescents.
The involvement of parents is critical to overweight management in children. Our Web-based program included information for parents related to their adolescent’s weight-related health behaviors (eating, physical activity, and coping) and way to improve these behaviors and healthy lifestyles and healthy weight. Other studies had suggested that parental involvement can improve healthy weight in children and adolescents [33–35]. As Chinese parents are typically heavily involved in every aspect of their children’s lives, the involvement of parents in a healthy lifestyle and healthy weight program is imperative [36].
Although we did not find a reduction in BMI, the waist-to-hip ratio and DBP were decreased significantly in the intervention group. The possible explanation for no difference was found in BMI could due to short follow up time (only 6 months). Future study needs to examine the impact of health lifestyles intervention with longer follow up. Nonetheless, our intervention suggests that improvements in DBP last 6 months after the intervention. Maintaining healthy weight and healthy lifestyle in adolescents is critical in improving their cardiovascular health.
Adolescents in the intervention group also increased vegetable and fruit intake and physical activity level in all follow-up assessments in the study. Moreover, we found that children in the intervention group also improved their knowledge about physical activity and nutrition. Results of this study are consistent with results of other studies that indicated that Web-based interventions can improve food intake and physical activity in children and adolescents [11, 18, 37]. The successful of the program in improving adolescents’ weight-related health behaviors and knowledge may be attributable to the interactive nature and individualization of the Web-based program. The Web-based program includes several components that involve setting realistic and achievable goals, and monitoring eating and physical activity in the form of documenting number of steps reported per day via our secure Web site. Thus, intervention for healthy weight management in Chinese American adolescents should incorporate information related to adequate diet and active lifestyles and should be tailored to the individual’s needs.
Although this study is one of the first to examine the feasibility and efficacy of a Web-based behavioral intervention program for Chinese American adolescents and their families, we acknowledge several limitations. These limitations include convenience sampling, parents with high education, use of self-report measures, involving only Chinese American adolescents, and follow-up for only 6 months after the intervention. In addition, the use of food diary for recording dietary intake in adolescents needs to be examined for its reliability and validity. Future research should examine the long-term effects of this program on weight-related health behaviors and other related cardiovascular functions as well.
In conclusion, the results of this study indicate significant improvements in waist-to-hip ratio, DBP, fruit and vegetable intake, and physical activity in Chinese American adolescents; all proxies for improved general health. Given the significant impact of being overweight on Chinese American adolescents’ health and the high financial cost of running an individual or group consulting program for behavioral change and weight management, a Web-based behavioral program can involve more families who may not otherwise be able to participate—and at substantially lower total cost.
Acknowledgments
Source for support: This publication was made possible by grant number KL2 RR024130 to J.L.C. from the National Center for Research Resources, a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research, Hellman research grant, and in part by NIH grant DK060617 to M.B.H.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Moya M. An update in prevention and treatment of pediatric obesity. World J Pediatr. 2008;4(3):173–185. doi: 10.1007/s12519-008-0033-7. [DOI] [PubMed] [Google Scholar]
- 2.Au L, et al. Prevalence of overweight and obesity in Chinese American children in New York City. J Immigr Minor Health. 2009;11(5):337–341. doi: 10.1007/s10903-009-9226-y. [DOI] [PubMed] [Google Scholar]
- 3.Daniels SR. Complications of obesity in children and adolescents. Int J Obes (Lond) 2009;33 Suppl 1:S60–S65. doi: 10.1038/ijo.2009.20. [DOI] [PubMed] [Google Scholar]
- 4.Schuster DP. Changes in physiology with increasing fat mass. Semin Pediatr Surg. 2009;18(3):126–135. doi: 10.1053/j.sempedsurg.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Stevens J. Ethnic-specific revisions of body mass index cutoffs to define overweight and obesity in Asians are not warranted. Int J Obes Relat Metab Disord. 2003;27(11):1297–1299. doi: 10.1038/sj.ijo.0802417. [DOI] [PubMed] [Google Scholar]
- 6.Tan CE, et al. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care. 2004;27(5):1182–1186. doi: 10.2337/diacare.27.5.1182. [DOI] [PubMed] [Google Scholar]
- 7.Trasande L, Chatterjee S. The impact of obesity on health service utilization and costs in childhood. Obesity (Silver Spring) 2009;17(9):1749–1754. doi: 10.1038/oby.2009.67. [DOI] [PubMed] [Google Scholar]
- 8.Daniels SR. The consequences of childhood overweight and obesity. Future Child. 2006;16(1):47–67. doi: 10.1353/foc.2006.0004. [DOI] [PubMed] [Google Scholar]
- 9.Rydell SA, et al. Use of a Web-based component of a nutrition and physical activity behavioral intervention with Girl Scouts. J Am Diet Assoc. 2005;105(9):1447–1450. doi: 10.1016/j.jada.2005.06.027. [DOI] [PubMed] [Google Scholar]
