Abstract
Examined the effects of a home-based intervention on mother–infant interaction among drug-using women and their infants. At 2 weeks postpartum, mothers and infants were randomly assigned to either an intervention (n = 84) or a control (n = 87) group. Control families received brief monthly tracking visits, and intervention families received weekly visits by trained lay visitors. Mother–infant interaction was evaluated at 6 months through observation of feeding. Although there were no direct effects of the intervention, in the control group, mothers who continued to use drugs were less responsive to their babies than mothers who were drug free. In the intervention group, drug use was not associated with maternal responsiveness. Weekly home-based intervention may be a protective strategy for children of drug-using women because it disrupts the relation between ongoing maternal drug use and low maternal responsiveness.
Drug abuse among women is often associated with a chaotic caregiving environment (Butz, Lears, O’Neil, & Lukk, 1998), placing infants at significant risk for poor outcome because of prenatal drug exposure and nonresponsive parenting. Maternal substance abuse has been associated with domestic abuse (Amaro, Fried, Cabral, & Zuckerman, 1990), child abuse (Kelley, 1992; Leventhal et al., 1997), and attachment problems (Kelley, 1992), yet the research findings on the parenting of drug-using mothers are contradictory. Some researchers have found that drug-using mothers show less enjoyment and enthusiasm compared with nondrug-using mothers (Burns, Chethik, Burns, & Clark, 1997), and others have found no differences in maternal behavior (Black, Schuler, & Nair, 1993; Schuler, Black, & Starr, 1995).
The focus of much of the research on drug-using mothers and their infants has been on the short- and long-term effects of prenatal drug exposure. Few researchers have examined the impact of ongoing maternal drug use on parenting ability or infant outcome. Although maternal drug use beyond the neonatal period has been measured by using urine analysis and hair analysis (Callahan et al., 1992; Graham, Koren, Klein, Schneiderman, & Greenwald, 1989), the majority of studies have used maternal report even though the accuracy of this method has been questioned (Zuckerman et al., 1989). Regardless of how it is assessed, drug addiction is a chronic relapsing disease. Women who continue to use drugs often are unable to provide a consistent, nurturing environment for their children (Hawley, Halle, Drasin, & Thomas, 1995; Zuckerman, 1994). Drug-exposed children raised in homes with ongoing maternal drug use are more likely to display problems in cognitive development at 3 years than drug-exposed children raised in drug-free environments (Griffith, Azuma, & Chasnoff, 1994). This relation may be at least partially explained by drug-using parents’ inability to provide a stable, nurturing environment (Zuckerman, 1993), together with low levels of positive maternal and infant behaviors during mother–infant interaction.
Interventions often are designed to help mothers identify and implement coping strategies that will enhance their parenting skills and improve the outcome of the children in high-risk families. Results from a multisite, randomized trial indicate that at 3 years, premature infants in a comprehensive early intervention had better cognitive and behavioral outcomes (Infant Health and Development Program [IHDP], 1990). Other research from the IHDP indicates that the intervention led to more positive maternal and child behavior during mother–child interaction at 30 months (Spiker, Ferguson, & Brooks-Gunn, 1993).
Home- and center-based intervention programs have been used with drug-using parents and their children. Home-based intervention programs with drug-using women often use community health nurses to provide a child development curriculum and assistance with maternal social needs (Black et al., 1994; Hofkosh et al., 1995). These home-based interventions over the first 12 to 18 months postpartum led to better mother–infant interaction (Hofkosh et al., 1995), higher infant cognitive scores, and a more stimulating and responsive home environment (Black et al., 1994) in comparison with control infants. Among adolescent drug-using mothers, one successful center-based program included drug treatment and parenting and vocational classes. This center-based program led to better mother–infant interaction scores and higher infant cognitive scores in comparison with control group mothers and infants (Field et al., 1998). A combined home-based and parenting skills training program with opiate-addicted parents increased positive involvement and communication between the parents and their children, despite ongoing drug use in 20% of the parents (Catalano, Haggerty, Gainey, & Hoppe, 1997).
In summary, the research indicates that ongoing maternal drug use and the effects of an intervention program may be associated with infant and maternal outcomes. Ongoing maternal drug use negatively affected cognitive outcomes among drug-exposed children (Griffith et al., 1994), but few researchers have examined how ongoing maternal drug use affects behavior during mother–infant interaction. Home- and center-based interventions led to more positive behavior during mother–infant interaction (Field et al., 1998; Hofkosh et al., 1995; Spiker et al., 1993). Finally, the research suggests that there might be an interaction between ongoing maternal drug use and intervention group status. Ongoing maternal drug use without an intervention led to lower cognitive scores in children (Griffith et al., 1994), but an intervention led to more positive involvement and communication between parents and children despite ongoing parental drug use (Catalano et al., 1997).
