Abstract
Developmental dysplasia of the hip (DDH) is a spectrum of anatomical abnormalities of the hip joint in which the femoral head has an abnormal relationship with the acetabulum. Most studies report an incidence of 1 to 34 cases per 1,000 live births and differences could be due to different diagnostic methods and timing of evaluation. Risk factors include first born status, female sex, positive family history, breech presentation and oligohydramnios. Clinical presentations of DDH depend on the age of the child. Newborns present with hip instability, infants have limited hip abduction on examination, and older children and adolescents present with limping, joint pain, and/or osteoarthritis. Repeated, careful examination of all infants from birth and throughout the first year of life until the child begins walking is important to prevent late cases. Provocative testing includes the Barlow and Ortolani maneuvers. Other signs, such as shorting of the femur with hips and knees flexed (Galeazzi sign), asymmetry of the thigh or gluteal folds, and discrepancy of leg lengths are potential clues. Treatment depends on age at presentation and outcomes are much better when the child is treated early, particularly during the first six months of life.
Key words: developmental dysplasia of the hip.
Terminology
The term developmental dysplasia of the hip (DDH) has replaced congenital dislocation of the hip as it describes the full range of abnormalities affecting the immature hip more accurately. Some children may have a normal femoro-acetabular relationship at birth and only later go on to develop a dysplastic hip.1
Definitions
Any abnormality in the shape, size and orientation of the femoral head, acetabulum or both is referred to as hip dysplasia. It has been seen that the majority of abnormalities arise as a result of maldevelopment of the acetabulum. The femoral head is involved secondarily as a result of non-physiological biomechanics from the anteverted acetabulum or as a result of treatment.
A hip is unstable when the tight fit between the femoral head and the acetabulum is lost and the femoral head is able to move within or outside the confines of the acetabulum.2 Subluxation of hip refers to incomplete contact between the articular surfaces of the femoral head and acetabulum. A dislocated hip has no contact between the femoral head and acetabulum. A teratologic dislocation of the hip (TDH) shows very marked and advanced changes in the hip joint at the time of birth and is in a fixed dislocated position. There is an association with other severe malformations, such as spina bifida, arthrogryposis multiplex congenita, lumbosacral agenesis, chromosomal abnormalities, diastrophic dwarfism, Larsen syndrome and other rare syndromes.3
Epidemiology
The exact incidence of DDH is difficult to determine because of a discrepancy in definition of the condition, type of examination used and different levels of skills of clinicians. The incidence ranges from as low as 1 per 1,000 to as high as 34 per 1,000. Higher incidences are reported when ultrasonography is also used in addition to clinical examination.4 Risk factors include first born status, female sex, positive family history, breech presentation and oligohydramnios.5 Carter and Wilkinson reported an overall incidence of one per 1,000 live births, with one in 600 girls and one in 4,000 boys having the disorder.6 Other associated factors include ethnic background (e.g. native Americans who use swaddling that forces the hips into extension and adduction), torticollis and lower limb deformity.7
Etiology
The etiology of DDH is multi factorial. There are a number of predisposing factors that lead to the development of DDH, including ligament laxity, breech presentation, postnatal positioning and primary acetabular dysplasia.
Hereditary ligament laxity and other neuropediatric disorders with an abnormal muscle tension, such as cerebral palsy, myelomeningocele and arthrogryposis, are the major factors for the inheritance of DDH.8 There is increased incidence of DDH in identical twins as compared to fraternal twins, also suggesting a genetic influence. Female newborns are more prone to develop DDH as they respond to maternal relaxing hormones which cross the placenta and induce laxity.
Intrauterine crowding also affects the developing hip. There is an increased incidence of DDH in infants who are born in breech presentation, most notably when the knees are extended.9 Other factors include first born child and oligohydramnios. In addition, postnatal positioning also plays a role in the development of DDH. A higher incidence of DDH is reported in babies wrapped with the hip in extended position, as compared to the babies wrapped in flexed and abducted position. Also, a permanent supine position of newborns which can reduce the risk of sudden infant death seems to increase the risk of DDH.
Natural history
A failed diagnosis of DDH may follow one of four clinical patterns: the hip may reduce spontaneously, it may sublux and maintain partial contact, it can develop frank dislocation, or it can develop dysplastic features whilst remaining located.10
The natural history of untreated hip dysplasia can be more variable with some patients presenting with minor symptoms and others only found to have hip dysplasia as an incidental finding on radiographic imaging. There is growing evidence, however, that hip dysplasia leads to progressive degenerative joint disease in adults, in particular females.11 Long-term follow up of treated subluxed and dysplastic hips also revealed a higher incidence of degenerative joint disease in hips that re-subluxed over time.12 The reasons behind this phenomenon are probably mechanical and related to a high degree of contact stress over time on a relatively small surface area.
