Abstract
Objectives
Laboratory technicians, students, and instructors are at high risk, because they deal with chemicals including formaldehyde. Thus, this preliminary study was conducted to measure the concentration of formaldehyde in the laboratories of the University of Sharjah in UAE.
Materials and Methods:
Thirty-two air samples were collected and analyzed for formaldehyde using National Institute for Occupational Safety and Health (NIOSH) method 3500. In this method, formaldehyde reacts with chromotropic acid in the presence of sulfuric acid to form a colored solution. The absorbance of the colored solution is read in spectrophotometer at wavelength 580 nm and is proportional to the quantity of the formaldehyde in the solution.
Results:
For the anatomy laboratory and in the presence of the covered cadaver, the mean concentration of formaldehyde was found to be 0.100 ppm with a range of 0.095–0.105 ppm. Whereas for the other laboratories, the highest mean concentration of formaldehyde was 0.024 ppm in the general microbiology laboratory and the lowest mean concentration of formaldehyde was 0.001 ppm in the environmental health laboratory. The 8-hour (time-weighted average) concentration of formaldehyde was found to be ranging between 0.0003 ppm in environmental health laboratory and 0.026 ppm in the anatomy laboratory.
Conclusions:
The highest level of concentration of formaldehyde in the presence of the covered cadaver in anatomy laboratory exceeded the recommended ceiling standard established by USA-NIOSH which is 0.1 ppm, but below the ceiling standard established by American Conference of Governmental Industrial Hygienists which is 0.3 ppm. Thus, it is recommended that formaldehyde levels should be measured periodically specially during the dissection in the anatomy laboratory, and local exhaust ventilation system should be installed and personal protective equipment such as safety glass and gloves should be available and be used to prevent direct skin or eye contact.
Keywords: Anatomy, cadaver, concentration, formaldehyde, Sharjah University, UAE
INTRODUCTION
Formaldehyde is a colorless, strong-smelling gas. Commonly known as preservative in medical laboratories and mortuaries, formaldehyde is also found in other products such as chemicals, particle board, household products, glues, permanent press fabrics, paper product coatings, fiberboard, and plywood. It is also widely used as an industrial fungicide, germicide, and disinfectant.[1]
Acute and chronic exposure to formaldehyde by inhalation in humans has been associated with respiratory symptoms and eye, nose, and throat. Contact with formalin causes white discoloration, smarting, drying, cracking, and scaling. Formaldehyde solutions splashed in the eye can cause injuries ranging from transient discomfort to severe, permanent corneal clouding and loss of vision.[2,3]
The perception of formaldehyde by odor and eye irritation becomes less sensitive with time as one adapts to formaldehyde. This can lead to overexposure if a worker is relying on formaldehyde's warning properties to alert him or her to the potential for exposure.[4]
Occupational studies have noted statistically significant associations between exposure to formaldehyde and increased incidence of lung and nasopharyngeal cancer. This evidence is considered to be ‘limited’, rather than 'sufficient’, due to possible exposure to other agents that may have contributed to the excess cancers. Animal studies have reported an increased incidence of nasal squamous cell carcinomas by inhalation exposure. Environmental Protection Agency (USA) considers formaldehyde to be a probable human carcinogen and has ranked it in Environmental Protection Agency's Group B1.[5]
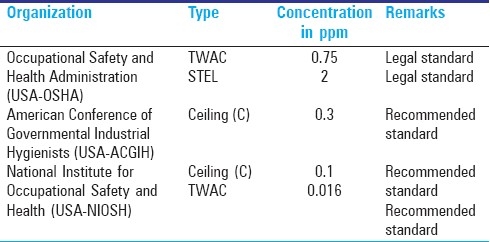
Standards referred to as legal standards or as recommendation standards are established by several organizations in the world. These standards include ‘Ceiling Limit’, a limit that should not be exceeded even instantaneously at any time during the work day; short-term exposure level (STEL) refers to the concentration to which employees can be continuously exposed for 15 min without any adverse health effects; and time-weighted average (TWA) concentration which is an 8-h (working-day or 40 h work-week) average concentration under which it is believed that nearly all the employees may be repeatedly exposed to throughout their lifework without any adverse health effects; these legal and recommended standards are established to protect subjects from acute and chronic health effects of the substances. Legal and recommended standards suggested by international organization for formaldehyde are shown in Table 1.[6–8]
Table 1.
