Abstract
Objective:
Elevation and intermittent compression are routinely prescribed after soft tissue injury. Individuals must, however, resume activity in an upright position. The effect of gravity-dependent positioning after elevation and intermittent compression has not been extensively examined. Our purpose was to examine the effects of gravity-dependent positioning after elevation and intermittent compression on the volume of injured ankles.
Design and Setting:
Ankle-injured subjects were randomly assigned to 1 of 2 treatment groups: elevation or elevation and intermittent compression. Each treatment lasted 30 minutes.
Subjects:
Twelve college students with inversion ankle sprains 2 to 4 days earlier participated.
Measurements:
Measurements of ankle volume were performed before treatment and at 5, 10, 15, 20, 25, 30, 45, and 60 minutes after treatment.
Results:
Regardless of treatment, ankle volume decreased (by 17.25 ± 4.05 mL) between the pretreatment measurement and the immediate posttreatment measurement (P < .05). The effects of both treatments, however, lasted less than 5 minutes after the limb was returned to a gravity-dependent position.
Conclusions:
These results suggest that elevation or elevation and intermittent compression do not effectively decrease ankle volume for a prolonged period of time in patients with postacute ankle sprains.
Keywords: edema, effusion, swelling, volumetric measurement
Trauma or injury to the soft tissues or joints of the body is accompanied by local inflammation.1–3 Although inflammation indicates the start of the healing process, it often results in the formation of effusion (the escape of fluid from blood vessels) and edema (the accumulation of protein-rich fluid in the interstitial spaces).3 The ability of the individual to return to normal activity or athletic participation is often hindered by the swelling, pain, and functional decrements caused by edema.1–3 Therefore, control and resolution of edema are essential for early recovery after many musculoskeletal injuries.
Current methods of treatment directed at reducing edema are based on known principles affecting the lymphatic system, skeletal muscle contractions, local pressure gradients, and the influence of gravity. Common treatment methods include elevation, the application of elastic bandages, the combination of elastic bandages and foam pads, and various forms of pneumatic compression devices. These methods are directed at reducing edema by altering pressure gradients via compression of the local tissues.
Many investigators have studied the effects of elastic bandages and intermittent compression on edema. Rucinski et al4 measured edema in ankle sprains and found decreased volume after 30 minutes of elevation alone compared with increased volume after elevation and intermittent compression or elastic bandage wrap. Using computed tomography, Airaksinen et al5 found significant decreases in lower leg edema after 5 treatment sessions of intermittent pneumatic compression. Guskiewicz et al6 used a water-displacement tank to measure volumetric differences in ankle sprains treated with 3 external supports (elastic wrap with felt pads, Aircast Sport Stirrup [Aircast, Inc, Summit, NJ], Omni Multiphase orthoses [Omni Scientific, Inc, Concord, CA]). No significant differences in volume, level of function, or self-perception of symptoms were found among the groups.
Although the efficacy of some of these methods has been reported, information regarding the effect of gravity on edema resolution is sparse. The common protocol during rehabilitation of ankle sprains is to apply an edema-reduction modality, followed by rehabilitative exercises. These exercises are typically performed in an upright, or gravity-dependent, position, thus increasing resistance to venous and lymphatic drainage. Activity or exercise may also detrimentally affect edema by increasing blood flow in the involved areas, leading to an increase in filtration pressure and a rise in tissue osmolality.7 Therefore, the concomitant changes in blood flow and resistance from gravity produce an increase in edema.7,8 This reformation of edema after initial modality treatment has not been examined.
Our purpose was to examine the effects of gravity-dependent positioning after elevation and intermittent compression on the volume of postacute sprained ankles. A secondary goal was to determine the effectiveness of elevation and intermittent compression in reducing ankle edema.
