Abstract
Background:
Construction sector is a booming industry and involves many hazardous activities. Migrant labor in the industry is susceptible to various health and occupational hazards. In a unique public–private partnership project, a medical team from a public sector teaching hospital in Mumbai provided comprehensive on-site health care services to the construction workers of a private construction company.
Objective:
To study socio-demographic profile and morbidity pattern of construction workers.
Setting and Design:
A cross-sectional study at construction site Vidyavihar (West), Mumbai, was carried out over the period of May to November 2010.
Materials and Methods:
A medical team provided comprehensive on-site health care services, and a Health Card was devised to maintain the record of socio-demographic, occupational details, and complete physical examination findings of the workers who participated in the study.
Statistical Analysis Used:
Statistical analysis was done using SPSS 15.0.
Results:
Of the 1337 workers (all males) examined, 1289 (96.4%) belonged to 15–45 years age group. The mean age of the workers was 26.25 ± 8.49 years. A third of the migrants belonged to West Bengal. The average number of health problems in the workers was 1.41. Regular consumers of tobacco and alcohol were 50.48 and 14.65%, respectively. Nearly one-fifth of the workers had febrile illness, of which 20.71% had suspected malaria; 12.6% had respiratory infections, while 3.4% were found to have hypertension. There was a statistically significant association (P < 0.05) between type of occupation and morbidity status.
Keywords: Construction sector, health profile, migrant laborers
INTRODUCTION
Workers represent half the world's population and are major contributors to economic and social development.[1] In India, nearly two-thirds of the contribution to the net domestic product is by the unorganized sector.[2] According to the National Sample Survey Organization (NSSO, 1999–2000), 370 million workers constituted 92% of the total unorganized workforce in the country.[3] There are about 37 million unorganized laborers in Maharashtra.[4] As per census 2001, 29.90 million workers migrated for reasons of employment.[5] Employment-driven migration is mainly from the “relatively less developed” states to large metropolises and other large cities, wherein the migrants get absorbed in low-paid jobs in the unorganized sectors.[6] The workers’ living conditions are poor with denial of basic amenities to maintain the standard of living, making them prone to health problems.
The construction sites create breeding grounds for various vectors and unprotected laborers act as potential baits. In addition, immigrants from disease-endemic areas settle in urban slums with highly vector-receptive and unprotected housing, introducing new and drug-resistant strains. As a consequence of the focus on development of infrastructure in urban areas and urban renewal scheme, the unorganized sector in India will continue to expand in future, making it necessary to have strengthened and activated system so as to enable the workers to live in a healthy socio-economically productive life. In the same quest, a cross-sectional study was planned in one of the construction sites in the city of Mumbai to study the baseline socio-demographic profile and morbidity pattern of construction workers, to enable determination of appropriate interventions for the problems identified.
MATERIALS AND METHODS
Setting a unique example of Public Private Partnership, the Department of Community Medicine collaborated with a construction company in Vidyavihar (West), Mumbai, employing a large number of migrant workers, to provide comprehensive health services during the working hours of the hospital. A health team comprising resident medical officer, interns, and medical social workers was posted onsite. The referrals, if any, were made to the nearest municipal hospitals. Due to constraints of the construction company and the nature of the work, all the workers were males, staying on the site. Logistic and drug support was provided by the construction company and make-shift out patient department was provided. Besides providing the curative services for the ailments, first-aid services, health education, training of supervisors in handling the medical emergencies, and collaboration with the Public Health Department for Malaria Control was carried out. A cross-sectional study design was chosen and sample size was calculated using the formula for estimating a population proportion with specified absolute precision.[7]
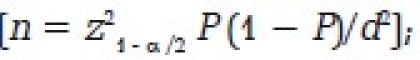
where α = 0.05, P = 0.50, and d = 3%.
The minimum sample size was calculated to be 1067; however, the number of workers studied was 1337. The study was started after taking necessary permissions from the authorities and the Institutional Ethics Committee. It was conducted over the period of May to November 2010.
