Abstract
Bipolar disorder is frequently encountered in primary care settings, often in the form of poor response to treatment for depression. Although lifetime prevalence of bipolar I disorder is 1%, the prevalence of bipolar spectrum disorders (e.g., bipolar I, bipolar II, and cyclothymia) is much higher, especially among patients with depression. The consequences of misdiagnosis can be devastating. One way to improve recognition of bipolar spectrum disorders is to screen for them. The Mood Disorder Questionnaire is a brief, self-report screening instrument that can be used to identify patients most likely to have bipolar disorder. Once identified, and subsequently appropriately diagnosed, the lives of those with bipolar disorder may be considerably improved.
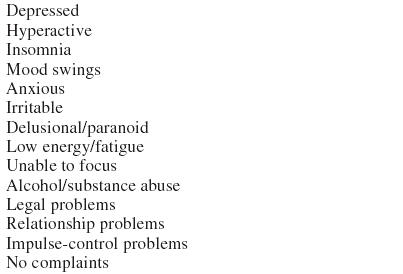
Primary care providers in the United States treat many patients with depression. Although 60% to 70% of patients with depression improve, about one third do not, and many do not achieve full remission.1 One reason for poor or incomplete response may be undiagnosed bipolar spectrum disorder. Bipolar spectrum disorders have been defined in a variety of ways2,3 but typically include bipolar I, bipolar II, cyclothymia, and bipolar disorder not otherwise specified. Signs and symptoms are diverse and include impulsive behavior, alcohol/substance abuse, fluctuations in energy level, and legal problems (Table 1). In addition, the depressed mood typically associated with the depressive phase of these disorders is often misdiagnosed as depression. Consequently, bipolar disorder may go unrecognized for 7 to 10 years.4,5 Furthermore, many patients with bipolar disorder undergo 3 or more professional evaluations before receiving correct diagnosis and treatment.4 The consequences of a delayed or incorrect diagnosis can be devastating, as the medical management of bipolar disorder differs substantially from that of depression. This article provides an overview for screening and diagnosis of bipolar disorder in the primary care setting.
Table 1.
Signs and Symptoms of Bipolar Disorder
FINANCIAL AND SOCIAL COSTS OF BIPOLAR DISORDER
According to 1991 data compiled by Wyatt and Henter,6 direct costs for inpatient and outpatient care associated with bipolar disorder are thought to total $7 billion. Indirect costs account for approximately $38 billion in expenditures.6 A more recent analysis reported by Begley and colleagues7 in 2001 suggests lifetime cost of patients diagnosed with bipolar disorder in 1998 will be $24 billion, with average lifetime cost per patient ranging from about $11,000 for persons with a single manic episode to over $600,000 for those with chronic or nonresponsive disease. Indeed, bipolar disorder is sixth among all health conditions in terms of causing disability across the world.8 Greater recognition of bipolar disorder warning signs in the primary care environment could very likely improve treatment outcomes, which could translate to a reduction in use of expensive treatment facilities.
Untreated/Misdiagnosed Bipolar Disorder
Results from the National Depressive and Manic-Depressive Association (NDMDA) survey4 indicate that 73% of patients with bipolar disorder were misdiagnosed on initial presentation to a health care professional. The most frequent misdiagnosis was depression. Other misdiagnoses included anxiety disorder, schizophrenia, personality disorder, and alcohol abuse.4
Several doctor's office clinical studies confirm these survey findings. For example, in 1 family practice setting, over one quarter of patients presenting with depression or anxiety suffered from bipolar spectrum disorder.9 Similarly, in a sample of 261 outpatients with bipolar disorder, Suppes and colleagues10 reported an average 10-year elapse between the first symptoms of bipolar disorder and first treatment. During this period, many patients received antidepressants without concurrent mood stabilizers. The situation is not improving. The NDMDA survey was repeated in 2000. Unfortunately, over one third of the new sample of bipolar patients waited at least 10 years for a correct diagnosis, just as in 1994.1
One reason for this substantial delay in diagnosis and appropriate treatment is that bipolar patients are misdiagnosed as suffering from unipolar depression. In a study of outpatients in a psychiatric clinic, over one third of patients with a history of mania or hypomania had been misdiagnosed as having unipolar depression.11 The consequences of this misdiagnosis were serious—55% of those prescribed antidepressants developed a manic/hypomanic episode, and 23% developed rapid cycling.11
The clinical course of bipolar disorder is pernicious. In patients with bipolar disorder, rates of suicide attempts have been estimated to range from 25% to 50%; the rate of suicide completion, based on a meta-analysis of 10 studies, is 19%, although rates vary considerably among studies (12%–60%).12 It has been calculated that patients spend one fifth of their lives in an episode of illness.13 Patients who are misdiagnosed as depressed and treated with antidepressants may experience rapid cycling and/or mania. Rapid cycling (4 or more mood episodes during the previous 12 months) occurs in 5% to 20% of patients with bipolar disorder.14
DIAGNOSING BIPOLAR DISORDER
The diagnosis of bipolar disorder requires a clinical evaluation, including a mental status examination and psychiatric history. The clinician must inquire about past episodes of mania, hypomania, and mood swings. Identifying high-risk patients may save the busy clinician valuable time. One method to identify high-risk patients is to screen for bipolar disorder, particularly among patients with depression.