- 10.Thompson D, et al. Boy Scout 5-a-Day Badge: outcome results of a troop and Internet intervention. Prev Med. 2009;49(6):518–526. doi: 10.1016/j.ypmed.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Thompson D, et al. Food, fun, and fitness internet program for girls: pilot evaluation of an e-Health youth obesity prevention program examining predictors of obesity. Prev Med. 2008;47(5):494–497. doi: 10.1016/j.ypmed.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Wantland DJ, et al. The effectiveness of Web-based vs. non-Web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res. 2004;6(4):e40. doi: 10.2196/jmir.6.4.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doyle AC, et al. Reduction of overweight and eating disorder symptoms via the Internet in adolescents: a randomized controlled trial. J Adolesc Health. 2008;43(2):172–179. doi: 10.1016/j.jadohealth.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williamson DA, et al. Two-year internet-based randomized controlled trial for weight loss in African-American girls. Obesity (Silver Spring) 2006;14(7):1231–1243. doi: 10.1038/oby.2006.140. [DOI] [PubMed] [Google Scholar]
- 15.Chen JL, Kennedy C. Cultural variations in children's coping behaviour, TV viewing time, and family functioning. Int Nurs Rev. 2005;52(3):186–195. doi: 10.1111/j.1466-7657.2005.00419.x. [DOI] [PubMed] [Google Scholar]
- 16.Chen JL, Kennedy C. Family functioning, parenting style and Chinese children's weight status. Journal of Family Nursing. 2004;10:186–195. [Google Scholar]
- 17.Kalarchian MA, et al. Family-based treatment of severe pediatric obesity: randomized, controlled trial. Pediatrics. 2009;124(4):1060–1068. doi: 10.1542/peds.2008-3727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cullen KW, Thompson D. Feasibility of an 8-week African American web-based pilot program promoting healthy eating behaviors: Family Eats. Am J Health Behav. 2008;32(1):40–51. doi: 10.5555/ajhb.2008.32.1.40. [DOI] [PubMed] [Google Scholar]
- 19.Wadden TA, Butryn ML, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology. 2007;132(6):2226–2238. doi: 10.1053/j.gastro.2007.03.051. [DOI] [PubMed] [Google Scholar]
- 20.Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviors. Prog Behav Modif. 1992;28:183–218. [PubMed] [Google Scholar]
- 21.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 22.Suinn RM. Measurement of Acculturation of Asian Americans. Asian Am Pac Isl J Health. 1998;6(1):7–12. [PubMed] [Google Scholar]
- 23.Freedman DS, Perry G. Body composition and health status among children and adolescents. Preventive Medicine. 2000;31:34–53. [Google Scholar]
- 24.Eston RG, Rowlands AV, Ingledew DK. Validity of heart rate, pedometry, and accelerometry for predicting the energy cost of children's activities. J Appl Physiol. 1998;84(1):362–371. doi: 10.1152/jappl.1998.84.1.362. [DOI] [PubMed] [Google Scholar]
- 25.Trost SG, et al. Validity of the computer science and applications (CSA) activity monitor in children. Med Sci Sports Exerc. 1998;30(4):629–633. doi: 10.1097/00005768-199804000-00023. [DOI] [PubMed] [Google Scholar]
- 26.Kelly L, Reilly J, Fairweather S, Barrie S, Grant S, Paton J. Comparison of two accelerometers for assessment of physical activity in preschool children. Pediatric Exercise Science. 2004;16:324–333. [Google Scholar]
- 27.Baxter SD. Accuracy of fourth-graders' dietary recalls of school breakfast and school lunch validated with observations: in-person versus telephone interviews. J Nutr Educ Behav. 2003;35(3):124–134. doi: 10.1016/s1499-4046(06)60196-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weber JL, et al. Validity of self-reported dietary intake at school meals by American Indian children: the Pathways Study. J Am Diet Assoc. 2004;104(5):746–752. doi: 10.1016/j.jada.2004.02.029. [DOI] [PubMed] [Google Scholar]
- 29.United States Department of Agriculture (USDA) Steps to a healthier you. 2006
- 30.Association AH, editor. Children’s Health. Dallas, TX: American Heart Association; 2006. [Google Scholar]
- 31.Edmundson E, et al. The effects of the Child and Adolescent Trial for Cardiovascular Health upon psychosocial determinants of diet and physical activity behavior. Prev Med. 1996;25(4):442–454. doi: 10.1006/pmed.1996.0076. [DOI] [PubMed] [Google Scholar]
- 32.Matheson DM, et al. Children's food consumption during television viewing. Am J Clin Nutr. 2004;79(6):1088–1094. doi: 10.1093/ajcn/79.6.1088. [DOI] [PubMed] [Google Scholar]
- 33.Golan M, Kaufman V, Shahar DR. Childhood obesity treatment: targeting parents exclusively v. parents and children. Br J Nutr. 2006;95(5):1008–1015. doi: 10.1079/bjn20061757. [DOI] [PubMed] [Google Scholar]
- 34.Vignolo M, et al. Five-year follow-up of a cognitive-behavioural lifestyle multidisciplinary programme for childhood obesity outpatient treatment. Eur J Clin Nutr. 2007 doi: 10.1038/sj.ejcn.1602819. [DOI] [PubMed] [Google Scholar]
- 35.Chen JL, et al. Efficacy of a child-centred and family-based program in promoting healthy weight and healthy behaviors in Chinese American children: a randomized controlled study. J Public Health (Oxf) 2010;32(2):219–229. doi: 10.1093/pubmed/fdp105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen JL, Kennedy C. Factors associated with obesity in Chinese-American children. Pediatr Nurs. 2005;31(2):110–115. [PubMed] [Google Scholar]
- 37.Jago R, et al. Fit for Life Boy Scout badge: outcome evaluation of a troop and Internet intervention. Prev Med. 2006;42(3):181–187. doi: 10.1016/j.ypmed.2005.12.010. [DOI] [PubMed] [Google Scholar]