Diagnosis
A careful clinical examination should be carried out on all newborn children especially those with risk factors for DDH. Routine screening should include both the Ortolani test and the Barlow maneuver, and each hip should be examined separately. For physical examination, the child should be completely relaxed, on a smooth, warm, comfortable surface in a quiet environment. Roser first reported hip instability in newborn infants in 1879. In 1910, Le Damany and Saiget described a clinical test for hip instability and this was highlighted in 1937 by Ortolani. Palmen in 1961 and Barlow in 1962 developed further tests to provoke dislocation or subluxation.13 Although the clinical tests described below can be a helpful diagnostic tool, a repetition of the maneuvers is not indicated due to increased risk of an iatrogenic damage to the cartilage.
In the Ortolani test, the baby should be supine with hips flexed to 90 degrees. The examiner's index and long fingers are placed laterally over the child's greater trochanter with the thumb positioned medially near the groin crease. The child's pelvis is stabilized by holding the contra lateral hip still while the opposite hand gently abducts the hip being tested while simultaneously exerting an upward force through the greater trochanter laterally. The sensation of a palpable clunk is a positive Ortolani test and represents the reduction of a dislocated hip into the acetabulum.
For Barlow's, test the pelvis is stabilized and the patient is positioned similar to the Ortolani test position. The Barlow's test detects potential posterior subluxation or dislocation by a gentle downward force in the longitudinal axis of the femur in an adducted hip. After three to six months, soft tissue contractures limit motion of the hip even if it is dislocated.14
Examination of an older child also includes careful assessment of extremities for asymmetric skin folds or leg length discrepancy in case of unilateral hip dislocation. A positive Galeazzi sign is another indicator of hip dislocation. It is elicited by laying the child supine and flexing both hips and knees. A positive sign is indicated by an inequality in the height of the knees. Limited abduction may be particularly helpful in diagnosing children with bilateral hip dislocation because the Galeazzi sign will be negative. Maximal abduction of hips should be greater than 60°.
In neglected cases, DDH may be diagnosed when children approach walking age with a limp on the affected side (positive Trendelenberg's sign) and hyperlordosis.
Ultrasonography and plain radiographs
Plain radiographs are of limited value for diagnosis in the newborn child because the femoral head and acetabulum are largely cartilaginous. Ultrasound scanning is the investigation of choice to evaluate DDH in infants younger than six months of age and is useful to diagnose more subtle forms of the disorder when clinical exam is equivocal.15 It is also the only imaging modality that enables a three-dimensional real-time image of a neonate's hip.16 This investigation is highly observer-dependent and may over diagnose dysplasia, especially in the first six weeks of life.17 Infants may be subjected to unnecessary treatment, but in many countries of the Western world, routine ultrasound screening is recommended. It is difficult to perform routine screening in developing countries due to limited resources and expertise. However, it is generally agreed that infants belonging to the high-risk group (as mentioned above) need to undergo a screening ultrasound to diagnose DDH.
As the child reaches three to six months of age, the dislocation will be evident on X-rays but the examiner must be familiar with landmarks of the immature pelvis in order to identify the abnormality. In infants, the upper femur is not ossified and most of the acetabulum is also still cartilaginous. There are several classic lines that are helpful in evaluating the immature hip.
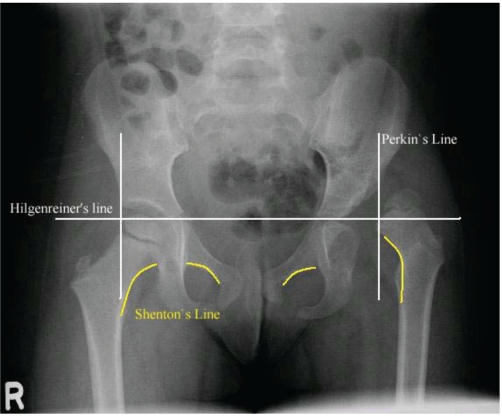
Hilgenreiner's line is a line through the tri-radiate cartilages. Perkin's line, drawn at the lateral margin of the acetabulum, is perpendicular to Hilgenreiner's line. Shenton's line is a curved line that begins at the lesser trochanter, goes up the femoral neck, and connects to a line along the inner margin of the pubis. In a normally located hip, the medial beak of the femoral metaphysis lies in the lower, inner quadrant produced by the intersection of Perkin's and Hilgenreiner's lines. Shenton's line is smooth in the normally located hip with no step off. In the dislocated hip, Shenton's line has a step off because the femoral neck lies cephalic to the line from the pubis (Figure 1).
Figure 1.
Pelvis X-Ray (AP view) showing left sided dysplastic hip with femur head lying in the upper outer quadrant and disrupted Shenton's line.