METHODS
Subjects
Twelve subjects (8 males, 4 females, age = 19.0 ± 1.5 years, height = 176.0 ± 11.0 cm, mass = 72.9 ± 11.9 kg) participated in the study. Each subject presented with a postacute inversion ankle sprain (7 right, 5 left) sustained 2 to 4 days earlier. Upon visual inspection, the injured ankles were greater in volume than the uninjured ankles. Each subject read and signed an informed consent form in accordance with the university's internal review board, which approved the study. All testing was performed in the Pennsylvania State University Athletic Training Research Laboratory.
Procedures
Each subject rested for 10 minutes in a gravity-dependent position (sitting) before the initial measurement of ankle volume. After the 10-minute rest period, the subject's blood pressure was measured and recorded. After we obtained baseline volumetric measurements of both ankles, subjects assumed the supine position with the injured leg elevated to near vertical (Figures 1 and 2) either with or without simultaneous intermittent compression. Treatment lasted 30 minutes, after which the subject returned to a gravity-dependent position, sitting in a chair with both feet on the ground (Figure 3). After the treatment ended, we obtained volumetric measurements every 5 minutes for the first 30 minutes and at 45 minutes and 60 minutes posttreatment.
Figure 1.
Treatment position for elevation.
Figure 2.
Treatment position for elevation and intermittent compression.
Figure 3.
Gravity-dependent positioning.
The PresSsion intermittent compression pump (model 4322, Chattanooga Group, Inc, Chattanooga, TN) was used in conjunction with its pneumatic ankle garments to apply intermittent compression to the injured ankles. We followed guidelines established by the manufacturer for the application and operation of the garment and pump. The pressure level (mm Hg) of the pneumatic garment was set at the subject's measured diastolic blood pressure reading. A duty cycle of 3:1 was used (45 seconds of inflation, 15 seconds of deflation).
We quantified ankle volume by immersing the limb into a volumetric tank and weighed the displaced water (1 mL = 1 g). The reliability of this volumetric measurement system was established before this study: intraclass correlation coefficient = .99, standard error of measurement = 1.48 to 1.64 g.9
Before the initial measurement, we wiped the ankle and lower leg with a moist towel to minimize absorption of water by the skin. Before each immersion, the volumetric tank was filled with a standardized volume of room-temperature water. The subject was instructed to slowly immerse the ankle and foot into the volumetric tank, taking special care to not create waves. The subject was then instructed to position the foot so the medial border and heel of the immersed foot were touching the respective sides of the volumetric tank. We then marked this position, allowing for accurate repositioning with subsequent measurements. After immersion and positioning of the ankle, the water was allowed to settle before removal of the flow gate. The displaced water was collected in a graduated cylinder and then weighed on the digital scale.
The volumetric tank used in this study was a modified foot volumeter (Smith and Nephew, Inc, Carlsbad, CA). The tank is constructed of 0.5-cm-thick Plexiglas (Atoglas, Philadelphia, PA) with dimensions of 14 cm × 33 cm × 23 cm (width × length × height). To increase the accuracy of measurements, we modified the tank by repositioning the angled overflow spout to a horizontal position. A flow gate was added to control the movement of water through the overflow spout. The displaced water was measured on a calibrated digital scale (PS30, Mettler Toledo, Inc, Columbus, OH), which has a sensitivity of ±0.1 g.
Data Analysis
We used a 1-between (group) and 1-within (time) analysis of variance with repeated measures for time. Tukey Honestly Significant Difference post hoc analyses were performed for all significant findings. Level of significance (P < .05) was set a priori for all statistical analyses. To assess the magnitude of changes, effect sizes for various time periods were calculated as mean volume change/standard deviation of baseline. Analyses were performed with SPSS statistical software package (version 10.0; SPSS, Inc, Chicago, IL).
