Abstract
This study tested the hypothesis that all-ceramic core-veneer system crown reliability is improved by modification of the core design. We modeled a tooth preparation by reducing the height of proximal walls by 1.5 mm and the occlusal surface by 2.0 mm. The CAD-based tooth preparation was replicated and positioned in a dental articulator for core and veneer fabrication. Standard (0.5 mm uniform thickness) and modified (2.5 mm height lingual and proximal cervical areas) core designs were produced, followed by the application of veneer porcelain for a total thickness of 1.5 mm. The crowns were cemented to 30-day-aged composite dies and were either single-load-to-failure or step-stress-accelerated fatigue-tested. Use of level probability plots showed significantly higher reliability for the modified core design group. The fatigue fracture modes were veneer chipping not exposing the core for the standard group, and exposing the veneer core interface for the modified group.
Keywords: all-ceramic crown, mechanical testing, step-stress fatigue, core design
Introduction
Great effort has been expended in the development of stronger and more reliable ceramics. Fracture strengths have progressively increased from glass-ceramic (Empress II, 320 MPa) to alumina (547 MPa) and to zirconia (900 MPa) (Deng et al., 2002). The high value found for the latter, similar to metals such as steel (Manicone et al., 2007), has encouraged its use for hip (Chevalier and Gremillard, 2009) and knee replacements, dental crowns, fixed dental prostheses (FDP), and dental implants (Kohal and Klaus, 2004; Kohal et al., 2006; Silva et al., 2009). Zirconia’s intermediate elastic modulus has been shown to be advantageous in reinforced layered structures, shifting damage and fracture modes into the porcelain veneer layer (B. Kim et al., 2007).
Fracture (chipping) of the veneer has been reported as the major clinical reason for technical complications of zirconia-supported restorations in the posterior region (Sailer et al., 2007b; Della Bona and Kelly, 2008). While combined fracture of the veneer and core is rare, efforts to reduce chipping represent a chief concern in the use of zirconia restorations. The oscillation between positive (Molin and Karlsson, 2008; Beuer et al., 2009) and less encouraging success rates (Larsson et al., 2006; Raigrodski et al., 2006; Sailer et al., 2007b) in clinical studies leads to a confusing rationale for materials selection where mechanical properties have limited association with clinical longevity (Rekow et al., 2007).
Besides materials strength, other factors affect restorations’ clinical longevity, such as prosthesis design (Rekow and Thompson, 2007). However, the effects of changes in design have not been thoroughly evaluated. Alterations in the dimensions and thicknesses of crown restorations have been empirically used, but not systematically evaluated for either in vivo or in vitro studies (McLaren and White, 1999).
A laboratory testing method for anatomically based crowns has been shown to reproduce the clinical failures of zirconia crowns (Coelho et al., 2009a). A subsequent study using the same molar crowns showed that sliding fatigue in the disto-buccal cusp led to cohesive failures of similar pattern and comparable reliability for both zirconia systems investigated (Coelho et al., 2009b). While these studies fatigued the buccal cusp, known as the centric contact for mandibular posterior teeth, it is interesting to note that clinically cohesive failures in the lingual cusps of mandibular posterior all-ceramic restorations have been reported in several studies (Raigrodski et al., 2006; Sailer et al., 2007a; Guess et al., 2009). One possible reason is that group function is the most frequent occlusal scheme in the natural permanent dentition (41% compared with 26% of canine-protected articulation), also found to increase with age (Panek et al., 2008). Hence, from a dynamic occlusion perspective, a laterotrusive movement (working side) in an Angle Class I group function occlusal scheme may involve the inner inclines of the mandibular lingual cusps sliding against the outer inclines of the maxillary lingual cusps (Okeson, 1998; Ash, 2003). Thereby, core design modifications increasing the support of the porcelain in the lingual cusp could improve fatigue response.