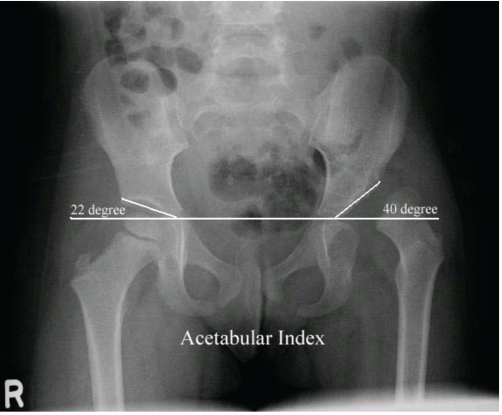
Acetabular index is another useful measurement, formed by the junction of Hilgenreiner's and a line drawn along the acetabular surface. In normal newborns, the acetabular index averages 27.5 degrees, at six months 23.5 degrees and at two years, 20 degrees. Thirty degrees is considered the upper limit of normal18,19 (Figure 2).
Figure 2.
Pelvis X-Ray (AP view) showing left sided dysplastic hip with an increased acetabular index.
In older children, center edge angle is a useful measure. It is the angle between the Perkin's line and the line joining the centr of femoral head with the lateral acetabulum. In children aged 6–13 years, an angle greater than 19 is considered normal, while in older children an angle greater than 25 is considered normal.
Magnetic resonance imaging provides excellent visualization of the infant hip.20 However, it is not routinely performed due to the need for sedation/general anesthesia to make sure the pelvis is still during the examination.
Management of developmental dysplasia of the hip
The treatment of DDH is age-related and the goal is to achieve and maintain concentric reduction of the femoral head into the acetabulum. The best outcome can be expected only if the treatment is started very early. This has been achieved in the developed world through improved awareness and training, increased surveillance (use of ultrasonography), and quicker access to pediatric orthopedic surgeons.21 It must be noted that there are very few specialized pediatric orthopedic surgeons in the developing world, and fellowship programs for pediatric orthopedic surgery should be initiated to cater for this requirement, in addition to the myriad of other pediatric orthopedic conditions.22
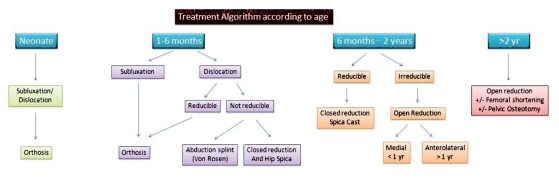
The management of this complex problem varies according to age. It is described below in detail and summarized in Figure 3.
Figure 3.
Treatment algorithm for developmental dysplasia of the hip according to different age groups.
Treatment of a neonate with developmental dysplasia of the hip
Subluxation of hip noted at birth may correct spontaneously. Some physicians may continue with observation before initiating treatment. When observation is chosen, steps should be taken to ensure close follow up because some of these hips will subsequently dislocate if left alone. The child should then be re-evaluated both clinically and by ultrasound at three weeks of age to confirm concentricity. Hips that are still dislocated need further treatment. Orthoses, such as Erlanger, Thübinger or Pavlik, which promote abduction and flexion of the hip joint can reduce unphysiological pressure to the anterolateral acetabulum and are a preferred treatment option in this age group, aiming for development of a normal lateral edge of the cartilaginous acetabulum. A dislocated hip which can be reduced and a reduced hip that can be subluxated should be treated with the orthosis. All such hips should be treated in orthosis or harness beginning at the time of diagnosis. These harnesses are very dynamic and successful tools in the treatment of DDH, although they are sometimes difficult to handle for the parents. Once properly applied, they allow motion while the hips are flexed (>90°) as well as abducted and treatment is continued until the hip is stable, as evidenced by negative Barlow and Ortolani tests. The normal degree of valgus of femoral head and neck requires this degree of flexion to promote spontaneous reduction of dislocation. Application of an orthosis should be followed by bi-weekly clinical examination, and ultrasonography if required. If the hip is reduced at three weeks following application of orthosis, the patient may continue to wear it for a further three weeks. After six weeks, the orthosis is removed and the hip is examined both clinically and by ultrasound. If the hip is reduced then the orthosis can be discontinued. The dislocated hip, even after 3–4 weeks of orthosis use, should be evaluated and may be treated with an abduction brace.23 The child needs regular follow up until skeletal maturity to identify the late sequelae, such as acetabular dysplasia.24
The hip should not be placed in a position of hyperflexion and hyperabduction as it may result in high pressure on the femoral head leading to osteonecrosis. In addition, there is evidence of an increased risk of femoral nerve palsy25 or inferior dislocation of the femoral head due to hyperflexion.26 On the other hand, inadequate flexion will fail to reduce the hip.
