Abstract
The IADR Global Oral Health Inequalities Task Group on Dental Caries has synthesized current evidence and opinion to identify a five-year implementation and research agenda which should lead to improvements in global oral health, with particular reference to the implementation of current best evidence as well as integrated action to reduce caries and health inequalities between and within countries. The Group determined that research should: integrate health and oral health wherever possible, using common risk factors; be able to respond to and influence international developments in health, healthcare, and health payment systems as well as dental prevention and materials; and exploit the potential for novel funding partnerships with industry and foundations. More effective communication between and among the basic science, clinical science, and health promotion/public health research communities is needed. Translation of research into policy and practice should be a priority for all. Both community and individual interventions need tailoring to achieve a more equal and person-centered preventive focus and reduce any social gradient in health. Recommendations are made for both clinical and public health implementation of existing research and for caries-related research agendas in clinical science, health promotion/public health, and basic science.
Keywords: Dental caries, health inequalities, health disparities, implementation research, translational research
Introduction
The members of the Dental Caries Task Group of the Global Oral Health Inequalities Research Initiative were identified on the basis of their global involvement in cariology research and the implementation of research findings, as well as for their expertise in caries research areas from basic to clinical science and health services research, in evidence-based dentistry, epidemiology, dental public health, and health promotion.
The remit of this Task Group was to review the field to identify:
global inequalities in dental caries, taking into account inequalities within as well as between countries;
likely reasons to account for these oral health inequalities;
fundamental gaps in knowledge and understanding;
reasons for failure to implement at scale measures which have been shown to be effective in clinical or laboratory studies;
priorities for both basic and applied research; and
a five-year research agenda, which will lead to key improvements in global oral health, with particular reference to inequalities between and within countries.
The Task Group has examined implementation gaps and articulated a research agenda to address inequalities in caries experience and the implementation of effective caries prevention strategies in a coherent way, related to the Global (Oral) Health Promotion Agenda already being pursued by WHO and others.
Initial Deliberations
The Caries Task Group began by reviewing the IADR President’s Address to the Miami General Session (Williams, 2009) and the evidence and future research directions synthesized in a 2007 Lancet review paper on dental caries (Selwitz et al., 2007). The Task Group endorsed the principles outlined by the World Health Organization (WHO) at the World Health Assembly (Petersen, 2008), where “the Member States agreed on an action plan for oral health and integrated disease prevention.” The key points included urging member states to consider mechanisms to provide coverage of the population with essential oral health care, to incorporate oral health into the framework of enhanced primary health care for chronic noncommunicable diseases, and to promote the availability of oral health services that should be directed toward disease prevention and health promotion for poor and disadvantaged populations, in collaboration with integrated programs for the prevention of chronic non-communicable diseases. Other recommendations were for those countries without access to optimal levels of fluoride, and which have not yet established systematic fluoridation programs, to consider the development and implementation of fluoridation programs, to incorporate an oral health information system into health surveillance plans so that oral health objectives are in keeping with international standards, to evaluate progress in promoting oral health, to strengthen oral health research and use evidence-based oral health promotion and disease prevention to consolidate and adapt oral health programs, to encourage the intercountry exchange of reliable knowledge and experience of community oral health programs, and to increase, as appropriate, the budgetary provisions dedicated to the prevention and control of oral and craniofacial diseases and conditions.
The Task Group also drew on the recently published report of the International Conference on Novel Anti-Caries and Remineralizing Agents (ICNARA, 2009). This international conference recognized the strong evidence for the effectiveness of fluoride in caries prevention, and evaluated the evidence and potential of other novel anti-caries and remineralizing agents for caries prevention and repair, with the objective of developing an agreed multidisciplinary research agenda for the next decade.
Links between and among the IADR, WHO, and the FDI World Dental Federation have been very important in implementing research findings, as have links with the International Caries and Detection System (ICDAS) Foundation. This charitable foundation has developed “an evidence-based clinical caries scoring system for use in dental education, clinical practice, research, and epidemiology designed to “lead to better quality information to inform decisions about appropriate diagnosis, prognosis, and clinical management at both the individual and public health levels” (ICDAS, 2010a). Key joint work of relevance carried out for this initiative in partnership by Group members is detailed further in the Appendix.
Findings of the Task Group
Global Inequalities in Oral Health and Dental Caries, Taking into Account Inequalities within as Well as between Countries
There are marked differences in caries-related health inequalities in developing as well as developed countries, and both must be addressed. It is also evident that there is a gradient in caries levels between the least- and most-well-developed countries. The situation is further complicated by the fact that some countries are in rapid transition. While there are very significant differences in all aspects of dental care between such countries, the fundamental clinical options and the science supporting caries prevention and control are universal. For these reasons, we have taken an international approach and stated that all solutions should be appropriate for the particular characteristics, cultures, and behaviors of the end user location.