This study utilized a step-stress fatigue method to assess the reliability and failure modes of all-ceramic zirconia-based single crowns cemented on a standardized mandibular first molar replica, exploring the effects on the fatigue lifetime of a modified core design. The hypothesis of this study was that higher sliding contact fatigue reliability is to be expected when core design provides more veneer support.
Materials & Methods
An acrylic replica of an anatomically based mandibular first molar full crown preparation was obtained from a plastic model that was created by milling technology from a CAD file as previously described (Coelho et al., 2009a). The replica was positioned in a dental mannequin with opposing and adjacent dentition. Impressions of the prepared, adjacent, and opposing teeth were taken (Aquasil, Dentsply, York, PA, USA) and sent to a CAD/CAM milling center for fabrication of the yttria-tetragonal zirconia polycrystal (Y-TZP) cores (LAVA, 3M/ESPE, St. Paul, MN, USA). These Y-TZP cores were fabricated with 2 different core designs, thus assigned to groups described as follows:
• Group standard (STD): For this group (n = 17), the Y-TZP cores were fabricated with an even 0.5-mm thickness, identified as standard cores (Fig. 1).
Figure 1.

Schematic of core designs and loading location. Image “A” represents a lateral view of a full crown preparation. “B1” and “B2” show core designs for groups STD and MOD, respectively. Total crown height was 5 mm (C). Note, for the MOD design, the 2.5-mm height at the lingual extending to the proximals, providing more ceramic support (D). Load was applied at the buccal incline of the mesio-lingual cusp for STD and MOD. (E) Occlusal view of first lower molar configuration with the area of sliding contact indicated (black oval shape).
• Group modified (MOD): For this group (n = 17), a design modification of the core was proposed and comprised a standard core increased by a 1-mm thickness in the proximal area, and a 2.5-mm-height cervical margin on the lingual, which extended proximally (Fig. 1).
All Y-TZP cores were veneered with porcelain (LAVA Veneer, 3M/ESPE, St. Paul, MN, USA) by a commercial dental laboratory (Marotta Dental Studio, Huntington, NY, USA), using the dental mannequin for occlusal and proximal contacts and appropriate geometry (Fig. 1). To standardize the thickness of the veneering ceramic, a silicone index made from an impression of the waxed desired anatomy was used to guide porcelain contour and anatomy in all crowns.
Thirty-four prepared tooth composite (Z100, 3M/ESPE, St. Paul, MN, USA) dies were fabricated from hard addition silicon impressions (Aquasil, Dentsply, York, PA, USA) of the machined plastic model described above. The dies were stored in distilled water at 37°C for at least 30 days to ensure full hydration and eliminate any effect of water-uptake dimensional expansion (Huang et al., 2007).
The crowns were cemented (RelyX Unicem, 3M/ESPE, St. Paul, MN, USA) under a 10-N load following manufacturer’s instructions. The cemented crowns were embedded in acrylic resin (Orthoresin, Degudent, Mainz, Germany) in a 25-mm-diameter PVC tube, leaving buccal, lingual, and interproximal cervical margins exposed 2 mm above the potting surface. The long axis of the crown-die assembly was aligned with the long axis of the tube.