The purpose of this research was to compare mother–infant interaction among drug-using mothers who did and did not receive a home-based intervention. First, we hypothesized that mothers and infants in the intervention group would display significantly more positive behaviors during mother–infant interaction than mothers and infants in the control group. Second, based on previous research, we hypothesized that intervention group status and ongoing maternal drug use would be related to maternal and infant behavior during mother–infant interaction. Finally, because previous research indicates that drug-affected families benefitted from an intervention despite ongoing parental drug use, we hypothesized that regardless of ongoing maternal drug use, mothers and infants in the intervention group would display more positive behavior.
Method
Participants
Participants were part of an ongoing longitudinal randomized clinical trial among drug-using women and their infants. They were recruited from a university hospital that serves a largely inner-city African American population. Women were eligible for recruitment if they or their infants had a positive urine toxicology screen at birth or if a history of recent drug use was noted in the medical charts. Infants who were not discharged into the care of their mothers were not eligible. Infants who had serious developmental or congenital problems that required special services (e.g., spina bifida) were not eligible because the services received by the infants often included a home-visiting component, which would have interfered with the randomization in this study.
Of the drug-using women who were approached about participating in the study, 28% declined to participate. The mothers who declined to participate did so for various reasons: 41% said they were not interested in participating, 17% denied drug use, 27% preferred to receive primary pediatric care at another site, and 15% declined for other reasons (the baby’s father refused, they had a transportation problem, or the mother was in another research program).
Available Data
This study included 171 families (87 control, 84 intervention). Thirty-one dyads were lost before the 2-week baseline visit, and 32 additional families were lost after the 2-week visit (see Table 1). Thus, 192 (97 control, 95 intervention) families were seen for the 6-month evaluation visit. Observation data were dropped from 13 families because the interaction involved a caretaker other than the mother, and data from 8 families were lost because of mechanical difficulties (the camera was out of focus or knocked off balance). There were no significant group differences on any maternal demographic or infant perinatal variables between dyads included in this study and those dyads that were not.
Table 1.
Reasons for Subject Loss Before and After 2-week Baseline Visit
| Before 2-Week Visita | After 2-Week Visitb | |
|---|---|---|
| Infant Died | 1 | 3 |
| Infant in Foster Care | 9 | 9 |
| Family Not Found | 4 | 6 |
| Family Withdrew | 2 | 0 |
| Family Noncompliant | 15 | 0 |
| Family Moved Out of State | 0 | 2 |
| Error in Recruitment | 0 | 3 |
| Mother Entered Long-Term Residential Drug Treatment | 0 | 1 |
| Noncompliant With Scheduled Visit | 0 | 8 |
n = 31.
n = 32.
Home Visiting
One full-time African American lay visitor was recruited to visit the control families. Mothers in the control group received brief monthly home tracking visits to reduce attrition. The mean number of home visits made to the control families during the first 6 months was 2.7 (SD = 1.7, range = 0–7), and the mean length was 16.6 min (SD = 5.4). The control worker met with a psychologist and a pediatrician for bimonthly supervisory meetings.
Mothers in the intervention group received weekly home visits during the first 6 months postpartum from one of two full-time lay visitors. The visitors were two middle-age African American women who had previous experience making home visits and knew the community where the mothers lived. The visitors shared the caseload of families, but each visitor was assigned to specific families. The mean number of visits made during the first 6 months was 8.9 (SD = 5.6, range = 0–23), and the mean length was 30.1 min (SD = 5.8). The intervention visitors met with a psychologist and a pediatrician weekly to track the progress of the families and to discuss concerns about the families.
Home Intervention Protocol
The home intervention was developmentally oriented and was based on the program used by the IHDP (1990). The IHDP program had three components: home-based intervention starting in the first year, child attendance at a child development center, and parent group meetings starting the second year postpartum. The focus in this article is on the home-visiting protocol and parent–infant interaction at 6 months of age.
As specified in the IHDP program, the home intervention had both a parent and an infant component. However, because the IHDP program was not focused on drug-using parents, we added information about drug use and drug treatment to the content of the home intervention. The goal of the parent component was to increase maternal empowerment by enhancing the mothers’ ability to manage self-identified problems by using existing services and family and social supports. The topics covered during the maternal component included housing, public assistance programs (e.g., Supplementary Nutritional Services to Women, Infants, and Children), partner abuse, and the effects of drug use and drug treatment. To establish consistency in the content of the home visit, we created a Personal Contact Form. The contact form documented the time spent with the family and the content and quality of the contact. It also contained information about the four levels of contact used during the maternal home intervention: relationship building between the mother and home visitor, caretaker’s personal problems/concerns, infant development, and health education.
The goal of the infant component was to promote infant development by using a program of games and activities. The home visitors were trained to use the HELP at Home: Hawaii Early Learning Profile (1991), which is a comprehensive curriculum containing 650 developmental skills for children ages birth to 36 months. An activity sheet to use as a guide to help parents learn about child development accompanies each developmental skill. The home visitors modeled the behavior/activity on the sheet. By teaching mothers appropriate ways to play with their infants, our goal was to enhance communication between mothers and infants and to help the mothers provide a developmentally stimulating play environment.