A Health Card was designed by the Community Medicine department to record the medical history (later adopted by the public health department in a summarized format) consisting of standard questions related to socio-demographics, including occupational history, addictions, medical history, and record of complete medical examination. The malaria investigator of the Malaria Surveillance unit of public health department was assigned for taking peripheral blood smear for malaria parasite. The participant staying in the study area for 5 years or less was considered to be a “migrant.” A person using any tobacco product on daily basis for more than 1 year was labeled as “tobacco user.” A “skilled worker” is one who is capable of working independently and efficiently and capable of reading and working on simple drawing circuits and process, if necessary. An “unskilled worker” is one who possesses no special training and whose work involves the performance of the simple duties that require the exercise of little or no independent judgment or previous experience, although a familiarity with the occupational environment is necessary.[8] Alcohol users were considered as those who had consumed alcohol at least once per month. Modified BG Prasad classification was used for economic classification.[9] As a routine, the induction training for the construction workers was conducted by the safety department. The workers were diverted for the health check-up (detailed history taking and medical examination). Illnesses, if any, were treated symptomatically. The blood pressure was recorded using a mercury sphygmomanometer. The Joint Nation Committee VII criteria[10] were used to diagnose hypertension.
Investigations such as Peripheral Smear for Malaria Parasite were carried out onsite. Information, Education, and Communication material on topics such as monsoon-related illness, HIV/AIDS, and addictions in the form of flip charts were used. Data were analyzed using SPSS 15 version. Chi-square test was performed to detect the statistical significance between socio-demographic determinants and morbidity.
RESULTS AND DISCUSSION
Socio-demographics
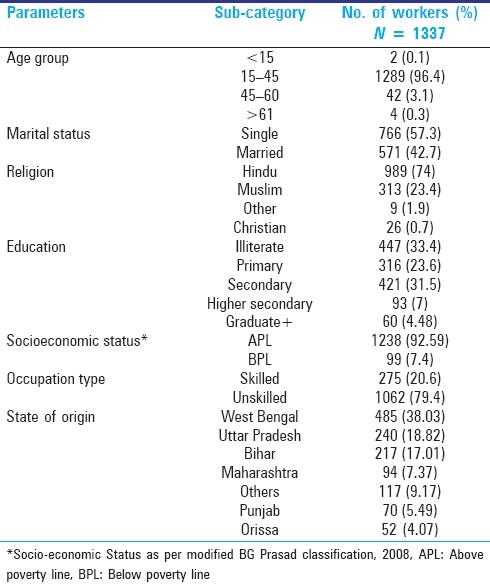
Out of 1337 workers (all males), 1289 (96.4%) belonged to 15–45 years age group [Table 1]. The mean age of workers was 26.25 ± 8.49 years. A total of 766 (57.3%) workers were unmarried, 989 (74%) were Hindu followed by 313 (23.4%) Muslims. In all, 447 (33.4%) were illiterate, while those with primary and secondary/higher education were 316 (23.6%) and 574 (43%), respectively. A total of 99 (7.4%) belonged to below poverty line. Majority of workers were unskilled laborers (1062, 79.4%). Out of 1275 migrants, 485 (38.03%) workers had migrated from West Bengal, followed by Uttar Pradesh (240, 18.82%), and 94 (7.37%) were from other parts of Maharashtra.
Table 1.
Socio-demographic profile
Health problems
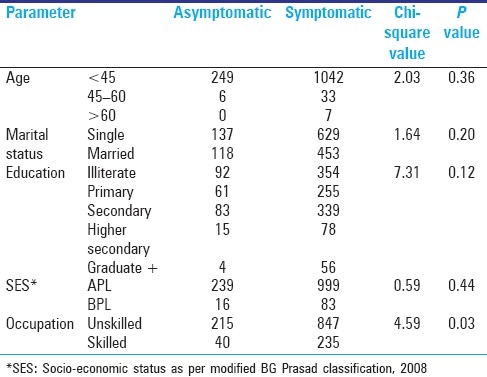
The morbidity profile revealed that the average number of health problems in the workers was 1.41. Workers suffering with any kind of fever were 309 (23.11%) followed by respiratory infections present in 168 (12.6%). Of the 309 cases of fever, 277 (20.71%) were suspected of malaria. The slide positivity rate for the malaria was 8.11%. In all, 45 (3.4%) had hypertension; 675 (50.48%) of the workers consumed tobacco and 196 (14.65%) consumed alcohol [Table 2]. There was a significant association between type of occupation and morbidity status (P < 0.05). The association between socio-economic and demographic variables and health status is depicted in Table 3.
Table 2.
Morbidity profile
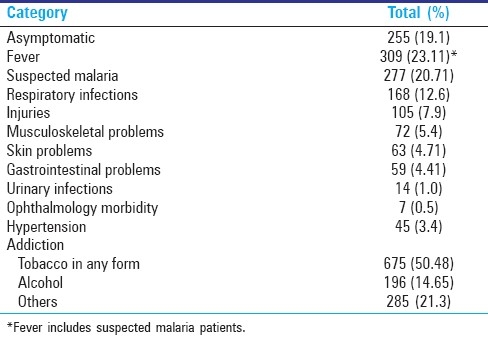
Table 3.
