Abstract
In developing countries, due to limited availability of modern anesthesia and overcrowding of the hospitals with patients who need surgery, high-risk patients with “intertrochanteric” fractures remain unsuita ble for open reduction and internal fixation.
The aim of this study was to analyze the results of external fixation of “intertrochanteric” fractures in high-risk geriatric patients in a developing country.
The results of 62 ambulatory high-risk geriatric patients with a mean age of 70 years (range 58–90 years) with “intertrochanteric” fractures, in whom external fixation was performed, are reported.
Eight patients died during follow-up due to medical causes unrelated to the surgical procedure. So only 54 patients were available for final assessment. Procedure is simple, performed under local anesthesia, requires less time for surgery and is associated with less blood loss. Good fixation and early ambulation was achieved in most of the patients. Average time to union was 14 weeks. Thirty-one patients developed superficial pin tract infection and 28 patients had average shortening of 15 mm due to impaction and varus angulation. Functional outcome was assessed using Judet's point system. Good to excellent results were achieved in 44 patients.
This study demonstrated that external fixation of “intertrochantric” fractures performed under local anesthesia offers significant advantage in ambulatory high-risk geriatric patients especially in a developing country.
Introduction
The increase in average life expectancy has led to a dramatic increase in incidence of fracture of the proximal part of the femur. The patients with this type of fracture occupy 30% of beds in the orthopedic hospitals.1 “Intertrochanteric” fractures constitute the majority among these fractures. In developing countries, due to limited availability of modern anesthesia and overcrowding of the hospitals with patients who need surgery, high-risk patients with “intertrochanteric” fractures remain unsuitable for open reduction and internal fixation. Due to the dangers associated with prolonged recumbency, the role of conservative treatment (for example traction) is negligible except in terminally ill or non-ambulatory patients.2
Goal of treatment remains restoration of patient to his / her pre-operative status as early as possible with low morbidity and mortality. External fixation, performed under sedation and local anesthesia, offers significant advantages in high-risk geriatric patients in the form of minimal blood loss, minimal surgical trauma, preservation of fracture hematoma, a shorter hospital stay, early ambulation of patients as compared to patients treated conservatively, and removal of implant as easy outpatient procedure.3,4
The aim of our study was to analyze the role and effectiveness of this simple minimally invasive procedure in high-risk geriatric patients in a developing country where many patients with intertrochantric fractures remain high-risk with conventional anesthesia.
Materials and Methods
Sixty-two high-risk geriatric patients (ASA Grade II and III) with a mean age of 70 years (range 58–90 years) were included in the study. Patients with unstable fractures, multiple fractures, osteoporosis (Singh's index <Grade 4), or with bone and joint disease that could interfere with rehabilitation were excluded from the study.
Patients who presented after one week were also excluded. Patient data is shown in Table 1.
Table 1. Patient data.
| Total number of patients | 62 |
| ASA Grade | Grade II9 |
| Grade III53 | |
| Male: female ratio | 1:1.58 |
| Number of patients dying during follow-up | 8 (3 female and 5 males) |
| Number of patients available for final follow-up | 54 |
| Age (mean) | 70 years |
| Age distribution | 58–65: 15 |
| 66–75: 33 | |
| 76–85: 10 | |
| 86–90: 04 | |
| Right: left ratio | 1:1.85 |
| Mode of injury | Fall while walking34 |
| Fall from height11 | |
| Road traffic accidents7 | |
| Miscellaneous9 | |
| Injury to surgery interval (mean) | 3 days (range 1–5 days) |
Patients received sedation with local anesthesia (1% lidocaine used for skin and periostium). Fracture was reduced under image intensifier using a fracture table. Two 4.5 mm cancellous Schanz Screws were passed across the fracture site percutaneously along the axis of the neck of femur at an angle of 130° (approximately) with the shaft using a hand drill. Both pins were parallel in AP view and central in lateral view. The superior pin was passed just above the center of the neck and head, and the inferior pin was passed along the inferior part of the neck and head. Pins were advanced to a point 5 mm short of the subchondral bone of the head. Once the fracture site was stabilized by “trochanteric” pins, the knee was flexed to 90° and traction was shifted from the foot piece to the upper tibial pin (which was inserted on the day of admission). Three 4.5 mm cortical Schanz Screws were introduced at a right angle to the shaft of femur as close to the fracture site as possible. The intra-operative time was measured from the time the incision for the insertion of first pin was made to when the fixator was completely mounted. Blood loss was estimated by comparing the weight of the wet and dry swab.