Measures
Drug use
All the mothers in this study had a history of cocaine and/or heroin use. At the 6-month evaluation visit, mothers were asked about their prior and current use of cigarettes, alcohol, heroin, cocaine, marijuana, tranquilizers, amphetamines, barbiturates, and methadone. Mothers who reported that they had continued using cocaine and/or heroin in the last 6 months were given a score of 1. Mothers reporting that they had stopped using heroin and cocaine were given a score of 0. Marijuana and alcohol use were coded the same way (0 = no use, 1 = use).
Mother–infant interaction
We assessed maternal and infant behavior by using videotaped observations of mothers and infants during feeding at 6 months. We used a feeding interaction rather than play because infants and mothers spend much of their time feeding, and feeding often elicits more behavioral extremes than does play (Black, Hutcheson, Dubowitz, Starr, & Berenson-Howard, 1996). We scored the mother–infant interactions by using rating scales (Cowan & Cowan, 1992) that were used previously in a population of at-risk, inner-city, African American families (Hutcheson et al., 1997). These scales are based on the quality of the parent–child interaction; thus, they are not tied to specific age-related behaviors in the child (P. Cowan, personal communication, September 23, 1999). For example, parental warmth is based on a range of behaviors that include the parent demonstrating affection, laughing, hugging, and touching the child; a feeling of connection between parent and child; and the parent providing reassurance, encouragement, and a generosity of affect. Each item on the parent rating scale and infant rating scale represented a global rating of the behavior during the 10-min interaction. Items were scored on a 5-point scale ranging from 1 (very low) to 5 (excessive). Because both very low and very high scores were nonoptimal, the high nonoptimal scores were recoded before the analyses so that high scores represented the most positive interactions.
We dropped two maternal behaviors (limit-setting, maturity demands) and eight child behaviors (compliance, defiance, anxiety, planfulness, persistence, creativity, precision in language, shyness) because they were not appropriate for use with 6-month-olds. The remaining 17 maternal behaviors were pleasure, displeasure, respect, confidence, expressiveness, precision in language, structure, warmth, coldness, anger, responsiveness, interactiveness, creativity, activity level, happiness, sadness, and anxiety. The remaining 14 infant behaviors were warmth, coldness, dependency, autonomy, anger, enthusiasm, frustration, expressiveness, curiosity, activity level, interactiveness, attentiveness, happiness, and sadness. Cronbach’s alpha was used to measure the internal consistency of the remaining maternal and infant behaviors. The alpha coefficients were .95 and .90, respectively.
Trained coders who were unaware of the purpose of the research or the intervention status of the families scored the videotapes. There were two independent groups of coders; one group coded maternal behavior, and the other group coded child behavior. All coders were trained until they reached over 90% reliability on the scales, and reliability was maintained through weekly reliability checks. Reliability was defined as no more than a 1-point difference among the coders. Approximately 10% of the tapes were used for reliability checks for parent behavior, and the interrater agreement ranged from .82 to .99. Approximately 12% of the tapes were used for reliability checks for infant behavior, and the interrater agreement ranged from .79 to .98.
Procedure
Eligible mothers were approached in the hospital shortly after giving birth. Mothers who agreed to participate signed a consent form approved by the Institutional Review Board of the University of Maryland and completed a short demographic and tracking form, administered orally. The mothers were given an appointment for a 2-week baseline visit. At the end of the baseline visit, the mothers were assigned randomly to the intervention or control group. Research assistants who were unaware of the intervention status of the mothers and infants conducted all evaluation visits in a hospital clinic. All mothers were given information on drug treatment programs; however, treatment was not mandatory to participate in the study. Mothers were paid for each clinic evaluation visit and were given bus tokens to get home.
As part of the 6-month evaluation visit, the mothers completed measures assessing maternal drug use over the last 6 months, and the mother–infant dyads were videotaped for 10 min during feeding. Baby food, a high chair, a table, and several adult chairs were provided. Mothers were instructed to feed their infant using the method they used at home (e.g., high chair or holding in their laps). The camera was in the room, but an operator was not present.
Results
We ran two principal components analyses to reduce the number of maternal and infant interaction dimensions. Only those dimensions with factor loadings above .50 were retained. Five maternal dimensions were selected to form a maternal responsiveness factor: responsiveness, confidence, structure, lack of anger, and lack of anxiety (factor loadings ranged from .52 to .74). Eight infant dimensions were selected to form an infant warmth factor: warmth, enthusiasm, interactiveness, happiness, curiosity, lack of coldness, lack of anger, and lack of frustration (factor loadings ranged from .53 to .83). The eigenvalues for both factors exceeded 1. The correlation between maternal responsiveness and infant warmth was .38 (p < .01), indicating modest overlap.
The analyses in this study are based on intention to treat rather than the amount of intervention received (Meinert, 1986), because this method provides a conservative estimate of the intervention effect. Thus, mothers who were randomized into the intervention group were retained in that group, even if they refused all intervention (n = 6). We used multivariate analysis of variance and chi-square analyses to determine if there were significant group (control vs. intervention) differences. There were no significant group differences on any maternal demographic or infant perinatal variable (see Table 2). At 6 months, there were no significant group differences on maternal responsiveness or infant warmth, Fs(2, 171) < 1.0, ps > .05 (see Table 3). There were no significant group differences in use of existing services at 6 months, χ2s(1, N = 171) < 1.8, ps > .05, except that significantly more control mothers reported being currently involved with Protective Services, χ2(1, N = 171) = 9.2, p < .01 (see Table 3).