The Pavlik harness is contraindicated ‘when there is major muscle imbalance, as in myelomeningocele (L2 to L4 functional level); major stiffness, as in arthrogryposis, ligamentous laxity, as in Ehlers-Danlos syndrome’ or where the family situation cannot guarantee careful and consistent use of the harness.
Treatment of a child (one to six months)
Orthosis is the choice of treatment in this age group. The hip should be placed in 90 degree flexion with the proximal femur pointing towards tri-radiate cartilage. The hip which is not reducible at the time of clinical examination may still be treated with orthosis; however, higher dislocations are less likely to reduce than the lower ones.27 The position of the hip must be confirmed after application of orthosis with AP X-ray. The child should be examined at regular intervals to ensure the reduction. The orthosis should be continued for at least six weeks after the stability is achieved. If the hip fails to reduce with orthosis then other options should be considered, such as an abduction (Von Rosen) splint. The main aim of treatment is to achieve concentric reduction and to prevent avascular necrosis. Whatever method is used, it must be ensured that reduction can occur spontaneously. The hips should never be immobilized in a forced position.
Nakamura et al. reported his results of 115 patients with 130 hips. The mean age was 4.8 months and there was a mean follow up of 16 years. Patients were treated with a Pavlic harness with a mean duration of treatment of 6.1 months. Twenty-two hips required supplementary surgery for residual dysplasia, the choice of surgery depending on the state of joint and surgeon's preference. A satisfactory outcome (Severin classes I and II) was achieved in 119 patients.28
Treatment of child (six months to two years)
The child in this age group may be treated with either closed or open reduction, followed by a spica cast. The aim is to achieve reduction without damaging the femoral head. There are several studies favoring reduction of hips after the appearance of ossific nucleus.29 Segal et al. reported on 57 hips in 49 children under 12 months of age. Thirty-eight hips were reduced closed while 17 were reduced by an open method. One patient with bilateral hip dislocation was treated initially by closed means and later treated by open reduction at three months. Avascular necrosis (AVN) developed in only one of 25 patients in which a nucleus was present while 17 of 32 patients developed AVN when reduction was performed before the appearance of an ossific nucleus at a mean follow up of 59 months.30 Roposch et al. conducted a meta-analysis including 6 observational studies of a total of 358 patients with a mean age of 9.6 months at the time of reduction. Closed as well as open reduction was performed in 3 studies, open reduction alone was performed in 2 studies and closed reduction alone was performed in one study. They noted that the presence of an ossific nucleus had an insignificant effect on the development of AVN when all grades were considered. Forty-one (19%) patients developed AVN when an ossific nucleus was present as compared to 30 (22%) patients when this was absent. However, the absence of an ossific nucleus was associated with the development of osteonecrosis when grade II or more were considered; 14 (7%) patients with an ossific nucleus and 18 (16%) without an ossific nucleus.31 On the other hand, there are studies which do not confirm this. Konigsberg et al. presented his results of 40 patients in whom an open reduction through a medial approach had been performed. Average age was 7.7 months, ranging from 2.4 to 18.9 at the time of surgery, with a mean follow up of 10.3 years. Only one of 20 hips reduced before the age of six months developed AVN.32 Other investigators have reported that hips reduced after the appearance of an ossific nucleus have a higher number of operative procedures.33 In addition, due to reduced growth potential, hips reduced later will not remodel as well as those reduced earlier.
The use of pre-reduction traction is controversial. It is supported by many studies showing a decreased rate of AVN and relative success of closed reduction.34–36 On the other hand, there are studies showing a similar rate of open reduction37 and AVN in which traction was not used.38
Open reduction may be achieved through a medial or anterior approach. Minimal dissection is required in a medial approach and allows the surgeon to achieve a stable reduction without the risk of AVN.39 Disadvantages of the medial approach include inadequate exposure, risk to medial circumflex femoral vessels and inability to perform capsulorrhaphy. Post-operatively a cast is applied and changed after six weeks for a total period of three months. The anterior approach has a better visualization and allows the surgeon to perform a good capsulorrhaphy.40 The choice of approach depends upon patient age and the surgeon's experience. A medial approach is recommended for children under one year of age with a maximum age limit of 18 months in expert hands.