The scale and enduring nature of the caries inequalities in both developing and developed countries are well-established. WHO Reports and the global policy for improvement of oral health adopted by the World Health Assembly in 2007 (Petersen, 2008) state that:
Oral disease is still a major public health problem in high-income countries, and the burden of oral disease is growing in many low- and middle-income countries.
Oral disease, such as dental caries. . . ., is a serious public-health problem. Its impact on individuals and communities in terms of pain and suffering, impairment of function, and reduced quality of life is considerable. Globally, the greatest burden of oral diseases lies on disadvantaged and poor populations. The current pattern of oral disease reflects distinct risk profiles across countries related to living conditions, behavioral and environmental factors, oral health systems, and implementation of schemes to prevent oral disease.
In several high-income countries with preventive oral care programs, the prevalence of both dental caries in children and tooth loss among adults has fallen. Globally, the burden of oral disease is particularly high among older people and has a negative effect on their quality of life. In most low- and middle-income countries, the general population does not benefit from systematic oral health care, and preventive programs have not been established. In some countries, the incidence of dental caries has increased over recent years and may further increase as a result of the growing consumption of sugars and inadequate exposure to fluorides.
Social inequality in oral health status and the use of services is somewhat universal. Even in the Nordic countries, with public responsibility in financing and delivery of oral health care, remarkable differences are observed by social class.
Surprisingly, despite recent efforts to make the most of available data from WHO and elsewhere—such as in the FDI World Dental Federation “Oral Health Atlas” (FDI, 2009)—the quality, coverage, and utility of much of the information available for caries status and inequalities are poor. Reasons for this include variable methodological and quality standards, and dependence on the assessment of dentin cavitation to estimate the need for restorative care. Research findings are out of date, and there is an absence of reliable, recent data from many countries and regions that cover the disease severity continuum. The need for timely information relates to both the severe end of the spectrum, with regard to pain, sepsis, and urgent needs, and the opposite end of this spectrum, where reliable information is lacking on the prevalence and pattern of initial caries amenable to preventive and nonsurgical interventions. It may safely be concluded, however, that there are profound inequalities in caries status, both between and within countries, and that the distribution of disease in a population is a changing dynamic.
Likely Reasons to Account for These Oral Health Inequalities
A wide range of factors has been implicated in caries initiation and progression (see Fig. 1), but these are dominated by the social determinants of health. The “personal” and social factors in the outer circle, particularly income, education, and behaviors, have been shown to have profound effects. Other macro-level factors include access to and use of fluorides, diet, and access to preventive and restorative care services. However, it is also important to understand the research evidence in all parts of the diagram, since the oral environmental factors have a major impact on the core factors that are required for the initiation or progression of caries. There are also suggestions that one of the major barriers to achieving equitable improvements in caries prevention and control has been the lack of effective communication among dental stakeholders about the cariology evidence which has developed over the last decades.
Fig. 1.
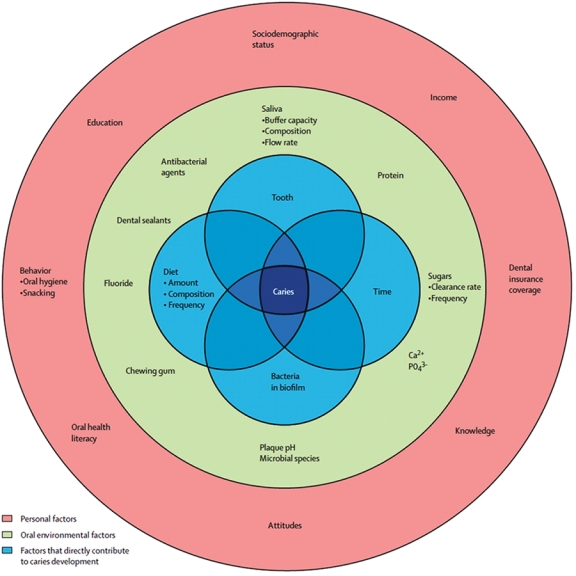
Illustration of the factors involved in caries development and progression; reproduced with permission from Selwitz et al., 2007.
Despite good evidence about methods for delivering effective clinical prevention and caries control, the existence of implementation gaps has meant that health systems have been slow to move away from the traditional restorative approach to caries management, which is linked directly to access to dentists providing surgically based interventions beyond the economic reach of many. WHO recommends the building of capacity in oral-health systems oriented to disease prevention and primary health care, with special emphasis on meeting the needs of disadvantaged and poor populations (Petersen, 2008).
Fundamental Gaps in Knowledge and Understanding
Basic Cariology Sciences
The key basic science knowledge gaps that need to be addressed in terms of understanding the caries process include the delivery of more effective remineralization, and the dynamics of the biofilm, with the potential this has to develop novel antibacterial approaches.
