Abstract
The main options for the treatment of wrist ganglia are reassurance, aspiration, arthroscopic resection and open excision. Variations within each option have been described and the literature is clouded by widespread variability in the results reported. We present the results of our own long-term retrospective study, review the literature and question the surgical risks and demands placed on healthcare resources. A retrospective review of the surgical results of dorsal and volar wrist ganglia excision between January 1998 and March 2005 was undertaken at a single institution. Of the 152 patients in this consecutive series, 117 (77%) patients responded to a telephone questionnaire. The mean length of follow-up in this series of 117 patients was 4.2 years (range 1.5–8.7 years). The overall recurrence rate following excision of all wrist ganglia in this series was 41.8 %. When looking just at volar ganglia, the risk of recurrence is higher at 46.8%. Should the ganglion recur, the risk of developing a moderate to severely tender scar is 34.6% and the risk of developing an unsightly scar is 8.2%. This study questions the effectiveness of surgical excision in the treatment of wrist ganglia when performed by a mixture of surgeons in that the recurrence rates are very similar to the rates seen in studies that merely observe or aspirate wrist ganglia. We propose that for symptomatic ganglia, specialists in hand surgery may be more appropriate at treating such a pathology.
Key words: wrist ganglia, patient satisfaction, recurrence.
Introduction
Ganglions are mucin filled cysts which may be uni- or multi-lobulated. They are the most common soft tissue tumour of the hand, representing up to 70% of all such tumors. Dorsal wrist ganglia represent 70% of all ganglia and volar wrist ganglia up to 20%.1 Different treatments for wrist ganglia have been described and are as varied as opinion on their etiology. The treatments range from simple observation2 to aspiration with2–6 or without injection of various agents7–9 to arthroscopic resection10–13 and open excision.12,14–17 Recurrence rates have been documented widely, varying from 1% reported by Angelides and Wallace in 197614 to 42%18 for open excision. Arthroscopic resection of dorsal and more recently volar ganglia show a recurrence rate up to 7%.19 Few studies have reported large case series with long-term follow-up and patient satisfaction. The purpose of this study was to review the results of surgical excision in a single institution regardless of previous ganglion aspiration with reference to recurrence, scar tenderness, scar cosmesis and overall satisfaction and compare these results to the current literature.
Patients and Methods
A retrospective review was performed on 152 consecutive patients undergoing surgical excision of dorsal and volar wrist ganglia between January 1998 and March 2005. Surgery was performed at The Royal Free Hospital NHS Trust by both junior and senior surgeons in the specialities of Orthopaedic, General and Plastic Surgery. Patients were tracked using an electronic patient database. One hundred and seventeen (77%) patients (34 male, 83 female) responded to a telephone questionnaire. There were 35 non-responders (23%) that either did not consent to be involved in the study or were lost to follow-up due to inadequate data recording or because of a change of address.
The patient cohort consisted of all patients undergoing surgical excision of wrist ganglia regardless of age. The minimum follow-up was 1.5 years and patients who had previously had their ganglion aspirated were also included. No arthroscopic resections were performed.
From the clinical notes and a telephone interview we determined: 1) recurrence of the ganglia after excision, 2) whether further surgery was performed, 3) previous aspiration of the ganglion, 4) scar tenderness, 5) dissatisfaction of scar cosmesis, 6) overall satisfaction and 7) whether in hindsight the patient would have the procedure again.
Results
The mean length of follow-up in this series of 117 patients was 4.2 years (range 1.5–8.7 years). The mean age of the 34 (29%) males was 40.6 years (range 9.2–85.7 years) and for the 83 (71%) females was 41.9 years (range 10.4–88.7 years). Ganglia were located on the dorsal aspect of 40 (34%) patients and on the volar aspect of 77 (66%) patients. The overall recurrence rate for the series was 41.8% (49 patients). There was recurrence in 13 (32.5%) dorsal and 36 (46.8%) volar ganglia. There was no difference in gender predominance for recurrence: 14 recurrences in 34 males (41.2%) and 35 recurrences in 83 females (42.2%). Of these 49 patients, 9 underwent further surgical excision, with no subsequent recurrence. A total of thirty-one (26%) patients had a previous aspiration of their ganglion. Eighteen of the 49 recurrences had a previous aspiration (36.7%) and thus 58% of ganglia that had recurred after aspiration, also recurred following surgical excision.