Threshold limit values for formaldehyde
Objectives
Laboratory technicians are at high risk, because they deal on a daily bases with chemicals including formaldehyde. In addition, students and instructors are also exposed to formaldehyde during their work in the laboratories. Thus, the objectives of the preliminary study were to measure the concentration of formaldehyde in the laboratories of the University of Sharjah and to compare the findings with the standards.
MATERIALS AND METHODS
Fifteen laboratories at the University of Sharjah were selected for this study, and two area air samples were collected from each laboratory. For the anatomy laboratory, samples were collected in the presence and absence of the cadaver. The sampling time ranged between 2 and 3 h and covered the laboratory session.
The air samples were collected and analyzed for formaldehyde using National Institute for Occupational Safety and Health (NIOSH) method 3500.[9]
Collection and analysis of the samples
Samples were collected with a constant flow pump and a midget impinger containing 20 mL of 1% sodium bisulphite solution. Samples were then analyzed in the same day. The flow rate of the pump was measured before and after each sampling by a pre-calibrated flow meter.
Each sample was analyzed by adding 0.1 mL of 1% chromotropic acid and 6 mL of concentrated H2SO4 to 4 mL of the sample solution. The solution was gently swirled to mix and left for 2–3 hours to cool down and to form a colored solution.
A 1-cm cuvette was filled with the colored solution and placed in the spectrophotometer (Model 20 Genesys - Spectronic Unicam- U.K), and the absorbance was read at 580 nm, against a blank solution (a solution containing 4-mL deionized water and treated as a sample). Finally, the formaldehyde content of the sample was determined using curve estimation regression model.
Standards and curve estimation regression model
Formaldehyde Standard Solution (A) (0.95 mg/mL) was prepared by weighing 2.2352 g of sodium formaldehyde bisulfite (95% purity) and dissolved in 500 mL of deionized water and prepared weekly.
Formaldehyde Standard Solution (B) 9.5 μ/mL was prepared by diluting 1 mL of the Formaldehyde Standard Solution (A) to 100 mL and prepared daily.
Four formaldehyde standard solutions containing 0.475, 0.7125, 0.950, and 1.425 μg were prepared from the Formaldehyde Standard Solution (B) and analyzed in the same way and on the same day the samples analyzed. Finally, the absorbance of standard solutions and the weight of the formaldehyde were entered into SPSS as independent and dependent variable, respectively, for curve estimation regression model. The relationship between the formaldehyde and the absorbance was found to be linear or quadratic.
The 8-hour TWA concentration was calculated with the assumption that unsampled time was zero exposure because students and staff were exposed only during the laboratory sessions using the following formula:
C1T1 /8 h
Where C1 is the concentration of formaldehyde during the sampling time T1 , and T1 is the time of sampling in hours.
RESULTS
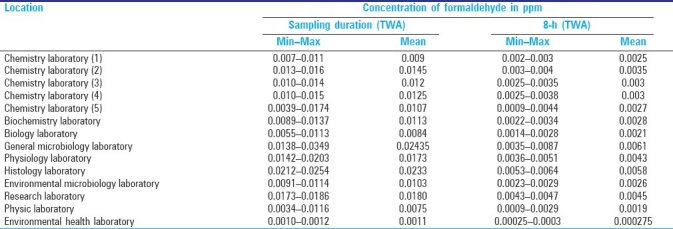
Tables 2 and 3 show the airborne concentration of formaldehyde in the anatomy laboratory and the other laboratories, respectively. The results are presented for the duration of time during which the samples were collected and as 8-h TWA.
Table 2.