RESULTS
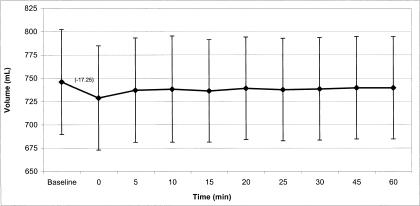
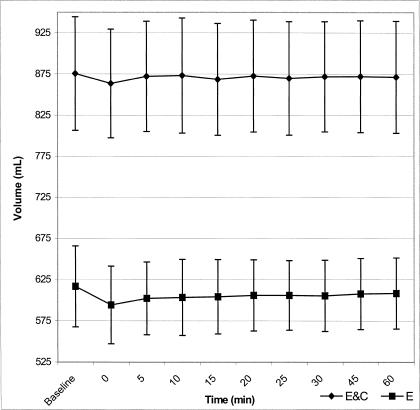
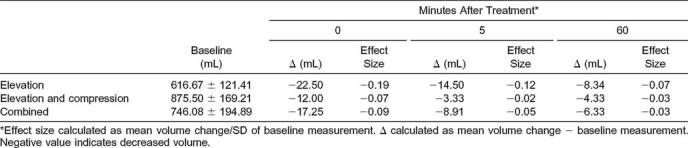
Injured ankles (746.08 ± 194.89 mL) were significantly larger than uninjured ankles (652.66 ± 184.47 mL) (P < .001). Regardless of treatment group, ankle volume was significantly decreased (by 17.25 ± 4.05 mL) between the pretreatment measurement and the immediate posttreatment measurement (P < .05); however, a small effect size of 0.09 was calculated for this time period. Tukey post hoc analyses revealed no significant differences between measurements at 5, 10, 15, 20, 25, 30, 45, or 60 minutes posttreatment and the baseline measurement, indicating that the effects of both treatments lasted for less than 5 minutes after the limb was returned to a gravity-dependent position (Figure 4). No significant interaction (P = .69, 1 − β = .7) or main effect for treatment group (P = .45, 1 − β = .9) were found (Figure 5). Small effect sizes (<0.19) were calculated (Table) for the elevation group, elevation and compression group, and combined groups at the 0-, 5-, and 60-minute time periods. The random assignment of subjects to treatment groups resulted in greater mean baseline ankle volumes in the elevation and compression group than in the elevation group (see Figure 5).
Figure 4.
Volume changes for treatment groups combined. P < .05.
Figure 5.
Volume changes by treatment groups. P = .691; 1 − β = .7. E&C indicates elevation and compression group; E, elevation group.
Effect-Size Calculations for 3 Time Periods (Mean ± SD)
DISCUSSION
The use of elevation and intermittent compression, separately or concomitantly, has become standard practice in the management of acute musculoskeletal injuries. These methods of treatment are directed at reducing edema based on principles affecting the lymphatic system, skeletal muscle contractions, local pressure gradients, and the influence of gravity. However, debate still exists among clinicians and researchers regarding the effectiveness of these treatments. Less understood is the effect of gravity-dependent positioning on the formation of edema. In our study, ankle volume decreased between the pretreatment and immediate posttreatment measurements; however, the effects of the treatment lasted for less than 5 minutes after the limb was returned to a gravity-dependent position. Our results suggest that elevation or elevation with intermittent compression of postacute ankle sprains does not effectively decrease edema or ankle volume for a prolonged period of time after treatment.
Our findings should be interpreted with care because of the small sample size, which produced only a modest power level of 1 − β = .7. The small effect sizes calculated for the various time periods attest to the minimal impact of the treatment conditions on ankle volume. However, a strength of our study is the reliability (intraclass correlation coefficient = .99) and precision of volumetric measurement (standard error of the mean = 1.48 to 1.64 g). The development of our protocol was previously reported9 and stems from the work of Dolan et al.10 Other researchers using similar volumetric measurement techniques have reported less precise measurements, with a standard error of the mean as large as 17 mL,11 which is often larger than reported volume changes. Differences in standard error of the mean are a result of technique and equipment. Standard volumetric measurement techniques use large beakers or graduated cylinders to collect the displaced volume of water. These items usually have large measurement intervals, requiring the investigator to estimate volume levels. The use of a digital scale, as in our protocol, removes the error of estimating and allows for precise measurement of water volume.