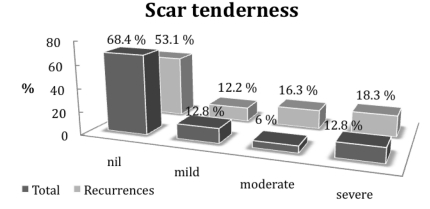
Patients graded scar tenderness subjectively as nil, mild, moderate or severe. In the recurrence group, 6/14 males (42.8%) described moderate pain and 11/35 females (31.4%) described severe pain. Thus 17/49 (34.6%) described moderate to severe pain in this group (Figure 1).
Figure 1.
Comparison of scar tenderness as a percentage in total patient cohort compared with those with ganglion recurrence.
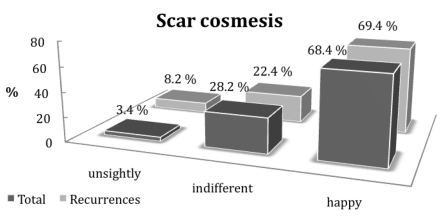
Patient's opinion on their scar cosmesis was graded subjectively as unsightly, indifferent or happy. Four out of 49 patients (8.2%) with recurrent ganglia complained of unsightly scars compared with 3.4% of the entire patient group (Figure 2).
Figure 2.
Comparison of scar cosmesis as a percentage in total patient cohort compared with those with ganglion recurrence.
On direct questioning of this recurrence group, 25 of the 49 were not satisfied with the treatment but only 19 would not have had the surgery if given the choice again. Eighty-six (74%) patients claimed that they were satisfied with the overall result of their surgery. Of the thirty-one (26%) patients who were not satisfied, 22 would not have had the surgery if given the choice again.
Discussion
Ganglions are mucin filled cysts which may be uni- or multi-lobulated and are closely associated with either the wrist joint or tendon sheath. They are the commonest benign tumors of the hand accounting for up to 70% of all such tumors. Dorsal wrist ganglia represent up to 70% of all ganglia and volar wrist ganglia up to 20%.1 They may affect any age group, however, they are more common in the twenties to forties. Incidence in males is 25/100,000 and in females 43/100,000. Prevalence is 19% in patients reporting wrist pain and 51% in the asymptomatic population.20
Patients are often referred to hand surgeons for evaluation due to cosmesis (38%), for fear that the lesion may be malignant (28%), pain (26%) or altered sensation (8%).21 Ganglions may fluctuate in size over time and restrict wrist movement. For small occult ganglia that are not palpable but cause pain, magnetic resonance imaging or ultrasound is of value in characterizing these lesions.22,23
The main options for the treatment of wrist ganglia are reassurance,2 aspiration with2–6 or without7–9 injection of various agents, arthroscopic resection10–13 or open excision.12,14–17 The literature is clouded by widespread variability in the results reported.
During consultation, patients are often concerned by the nature of the lesion. Simply discussing the benign nature of the ganglion can allay fear. It is important to highlight the natural history of the ganglion, which may fluctuate in size over time. Mc Evedy demonstrated that 40% of lesions become smaller with no treatment.2 If the ganglion is symptomatic, aspiration can immediately reduce size and provide reassurance to the patient. Aspiration alone has shown success in 33–85% of patients.6–9 Results for aspiration with the injection of various agents; hyaluronidase,3 sclerosant2 and steroid3–5 have shown success in 57%, 81% and 60–85%, respectively. Varley et al.6 however reported a 33% success rate with aspiration and found additional injecting with steroid added no benefit to success but did have a risk of subcutaneous fat necrosis and a change in skin color.