Remineralization is the natural repair process for caries lesions. While the existence of this process has been known for at least a hundred years, it is only in recent decades that the therapeutic importance of remineralization has been appreciated. Fluoride delivered topically in various vehicles has produced major reductions in the prevalence and incidence of dental caries, in part through its role in remineralization. However, when the bacterial challenge is high or the salivary components are lacking, the ensuing remineralization is insufficient to arrest or reverse the caries process. Consequently, there is a need to discover how to enhance remineralization and to transfer such knowledge into clinical therapy (Featherstone, 2009).
Although the use of fluoride schemes has been successful, the discovery of effective antimicrobial therapies would increase the range of caries-preventive products and make prevention less dependent on fluoride. Because caries is caused by bacterial metabolites, reducing the quantity and pathogenicity of dental plaque could work synergistically with fluoride. New paradigms of caries etiology focus on ecological factors and complex microflora, rather than on the traditional caries pathogens. This is because of appreciation of the fact that dental plaque has the properties of a biofilm, with bacteria growing on a surface and embedded in a polysaccharide matrix. This has opened promising new approaches for study of the etiology of dental caries. Furthermore, findings on other environmental biofilms and approaches to their reduction might be applicable to the development of oral biofilm remedies. There is optimism that the study of antimicrobials from this perspective could lead to the development of more effective caries-preventive agents (ten Cate, 2009).
Gaps in Clinical Knowledge and Understanding
The issues in this domain center on the failure in many countries to move away from the restorative-oriented approach to treatment planning and caries management. These have generally been based on the flawed assumption that the disease could be “treated away” with dental amalgam (Elderton, 1990; Pitts, 2004) or other imperfect substitutes for tooth tissue, without modifying either etiological factors or patient behaviors. The difficulty in achieving a paradigm shift has been frustrated by organizational and economic system influences, with the result that little real progress has been made in many developed countries since the 1970s. Furthermore, this approach is not only ineffective, but is also completely unaffordable and inappropriate in many developing countries.
Dental Public Health: Implementation Gaps in Knowledge and Understanding
Despite advocacy over a long period for the common risk factor approach to the management of caries, the integration of oral health promotion into health promotion strategies, and emphasis on the importance of oral health to systemic well-being (Petersen, 2008), there remains a disappointing focus on separate, dedicated, dental health education. It is not surprising that this approach has had limited impact. It appears, in some countries, that traditional dental public health advocates have had limited opportunity to update their knowledge or to gain an understanding of the potential synergies between aligned public health and clinical preventive strategies.
A further knowledge gap relates to understanding the impact of the different caries detection levels legitimately used when caries assessments are made for different purposes. Traditionally, there has been an assumption that there must be a single index or method for collecting caries information, but it is now appreciated that a “one size fits all” approach is inappropriate. Debates during the development of the European Oral Health Indicators Project (Bourgeois et al., 2008), around the use of ICDAS assessments in epidemiology and public health (Pitts, 2009) and in setting up the current FDI Global Caries initiative, have all underscored the importance of having available a caries measurement method appropriate to the task at hand. Fig. 2 shows the ICDAS adaptation of the WHO “Stepwise” approach to Surveillance of Non-Communicable Diseases for use with oral health indicators and caries surveillance employed in these initiatives. This approach gives a choice of measures with different levels of detail and complexity, appropriate to the task at hand and the resources available.
Fig. 2.
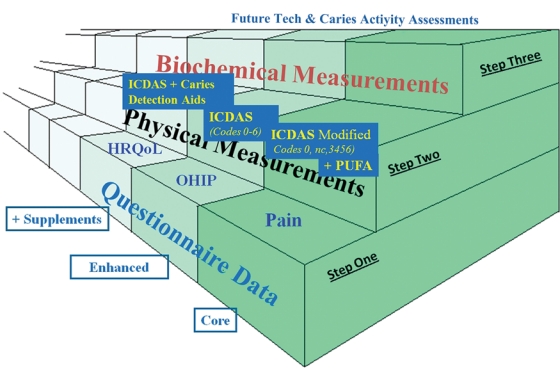
ICDAS adaptation of the WHO “Stepwise” approach to the Surveillance of Non-Communicable Diseases for use with dental caries and oral health indicators. Reproduced with permission of S. Karger AG, Basel (Pitts, 2009).
Fig. 3.
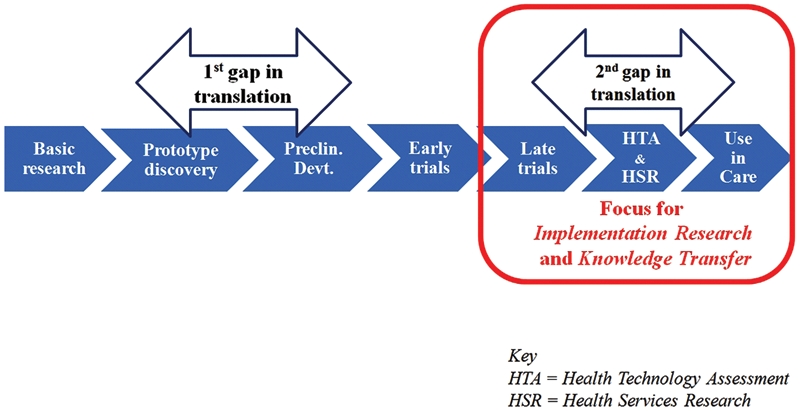
The two implementation gaps which thwart the translation of health research into practice.