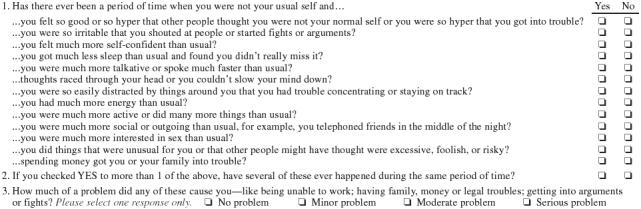
The Mood Disorder Questionnaire (MDQ) (Appendix 1)15 is a screening instrument for bipolar disorder that can easily be utilized in primary care settings. The MDQ has both good sensitivity and very good specificity.15 The MDQ can correctly identify 7 of 10 patients with bipolar disorder, while 9 of 10 patients without bipolar disorder would be correctly screened out. The MDQ includes 13 questions plus items assessing clustering of symptoms and functional impairment. The MDQ can provide primary care physicians with a quick and easy way to identify patients most likely to have bipolar disorder.
If the patient screens positive on the MDQ, the physician should proceed with a full clinical evaluation for bipolar disorder. Probing based on the MDQ responses may be helpful in guiding questions. Appropriate laboratory testing includes thyroid function tests and liver function tests.
Psychiatric Referral
When should primary care physicians refer patients suspected of having bipolar disorder to psychiatrists? Patients with current or past psychotic symptoms, those who are at risk for suicide or harm to others, and those whose symptoms are so severe that they may require hospitalization should be referred to a psychiatric specialist.
Follow-Up
Psychiatrists often are the initiators of treatment for bipolar disorder. Follow-up may be done by either the psychiatrist or the primary care physician. Patient and family education can help substantially with compliance and vigilance for early detection of relapse.
Appendix 1
The Mood Disorder Questionnaire
See also Editorial on page 7.
Footnotes
Preparation of this manuscript was supported by an educational grant from GlaxoSmithKline, Research Triangle Park, N.C., to ApotheCom Associates, Boston, Mass.
Dr. Hirschfeld has received grant/research support from Abbott, Bristol-Myers, GlaxoSmithKline, Organon, and Wyeth-Ayerst; has been a consultant or an advisory board member for Abbott, Bristol-Myers, GlaxoSmithKline, Forest, Lilly, Pfizer, Organon, Pharmacia & Upjohn, Janssen, Wyeth-Ayerst, Sepracor, and Novartis; and has been on the speakers' bureau of Abbott, Bristol-Myers, Forest, Lilly, Organon, and Pfizer.
REFERENCES
- National Depressive and Manic-Depressive Association. Perceptions and impact of bipolar disorder: how far have we really come? Presented at the 4th International Conference on Bipolar Disorder. 14–16June2001 Pittsburgh, Pa. [Google Scholar]
- Klerman GL. The spectrum of mania. Compr Psychiatry. 1981;22:11–20. doi: 10.1016/0010-440x(81)90049-3. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Pinto O. The evolving bipolar spectrum: prototypes I, II, III, IV. Psychiatr Clin North Am. 1999;22:517–524. doi: 10.1016/s0193-953x(05)70093-9. [DOI] [PubMed] [Google Scholar]
- Lish JD, Dime-Meenan S, Whybrow PC, et al. The National Depressive and Manic-Depressive Association (DMDA) survey of bipolar members. J Affect Disord. 1994;31:281–294. doi: 10.1016/0165-0327(94)90104-x. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Sachs GS, Chiou AM, et al. Is bipolar disorder still underdiagnosed? are antidepressants overutilized? J Affect Disord. 1999;52:135–144. doi: 10.1016/s0165-0327(98)00076-7. [DOI] [PubMed] [Google Scholar]
- Wyatt RJ, Henter I. An economic evaluation of manic-depressive illness—1991. Soc Psychiatry Psychiatr Epidemiol. 1995;30:213–219. doi: 10.1007/BF00789056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begley CE, Annegers JF, Swann AC, et al. The lifetime cost of bipolar disorder in the US: an estimate for new cases in 1998. Pharmacoeconomics. 2001;19:483–495. doi: 10.2165/00019053-200119050-00004. [DOI] [PubMed] [Google Scholar]
- Woods SW. The economic burden of bipolar disease. J Clin Psychiatry. 2000;61(suppl 13):38–41. [PubMed] [Google Scholar]
- Manning JS, Haykal RF, Connor PD, et al. On the nature of depressive and anxious states in a family practice setting: the high prevalence of bipolar II and related disorders in a cohort followed longitudinally. Compr Psychiatry. 1997;38:102–108. doi: 10.1016/s0010-440x(97)90089-4. [DOI] [PubMed] [Google Scholar]
- Suppes T, Leverich GS, Keck PE Jr, et al. The Stanley Foundation Bipolar Treatment Outcome Network, 2: demographics and illness characteristics of the first 261 patients. J Affect Disord. 2001;67:45–59. doi: 10.1016/s0165-0327(01)00432-3. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study [CME] J Clin Psychiatry. 2000;61:804–808. doi: 10.4088/jcp.v61n1013. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Jamison KR. Manic-Depressive Illness. New York, NY: Oxford University Press. 1990 [Google Scholar]
- Angst J, Sellaro R. Historical perspectives and natural history of bipolar disorder. Biol Psychiatry. 2000;48:445–457. doi: 10.1016/s0006-3223(00)00909-4. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Keck PE Jr. Rapid cycling. In: Dunner DL, ed. Current Psychiatric Therapy. Philadelphia, Pa: WB Saunders. 1993 [Google Scholar]
- Hirschfeld RMA, Williams JBW, Spitzer RL, et al. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000;157:1873–1875. doi: 10.1176/appi.ajp.157.11.1873. [DOI] [PubMed] [Google Scholar]