The indications for arthroscopic ganglion resection or open excision include pain, interference with activity, nerve compression or patient request.13 Arthroscopic resection of ganglia was originally described by Osterman and Raphael.24 It is technically demanding and occasionally requires several ports for access to identify the origin of the ganglion. Results have been promising with recurrence in series from 0%10 to 7%.1,9 However most of the early studies have been small series with short follow-up time. Conversion to an open excision may be required in difficult cases or where there is an intraoperative complication such as hematoma formation or identifiable nerve injury.
Open excision of ganglia have generally been thought to offer good results perhaps on the basis of Angelides and Wallace's study14 reporting a 1% recurrence rate following 346 dorsal wrist ganglion excisions. Clay and Clement15 had a similar low recurrence rate of 3% following 62 dorsal ganglion excisions. However, there have also been series reporting much higher recurrence rates: McEvedy2 reported 40% recurrence following the excision of both dorsal and volar ganglia, Jacobs and Govaers25 reported a rate of 28% and more recently Dias et al.16 have reported a 39% recurrence rate in a six year prospective study of dorsal ganglion excision.
Few studies have reported large case series with long-term follow-up and patient satisfaction. In this study, reviewing surgical excision of wrist ganglia, the overall recurrence rate of dorsal and volar excisions was 41.8%. When subdivided into dorsal and volar ganglia, the rates were 32.5% and 46.8%, respectively. This higher rate seen on the volar surface are comparable to those of Dias and Buch18 and may represent a technically more difficult operation with inadequate excision of the ganglion base due to anatomy on the volar side. The demographics of our study are also comparable with this study regarding sex distribution (females>males) and the average age of the patient group. The increased prevalence of ganglia on the volar aspect are also consistent with prevalence of wrist ganglia in asymptomatic patients in Lowden's study using MRI scans of the wrist.20
A limitation of this study was the 77% (117 patients) response rate of the telephone survey. This was due to either patients not consenting to be involved in the study or being lost to follow-up due to inadequate data recording or because of a change of address. We believe that a 77% response rate for a retrospective study over nine years is a realistic response rate for studies with this methodology.
Whilst this study has looked at the results of surgical treatment of wrist ganglia, information regarding previous attempted aspiration of the ganglia was also collected. This showed that 31 of the 117 ganglia coming to surgery had had an attempted aspiration (26.5%). When reviewing the recurrences of ganglia following surgery it is seen that 18 of the 49 had previous attempted aspiration (36.7%). Dias et al.16 showed in their prospective review that recurrence after aspiration could be as high as 58%. Whether there is a direct effect of attempting to aspirate the ganglion and subsequently increasing the risk of recurrence following surgery can only be ascertained by further studies.
When reviewing patient satisfaction regarding their treatment, it can be seen that despite 49 patients being in the recurrence group, 24 of this group were still satisfied with their treatment. In addition, when asked directly whether they would proceed with surgery again knowing the risks of recurrence, 30 of the 49 would still have surgery. This reinforces that appropriate consent is of the utmost importance as well informed patients are more satisfied with treatment despite there being a recurrence and associated morbidity of scar tenderness or an unsightly scar.
The variability shown in the literature with regards to recurrence rates demonstrates that ganglion surgery is challenging. In principal complete removal of the ganglion base is required to avoid recurrence. The cases of recurrence are often due to incomplete ganglion stalk resection, which is greater on the volar aspect due to the more complex volar anatomy. The risks of complication are higher because of the proximity of the superficial palmar branch of the radial artery, the terminal branches of the superficial radial nerve and the palmar cutaneous branch of the median nerve.12,26
Surgical treatment of wrist ganglions must not be undertaken without careful consent. Hand surgeons experienced in treating hand and wrist pathology should perform arthroscopic resection or open excision. Aspiration of ganglia may be used as a temporizing measure for painful, symptomatic ganglia, however, patients must be informed of the likelihood of recurrence.