Reasons for Failure to Implement at Scale Measures That Have Been Shown to Be Effective in Clinical or Laboratory Studies
The failure to implement promising research findings is not unique to the management of dental caries, but is common across the health sciences. There is increasing concern about research findings not making a difference, not improving health, and failing to have a positive impact on reducing caries and inequalities in oral health. This is not a new concern, but it is a persisting one, thrown into sharper focus in an era of more stringent financial constraints.
Over the past decade, medical scientists and public health policymakers in the US have been increasingly concerned that the scientific discoveries of the past generation are not translated efficiently into tangible clinical benefit. This concern was addressed in June 2000 by the Clinical Research Roundtable at the Institute of Medicine, one outcome of which was the identification of two translational blocks. The first of these was the translation of basic science discoveries into human clinical studies; the second was the translation of new findings into clinical practice and health decision-making in systems of care (Sung et al., 2003). Similar concerns have also been raised in the United Kingdom by the Cooksey Report (Cooksey, 2006), which recognized the same two translation gaps. The previously rarely acknowledged second gap, between the end stage of clinical trials and appropriate adoption in routine care, has now been prioritized as the focus for implementation research to understand the best way to achieve knowledge transfer.
Translation of Basic Science Research – the First Implementation Gap
Past failures to translate the findings from basic science research into practice are in large measure the result of poor communication between basic and clinical sciences and the lack of a systematic route for the translation of research findings into clinical or public health practice. The failure to develop a systematic approach to the integration of basic science and clinical research to achieve improvements in oral health outcomes, and particularly to reduce health inequalities, has been a major obstacle to progress. A further issue has been that research into caries has also been accorded a low priority by funders of research, in some developed countries, because of the erroneous belief that caries is no longer a public health problem. In addition, the complex role that the ecology of the biofilm plays in caries initiation and prevention has not been understood.
Clinical Sciences and Public Health Practice – the Second Implementation Gap
Advances in dental materials have dominated restorative dentistry to a greater extent than any advance in the field of cariology. The failure to change how caries is managed can be attributed in large measure to factors such as clinical and professional conservatism, economic incentives that reward surgical treatment more highly than preventive caries control, and the consistent failure of communication between the dental sub-groups, with poor communication by the research community and limited attempts at systematic implementation of research findings by clinicians working in health systems that promote the status quo.
The existence of the deep silos which dental public health practitioners, clinicians, and researchers inhabit has militated against the translation of research into policy and practice. There has also been a view that the public health and clinical perspectives on caries management have been mutually exclusive, instead of potentially synergistic.
Strategies to Close the Implementation Gaps in Caries Prevention and Treatment
Promoting consistency in terminology and knowledge across the silos of research, practice, epidemiology, public health, and education. This process has begun with the promulgation of a standardized “Glossary” of key caries terms (Longbottom et al., 2009) produced by ICDAS, the European Organisation of Caries Research (ORCA), and the American Dental Education Association (ADEA). This has now also been adopted by the FDI and is being developed further.
Getting research findings, distilled systematically as best evidence, into both practice and policy. These processes are being documented with knowledge bases from outside of dentistry—for example, from medicine and psychology—and are being addressed in several ways, outlined below.
Addressing inequalities at the regional, country, and local levels and improving the methodology by which we can recognize and monitor inequalities at these levels. A series of options to record and monitor caries impact using appropriate oral health indicators should be developed further.
Using the Collaboration for Improving Dentistry model to build partnerships in the caries world. This model (Pitts and Wefel, 2009) is proving helpful in discussions with numerous stakeholders in determining how multiple partners, including industry as well as other global organizations, can engage most effectively to improve oral health and reduce inequalities in caries. The Collaboration for Improving Dentistry model is shown in Fig. 4.
Using implementation research to improve the knowledge transfer process. Implementation research is itself a developing and complex field, but with the increasing importance of all types of translational research, there is much confusion in the research and health communities. The key priority is to meet the need to move knowledge into action (Graham et al., 2006); in clinical settings, we need not only evidence-based guidelines, but also a process by which knowledge is developed into specific tools and products. These need to be appropriate to the local context and applied in tailored interventions, the outcomes of which are evaluated so knowledge use can be optimized and sustained.
Fig. 4.