Table 2.
Maternal Demographic and Infant Perinatal Variables Among the Control and Intervention Groups
| Controla |
Interventionb |
|||
|---|---|---|---|---|
| M | SD | M | SD | |
| Maternal Variables | ||||
| Maternal Age (Years) | 27.1 | 5.2 | 27.0 | 5.2 |
| Maternal Education (Years) | 10.9 | 1.6 | 10.9 | 1.4 |
| Age at First Pregnancy (Years) | 18.7 | 4.3 | 18.2 | 3.8 |
| % Single | 96.4 | 91.7 | ||
| % Unemployed | 97.7 | 100.0 | ||
| % African American | 97.7 | 94.0 | ||
| Infant Variables | ||||
| Birth Weight (gm) | 2,784 | 497 | 2,812 | 483 |
| Head Circumference (cm) | 32.7 | 1.8 | 33.0 | 2.3 |
| Birth Length (cm) | 47.4 | 6.1 | 47.8 | 2.8 |
| Gestational Age (Weeks) | 38.8 | 2.3 | 38.3 | 2.1 |
| 1-min Apgar | 8.1 | 1.1 | 7.9 | 1.2 |
| 5-min Apgar | 8.9 | 0.3 | 8.9 | 0.5 |
| % Male | 48.9 | 44.0 | ||
| % Preterm (<37 Weeks) | 11.2 | 17.6 | ||
n = 87.
n = 84.
Table 3.
Group Differences on Dependent, Predictor, and Outcome Variables Measured at the 6-Month Visit
| Controla |
Interventionb |
|||
|---|---|---|---|---|
| M | SD | M | SD | |
| Maternal Responsivenessc | 3.3 | 0.4 | 3.6 | 0.4 |
| Infant Warmthc | 2.5 | 0.4 | 2.5 | 0.4 |
| Substance Use (%) in Past 6 Months | ||||
| Alcohol | 68.0 | 64.8 | ||
| Marijuana | 37.8 | 25.4 | ||
| Cocaine and/or Heroin | 44.0 | 45.6 | ||
| Families Receiving Services in the Last 6 Months (%) | ||||
| AFDC | 85.1 | 89.3 | ||
| Medical Assistance | 93.1 | 91.7 | ||
| WIC | 89.7 | 95.2 | ||
| Food Stamps | 87.4 | 91.7 | ||
| Protective Services | 31.0 | 11.9* | ||
Note: AFDC = Aid to Families With Dependent children; WIC = Supplementary Nutritional Services to Women, Infants, and Children.
n = 87.
n = 84.
Higher scores optimal.
p < .01.
At 6 months, there were no significant group differences in cocaine and/or heroin use, alcohol use, χ2s(1, N = 146) < 1, ps >.05, or marijuana use, χ2(1, N = 146) = 2.6, p >.05, during the last 6 months (see Table 3). However, as Table 3 indicates, 44% of the control mothers and 46% of the intervention mothers reported ongoing cocaine and/or heroin use at 6 months. In addition, 68% of the control mothers and 65% of the intervention mothers reported ongoing alcohol use. Finally, 38% of the control mothers and 25% of the intervention mothers reported ongoing marijuana use.
We used two hierarchical multiple linear regression analyses to examine the association among group status (control vs. intervention), ongoing maternal drug use, and mother or infant behavior during feeding. Maternal age, infant birth weight, and infant sex were correlated with either maternal responsiveness or infant warmth. Therefore, as a means of controlling for these variables, they were entered on the first step in both regressions.
In the first hierarchical multiple linear regression, the dependent variable was maternal responsiveness. Maternal age, infant birth weight, and infant sex were entered on the first step. Group status (control vs. intervention) was entered on the second step. To prevent ongoing marijuana and alcohol use from being confounded with the effects of ongoing cocaine and/or heroin use, we entered marijuana and alcohol use in the third step. Then ongoing drug use was entered, followed by the Group × Ongoing Drug Use interaction. The interaction of Group × Ongoing Drug Use was entered to examine whether the association between ongoing drug use and maternal responsiveness differed for those in the intervention and control groups. The overall equation was significant, F(8, 136) = 3.8, p < .01. There were two significant predictors of maternal responsiveness: infant birth weight, F(3, 141) = 5.0, p < .01, and the interaction of group status and ongoing drug use, F(1, 136) = 9.9, p < .01 (see Table 4).
Table 4.