After surgery, patients were assisted in sitting, knee bending and quadriceps exercise from the second day of surgery. Patients were allowed non-weight bearing crutch walking with only toe touching for the first six weeks. After which patients were allowed partial weight bearing for the next four weeks as per pain tolerance, and full weight bearing was allowed after adequate clinical and radiological signs of fracture union were seen. Appropriate physiotherapy was advised for hip and knee motion. Pin sites were dressed daily with saline and the families of the patients were given instructions for continuing care after discharge. The fixator was removed at 16 weeks without anesthesia in the outpatient clinic. All patients were reviewed at six weeks, 12 weeks, 18 weeks, 24 weeks and one year. Observation regarding shortening, malunion, varus angulation, pain at the hip and knee, range of motion of the hip and knee, and evidence of infection and union were recorded. The functional results were graded using Judet's point system5 (Table 2A and B). The final follow-up was at 12 months.
Table 2A. Judet's point system for grading disability.
| Pain | Range of motion | Ability to walk | |||
|---|---|---|---|---|---|
| Observation | Grade | Observation (Degrees) | Grade | Observation | Grade |
| Severe pain at rest | 1 | 0 (limb in poor position) | 1 | Bedridden | 1 |
| Severe pain on walking | 2 | 0 (limb in good position) | 2 | Walking very limited with or without a cane | 2 |
| Pain tolerable | 3 | 0–70 | 3 | Walking limited with one cane | 3 |
| Pain with fatigue | 4 | 70–140 | 4 | Long distances with one cane | 4 |
| Slight pain | 5 | 140–200 | 5 | No cane but limp | 5 |
| No pain | 6 | 20–300 | 6 | Normal | 6 |
Table 2B. Judet's terminology for ratings.
| Summation of Judet's point* | Rating |
| 8 or less | Bad |
| 9–11 | Fair |
| 12–15 | Good |
| 16 or more | Excellent |
For pain, range of motion, and ability to walk. Reprinted with permission from the Journal of Bone and Joint Surgery, Inc.
Results
A summery of results is given in Table 3.
Table 3. Results.
| Patients available for final assessment | 54 (35 females,19 males) |
| Hospital stay (mean) | 3 days (range 2–5 days) |
| Surgery time (mean) | 30 minutes (range 25–40 minutes) |
| Blood loss | 20–30 mL |
| Time to union (mean) | 14 weeks |
| Pain scale at final follow-up | No pain34 |
| Slight pain10 | |
| Pain with fatigue6 | |
| Pain tolerable4 | |
| Pain scale (mean) at final follow-up | 5.3 |
| Range of motion (mean) at final follow-up | 230(range 100–300) |
| Walking ability at final follow-up | Normal26 |
| No cane but limp8 | |
| Long distance with one cane10 | |
| Walking limited with a cane6 | |
| Walking very limited with or without a cane4 | |
| Final results | Excellent20 |
| Good24 | |
| Fair6 | |
| Poor4 | |
| Complications | |
| Varus angulation | 24 |
| Shortening | 28 (mean 15 mm, range 10–35 mm) |
| Pin track infection(Superficial) | 31 |
A total of 62 patients were treated using an external fixator. There were 38 females and 24 males. Eight patients died (3 females and 5 males) during follow-up. So only 54 patients (35 females and 19 males) were available for final assessment.
The average age in our series was 70 years. Hospital stay was short averaging three days (range 2–5 days).
A small frame, which did not interfere with sitting, lying or walking in conventional clothes, was used.