Treatment of older child (two years of age and older)
In older children, the femoral head lies in a more proximal location. Previously, pre-operative traction was used to bring the head into the normal position, but now femoral shortening has replaced the use of traction. Femoral shortening is usually required after the age of two years to reduce the pressure on the femoral head after reduction. This will decrease the risk of osteonecrosis.41 Sankar et al. studied the factors predicting the need for femoral shortening in 72 hips (64 patients). All patients underwent open treatment for DDH with a mean age of 35.6 months and a mean follow up of 21.4 months. He concluded that the patients over the age of 36 months and patients with vertical displacement greater than 30% of the width of pelvis were more likely to require femoral shortening.42
The aim of femoral derotation varus osteotomy is to achieve concentric reduction. Spence et al. compared two groups of patients undergoing open reduction through an anterior approach either with femoral derotation osteotomy (38 patients with 47 hips) or innominate ostetomy (33 patients with 37 hips). Mean age at reduction was 25.3 months in the first group and 21.9 months in the second group. Mean duration of follow up was 6.2 years. Acetabular remodeling and stability was better in the patients with innominate osteotomy compared to femoral derotation osteotomy.43
Adequate post-reduction coverage of the femoral head is essential. The risk of residual dysplasia at skeletal maturity increases as open reduction is performed in older children. If femoral head coverage is inadequate, then pelvic osteotomy should be considered in this age group. Salter innominate and Pemberton osteotomies are the most commonly used techniques.44 If closed or open reduction is performed in a child under 18 months of age, the child should be followed till the age of 3.5–4 years. If the femoral head coverage is still inadequate, then pelvic osteotomy should be considered. Bohm et al. studied 73 hips in 61 patients with a mean age of 4.1 years at the time of surgery. He concluded that good clinical results can be expected if normal acetabular anatomy is restored without the development of AVN. However, pelvic osteotomy should preferably be performed at a later stage than at the time of open reduction.45 Thomas et al. presented the results of 80 hips in 60 patients with a mean follow up of 43.3 years. All patients underwent open reduction, capsulorraphy and Salter innominate osteotomy at a mean age of 2.8 years. Failure was defined as the joint requiring replacement surgery. They reported a 54% survival rate with excellent prognosis in two-thirds who were able to function at a high level.46
El-Sayed et al. reported 71 surgical interventions in 55 patients (ages ranging from two to four years) in whom open reduction, Salter innominate osteotomy, and proximal femoral osteotomy were performed in a single stage. The mean follow up was five years and four months. They reported favorable clinical and radiological results. Mean pre-operative acetabular index was 41.86 while the final mean acetabular index was 16.78.47
Late presentation acetabular dysplasia
A number of patients present late in adolescence with complaints of aching pain either in the groin or lateral hip pain which increases after exertion. After detailed physical and radiographic assessment, a treatment strategy is devised for these dislocated hips. The goal of treatment is to attain concentric reduction by realignment osteotomy of the acetabulum to cover the femoral head such as Salter, Pemberton and Dega osteotomy. For hips that can not be concentrically reduced, the aim is to cover the femoral head with structures that become fibrocartilage. The Chiari osteotomy and the shelf procedure are two such approaches.48
Complications
Avascular necrosis
This results from excessive pressure on the femoral head after reduction in extreme abduction and internal rotation leading to vascular occlusion. The incidence of AVN varies widely from 0–73%49 depending on the age, mode of treatment and criteria used to describe AVN. Four percent incidence was reported by Weiner et al. in children under the age of three months.50 AVN can easily be prevented by performing femoral shortening. Change in femoral head density, failed ossification and widening of the femoral neck suggest avascular changes.51 The greater trochanter is usually preserved and continues to grow whereas the femoral epiphysis is damaged which disturbs hip biomechanics. There are a number of procedures to correct the mechanical imbalance, such as trochanteric epiphysiodesis,52 trochanteric advancement53 and a lateral closing wedge along with trochanteric advancement.
Residual dysplasia
Acetabular index measures the severity of the residual dysplasia. In current literature, the definition of acetabular dysplasia is inconsistent.54 Gwynne et al. defines dysplasia as definite if the acetabular index is more than 30 degrees at 6-month X-rays (corresponding to more than 2 SD above normal at this age) and as mild if greater than 25 degrees.55 Cashman reported a 3.5% incidence of residual acetabular dysplasia in his study.56 Acetabulum remodels in response to the pressure exerted by the femoral head after concentric reduction. However, this process may remain inefficient and results in a shallow acetabulum providing inadequate coverage and poor outcome.57 This can be treated by acetabular reorientation surgery.58
Conclusions
Developmental dysplasia of the hip is a challenging condition. Formal training in the treatment of various age groups with DDH is mandatory. Pediatricians and family physicians should have a high index of suspicion and referral to a pediatric orthopedic surgeon should be made early. The outcome of treatment during the first six months of life is much better than in late-diagnosed DDH. Successful treatment with orthoses requires careful counseling of parents. Surgical management requires careful pre-operative planning and adequate follow up to ensure the best clinical outcomes.