Gravity-Dependent Positioning
Elevation of an extremity after musculoskeletal injury is a universal treatment aimed at decreasing effusion and edema formation. It is generally accepted that elevation affects edema formation by altering the influences of gravity. When an extremity is in a gravity-dependent position, the force of gravity increases hydrostatic pressure in the peripheral blood vessels while also increasing resistance to venous and lymphatic flow. This results in an increase in fluid movement into the tissues, thereby increasing extremity volume. By placing the injured extremity in an elevated position, the force of gravity assists the return of fluids back to the heart via the venous and lymphatic systems and decreases hydrostatic pressure by resisting flow into the elevated peripheral vessels.
The effect of elevation and gravity-dependent positioning has been demonstrated in uninjured ankles.8,10,12 Sims8 examined the effects of positioning on ankle volume by placing his subjects in either a seated position or an elevated position. After 20 minutes, ankle volumetric measurements of the seated subjects were significantly larger than those of the elevated subjects. This effect was also demonstrated by investigators examining the impact of dependent positioning and water immersion on uninjured ankle volume.10,12 McCulloch and Boyd12 and Dolan et al10 reported increased ankle volume after dependent positioning in an empty whirlpool. McCulloch and Boyd12 also reported decreased ankle volume in subjects after 20 minutes of supine positioning.
The presence of edema may also influence the effects of elevation and gravity-dependent positioning. We9 previously used the same 30-minute elevation protocol on subjects with uninjured ankles and also found a decrease in ankle volume, but this effect lasted for at least 60 minutes after subjects returned to a gravity-dependent position. Findings from our current study support those of the previous investigators, as our subjects initially exhibited decreased ankle volume after 30 minutes of elevation, which quickly increased 5 minutes after they returned to a gravity-dependent position. We speculate that the homeostatic filtration process is exacerbated in the presence of edema (eg, increased tissue osmotic pressure), leading to the rapid increase in volume and minimizing the therapeutic effect of the treatment. These findings clearly illustrate the benefits of elevation treatment as well as the detrimental effects of gravity-dependent positioning in an edematous environment.
Intermittent Compression
The effectiveness of compression devices to reduce edema resides in their ability to affect the pressure gradient of the disrupted environment. Starling forces describe the regulation of movement across the endothelial membrane of the capillaries.3,13 In general, capillary osmotic pressure and the actions of the lymphatic system are sufficient to maintain a homeostatic environment. After injury, effusion and edema develop as a result of disruption to the normal filtration gradient between the arterioles and venules (ie, the capillaries). The movement of substances across the capillary membrane increases because of membrane derangement from physical trauma and the actions of various chemical mediators. The result is an increase in tissue osmotic pressure and a decrease in capillary osmotic pressure. Effusion and edema develop as the lymphatic system is overwhelmed by the influx of movement out of the capillaries. It is also important to remember that effusion develops in both the interstitial and intra-articular spaces.
Compression devices are usually applied in the form of elastic bandages or pneumatic units that allow control of intermittent or sequential pressures (or both). External compression devices, such as elastic wraps and pneumatic compression garments, can increase tissue hydrostatic pressure when applied over the area of effusion and edema. Although the increase in tissue hydrostatic pressure can assist in moving fluid across the capillary membrane and back into the venules, protein and debris are not affected, as they are only removed via the lymphatic vessels.
Previous investigations on the effectiveness of the pneumatic compression devices in reducing edema have resulted in conflicting findings.5,14–17 Using a computed-tomography technique, Airaksinen et al5 demonstrated decreased edema and increased tissue density in the lower leg after intermittent pneumatic compression. Similarly, Baulieu et al15 noted beneficial effects of intermittent pneumatic compression on upper extremity and lower extremity edema using radionuclide lymphography. Thordarson et al16,17 reported decreased ankle volumes in subjects with acute ankle fractures exposed to a pneumatic compression device applied to the foot preoperatively and postoperatively. Gardner et al14 also reported beneficial effects in subjects with various lower extremity conditions but attributed volume changes to the activation of a venous pump in the foot. Wilkerson and Horn-Kingery18 examined different focal-compression techniques on ankle volume after inversion ankle sprains. Focal compression was beneficial, but the techniques did not differ statistically.