Results of the analysis of the samples for formaldehyde in dissection anatomy laboratory
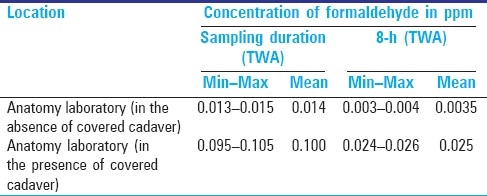
Table 3.
Results of the analysis of the samples for formaldehyde in other laboratories
For the anatomy laboratory [Table 2], the concentration of formaldehyde for the sampling duration ranged between 0.013 and 0.015 ppm with a mean of 0.014 ppm in the absence of cadaver. However, in the presence of the cadaver, the mean concentration of formaldehyde increased to 0.100 ppm with a range of 0.095–0.105 ppm.
For the other laboratories and for the duration of sampling [Table 3], the highest concentrations of formaldehyde were found to be 0.024 and 0.023 ppm in the general microbiology and histology laboratory, respectively. Whereas the lowest mean concentration of formaldehyde was found to be 0.001 ppm in the environmental health laboratory (dry laboratory).
The mean concentration of formaldehyde was found to be ranging between 0.008 and 0.014 ppm for the physic, biology, biochemistry, environmental microbiology, and the five chemistry laboratories. For the research and physiology laboratory, the mean concentration was found to be 0.018 and 0.017 ppm, respectively.
The 8-h (TWA) concentration of formaldehyde was found to be ranging between 0.0003 ppm in the environmental health laboratory and 0.026 ppm in the anatomy laboratory in the presence of cadaver.
DISCUSSION
The use of formaldehyde in the preservation of animals and human specimens has been a common practice for centuries. In medical colleges, cadavers for gross anatomy laboratories are usually prepared by using formaldehyde as embalming fluid. In the presence of cadavers and during the process of dissection, formaldehyde vapors are emitted from the cadavers, resulting in the exposure of medical students and their instructors to elevated levels of formaldehyde in the laboratory.
In this study, the concentration of formaldehyde in anatomy laboratory in the presence of covered cadaver was found to be higher than that reported in other laboratories due to the emission of formaldehyde from the embalmed cadaver. In addition, in other laboratories formaldehyde was not used during the measurement.
Thus, the levels of formaldehyde reported in this study in anatomy laboratory in the presence of covered cadaver were compared with levels reported by other researchers in anatomy laboratories.
The results of this study showed that for the short duration of sampling, the highest level of concentration of formaldehyde (0.105 ppm) in the presence of covered cadaver in anatomy laboratory exceeded the recommended ceiling standard established by USA-NIOSH which is 0.1 ppm, but below the recommended ceiling standard established by American Conference of Governmental Industrial Hygienists (USA-ACGIH) which is 0.3 ppm and below the legal STEL established by Occupational Safety and Health Administration (USA-OSHA) which is 2 ppm. Higher levels were reported by other researchers. Akbar-Khanzadah et al.[10] evaluated formaldehyde exposure in a group of 34 subjects in a gross anatomy laboratory and reported that TWA concentration of formaldehyde ranged from 0.07 to 2.94 ppm during dissecting operations. The authors reported that more than 94% of the subjects were exposed to formaldehyde in excess of the ceiling value of 0.3 ppm recommended by the ACGIH and 31.7% of the subjects exceeded the 8-h TWA action level of 0.5 ppm set by the OSHA. In addition, the authors reported irritation of eye, nose, throat, airways, and a change of forced vital capacity and forced expiratory volume in 3 s among the subjects.[10]
In other study, Akbar-Khanzadah and Mlynek[11] studied the changes in respiratory function of 50 non-smoking medical students exposed to formaldehyde in a gross anatomy laboratory. The authors reported that airborne concentrations of formaldehyde in the gross anatomy varying between 0.59 and 1.72 ppm with a mean of 0.97 is similar to the mean concentration of formaldehyde reported by this study in the anatomy laboratory which was 0.100. Akbar-Khanzadah et al.[11] reported that all medical students were exposed to levels of formaldehyde greater than 0.3 ppm threshold limit value ceiling recommended by ACGIH, and the exposure of 29.5 of the medical students exceeded the permissible level set by OSHA which was 0.75 ppm. In addition, medical students reported symptoms of irritation of nose, eyes, and throats, but the researchers did not find any association between acute respiratory changes and exposure to formaldehyde.