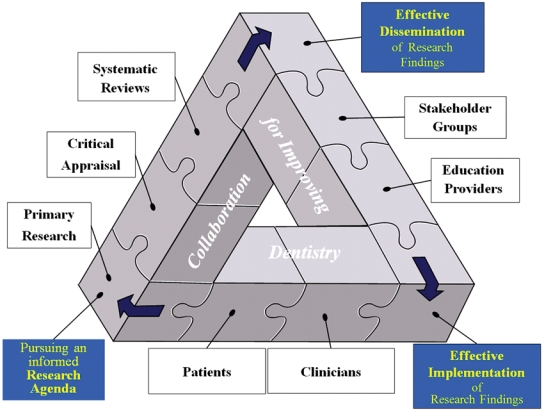
Collaboration for Improving Dentistry (CID) model of implementing research findings into practice. Reproduced with permission from Pitts and Wefel (2009).
Current Priorities for Both Basic and Applied Research
There are four overriding priorities for caries research in the context of this initiative:
It must play its part in integrating health and oral health wherever possible, using the common risk factors approach linking caries to diet and hygiene.
It must be able to respond to and influence international developments in health, healthcare, and health payment systems, as well as dental prevention and materials. This is particularly important in view of global discussions around the future use of dental amalgam.
It must explore the potential for novel funding partnerships with organizations, industry, and foundations which will allow research to be taken forward at a time of economic challenge.
It must establish effective two-way communication between and among the basic science, clinical science, and health promotion/public health research communities. Implementation research should be a priority for all three groupings.
Basic Cariology Sciences Priorities
ICNARA-derived priorities for caries research include caries remineralization and biofilm/antibacterial/probiotic approaches to caries management (ICNARA, 2009).
Remineralization
The aim of remineralization therapy is to facilitate caries control over a lifetime, using evidence-based, clinically effective, multifactorial prevention to keep the caries process in balance. The following priorities have been broadly agreed (Pitts and Wefel, 2009):
A validated menu of caries control strategies/methods/ products, which are effective for individuals, subgroups, and populations, is needed.
A corresponding menu of standardized, agreed, comparable protocols is also needed to allow for meaningful comparisons across studies.
Over the coming years, the dental research community in this field should also continue to apply new knowledge and methods from outside dentistry.
Biofilm and Caries Control
The successful approaches to caries control will be those that are clinically effective and profitable. The following have been highlighted as future priorities (Adair and Xie, 2009):
Development of targeted, rather than broad-spectrum, chemotherapeutic approaches, which are presently in their infancy. There is a need for a better understanding of biofilm physiology and pathogenicity, and the role of the biofilm in promoting oral health.
The genome revolution opens up new ways to view the biofilm and develop novel anticaries approaches, and these need to be explored.
Research should be conducted in synergistic approaches to promote simultaneous remineralization and biofilm-targeted anti-caries approaches.
Clinical Sciences Priorities
Over the past 8 years, the ICDAS framework for grading caries has resulted in the publication of many research papers from around the globe, using consolidated, compatible, and comparable measures of dental caries (ICDAS Foundation, 2010b). Since the IADR General Session in Miami in 2009, when the “Grand Challenge” was issued (Williams, 2009), the wider clinical caries management research and implementation priorities have been synthesized and taken forward by a broad group of stakeholders (see Appendix). This work has produced a new ICDAS-International Caries Classification and Management System (ICDAS-ICCMS™), a brief outline of which is reported here, since it reflects recent work undertaken to support this IADR initiative. The System addresses both clinical and public health issues: It is about applied cariology research translated into clinical practice, and it shares the overall health improvement goal agreed by the FDI World Dental Federation of seeking to bring optimal oral and thus general health and well-being to all people. It supports both general and personalized caries prevention, and, when implemented in concert with appropriate parallel upstream public health and integrated health promotion approaches, should facilitate a reduction in health inequalities.
Implemented effectively the ICDAS-ICCMS™ approach should support the objectives and approach set out in “Fair Society, Healthy Lives” (Marmot, 2010). This report stresses that, to reduce the steepness of the social gradient in health, actions must be universal, but with a scale and intensity that are proportionate to the level of disadvantage. Marmot also points out the challenge that “Greater intensity of action is likely to be needed for those with greater social and economic disadvantage, but focusing solely on the most disadvantaged will not reduce the health gradient, and will only tackle a small part of the problem.”
To translate best evidence from clinical sciences research into practice, the ICCMS™ groups the clinical procedures for caries prevention, management, monitoring, and review into four linked key elements (see Fig. 5).
Fig. 5.