Conclusion
The overall recurrence rate following excision of all wrist ganglia in this series was 41.8%. When looking just at volar ganglia the risk of recurrence is higher at 46.8%. Should the ganglion recur, the risk of developing a moderate to severely tender scar is 34.6% and the risk of developing an unsightly scar is 8.2%. This study questions the effectiveness of surgical intervention in the treatment of wrist ganglia when performed by a mixture of surgeons in that the recurrence rates are very similar to the rates seen in studies that merely observe or aspirate wrist ganglia. Ganglion surgery is challenging and one has to question the surgical risks that are undertaken and also the demands that surgical treatment places on healthcare resources. We propose that for symptomatic ganglia specialist hand surgeons should perform surgery as this will reduce recurrence rates.
Acknowledgments
SL, VR and PA contributed to the design of the study, drafting the script and final approval of the final script. SL acquired the data, analyzed and interpreted the data, and designed the graphs. VR analyzed and interpreted the data.
References
- 1.Angelides AC. Ganglions of the hand and wrist. In: Green DP, editor. Green's Operative Hand Surgery. 4th ed. Vol. 2. New York: Churchill Livingstone; 1998. pp. 2171–83. [Google Scholar]
- 2.McEvedy BV. The simple ganglion: a review of modes of treatment and an explanation of the frequent failures of surgery. Lancet. 1954;16(266):135–6. doi: 10.1016/s0140-6736(54)90983-6. [DOI] [PubMed] [Google Scholar]
- 3.Nelson CL, Sawmiller S, Phalen GS. Ganglions of the wrist and hand. J Bone Joint Surg Am. 1972;5:1459–64. [PubMed] [Google Scholar]
- 4.Holm PCA, Pandsey SD. Treatment of ganglia of the hand and wrist with aspiration and injection of hydrocortisone. The Hand. 1972;5:63–8. doi: 10.1016/0072-968x(73)90013-2. [DOI] [PubMed] [Google Scholar]
- 5.Derbyshire RC. Observation on the treatment of ganglia. With a report on hydrocortisone. Am J Surg. 1973;112:635–6. doi: 10.1016/0002-9610(66)90094-8. [DOI] [PubMed] [Google Scholar]
- 6.Varley GW, Needoff M, Davis TR, Clay NR. Conservative management of wrist ganglia. Aspiration versus steroid infiltration. J Hand Surg [Br] 1997;22:636–7. doi: 10.1016/s0266-7681(97)80363-4. [DOI] [PubMed] [Google Scholar]
- 7.Richman JA, Gelberman RH, Engber WD, Salamon PB, Bean DJ. Ganglions of the wrist and digits: results of treatment by aspiration and cyst wall puncture. J Hand Surg [Am] 1987;12:1041–3. doi: 10.1016/s0363-5023(87)80108-9. [DOI] [PubMed] [Google Scholar]
- 8.Nield DV, Evans DM. Aspiration of ganglia. J Hand Surgery. J Hand Surg [Br] 1986;11:264–264. doi: 10.1016/0266-7681(86)90278-0. [DOI] [PubMed] [Google Scholar]
- 9.Zubowicz VN, Ishii CH. Management of ganglion cysts of the hand by simple aspiration and cyst wall puncture. J Hand Surg. 1987;12A:618–20. doi: 10.1016/s0363-5023(87)80221-6. [DOI] [PubMed] [Google Scholar]
- 10.Ho PC, Lo WN, Hung LK. Arthroscopic resection of volar ganglion of the wrist. A new technique. Arthroscopy. 2003;19:218–21. doi: 10.1053/jars.2003.50035. [DOI] [PubMed] [Google Scholar]
- 11.Mathoulin C, Hoyos A, Pelaez J. Arthroscopic resection of wrist ganglia. Hand Surg. 2004;9:159–64. doi: 10.1142/s0218810404002169. [DOI] [PubMed] [Google Scholar]