Tanaka et al.[12] conducted a research over a period of 3 months during the anatomy dissection sessions to measure the gaseous formaldehyde concentrations in the anatomy dissection room. They found that immediately after removing the cadavers’ plastic covering, formaldehyde concentrations in the dissection room increased sharply and reached a peak point of 0.62 ppm after 10 min of starting of the class. This level was above the recommended level of 0.5 ppm set by Japan Society for Occupational Health. After 30 min of achieving the peak, the formaldehyde level started decreasing gradually to a level of 0.11 ppm and this level is comparable to the level of 0.105 ppm reported in this study in the anatomy laboratory in the presence of covered cadaver. The authors[12] reported that 59% of students experienced formaldehyde-related symptoms such as irritation of eyes, nose, throat, airways, skin, and headache.
Burroughs et al.,[13] assessed exposure of museum staff to formaldehyde during some wet specimen activities; the authors reported level of formaldehyde of 0.140 ppm for area samples collected for short time in collection management center and this level was comparable to that reported in this study which was 0.105 ppm in the anatomy laboratory in the presence of cadaver. However, the authors reported higher levels of formaldehyde (0.38 ppm) in comparative anatomy laboratory.
Ghasemkhani et al.[14] in their research to determine formaldehyde exposure level of staff in pathology laboratories, surgery rooms, and endoscopy wards of eight hospitals of Tehran University of Medical Sciences collected and analyzed 141 samples. The researches[14] reported mean levels of formaldehyde ranging between 0.13 ppm in endoscopy wards and 0.96 ppm in pathology laboratories. The authors concluded that the levels of formaldehyde at pathology laboratories exceeded the recommended ceiling standard established by USA-ACGIH which is 0.3 ppm.
Ohmichi et al.[15] evaluated formaldehyde levels in gross anatomy laboratory in three sessions of 20 laboratory sessions. The authors found that the room averages of formaldehyde concentrations were 0.45, 0.38, and 0.68 ppm, while the average personal exposure levels were 0.80, 0.45, and 0.51 ppm for instructors and 1.02, 1.08, and 0.89 ppm for students for the three sessions, respectively. The authors concluded that these levels were higher than the two limit values set in Japan for environmental exposure to formaldehyde as an average for general workplaces 0.08 and 0.25 ppm for specific workplaces and higher than the ACGIH ceiling limit (0.3 ppm).
In this study, the concentration of formaldehyde averaged over an 8-h work day (TWA) was found to be ranging from 0.024 to 0.026 at the anatomy laboratory exceeded the most stringent standard (8-h TWA exposure) recommended by USA-NIOSH which is 0.016 ppm; this result is consistent with the findings of Burroughs et al.[13]
The low levels of formaldehyde reported in this study in anatomy laboratory compared with other studies can be explained by the fact that measurements in this study were carried out in the presence of covered cadaver but no dissection or any operations taking place, while in the other studies measurement were conducted in anatomy laboratories during some wet specimen activities such as dissection.
CONCLUSIONS
Airborne concentrations of formaldehyde in the anatomy laboratory in the presence of covered cavader are higher than that in other laboratories. These concentrations were comparable to or lower than the levels documented in the literature for anatomy laboratories, but exceeded the recommended ceiling standard established by USA-NIOSH.
Based on the findings of this preliminary study, the following are recommended:
Formaldehyde levels should be measured periodically specially during the dissection in the anatomy laboratory and during the use of formaldehyde in other laboratories.
Local exhaust ventilation system should be used in the anatomy laboratory and in other laboratories where formaldehyde must be used.
Personal protective equipment such as safety glass or goggles, gloves, and apron should be available and be used to prevent direct skin or eye contact.