Association between variables and health status
DISCUSSION
The highest morbidity (23.11%) at the construction site was due to acute febrile illness. Out of these, 20.71% workers had suspected malaria. In a cross-sectional study by Venugopalan et al.,[11] slide positivity rate of 6.28% was found among migrant construction workers in Mangalore, South India. In our site the slide positivity rate was 8.11%, and the reason for such a high prevalence of malaria at this construction site may be due to favorable conditions for mosquito breeding sites offered by construction site environment and the unprotected workers acting as baits. The workers and their supervisors ought to be informed about the biological hazard such as mosquito breeding sites and use of personal protection measures with the help of repetitive Information, Education, and Communication activities.
In this study, 12.6% of workers had various respiratory infections. Gurav et al.[12] have reported respiratory problems in 4.86% of workers. The higher prevalence in this study may be due to higher exposure to dust during the working hours and post-working hours as the accommodation is situated within the campus.
In this construction site, 5.4% workers had musculoskeletal problems. Mohopatra[13] has reported that 40% of workers suffer from musculoskeletal disorders affecting various joints and muscles ranging from neck to foot. In this study, the prevalence of musculoskeletal disorder is less probably due to less manual activity, as the work is mostly mechanized.
This study reports 7.9% workers having some form of injury while working at the construction site. Construction industry is known for high incidence of accidents. More than 90% of accidents are preventable.[14] According to Ramsay,[15] the risk of accidents increases with extremes of temperature. Age, sex, personal habits (such as working under the influence of alcohol), personality traits (risk-taking behavior), and physical and mental state of the worker play an important role in the occurrence of accidents.[14] In a study by Shah and Mehta,[16] the prevalence of injuries was 25.42%, and the reason for the low prevalence in this study can be attributed to more of mechanized work and on-site periodic safety induction training given by the engineering company.
Skin problems such as fungal infection, contact dermatitis, and eczematous rash were found in 4.71% of the workers. Contact with cement and lime may lead to irritant dermatitis. The presence of chromate and cobalt in cement is known to cause allergic contact dermatitis.[17]
Some workers (4.41%) in this study had gastrointestinal problems such as loose motions, abdominal pain, constipation, and loss of appetite, as workers are exposed to chemical agents, parasitic agents, or infective agents at the work and residential place.
Hypertension was found in 3.4% of the workers. It is nearly same as the national prevalence of hypertension (3.55–5.99%) reported by Gupta et al.,[18,19] but more than the study conducted by Gurav et al.[9] However, there is a need to study the modifiable risk factors for hypertension in detail.
Tobacco consumption was present in 50.48% of the workers, which is nearly equal to the national prevalence (57%) as per the National Family Health Survey 2005–2006.[20]
Consumption of alcohol was reported by 14.65% of the workers and is less than the national estimate of 21% as per the National Household Survey on drug abuse.[21]
This study has shown the pattern of health problems among construction workers which will contribute to further development of health promotion strategies for construction workers.
This study had limitation, as it was not possible to conduct HIV testing of the construction workers. In addition, it was not possible to study the usage of personal protective gears and its impact in preventing injury at work.
The need of the hour is to have behavior change communication to target the vector-borne diseases and lifestyle diseases such as hypertension, addiction, and use of personal protective equipments to prevent the injuries. Active surveillance of fever cases should be given priority so that the infected patients are diagnosed early and receive radical treatment under supervision at the construction site, thereby decreasing the incidence of man-made malaria.
This is the first step toward having a healthy construction site and a healthy workforce, undertaken through a unique project of Public Private Partnership by the Department of Community Medicine.
CONCLUSION
The results of this study can be extrapolated to other construction sites employing the migrant workers. Benefits of the public–private partnership to the medical college will be in the form of research-oriented training for the postgraduate students in community medicine. The benefits to the construction company are to have a healthy workforce to achieve its targets and goals of the project as well as opting for the Occupational Health and Safety Assessment Series certification. The public–private partnership will act as a model to decrease morbidity and mortality created at construction site.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.World Health Organization [Internet]. Workers’ health: Global plan of action. [last accessed on 2010 May 15]. Available from: http://apps.who.int/gb/ebwha/pdf_fi les/WHA60/A60_R26-en.pdf .