Summary of Hierarchical Regression Analysis for Variables Predicting Maternal Responsiveness
| Variable | B | SE B | β |
|---|---|---|---|
| Step 1 | |||
| Infant Birth Weight | .0002 | .000 | .229* |
| Maternal Age | .0078 | .006 | .113 |
| Child Sex | .1280 | .060 | .113 |
| Step 2 | |||
| Group | .0562 | .058 | .078 |
| Step 3 | |||
| Alcohol Use | .0432 | .064 | .057 |
| Marijuana Use | .0015 | .065 | .002 |
| Step 4 | |||
| Ongoing Drug Use | −.1000 | .060 | −.138 |
| Step 5 | |||
| Group × Ongoing Drug Use | .3590 | .114 | .815* |
Note: Total R2 = .18, F(8, 136) = 3.81, p < .01. R2 = .10 for Step 1; R2 change = .01 for Step 2; R2 change = .01 for Step 3; R2 change = .02 for Step 4; R2 change = .06 for Step 5.
p < .01.
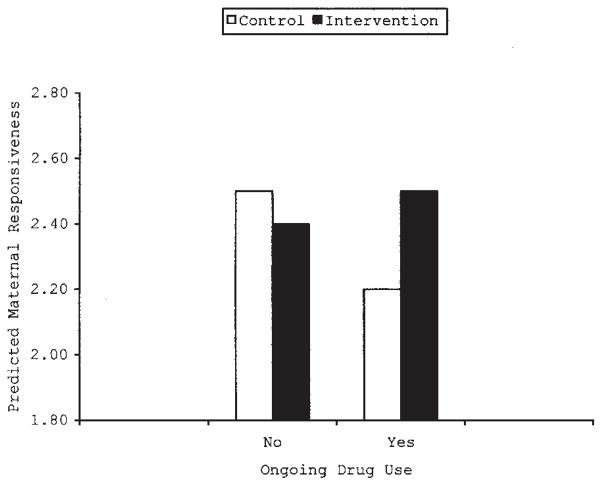
To interpret the interaction of group status and ongoing maternal drug use, we graphed the data (Cohen & Cohen, 1983). As Figure 1 shows, in the control group, maternal responsiveness was lower among mothers who continued to use cocaine and/or heroin. In contrast, among intervention mothers, maternal responsiveness did not differ between those who did and did not continue drug use (see Figure 1).
Figure 1.
Predicting maternal responsiveness from group membership (control vs. intervention) and ongoing maternal drug use (no vs. yes) using multiple regression analysis.
In the second hierarchical multiple linear regression, infant warmth was the dependent variable. Maternal age, infant birth weight, and infant sex were entered on the first step. Group status (control vs. intervention) was entered on the second step. To prevent ongoing marijuana and alcohol use from being confounded with the effects of ongoing cocaine and/or heroin use, marijuana and alcohol use were entered in the third step. Then ongoing drug use was entered, followed by the Group × Ongoing Drug Use interaction. We entered the interaction of Group × Ongoing Drug Use to examine whether the association between ongoing drug use and infant warmth differed for those in the intervention and control groups. The overall equation was significant, F(8, 136) = 3.2, p < .01. Infant birth weight was a significant predictor of infant warmth, F(3, 141) = 6.6, p < .01, but no other variable entered the equation (see Table 5).
Table 5.
Summary of Hierarchical Regression Analysis for Variables Predicting Infant Warmth
| Variable | B | SE B | β |
|---|---|---|---|
| Step 1 | |||
| Infant Birth Weight | .0003 | .000 | .346* |
| Maternal Age | .0016 | .006 | .022 |
| Child Sex | .0725 | .061 | .096 |
| Step 2 | |||
| Group | .0640 | .059 | .085 |
| Step 3 | |||
| Alcohol Use | .0702 | .065 | .089 |
| Marijuana Use | −.0151 | .066 | −.019 |
| Step 4 | |||
| Ongoing Drug Use | .0562 | .061 | .075 |
| Step 5 | |||
| Group × Ongoing Drug Use | .1890 | .120 | .414 |
Note: Total R2 = .16, F(8, 136) = 3.19, p < .01. R2 = .12 for Step 1; R2 change = .01 for Step 2; R2 change = .01 for Step 3; R2 change = .01 for Step 4; R2 change = .02 for Step 5.
p < .01.
Discussion
Despite a relatively intensive intervention, the intervention had no overall effects on maternal responsiveness or infant warmth at 6 months. Although there were no direct effects, there was an association between ongoing maternal drug use and maternal responsiveness during mother–infant interaction, which differed by group. In the control group, mothers who continued to use drugs were less responsive to their babies than were mothers who were drug free. In the intervention group, drug use was not associated with maternal responsiveness. Other research also indicates that an intervention leads to more positive parenting among drug-using mothers (Black et al., 1994; Field et al, 1998).
Contrary to expectations, the intervention had no effect on maternal responsiveness during mother–infant interaction. This contradicts previous research that indicates that an intervention with drug-using women leads to better maternal interaction behavior (Field et al., 1998) and more positive parenting (Catalano et al., 1997). However, the caregivers in the previous studies were involved in drug treatment programs, and neither study used a home-based intervention exclusively. Research indicates that the home environments of drug-using women are disorganized and lack stability (Butz et al., 1998). Drug-using women are exposed to multiple negative risk factors such as violence, negative life events, and depression (Kettinger, Nair, & Schuler, 2000). In addition, all the families in this study continued to live in poverty, which is associated with higher family stress, maternal depression, and inadequate social support (Parker, Greer, & Zuckerman, 1988). The overwhelming effects of poverty and ongoing maternal drug use may blunt the effects of the home intervention on maternal responsiveness.