Conflicting results were presented by Rucinski et al,4 who compared intermittent compression, elastic wrap, and elevation in subjects with acute ankle sprains. Ankle volume decreased in the subjects who elevated, but those using intermittent compression and elastic wrap experienced increases in ankle volume. Our findings appear to support those of Rucinski et al,4 as we failed to demonstrate any additional benefits from the concomitant application of intermittent compression and elevation on the volume of injured ankles. A plausible explanation for our findings may be found in examining the structure of the lymphatic vessels.
The most peripheral structures of the lymphatic system are the lymphatic capillaries making up the lymphatic vessels, which are otherwise known as terminal lymphatics. The capillaries begin blindly (have a closed end) in most tissues of the body and consist of a sac of thin endothelial cells that loosely overlap. The cells are not joined together by tight junctions as they are in the blood capillaries. This design permits the flaps to open large enough gaps to allow the entry of bacteria and proteins. These cells are tethered to the surrounding tissue by protein filaments, which prevent the cells from collapsing. As effusion and edema develop, the connective fibers are placed under tension and the flaps are pulled open.3,19,20 If the tension becomes too great, the cells can be pulled apart and overdistended, making the flaps ineffective.
We theorize that adding intermittent compression to the injured area may have increased pressures to a level that overdistended the flaps, making them ineffective. Although we used standard protocols and recommendations for intermittent-compression treatments, these guidelines are vague and do not address existing pressure levels in the injured environment. Standard protocols recommend applying compression at levels between 30 mm Hg and the diastolic blood pressure of the individual.1,2 Pressure levels above the diastolic blood pressure are believed to cause distention of the lymphatics or collapse of local circulatory vessels or both.2 Similar to most other researchers, we did not assess the preexisting pressure of the edematous ankle before the intermittent compression was applied; therefore, the additional increase in pressure may have exceeded optimal treatment levels.
Previous investigators have demonstrating the beneficial effects of compression,5,14–17 so further examination into the topic is warranted. Areas of focus should include (1) optimal compression levels that will not overdistend the flaps, (2) various settings for on-off ratios during application, and (3) comparison between static intermittent compression and constant compression.
In conclusion, although ankle volume decreased between the pretreatment and immediate posttreatment measurements, whether subjects received elevation or elevation and intermittent compression, effects of the treatment lasted for less than 5 minutes after the limb was returned to a gravity-dependent position. We suggest that elevation or elevation with intermittent compression is effective in decreasing ankle volume after ankle sprain, but the change is not prolonged in the presence of edema.
ACKNOWLEDGMENTS
This study was supported by a grant from the Ronald M. and Susan J. Friedman Student Fund, Pennsylvania State University, Department of Kinesiology, 1999. We thank W.E. Buckley, PhD, ATC, for his support and guidance and his invaluable assistance in obtaining funding for this study. We also thank Todd Evans, PhD, ATC, CSCS, for his assistance in the review of the data analysis.