The procedure needed simple anesthesia and less time for surgery (25–40 min, average 30 min). Blood loss was minimal (20–30 mL). Patients started early ambulation with support. The average time to union was 14 weeks. There was no case of pin breaking and penetration of femoral head.
Twenty-eight patients had on average a limb shortening of 15 mm (10–35 mm). Shortening resulted from impaction and varus angulation. Among 24 patients who developed varus angulation, 16 developed 10°, 5 developed 20° and 3 developed 30° angulation approximately.
Thirty-one patients developed superficial pin tract infection usually involving the proximal pins. Infection was successfully treated with daily cleansing using normal saline and betadine plugs.
Initial knee stiffness was noticed in 36 cases. In these cases, while the fixator was in place, the range of knee motion was 40–70° and stiffness presented for a variable period of time. At the time of final follow-up, the average range of motion around the knee was 110°. Hip range of motion was initially less but it increased over a period of time. Most patients had gained good range of motion at hip and knee at the final assessment.
Varus angulation was seen in 24 patients.
The functional results were graded using Judet's point system.5 There were 20 excellent, 24 good, 6 fair results and 4 poor results.
Discussion
Longer life span has been accompanied by an increase in the incidence of “pertrochantric” fractures which mainly occur in the elderly.6 These elderly patients present a host of medical conditions which is associated with a high ratio of mortality and morbidity if open reduction and internal fixation is contemplated in a developing country where modern anesthesia is lacking in the majority of the hospitals which are overcrowded with patients who need surgery. Similarly conservative methods are associated with complications like thromboembolism, bed sores, pneumonia, etc. because of prolonged recumbency.
The need to reduce the risk of fracture fixation, permit early mobilization and reduce hospital stay, has prompted several orthopedic surgeons to propose external fixation as an alternative treatment option for these elderly high-risk patients.7–9 Studies using an external fixator for fixation of “trochanteric” fractures have shown better functional results, have shortened operative time, and resulted in less blood loss, less pain and a shorter hospital stay.10,11
Our study shows that an external fixator can be applied under local anesthesia with sedation and is appropriate for high-risk patients. External fixation is superior with regard to delay in surgery, especially in a developing country, the duration of surgery, blood loss and hospital stay. These advantages are of significant importance given the co-morbidity associated with these fractures.8
Varus angulation was seen in 24 of 54 patients which led to shortening. This is more than reported by Morine et al.12 who used hydroxyappetite coated pins. Though this seems to be suboptimal, considering the age of the patients it is acceptable, and our main aim of returning these patients to early ambulation was served.
Knee stiffness is probably the result of transfixing the vastus lateralis muscle4 but it was temporary in nearly all cases, recovering to near normal after removing the pin. The incidence of knee stiffness was less in our study, possibly due to more proximal placement of femoral shaft Schanz pins and flexion of the knee before this was performed.
The range of motion of hip was initially less but at the final follow-up all patients had good range of motion.
Pin tract infection has been reported to be the most common complication.2,8 Pin tract infection was seen in 31 patients but this was reduced in most patients with regular saline washes, antiseptic dressing, and finally with the removal of pins at 16 weeks.
Union is not a problem, as “intertrochanteric” fractures are through vascular cancellous bone. Functional outcome at one year in most of our patients was good to excellent, as was seen in various other studies.
Conclusions
The study has shown that external fixation is minimally invasive and can be performed under local anesthesia. This procedure causes less blood loss, requires short operative time, requires a shorter hospital stay, and complications associated with prolonged recumbency and open reduction and internal fixation are avoided. In a developing country where modern anesthesia is limited and hospitals are usually overcrowded with patients who need surgery, external fixation of “intertrochanteric” fractures is a viable option in high-risk geriatric patients given the morbidity and mortality associated with open reduction and internal fixation and prolonged recumbency.
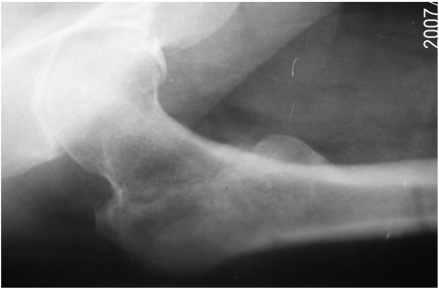
Figure 1.