The findings on infant warmth contradict research that indicates the beneficial effects of an intervention on infant interaction at 6 months among drug-exposed infants (Field et al., 1998). However, the infants in the Field et al. study were in center-based day care 5 days a week, whereas this study included only a home-visiting component at this age. Similar to other home-visiting programs with poor families living in the inner city (Hardy & Streett, 1989), the home visitors had a difficult time focusing on the specific components of the intervention. They spent a great deal of time dealing with the day-to-day crises these families faced such as housing problems, lack of electricity, no money, no food, and abusive relationships.
Although the intervention had no effect on either maternal responsiveness or infant warmth during mother–infant interaction at 6 months, the home-based intervention disrupted the relation between ongoing maternal drug use and low maternal responsiveness in the intervention group. Research indicates that drug-using mothers exposed to a high number of risk factors, such as depression, had poorer parenting attitudes than drug-using mothers exposed to a low number of risk factors (Kettinger et al., 2000). An intervention among drug-using adolescent mothers (Field et al., 1998) reduced depression and stress scores, which are some of the factors associated with poorer parenting attitudes (Kettinger et al., 2000). Thus, the intervention in this study may have provided enough support to the mothers to reduce the effects of other risk factors and to disrupt the association between ongoing drug use and low maternal responsiveness. However, more research is needed on the association between a home-based intervention and these other risk factors.
Although one component of the home-visiting protocol was to help the mothers use existing services (Aid to Families with Dependent Children, Medical Assistance, etc.), there were no significant group differences in use of services at 6 months. A high percentage of mothers in both groups reported using existing services, which may be the result of the hospital’s policy to register the mother for services before she left the hospital. Control group families were more likely to be involved with Child Protective Services than were intervention group families. However, some caution is warranted because the data were based on maternal report, and we could not access Child Protective Services records to verify who was still involved with the agency.
Finally, infant birth weight was a significant predictor of infant warmth and maternal responsiveness, which means that heavier infant birth weights were associated with higher infant warmth and maternal responsiveness scores. This finding is similar to other research which found that infant birth weight was a significant predictor of maternal behavior (Zahr, 1991) and infant behavior (Spiker et al., 1993) during mother–infant interaction. One possible explanation is that low infant birth weight has been associated with maternal stress (Robson, 1997) and depression (Gennaro, York, & Brooten, 1990; Singer et al., 1999), and both stress and depression are associated with poorer parenting among drug-using women (Kettinger et al., 2000). This finding raises concerns about the well-being of infants who are not healthy and who remain with their drug-using mothers.
The data presented here must be interpreted with caution. First, participants included only families in which the infant was discharged at birth into the mother’s care. Drug-exposed infants who are discharged into the care of mothers who continue to use drugs may be at greater risk than drug-exposed infants who are placed with another caregiver. Second, the mothers volunteered to participate in the study; therefore, this group may not be representative of all drug-using mothers but may be representative of those in studies. However, we found no differences between mothers who remained in the study and those who dropped out. Third, ongoing maternal drug use was based on self-report; thus, mothers may have underestimated their drug use. However, maternal report of ongoing drug use was high, with almost half admitting continued cocaine and/or heroin use. The mothers in this study may have felt more comfortable admitting ongoing drug use because of the continuity of the research team, because this investigation was conducted in the context of a special clinic for drug-using women, and because all participants were admitted drug users.
Another limitation is that maternal responsiveness and infant warmth were measured at one point in time, which may account for the lack of group differences. However, researchers (Black et al., 1996) found that among low-income urban African American families, behavior observed during mother–infant interaction was consistent with behavior measured by three other modalities (observations in the home, children’s performance on standardized developmental assessments, and maternal self-report on psychological variables). Finally, the analyses in this study were based on the intention to treat model. Although many mothers accepted the home visits, some mothers were noncompliant with the home visits. This variability in acceptance among drug-using mothers has been found before (Black et al., 1994). Future research needs to examine the differences between mothers who accept the intervention and those who do not.
Ongoing maternal drug use is a major concern. Almost half the mothers in this study continued to abuse cocaine and/or heroin and about two thirds used alcohol. Thus, they continued to live in a drug-using environment. Follow-up research on the impact of prenatal drug exposure has shown very few effects on children’s development when standardized tests are used (Azuma & Chasnoff, 1993; Hurt, Malmud, Betancourt, Braitman, et al., 1997; Hurt, Malmud, Betancourt, Brodsky, & Giannetta, 1997). However, some of these investigators have not considered ongoing maternal drug use or the parenting environment (relationship between mother and child). In one of the rare exceptions, researchers found that drug-exposed children living in homes with ongoing drug use had worse cognitive outcomes than drug-exposed children living in drug-free homes (Griffith et al., 1994). Thus, it is important that future investigators consider not only initial drug-using status but also the chronic remitting nature of drug use and design intervention programs that include drug treatment.