- 2.Labour.nic.in [Internet]. Informal sector in India: Approaches for social security. [last accessed on 2010 May 15]. Available from: http://labour.nic.in/ss/INFORMALSECTORININDIA-ApproachesforSocialSecurity.pdf .
- 3.Labour.nic.in [Internet]. Building and Other Construction Workers (Regulation of Employment and working Conditions) Act. 1996. [last accessed on 2010 Jun 30]. Available from: http://labour.nic.in/dglw/building_works.html .
- 4.Chatterjee P. Indianexpress.com [Internet]. Social security for unorganized sector remains on paper. [last accessed on 2010 Jul 20]. Available from: http://www.indianexpress.com/news/social-security-for-unorganised-sectorremai/647219 .
- 5.Pib.nic.in [Internet]. Ministry of Labour and Employment, Inter-state Migrant Workmen (regulation of employment and conditions of service) Act; 1979 [PIB (Press Information Bureau) Press Release] [last accessed on 2010 Jun 30]. Available from: http://www.pib.nic.in/release/rel_print_page1.asp?relid=23797 .
- 6.Mukherji S. Low quality migration in India: The phenomena of distressed migration and acute urban decay working for unorganised labour - The case of Mumbai. [last accessed on 2010 Jun 01]. Available from: http://www. Iariw.org/papers/2009.pdf .
- 7.Lwanga SK. Geneva: World Health Organization; 1991. Sample size determination in health studies’ a practical manual; pp. 25–6. [Google Scholar]
- 8.Government of Tamilnadu [Internet] [ast accessed on 2010 Jun 30]. Available from: http://www.tn.gov.in/gorders/labour/labemp-e-48-2D-2004.htm .
- 9.Government of India [Internet]. Office of the Economic adviser to the Government of India, Ministry of Commerce and industry. [last accessed on 2010 Jun 15]. Available from: http://www.eaindustry.nic.in .
- 10.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 11.Venugopalan PP, Shenoy DU, Kamath A, Rajeev A. Distribution of malarial parasites: Effect of gender of construction workers. Indian J Med Sci. 1997;51:89–92. [PubMed] [Google Scholar]
- 12.Gurav RB, Kartikeyan S, Wayal R, Joshi SD. Assessment of health profile of daily wage labourers. Indian J Occup Environ Med. 2005;9:115–7. [Google Scholar]
- 13.Mohopatra R, editor. Occupational Health Hazards and Remedies. 1st ed. New Delhi: Jaypee Brothers Medical Publishers Pvt Ltd; 2002. Occupational Health Hazards in Small Scale and Other Industries; pp. 54–5. (203-4). [Google Scholar]
- 14.Gupta MC, Mahajan BK, editors. Textbook of Preventive and Social Medicine. 3rd ed. New Delhi: Jaypee Brothers Medical Publishers Pvt. Ltd; 2003. Physical Environment: Place of Work or Occupation (Occupational Health) pp. 66–80. [Google Scholar]
- 15.Ramsay JD. Effect of workplace thermal conditions on safe work behaviour. J Safety Res. 1983;14:105–14. [Google Scholar]
- 16.Shah CK, Mehta H. Study of injuries among construction workers in Ahmadabad city, Gujarat. Indian J Practising Doctor. 2009;5:4–8. [Google Scholar]
- 17.Stevenson CJ. Occupational Diseases of Skin. In: Raffle PA, Adams PH, Baxter PJ, Lee WR, editors. Hunter's Disease of Occupations. 8th ed. London: Edward Arnold; 1994. pp. 691–719. [Google Scholar]
- 18.Gupta SP, Siwach SB, Moda VK. Epidemiology of hypertension based on total community survey in the urban population of Haryana. Indian Heart J. 1978;30:315–22. [PubMed] [Google Scholar]
- 19.Gupta SP, Siwach SB, Moda VK. Epidemiology of hypertension based on total community survey in the rural population of Haryana. Indian Heart J. 1977;29:53–62. [PubMed] [Google Scholar]
- 20.National Family Health Survey (NFHS-3) 2005-06. Vol. 1. Mumbai: IIPS; 2007. International Institute for Population Sciences (IIPS) and Macro International. [Google Scholar]
- 21.Srivastava A, Pal H, Dwivedi SN, Pandey A National Household Survey of Drug Abuse in India. Report submitted to Ministry of Social Justice and Empowerment, Government of India and United Nations Office on Drugs and Crime, Regional Office for South Asia. 2002 [Google Scholar]