REFERENCES
- 1.Starkey C. Therapeutic Modalities. 2nd ed. Philadelphia, PA: FA Davis Co; 1993. [Google Scholar]
- 2.Prentice WE. Therapeutic Modalities in Sports Medicine. 4th ed. Boston, MA: WCB McGraw-Hill; 1999. [Google Scholar]
- 3.Manjo G, Joris I. Cells, Tissues, and Disease: Principles of General Pathology. Cambridge, United Kingdom: Blackwell Science; 1996. [Google Scholar]
- 4.Rucinski TJ, Hooker DN, Prentice WE, Shields EW, Cote-Murray DJ. The effects of intermittent compression on edema in postacute ankle sprains. J Orthop Sports Phys Ther. 1991;14:65–69. doi: 10.2519/jospt.1991.14.2.65. [DOI] [PubMed] [Google Scholar]
- 5.Airaksinen O, Partanen K, Kolari PJ, Soimakallio S. Intermittent pneumatic compression therapy in posttraumatic lower limb edema: computed tomography and clinical measurements. Arch Phys Med Rehabil. 1991;72:667–670. [PubMed] [Google Scholar]
- 6.Guskiewicz KM, Riemann BL, Onate JA. Comparison of 3 methods of external support for management of acute lateral ankle sprains. J Athl Train. 1999;34:5–10. [PMC free article] [PubMed] [Google Scholar]
- 7.Cloughley WB, Mawdsley RH. Effect of running on volume of the foot and ankle. J Orthop Sports Phys Ther. 1995;22:151–154. doi: 10.2519/jospt.1995.22.4.151. [DOI] [PubMed] [Google Scholar]
- 8.Sims D. Effects of positioning on ankle edema. J Orthop Sports Phys Ther. 1986;8:30–33. doi: 10.2519/jospt.1986.8.1.30. [DOI] [PubMed] [Google Scholar]
- 9.Tsang KKW, Hertel J, Denegar CR, Buckley WE. The effects of gravity dependent positioning following elevation on the volume of uninjured ankle [abstract] J Athl Train. 2000;35(suppl):S50. [Google Scholar]
- 10.Dolan MG, Mendel FM, Teprovich JM, Marvar PJ, Bibi KW. Effects of dependent positioning and cold water immersions on non-traumatized ankle volumes [abstract] J Athl Train. 1999;34(suppl):S17. [Google Scholar]
- 11.Petersen EJ, Irish SM, Lyons CL, et al. Reliability of water volumetry and figure-of-eight method on subjects with ankle joint swelling. J Orthop Sports Phys Ther. 1999;29:609–615. doi: 10.2519/jospt.1999.29.10.609. [DOI] [PubMed] [Google Scholar]
- 12.McCulloch J, Boyd VB. The effects of whirlpool and the dependent position on lower extremity volume. J Orthop Sports Phys Ther. 1992;16:169–173. doi: 10.2519/jospt.1992.16.4.169. [DOI] [PubMed] [Google Scholar]
- 13.Knight KL. Cryotherapy: Theory, Technique, and Physiology. 1st ed. Chattanooga, TN: Chattanooga Corp; 1985. [Google Scholar]
- 14.Gardner AMN, Fox RH, Lawrence C, Bunker TD, Ling RSM, MacEachern AG. Reduction of post-traumatic swelling and compartment pressure by impulse compression of the foot. J Bone Joint Surg Br. 1990;72:810–815. doi: 10.1302/0301-620X.72B5.2211762. [DOI] [PubMed] [Google Scholar]
- 15.Baulieu F, Baulieu JL, Vaillant L, Secchi V, Barsotti J. Factorial analysis in radionuclide lymphography: assessment of the effects of sequential pneumatic compression. Lymphology. 1989;22:178–185. [PubMed] [Google Scholar]
- 16.Thordarson DB, Ghalambor N, Perlman M. Intermittent pneumatic pedal compression and edema resolution after acute ankle fracture: a prospective, randomized study. Foot Ankle Int. 1997;18:347–350. doi: 10.1177/107110079701800607. [DOI] [PubMed] [Google Scholar]
- 17.Thordarson DB, Greene N, Shepherd L, Perlman M. Facilitating edema resolution with a foot pump after calcaneus fracture. J Orthop Trauma. 1999;13:43–46. doi: 10.1097/00005131-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Wilkerson GB, Horn-Kingery HM. Treatment of the inversion ankle sprain: comparison of different modes of compression and cryotherapy. J Orthop Sports Phys Ther. 1993;17:240–246. doi: 10.2519/jospt.1993.17.5.240. [DOI] [PubMed] [Google Scholar]
- 19.Kolb P, Denegar C. Traumatic edema and the lymphatic system. Athl Train J Natl Athl Train Assoc. 1983;18:339–341. [Google Scholar]
- 20.Guyton AC. Textbook of Medical Physiology. 6th ed. Philadelphia, PA: WB Saunders Co; 1981. [Google Scholar]