In summary, mothers in the control group who continued to use drugs were less responsive to their infants during mother–infant interaction at 6 months postpartum than were control mothers who stopped using drugs. The intervention broke that pattern. Mothers in the intervention group were equally responsive regardless of ongoing drug use. Thus, the intervention may have given the mothers specific skills to interact with their infants. More longitudinal research is needed to determine how to decrease maternal drug use and, given the chronic unremitting nature of drug use, how to develop interventions that promote responsive parenting and interrupt negative aspects of maternal drug use on child rearing.
Acknowledgments
This study was supported by Grant DA07432 from the National Institute on Drug Abuse.
Footnotes
Parts of this article were presented at the annual meetings of the Ambulatory Pediatric Association in New Orleans, LA, May 1998.
References
- Amaro H, Fried L, Cabral H, Zuckerman B. Violence during the pregnancy and substance use. American Journal of Public Health. 1990;80:575–579. doi: 10.2105/ajph.80.5.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azuma S, Chasnoff I. Outcome of children prenatally exposed to cocaine and other drugs: A path analysis of three-year data. Pediatrics. 1993;92:396–402. [PubMed] [Google Scholar]
- Black MM, Hutcheson J, Dubowitz H, Starr RH, Berenson-Howard J. The roots of competence: Mother–child interaction among low income, urban, African American families. Journal of Applied Developmental Psychology. 1996;17:367–391. [Google Scholar]
- Black MM, Nair P, Kight C, Wachtel R, Roby P, Schuler M. Parenting and early development among children of drug-abusing women: Effects of home intervention. Pediatrics. 1994;94:440–448. [PubMed] [Google Scholar]
- Black MM, Schuler M, Nair P. Prenatal drug exposure: Neurodevelopmental outcome and parenting environment. Journal of Pediatric Psychology. 1993;18:605–620. doi: 10.1093/jpepsy/18.5.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns K, Chethik L, Burns W, Clark R. The early relationship of drug abusing mothers and their infants: An assessment at eight to twelve months of age. Journal of Clinical Psychology. 1997;53:279–287. doi: 10.1002/(sici)1097-4679(199704)53:3<279::aid-jclp11>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Butz A, Lears MK, O’Neil S, Lukk P. Home intervention for in utero drug-exposed infants. Public Health Nursing. 1998;15:307–318. doi: 10.1111/j.1525-1446.1998.tb00355.x. [DOI] [PubMed] [Google Scholar]
- Callahan C, Grant T, Phipps P, Clark G, Novack A, Streissguth A, Raisys A. Measurement of gestational cocaine exposure: Sensitivity of infants’ hair, meconium, and urine. Journal of Pediatrics. 1992;120:763–768. doi: 10.1016/s0022-3476(05)80245-8. [DOI] [PubMed] [Google Scholar]
- Catalano R, Haggerty K, Gainey R, Hoppe M. Reducing parental risk factors for children’s substance misuse: Preliminary outcomes with opiate-addicted parents. Substance Use & Misuse. 1997;32:699–721. doi: 10.3109/10826089709039371. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1983. [Google Scholar]
- Cowan P, Cowan C. Schoolchildren and their families project: Description of child-style ratings. Berkeley: University of California, Department of Psychology; 1992. [Google Scholar]
- Field T, Scafidi F, Pickens J, Prodromidis M, Pelaez-Nogueras M, Torquati J, Wilcox H, Malphurs J, Schanberg S, Kuhn C. Polydrug-using adolescent mothers and their infants receiving early intervention. Adolescence. 1998;33:117–143. [PubMed] [Google Scholar]
- Gennaro S, York R, Brooten D. Anxiety and depression in mothers of low birthweight and very low birthweight infants: Birth through 5 months. Issues in Comprehensive Pediatric Nursing. 1990;13:97–109. doi: 10.3109/01460869009009029. [DOI] [PubMed] [Google Scholar]
- Graham K, Koren G, Klein J, Schneiderman J, Greenwald M. Determination of gestational cocaine exposure by hair analysis. Journal of the American Medical Association. 1989;262:3328–3330. [PubMed] [Google Scholar]
- Griffith D, Azuma S, Chasnoff I. Three-year outcome of children exposed prenatally to drugs. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:20–27. doi: 10.1097/00004583-199401000-00004. [DOI] [PubMed] [Google Scholar]
- Hardy J, Streett R. Family support and parenting education in the home: An effective extension of clinic-based preventive health care services for poor children. Journal of Pediatrics. 1989;115:927–931. doi: 10.1016/s0022-3476(89)80744-9. [DOI] [PubMed] [Google Scholar]