- 12.Rocchi L, Canal A, Fanfani F, Catalano F. Articular ganglia of the volar aspect of the wrist: arthroscopic resection compared with open excision. A prospective randomised study. Scan J Plast Reconstr Surg and Hand Surg. 2008;42:253–9. doi: 10.1080/02844310802210897. [DOI] [PubMed] [Google Scholar]
- 13.Luchetti R, Badia A, Alfarano M, et al. Arthroscopic resection of dorsal wrist ganglia and treatment of recurrences. J Hand Surg. 2000;25B:38–40. doi: 10.1054/jhsb.1999.0290. [DOI] [PubMed] [Google Scholar]
- 14.Angelides AC, Wallace PF. The dorsal ganglion of the wrist: its pathogenesis, gross and microscopic anatomy, and surgical treatment. J Hand Surg [Am] 1976;1:228–35. doi: 10.1016/s0363-5023(76)80042-1. [DOI] [PubMed] [Google Scholar]
- 15.Clay NR, Clement DA. The treatment of dorsal wrist ganglia by radical excision. J Hand Surg [Br] 1988;13:187–91. doi: 10.1016/0266-7681_88_90135-0. [DOI] [PubMed] [Google Scholar]
- 16.Dias JJ, Dhukaram V, Kumar P. The natural history of untreated dorsal wrist ganglia and patient reported outcome 6 years after intervention. J Hand Surg Eur Vol. 2007;32:502–8. doi: 10.1016/J.JHSE.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Faithfull DK, Seeto BG. The simple wrist ganglion – more than a minor surgical procedure? Hand Surg. 2000;5:139–43. doi: 10.1142/s0218810400000235. [DOI] [PubMed] [Google Scholar]
- 18.Dias J, Buch K. Palmar wrist ganglion: does intervention improve outcome? A prospective study of natural history and patient reported treatment outcomes. J Hand Surg [Br] 2003;28:172–6. doi: 10.1016/s0266-7681(02)00365-0. [DOI] [PubMed] [Google Scholar]
- 19.Pederzini L, Ghinelli L, Soragni O. Arthroscopic treatment of dorsal arthrogenic cysts of the wrist. J Sports Traumatol and Related Res. 1995;17:210–15. [Google Scholar]
- 20.Lowden CM, Attiah M, Garvin G, et al. The prevalence of wrist ganglia in an asymptomatic population: Magnetic resonance evaluation. J Hand Surg [Br] 2005;30:302–6. doi: 10.1016/j.jhsb.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 21.Westbrook AP, Stephen AB, Oni J, Davis TR. Ganglia: the patient's perception. J hand Surg [Br] 2000;25:566–7. doi: 10.1054/jhsb.2000.0504. [DOI] [PubMed] [Google Scholar]
- 22.Teefey SA, Dahiya H, Middleton WD, et al. Ganglia of the hand and wrist: a sonographic analysis. AJR Am J Roentgenol. 2008;191:716–20. doi: 10.2214/AJR.07.3438. [DOI] [PubMed] [Google Scholar]
- 23.Goldsmith S, Yang SS. Magnetic imaging in the diagnosis of occult dorsal wrist ganglions. J Hand Surg Eur Vol. 2008;33:595–9. doi: 10.1177/1753193408092041. [DOI] [PubMed] [Google Scholar]
- 24.Osterman LA, Raphael j. Arthroscopic resection of dorsal ganglion of the wrist. Hand Clinics. 1995;11:7–12. [PubMed] [Google Scholar]
- 25.Jacobs LG, Govaers KJ. The volar wrist ganglion: just a simple cyst? J Hand Surg [Br] 1990;15:342–6. doi: 10.1016/0266-7681_90_90015-v. [DOI] [PubMed] [Google Scholar]
- 26.Rocchi L, Canal R, Pelaez J, et al. Results and complications in dorsal and volar wrist ganglia arthroscopic resection. Hand Surg. 2006;11:21–6. doi: 10.1142/S0218810406003127. [DOI] [PubMed] [Google Scholar]