Acknowledgments
The author wish to thank Ms. Badria Ahmed and Ms. Hind ALHuwaidi for their help in collection and analysis of the samples.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.U. S. Environmental Protection Agency. Health and Environmental Effects Profile for Formaldehyde. EPA/600/x-85/362. Environmental Criteria and Assessment Office, Office of Health and Environmental Assessment, Office of Research and Development, Cincinnati, OH. 1988 [Google Scholar]
- 2.Vol. 89. Geneva, Switzerland: World Health Organization; 1989. World Health Organization. Environmental Health Criteria for Formaldehyde. [Google Scholar]
- 3.Toxicological Profile for Formaldehyde (Draft) Atlanta, GA: Public Health Service, U.S. Department of Health and Human Services; 1997. Agency for Toxic Substances and Disease Registry (ATSDR) [Google Scholar]
- 4.Amoore JE, Hautala E. Odor as an aid to chemical safety: Odor thresholds compared with threshold limit values and volatilities for 214 industrial chemicals in air and water dilution. J Appl Toxicol. 1983;3:272–90. doi: 10.1002/jat.2550030603. [DOI] [PubMed] [Google Scholar]
- 5.Washington, DC: National Center for Environmental Assessment, Office of Research and Development; 1999. U. S. Environmental Protection Agency. Integrated Risk Information System (IRIS) on Formaldehyde. [Google Scholar]
- 6.TLVs and BEIs. Threshold Limit Values for Chemical Substances and Physical Agents, Biological Exposure Indices. Cincinnati, OH: 2002. American Conference of Governmental Industrial Hygienists (ACGIH) [Google Scholar]
- 7.Pocket Guide to Chemical Hazards. U. S. Department of Health and Human Services; 2004. National Institute for Occupational Safety and Health (NIOSH) p. 103. [Google Scholar]
- 8.Code of Federal Regulations. Code of Federal Regulations; 2005. Occupational Safety and Health Administration (OSHA) [Google Scholar]
- 9.NIOSH Manual of Analytical Methods (NMAM) Formaldehyde by VIS 3500. 4th ed. Cincinnati, OH: NIOSH; 1994. National Institute for Occupational Safety and Health . [Google Scholar]
- 10.Akbar-Khanzadah F, Vaquerano MU, Akbar-Khanzadah M, Bisesi MS. Formaldehyde exposure, acute pulmonary response, and exposure control options in a gross anatomy laboratory. Am J Ind Med. 1994;26:61–75. doi: 10.1002/ajim.4700260106. [DOI] [PubMed] [Google Scholar]
- 11.Akbar-Khanzadah F, Mlynek JS. Changes in respiratory function after one and three hours of exposure to formaldehyde in non-smoking subjects. Occup Environ Med. 1997;54:296–300. doi: 10.1136/oem.54.5.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tanaka K, Nishiyama K, Yaginuma H, Sasaki A, Maeda T, Kaneko SY, et al. Formaldehyde exposure levels and exposure control measures during an anatomy dissecting course. Kaibogaku Zasshi. 2003;78:43–51. [PubMed] [Google Scholar]
- 13.Burroughs GE, Makos K, Hawks C, Ryan T. Exposure of museum staff to formaldehyde during some wet specimen activities. Collect Forum. 2006;20:49–54. [Google Scholar]
- 14.Ghasemkhani M, Jahanpeyma F, Azam K. Formaldehyde exposure in some educational hospitals of Tehran. Ind Health. 2005;43:703–7. doi: 10.2486/indhealth.43.703. [DOI] [PubMed] [Google Scholar]
- 15.Ohmichi K, Komiyama M, Matsuno Y, Takanashi Y, Miyamoto H, Kadota T, et al. Formaldehyde exposure in a gross anatomy laboratory--Personal exposure level is higher than indoor concentration. Environ Sci Pollut Res Int. 2006;13:120–4. doi: 10.1065/espr2005.06.265. [DOI] [PubMed] [Google Scholar]