References
- 1.Aronsson DD, Goldberg MJ, Kling TF, et al. Developmental dysplasia of the hip. Pediatrics. 1994;94:201–8. [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics, Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip: Clinical practice guideline: Early detection of developmental dysplasia of the hip. Pediatrics. 2000;105:896–905. doi: 10.1542/peds.105.4.896. [DOI] [PubMed] [Google Scholar]
- 3.LeBel ME, Gallien R. The surgical treatment of teratologic dislocation of the hip. J Pediatr Orthop B. 2005;14:331–6. doi: 10.1097/01202412-200509000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Rosendahl K, Markestad T, Lie RT. Ultrasound screening for developmental dysplasia of the hip in the neonate: the effect on treatment rate and prevalence of late cases. Pediatrics. 1994;94:47–52. [PubMed] [Google Scholar]
- 5.Bialik V, Bialik GM, Blazer S, et al. Developmental dysplasia of the hip: a new approach to incidence. Pediatrics. 1999;103:93–9. doi: 10.1542/peds.103.1.93. [DOI] [PubMed] [Google Scholar]
- 6.Carter CO, Wilkinson JA. Genetic and environmental factors in the etiology of congenital dislocation of the hip. Clin Orthop Relat Res. 1964;33:119–28. [PubMed] [Google Scholar]
- 7.Weinstein SL. Developmental hip dysplasia and dislocation. In: Morrissy RT, Weinstein SL, editors. Lovell and Winter's pediatric orthopaedics. 5 th ed. Vol 2. Philadelphia: Lippincott Williams and Wilkins; 2001. pp. 905–56. [Google Scholar]
- 8.Wynne-Davies R. Acetabular dysplasia and familial joint laxity: Two etiological factors in congenital dislocation of the hip. A review of 589 patients and their families. J Bone Joint Surg Br. 1970;52:704–16. [PubMed] [Google Scholar]
- 9.Suzuki S, Yamamuro T. Correlation of fetal posture and congenital dislocation of the hip. Acta Orthop Scand. 1986;57:81–4. doi: 10.3109/17453678608993223. [DOI] [PubMed] [Google Scholar]
- 10.Coleman SS. Congenital dysplasia of the hip in the Navajo infant. Clin Orthop. 1968;56:179–93. [PubMed] [Google Scholar]
- 11.Schwend RM, Pratt WB, Fultz J. Untreated acetabular dysplasia of the hip in the Navajo. A 34 year case series followup. Clin Orthop. 1999;364:108–16. doi: 10.1097/00003086-199907000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Malvitz TA, Weinstein SL. Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg Am. 1994;76:1777–92. doi: 10.2106/00004623-199412000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Dezateux C, Rosendahl K. Developmental dysplasia of the hip. Lancet. 2007;369:1541–52. doi: 10.1016/S0140-6736(07)60710-7. [DOI] [PubMed] [Google Scholar]
- 14.Barlow T G. Early diagnosis and treatment of dislocation of the hip. J Bone Joint Surg Br. 1962;44:292–301. [Google Scholar]
- 15.Harding MG, Harcke HT, Bowen JR, et al. Management of dislocated hips with Pavlik harness treatment and ultrasound monitoring. J Pediatr Orthop. 1997;17:189–98. doi: 10.1097/00004694-199703000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Harcke HT, Grissom LE. Infant hip sonography: current concepts. Semin Ultrasound CT MRI. 1994;15:256–63. doi: 10.1016/s0887-2171(05)80085-x. [DOI] [PubMed] [Google Scholar]
- 17.Godward S, Dezateux C. Surgery for congenital dislocation of the hip in the UK as a measure of outcome screening. MRC Working Party on Congenital Dislocation of the Hip. Medical Research Council [Published correction appears in Lancet 1998;351:1664] Lancet. 1998;351:1149–52. doi: 10.1016/s0140-6736(97)10466-4. [DOI] [PubMed] [Google Scholar]
- 18.Hensinger RN. New York: Raven Press; 1986. Standards in Pediatric Orthopedics. [Google Scholar]
- 19.Laurenson RD. The acetabular index: a critical review. J Bone Joint Surg Br. 1959;41:702–10. [Google Scholar]
- 20.Greenhill BJ, Hugosson C, Jacobsson B, et al. Magnetic resonance imaging study of acetabular morphology in developmental dysplasia of the hip. J Pediatr Orthop. 1993;13:314–7. doi: 10.1097/01241398-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Maxwell SL, Ruiz AL, Lappin KJ, et al. Clinical screening for developmental dysplasia of the hip in Northern Ireland. BMJ. 2002;324:1031–3. doi: 10.1136/bmj.324.7344.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Umer M, Nawaz H. Developmental dysplasia of hip--where do we stand? J Pak Med Assoc. 2008;58:2–4. [PubMed] [Google Scholar]