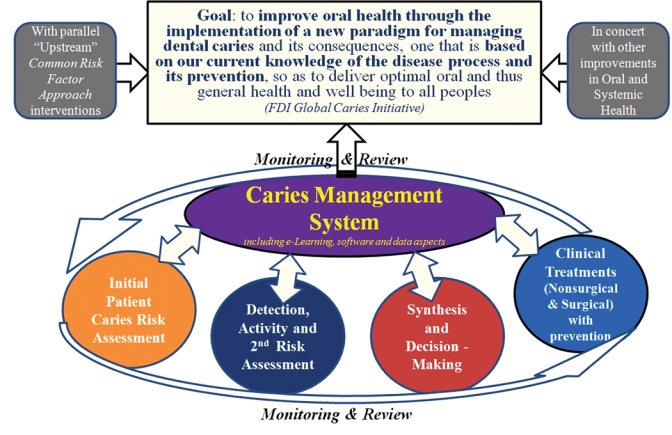
Graphical overview of the goal and components of the ICDAS-International Caries Classification and Management System (ICDAS-ICCMS™).
The System aims to expand the management decisions that are intuitively made by dentists to include secondary preventive measures applied on early or noncavitated caries lesions, as well as modern evidence-informed strategies for risk assessment, decision making, and minimally invasive restorative care. Using these management decisions, the ICDAS-ICCMS™ Group has developed analytical algorithms that will enable dentists to make clinical decisions that incorporate information on lesion extent and activity, as well as individual caries risk status.
The guiding principles for the ICDAS-ICCMS™ are as follows:
Prevention is a priority, with surgical intervention used only as a last resort.
Where surgery is indicated, use minimal removal of tooth tissue.
Cavity size and selection of material are governed by preservation of tooth tissue destruction and healthy patient outcomes.
Detailed practice-friendly protocols are being developed and tested by 11 universities from Colombia, Denmark, Germany, Iceland, Kuwait, the UK, and the US, and these should be evaluated in a range of settings. Discrete elements of the system may be evaluated in isolation, but, in addition, comparative effectiveness designs should be used to assess the overall impact and costs of the new System.
Implementation Research/Dental Public Health/Oral Health Promotion Priorities
The priority in implementation research is to embed a systematic process (see Fig. 4) in which the particular areas that need to be addressed are identified, with an improvement cycle incorporated. It requires an informed research agenda, mounting effective dissemination of research findings to key groups, and also taking proactive systematic steps to achieve effective implementation of the results by properly prepared clinicians to help informed patients. The clinical or public health systems so produced will, in turn, be re-evaluated.
Other priorities include theory-based studies to gain insights into the individual and organizational barriers to, and enablers of, the translation of research findings into primary care, and the evaluation of different payment systems for prevention.
Further topics identified by WHO include the development of appropriate information systems as an integral part of national surveillance of oral health and risk factors, provision of evidence for oral health policy and practice, formulation of goals and targets, and measurement of progress in public health. Priorities include: the promotion of research in oral health aimed at bridging gaps in research between low-/middle-income and high-income countries; conduct of operational research; and translation of knowledge about oral-health promotion and disease prevention into public health action programs.
In attempts to meet the need for more comprehensive epidemiological surveillance, research is under way supported by the IADR Regional Development Program in eight countries in Latin America using ICDAS epidemiology codes in field studies with standardized training and calibration. At this early stage, the project shows promise, and an extension to the study is planned. This work follows a range of enhanced caries surveillance activities ranging from National Surveys in Iceland, including initial lesions and radiographs (Agustsdottir et al., 2010), to the European Global Oral Health Indicators Projects EGOHID I and II (Bourgeois et al., 2008), and assessing the determinants of early childhood caries in low-income African American young children (Ismail et al., 2008). It is envisaged that this pattern of working jointly, with sharing of experiences and methodology as practiced by the European Association for Dental Public Health, will be further built with groups in IADR and the FDI World Dental Federation.
The surveillance and planning data generated will make a beneficial change to caries levels and other health inequalities only if they are used actively to promote prevention, health, and well-being. Furthermore, planned actions should be universal, but with a scale and intensity that are proportionate to the level of disadvantage (Marmot, 2010). While there is quite properly a focus on children and early years, it is also a priority to consider what action is needed across the life course. Disadvantage starts before birth and accumulates throughout life (Fig. 6). Action to reduce health inequalities must start before birth and be followed through the life of the child. Only then can the close links between early disadvantage and poor outcomes throughout life be broken. Meanwhile, there is much that can be done to improve the lives and health of people who have already reached school, working age, and beyond. Services that promote the health, well-being, and the dental and social independence of older people and, in so doing, prevent or delay the need for more intensive or institutional care, make a significant contribution to ameliorating oral health and health inequalities.
Fig. 6.