Pre operative radoigraph.
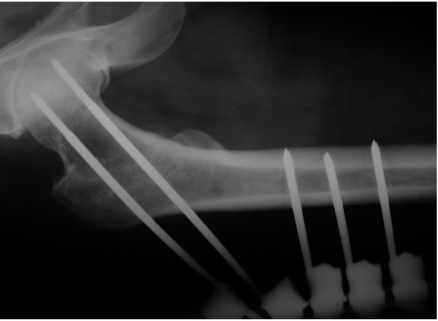
Figure 2.
Immediate post operative radiograph.
Figure 3.
Radiograph at 14 weeks.
Figure 4.
Radiograph after removal of the fixator.
References
- 1.Zetterberg C, Anderson BJ. Fractures of the proximal end of the femur in Goteborg, Sweden. Acta Orthop Scand. 1982;53:419–26. doi: 10.3109/17453678208992236. [DOI] [PubMed] [Google Scholar]
- 2.Aufrane OE, Jones WN, Truner RH. Severely communited intertrochanteric hip fractures. JAMA. 1967;199:140–3. doi: 10.1001/jama.199.13.140. [DOI] [PubMed] [Google Scholar]
- 3.Gotfreed Y. Intertrochanteric fractures in high risk geriatric patients treated by external fixation. Clin Orthop. 1985;6:769–74. doi: 10.3928/0147-7447-19850601-13. [DOI] [PubMed] [Google Scholar]
- 4.Dhal A, Varghese M, Bhasin VB. External fixation of intertrochanteric fractures in high risk geriatric fractures of the femur. J Bone Joint Surg. 1991;73-B:955–8. doi: 10.1302/0301-620X.73B6.1955444. [DOI] [PubMed] [Google Scholar]
- 5.Stinchfield FE, Cooperman B, Shea CE. Replacement of the femoral head by Judet or Austin Moore prosthesis. J Bone Joint Surg. 1957;39A:1043–58. [PubMed] [Google Scholar]
- 6.Sernbo I, Johnel O, Gentz CF, Nilson JA. Unstable intertrochanteric fractures of the hip treatment with ender pins compared with a compression hip screw. J Bone Joint Surg. 1988;70:1297–303. [PubMed] [Google Scholar]
- 7.Barros JW, Ferreira CD, Freitas AA, Farah S. External fixation in intertrochanteric fractures of the femur. Int Orthop. 1995;19:217–9. doi: 10.1007/BF00185225. [DOI] [PubMed] [Google Scholar]
- 8.Karn NK, Singh GK, Kumar P, Shresthea BP, et al. Comparison between external fixation and sliding hip screw in the management of trochanteric fractures of the femur in Nepal. J Bone Surg. 2006;88-B:1347–50. doi: 10.1302/0301-620X.88B10.18023. [DOI] [PubMed] [Google Scholar]
- 9.Devgon A, Sangwan SS. External fixator in the management of trochanteric fractures in high risk geriatric patients: a friend to the elderly. Indian J Med Sci. 2002;56:388–9. [PubMed] [Google Scholar]
- 10.Voninakis IC, Badras LS. The external fixator compared with the sliding hip screw for petrochanteric fractures of the femur. J Bone Joint Surg. 2002;64-B:23–9. doi: 10.1302/0301-620x.84b1.12034. [DOI] [PubMed] [Google Scholar]
- 11.Vossinakis IC, Badras LS. Management of pertrochanteric fractures in high risk patients with an external fixation. Int Orthop. 2001;25:219–22. doi: 10.1007/s002640100238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moroni A, Fadini C, Pegraffi FM, et al. Dynamic hip screw compared with external fixation treatment of osteoporotic pertrochanteric fractures: A prospective, randomized study. J Bone Joint Surg. 2005;87-A:753–9. doi: 10.2106/JBJS.D.01789. [DOI] [PubMed] [Google Scholar]