- 23.Hedequist D, Kasser J, Emans J. Use of an abduction brace for developmental dysplasia of the hip after failure of Pavlik harness use. J Pediatr Orthop. 2003;23:175–7. [PubMed] [Google Scholar]
- 24.Tucci JJ, Kumar SJ, Guille JT, et al. Late acetabular dysplasia following early successful Pavlik harness treatment of congenital dislocation of the hip. J Pediatr Orthop. 1991;11:502–5. doi: 10.1097/01241398-199107000-00016. [DOI] [PubMed] [Google Scholar]
- 25.Mubarak S, Garfin S, Vance R, et al. Pitfalls in the use of the Pavlik harness for treatment of congenital dysplasia, subluxation, and dislocation of the hip. J Bone Joint Surg Am. 1981;63:1239–48. [PubMed] [Google Scholar]
- 26.Rombouts JJ, Kaelin A. Inferior (obturator) dislocation of the hip in neonates: A complication of treatment by the Pavlik harness. J Bone Joint Surg Br. 1992;74:708–10. doi: 10.1302/0301-620X.74B5.1527118. [DOI] [PubMed] [Google Scholar]
- 27.Grill F, Bensahel H, Canadell J. The Pavlik harness in the treatment of congenital dislocating hip: Report on a multicenter study of the European Paediatric Orthopaedic Society. J Pediatr Orthop. 1988;8:1–8. doi: 10.1097/01241398-198801000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Nakamura J, Kamegaya M, Saisu T, et al. Treatment for developmental dysplasia of the hip using the Pavlik harness: long-term results. J Bone Joint Surg Br. 2007;89:230–5. doi: 10.1302/0301-620X.89B2.18057. [DOI] [PubMed] [Google Scholar]
- 29.Carney BT, Clark D, Minter CL. Is the absence of the ossific nucleus prognostic for avascular necrosis after closed reduction of developmental dysplasia of the hip? J Surg Orthop Adv. 2004;3:24–9. [PubMed] [Google Scholar]
- 30.Segal LS, Boal DK, Borthwick L, et al. Avascular necrosis following treatment of DDH: The protective influence of the ossific nucleus. J Pediatr Orthop. 1999;19:177–84. doi: 10.1097/00004694-199903000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Roposch A, Stöhr KK, Dobson M. The effect of the femoral head ossific nucleus in the treatment of developmental dysplasia of the hip. A meta-analysis. J Bone Joint Surg Am. 2009;91:911–8. doi: 10.2106/JBJS.H.00096. [DOI] [PubMed] [Google Scholar]
- 32.Konigsberg DE, Karol LA, Colby S, et al. Results of medial open reduction of the hip in infants with developmental dislocation of the hip. J Pediatr Orthop. 2003;23:1–9. [PubMed] [Google Scholar]
- 33.Luhmann SJ, Bassett GS, Gordon JE. Reduction of a dislocation of the hip due to developmental dysplasia: Implications for the need for future surgery. J Bone Joint Surg Am. 2003;85:239–43. doi: 10.2106/00004623-200302000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Gage JR, Winter RB. Avascular necrosis of the capital femoral epiphysis as a complication of closed reduction of congenital dislocation of the hip: A critical review of twenty years' experience at Gillette Children's Hospital. J Bone Joint Surg Am. 1972;54:373–88. [PubMed] [Google Scholar]
- 35.DeRosa GP, Feller N. Treatment of congenital dislocation of the hip: Management before walking age. Clin Orthop Relat Res. 1987;225:77–85. [PubMed] [Google Scholar]
- 36.Tavares JO, Gottwald DH, Rochelle JR. Guided abduction traction in the treatment of congenital hip dislocation. J Pediatr Orthop. 1994;14:643–9. doi: 10.1097/01241398-199409000-00018. [DOI] [PubMed] [Google Scholar]
- 37.Quinn RH, Renshaw TS, DeLuca PA. Preliminary traction in the treatment of developmental dislocation of the hip. J Pediatr Orthop. 1994;14:636–42. doi: 10.1097/01241398-199409000-00017. [DOI] [PubMed] [Google Scholar]
- 38.Weinstein SL. Traction in developmental dislocation of the hip: Is its use justified? Clin Orthop Relat Res. 1997;338:79–85. doi: 10.1097/00003086-199705000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Weinstein S. Closed versus open reduction of congenital hip dislocation in patients under 2 years of age. Orthopedics. 1990;12:221–7. doi: 10.3928/0147-7447-19900201-14. [DOI] [PubMed] [Google Scholar]
- 40.Dhar S, Taylor JF, Jones WA. Early open reduction for congenital dislocation of the hip. J Bone Joint Surg Br. 1990;72:175–80. doi: 10.1302/0301-620X.72B2.2312552. [DOI] [PubMed] [Google Scholar]