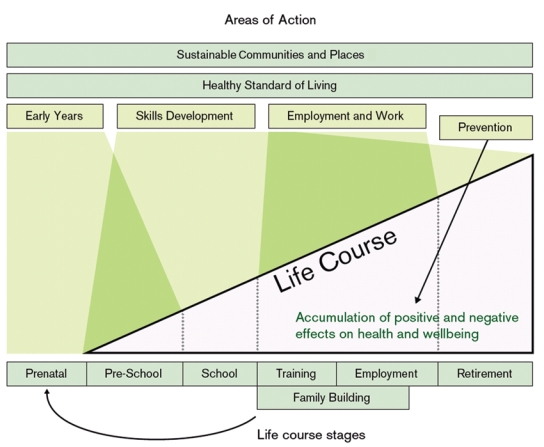
Areas of preventive action across the life course. Reproduced with permission from Marmot (2010).
The 7th WHO Global Conference on Health Promotion, toward integration of oral health, held in Nairobi, Kenya, in 2009 (Petersen and Kwan, 2010), highlighted the need to close the implementation gap and outlined strategies for tackling social determinants of oral health to improve oral health, including caries, and reduce inequalities. The meeting outlined a range of priorities to be carried out in support of the World Health Assembly Resolution (WHA60.17) on oral health.
A Five-year Research Agenda, Which Will Lead to Key Improvements in Global Oral Health, with Particular Reference to Inequalities between and within Countries
The research agenda should address all of the priorities for research listed in the preceding section. The research focus must be capable of being taken forward on a global basis, but must remain sensitive to countries, cultures, economies, and aspirations, nationally and locally.
Priority research recommendation: to translate existing evidence into routine clinical and public health practice; to tailor interventions to a more equal and person-centered preventive focus; and to reduce any social gradient in health. The sequence of priorities is to start with clinical and public health implementation of existing research findings, and, in parallel, to seek new basic science insights in key areas.
Clinical Sciences in Cariology Agenda
— The evaluation, as a holistic systems and social model, of the implementation of the ICDAS-ICCMS™ in educational and primary care network settings. This research should include the use of novel eHealth record linkages to assess the impact of caries prevention on a longitudinal basis, using patients in dental schools, in primary care, and in clinics. The use of comparative effectiveness designs will allow for clinical and economic real-world assessment of the overall disease management approach, as compared with the traditional restorative model of caries treatment.
—Optimization of the individual ICDAS-ICCMS™ elements of risk assessment, lesion detection, caries activity assessment, synthesis, decision making, nonsurgical treatment of lesions, and the monitoring and review of both patients and lesions are included under this umbrella.
Other research priorities for clinical caries management are set out as a more detailed list in the Appendix and include:
development of an agreed matrix of designs for in situ and in vivo research to develop and evaluate a menu of clinically effective caries control products for enamel, dentin, root-surface, and orthodontics-related caries across anatomic predilection sites, ages, and risk groups; and
determination of how best to educate health-care providers to deliver effective caries management incorporating remineralization, nonsurgical clinical management, and maintenance of early caries lesions.
Health Promotion/Public Health Caries Agenda
The key priority in this agenda is the evaluation of the impact of caries prevention programs designed to achieve a greater intensity of action and effectiveness for those with greater social and economic disadvantage, so reducing the health gradient while improving oral health for the whole population under study.
Within that overall scope, priorities include the evaluation and assessment of:
public health interventions delivering oral health promotion activity linked to general health promotion;
the feasibility and acceptability of epidemiological mapping by recording of the total clinical caries experience (including initial lesions as well as sepsis) to better recognize and monitor inequalities at regional, country, and local levels;
models of care in which there are integrated roles for dental, medical, and other health-care providers;
the barriers and facilitators to using the preventive caries management system approach, using theory-based methods from implementation science to better define options appropriate to different settings and economies;
the effectiveness and economic benefit of different skill-mix combinations used to deliver the ICDAS-ICCMS™ approach to improving health and reducing caries inequalities; and
the impact of remuneration systems on the types of clinical caries care delivered and the outcomes achieved.
Basic Sciences in Cariology Agenda
It is recommended that, to translate both existing and new research into clinical and public health practice to best effect, grouped topics should be considered at International Consensus Development Workshops on:
defining valid and efficient research methods for demonstrating caries arrest and assessing the remineralization potential of candidate agents; and
defining ways to ensure that findings about remineralization and new biofilm-based methods of effective caries control can be transferred more efficiently and rapidly into routine clinical therapy and practice.
Supplementary Material
Acknowledgments
We acknowledge the numerous wider collaborators who have participated willingly and helpfully in this process, particularly Dr. Michael Glick, Baltimore, MD, USA, in his capacity as Chair of the FDI Science Committee, and Dr. Mark Wolff, NYU, New York, US, both a caries researcher and a lead in the development of a new Cariology Section within the American Dental Education Association. The authors of this paper have all published specific studies relating to cariology. These studies were supported by a wide range of sources, ranging from government research funding agencies (e.g., National Institutes of Health), to research charities, to foundations and commercial companies working in the oral health industry.
Footnotes
A supplemental appendix to this article is published electronically only at http://adr.sagepub.com/supplemental.