- Hawley T, Halle T, Drasin R, Thomas N. Children of addicted mothers: Effects of the ‘crack epidemic’ on the caregiving environment and the development of preschoolers. American Journal of Orthopsychiatry. 1995;65:364–379. doi: 10.1037/h0079693. [DOI] [PubMed] [Google Scholar]
- HELP at Home: Hawaii Early Learning Profile. Palo Alto, CA: Vort; 1991. [Google Scholar]
- Hofkosh D, Pringle J, Wald H, Switala J, Hinderliter S, Hamel S. Early interactions between drug-involved mothers and infants. Archives of Pediatrics & Adolescent Medicine. 1995;149:665–672. doi: 10.1001/archpedi.1995.02170190075014. [DOI] [PubMed] [Google Scholar]
- Hurt H, Malmud E, Betancourt L, Braitman L, Brodsky N, Giannetta J. Children with in utero cocaine exposure do not differ from control subjects on intelligence testing. Archives of Pediatrics and Adolescent Medicine. 1997;151:1237–1241. doi: 10.1001/archpedi.1997.02170490063011. [DOI] [PubMed] [Google Scholar]
- Hurt H, Malmud E, Betancourt L, Brodsky N, Giannetta J. A prospective evaluation of early language development in children with in utero cocaine exposure and in control subjects. Journal of Pediatrics. 1997;130:310–312. doi: 10.1016/s0022-3476(97)70361-5. [DOI] [PubMed] [Google Scholar]
- Hutcheson J, Black MM, Talley M, Dubowitz H, Berenson-Howard J, Starr R, Thompson B. Risk status and home intervention among children with failure-to-thrive: Follow-up at age 4. Journal of Pediatric Psychology. 1997;22:651–668. doi: 10.1093/jpepsy/22.5.651. [DOI] [PubMed] [Google Scholar]
- Infant Health and Development Program. Enhancing the outcomes of low-birth weight, premature infants. Journal of the American Medical Association. 1990;263:3035–3042. doi: 10.1001/jama.1990.03440220059030. [DOI] [PubMed] [Google Scholar]
- Kelley S. Parenting stress and child maltreatment in drug-exposed children. Child Abuse & Neglect. 1992;16:317–328. doi: 10.1016/0145-2134(92)90042-p. [DOI] [PubMed] [Google Scholar]
- Kettinger L, Nair P, Schuler M. Exposure to environmental risk factors and parenting attitudes among substance abusing women. American Journal of Drug and Alcohol Abuse. 2000;26:1–11. doi: 10.1081/ada-100100586. [DOI] [PubMed] [Google Scholar]
- Leventhal JM, Forsyth B, Qi K, Johnson L, Schroeder D, Votto N. Maltreatment of children born to women who used cocaine during pregnancy: A population-based study [43 paragraphs] Pediatrics. 1997 August;100(2):e7. doi: 10.1542/peds.100.2.e7. [On-line serial] Retrieved December 10, 1997 for the World Wide Web: http://www.pediatrics.org. [DOI] [PubMed]
- Meinert CL. Clinical trials: Design, conduct, and analysis. New York: Oxford University Press; 1986. [Google Scholar]
- Parker S, Greer S, Zuckerman B. Double jeopardy: The impact of poverty on early child development. Pediatric Clinics of North America. 1988;35:1227–1240. doi: 10.1016/s0031-3955(16)36580-4. [DOI] [PubMed] [Google Scholar]
- Robson A. Low birth weight and parenting stress during early childhood. Journal of Pediatric Psychology. 1997;22:297–311. doi: 10.1093/jpepsy/22.3.297. [DOI] [PubMed] [Google Scholar]
- Schuler ME, Black MM, Starr RH. Determinants of mother–infant interaction: Effects of prenatal drug exposure, social support, and infant temperament. Journal of Clinical Child Psychology. 1995;24:397–405. [Google Scholar]
- Singer L, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. Journal of the American Medical Association. 1999;281:799–805. doi: 10.1001/jama.281.9.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiker D, Ferguson J, Brooks-Gunn J. Enhancing maternal interaction behavior and child social competence in low birth weight, premature infants. Child Development. 1993;64:754–768. doi: 10.1111/j.1467-8624.1993.tb02941.x. [DOI] [PubMed] [Google Scholar]
- Zahr L. Correlates of mother–infant interaction in premature infant from low socioeconomic backgrounds. Pediatric Nursing. 1991;17:259–264. [PubMed] [Google Scholar]
- Zuckerman B. Developmental considerations for drug- and AIDS-affected infants. In: Barth R, Pietrzak J, Ramler M, editors. Families living with drugs and HIV: Intervention and treatment strategies. New York: Guilford; 1993. pp. 37–58. [Google Scholar]
- Zuckerman B. Effects of parents and children. In: Besharov D, editor. When drug addicts have children. Washington, DC: Child Welfare League of America; 1994. pp. 49–63. [Google Scholar]
- Zuckerman B, Frank D, Hingson R, Amaro H, Levenson S, Kayne H, Parker S, Vinci R, Aboagye K, Fried L, Cabral H, Timperi R, Bauchner H. Effects of maternal marijuana and cocaine use on fetal growth. New England Journal of Medicine. 1989;320:762–768. doi: 10.1056/NEJM198903233201203. [DOI] [PubMed] [Google Scholar]