- 41.Schoenecker PL, Strecker WB. Congenital dislocation of the hip in children: Comparison of the effects of femoral shortening and of skeletal traction in treatment. J Bone Joint Surg Am. 1984;66:21–7. [PubMed] [Google Scholar]
- 42.Sankar WN, Tang EY, Moseley CF. Predictors of the need for femoral shortening osteotomy during open treatment of developmental dislocation of the hip. J Pediatr Orthop. 2009;29:868–71. doi: 10.1097/BPO.0b013e3181c29cb2. [DOI] [PubMed] [Google Scholar]
- 43.Spence G, Hocking R, Wedge JH, et al. Effect of innominate and femoral varus derotation osteotomy on acetabular development in developmental dysplasia of the hip. J Bone Joint Surg Am. 2009;91:2622–36. doi: 10.2106/JBJS.H.01392. [DOI] [PubMed] [Google Scholar]
- 44.Wenger DR. Congenital hip dislocation: Techniques for primary open reduction including femoral shortening. Instr Course Lect. 1989;38:343–54. [PubMed] [Google Scholar]
- 45.Bohm P, Brzuske A. Salter innominate osteotomy for the treatment of developmental dysplasia of the hip in children. Results of seventy three consecutive osteotomies after twenty-six to thirty-five years of follow-up. J Bone Joint Surg. 2002;84A:178–86. [PubMed] [Google Scholar]
- 46.Thomas SR, Wedge JH, Salter RB. Outcome at forty-five years after open reduction and innominate osteotomy for late-presenting developmental dislocation of the hip. J Bone Joint Surg Am. 2007;89:2341–50. doi: 10.2106/JBJS.F.00857. [DOI] [PubMed] [Google Scholar]
- 47.El-Sayed MM. Single-stage open reduction, Salter innominate osteotomy, and proximal femoral osteotomy for the management of developmental dysplasia of the hip in children between the ages of 2 and 4 years. J Pediatr Orthop B. 2009;18:188–96. doi: 10.1097/BPB.0b013e32832bf618. [DOI] [PubMed] [Google Scholar]
- 48.Staheli LT, Chew DE. Slotted acetabular augmentation in childhood and adolescence. J Pediatr Orthop. 1992;12:569–80. [PubMed] [Google Scholar]
- 49.Keret D, MacEwen GD. Growth disturbance of the proximal part of the femur after treatment for congenital dislocationof the hip. J Bone Joint Surg Am. 1991;73:410. [PubMed] [Google Scholar]
- 50.Weiner DS, Hoyt WA, Jr, O'Dell HW. Congenital dislocation of the hip: the relationship of premanipulative traction and age to avascular necrosis of the femoral head. J Bone Joint Surg Am. 1977;59:306–11. [PubMed] [Google Scholar]
- 51.Salter RB, Kostuik J, Dallas S. Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: A clinical and experimental investigation. Can J Surg. 1969;12:44–61. [PubMed] [Google Scholar]
- 52.Iversen LJ, Kalen V, Eberle C. Relative trochanteric overgrowth after ischemic necrosis in congenital dislocation of the hip. J Pediatr Orthop. 1989;9:381–5. [PubMed] [Google Scholar]
- 53.Macnicol MF, Makris D. Distal transfer of the greater trochanter. J Bone Joint Surg Br. 1991;73:838–41. doi: 10.1302/0301-620X.73B5.1894678. [DOI] [PubMed] [Google Scholar]
- 54.Dornacher D, Cakir B, Reichel H, et al. Early radiological outcome of ultrasound monitoring in infants with developmental dysplasia of the hips. J Pediatr Orthop B. 2010;19:27–31. doi: 10.1097/BPB.0b013e328330335e. [DOI] [PubMed] [Google Scholar]
- 55.Gwynne Jones DP, Vane AGS, Coulter G, et al. Ultrasound measurements in the management of unstable hips treated with the Pavlik harness. J Pedatr Orthop. 2006;26:818–22. doi: 10.1097/01.bpo.0000234999.61595.ec. [DOI] [PubMed] [Google Scholar]
- 56.Cashman JP, Round J, Taylor G, et al. The natural history of developmental dysplasia of the hip after early supervised treatment in the Pavlik harness. J Bone Joint Surg Br. 2002;84:418–25. doi: 10.1302/0301-620x.84b3.12230. [DOI] [PubMed] [Google Scholar]
- 57.Albiñana J, Morcuende JA, Weinstein SL. The teardrop in congenital dislocation of the hip diagnosed late: a quantitative study. J Bone Joint Surg Am. 1996;78:1048–55. doi: 10.2106/00004623-199607000-00009. [DOI] [PubMed] [Google Scholar]
- 58.Kim HT, Kim JI, Yoo CI. Acetabular development after closed reduction of developmental dislocation of the hip. J Pediatr Orthop. 2000;20:701–8. doi: 10.1097/00004694-200011000-00002. [DOI] [PubMed] [Google Scholar]