References
- Adair SM, Xie Q. (2009). Antibacterial and probiotic approaches to caries management. Adv Dent Res 21:87-89 [DOI] [PubMed] [Google Scholar]
- Agustsdottir H, Gudmundsdottir H, Eggertsson H, Jonsson SH, Gudlaugsson JO, Saemundsson SR, et al. (2010). Caries prevalence of permanent teeth: a national survey of children in Iceland using ICDAS. Community Dent Oral Epidemiol 38:299-309 [DOI] [PubMed] [Google Scholar]
- Bourgeois DM, Llodra JC, Christensen L.-B, Pitts NB, Ottolenghi L, Senekola E, editors (2008). Health surveillance in Europe. Oral health interviews and clinical surveys: guidelines. Lyon, France: University Lyon I, Publisher [Google Scholar]
- Cooksey Report (2006). A review of UK health research funding, 2006. URL available at: www.hm-treasury.gov.uk/independent_reviews/Cooksey_review/cookseyreview_index.cfm (accessed Dec. 23, 2010).
- Elderton RJ. (1990). Clinical studies concerning re-restoration of teeth. Adv Dent Res 4:4-9 [DOI] [PubMed] [Google Scholar]
- FDI World Dental Federation (2009). Oral health atlas, 2009. URL available at: http://www.fdiworldental.org/content/oral-health-atlas (accessed Dec. 23, 2010).
- Featherstone JD. (2009). Remineralization, the natural caries repair process—the need for new approaches. Adv Dent Res 21:4-7 [DOI] [PubMed] [Google Scholar]
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. (2006). Lost in knowledge translation: time for a map? J Cont Edu Health Prof 26:13-24 [DOI] [PubMed] [Google Scholar]
- ICDAS Foundation (2010a). Shared vision. URL available at: http://www.icdasfoundation.dk/s2.htm (accessed Dec. 23, 2010).
- ICDAS Foundation (2010b). ICDAS in the literature. URL available at: http://www.icdas.org/journal.htm (accessed Dec. 23, 2010).
- ICNARA (2009). Novel anti-caries and remineralizing agents, proceedings of an international conference held in Vina del Mar, Chile, January 10th-12th 2008. Adv Dent Res 21:3-89 [PubMed] [Google Scholar]
- Ismail AI, Lim S, Sohn W, Willem J. (2008). Determinants of early childhood caries in low-income African-American young children. Ped Dent 30:289-296 [PubMed] [Google Scholar]
- Longbottom C, Huysmans M-C, Pitts NB, Fontana M. (2009). Glossary of key terms. In: Detection, assessment, diagnosis and monitoring of caries. Monographs in Oral Science, Vol. 21 Pitts NB, editor. Basel: S. Karger AG, pp. 209-216 [DOI] [PubMed] [Google Scholar]
- Marmot M. (2010). Fair society, healthy lives - The Marmot Review. Strategic review of health inequalities in England post-2010. London: Marmot Review [Google Scholar]
- Petersen PE. (2008). World Health Organization global policy for improvement of oral health – World Health Assembly 2007. Int Dent J 58:115-121 [DOI] [PubMed] [Google Scholar]
- Petersen PE, Kwan S. (2010). The 7th WHO Global Conference on Health Promotion - towards integration of oral health (Nairobi, Kenya, 2009). Community Dent Health 27(Suppl 1):129-136 [Google Scholar]
- Pitts NB. (2004). Are we ready to move from operative to non-operative/preventive treatment of dental caries in clinical practice? Caries Res 38:294-304 [DOI] [PubMed] [Google Scholar]
- Pitts NB. (2009). Introduction. How the detection, assessment, diagnosis, and monitoring of caries integrate with personalised caries management. In: Detection, assessment, diagnosis and monitoring of caries. Monographs in Oral Science, Vol. 21 Basel: S. Karger AG, pp. 1-14 [DOI] [PubMed] [Google Scholar]
- Pitts NB, Wefel JS. (2009). Remineralization/desensitization: what is known? What is the future? Adv Dent Res 21:83-86 [DOI] [PubMed] [Google Scholar]
- Selwitz RH, Ismail AI, Pitts NB. (2007). Dental caries. Lancet 369:51-59 [DOI] [PubMed] [Google Scholar]
- Sung NS, Crowley WF, Jr, Genel M, Salber P, Sandy L, Sherwood LM, et al. (2003). Central challenges facing the national clinical research enterprise. J Am Med Assoc 289:1278-1287 [DOI] [PubMed] [Google Scholar]
- ten Cate JM. (2009). The need for antibacterial approaches to improve caries control. Adv Dent Res 21:8-12 [DOI] [PubMed] [Google Scholar]
- Williams DA. (2009) Presidential address. URL available at: http://newsmanager.commpartners.com/iadr/issues/2009-05-20/email.html#1 (accessed Dec. 23, 2010).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