Following cementation procedures, the specimens were kept in distilled water for 7 days to provide adequate water equilibration before mechanical testing. Three crowns of each group underwent single-load-to-fracture (SLF) testing in a universal testing machine equipped with a 6.25-mm-diameter tungsten carbide ball and 10-KN load cell at a cross-head speed of 1 mm/min (INSTRON 5666 machine, Canton, MA, USA). Based upon the mean load to failure from SLF, sliding-contact step-stress accelerated life-testing (SSALT) profiles were determined, being mild (n = 8), moderate (n = 4), and aggressive (n = 2), with the number of specimens assigned to each group following approximately the ratio 4:2:1 (Nelson, 1990). The 3 profiles involved fatigue loads ranging from a minimum of 50 N to a maximum of 800 N, requiring 190,000, 180,000, and 150,000 cycles for the mild, moderate, and aggressive profiles, respectively, to reach the maximum load. The difference in load application mode throughout the profiles was the magnitude of load increase during each step cycle, where the mild profile would cycle longer to reach the same load level as the aggressive profile. The specimens were attached to a servo-all-electric system (800L, TestResources, Shakopee, MN, US), and subjected to step-stress fatigue until failure or survival (Nelson, 1990). The criterion for survival was the absence of fracture at the end of a given profile (approximately 800-N load), either within the veneer (cohesive) or exposing the core (Rekow and Thompson, 2007). Loads above 800 N were considered of limited clinical interest, since they seldom occur in normal function (DeLong and Douglas, 1983). The sliding contact was obtained with a WC indenter of 6.25-mm diameter sliding 0.7 mm down the buccal incline of the mesio-lingual cusp, beginning at 0.5 mm buccal to the cusp tip. A master Weibull curve and reliability for completion of a mission of 50,000 cycles at 200- and 300-N loads were calculated (Zhao and Elsayed, 2005) (Alta Pro 7, Reliasoft, Tucson, AZ, USA). A power law damage accumulation model was used in these calculations.
The specimens were evaluated under polarized light (MZ-APO stereomicroscope, Carl Zeiss MicroImaging, Thornwood, NY, USA) at the completion of each fatigue step for crack evolution. Criteria used for failure were: delamination (core exposure), cohesive fracture within veneering porcelain (chipping), cracks that extended to the framework (radial cracks), and catastrophic failure (bulk fracture). Representative samples were gold-sputtered (Emitech K650, Emitech Products Inc., Houston, TX, USA), and fractographic analysis was performed by scanning electron microscopy (SEM) (Hitachi, Model 3500S, Osaka, Japan).
Results
The SLF mean values were 1134 ± 182 N and 767 ± 154 N for groups STD and MOD, respectively. The failure mode observed for all specimens after load to fracture was veneer delamination for both groups. No Y-TZP core fracture was detected.
The step-stress derived use level probability Weibull was calculated, and plots (reliability vs. number of cycles) were produced for a use stress of 200 N (Fig. 2). The resulting Betas of 2.37 for group STD and 6.38 for group MOD indicated that fatigue (damage accumulation) was an acceleration factor for both groups. The latter Beta appears as a steeper curve for the MOD group.
Figure 2.

Reliability vs. number of cycles for a 200-N load based upon a use level probability Weibull calculation for groups STD and MOD with the Beta values of 2.37 and 6.38, respectively. Note that group MOD is positioned to the right on the plot, and the two-sided 90% confidence intervals do not overlap. Five samples of each group were considered suspended.
All available data were considered in the analysis of times-to-failure. This included the case when a particular unit in a sample had been removed from the test prior to failure. The specimen that is removed from a reliability test at a specific profile before failure occurs, and is still operating at the time the reliability of these units is to be determined, is called a suspended sample. Five samples of each group were considered suspended after the pre-determined number of cycles of a specific step-stress profile was reached and fracture was not observed. The calculated reliability for both groups is shown in the Table, with 90% confidence intervals for a mission of 50,000 cycles at 200 N and 300 N. Reliability calculations for group MOD were significantly higher than those for group STD for both use load magnitudes. There was a trend to reduced reliability for group STD when the given load was increased from 200 N to 300 N. However, no statistical difference was seen as a result of overlap between upper and lower confidence bounds (Table).
Table.
Calculated Reliability at 90% Confidence Intervals (CI) for Standard (STD) and Modified (MOD) Core Design Groups
| Reliability 90% CI | STD 50K Cycles @ 200 N | STD 50K Cycles @ 300 N | MOD 50K Cycles @ 200 N | MOD 50K Cycles @ 300 N |
|---|---|---|---|---|
| Upper | 0.74 | 0.60 | 1.00 | 1.00 |
| Reliability | 0.53* | 0.21* | 0.99^ | 0.99^ |
| Lower | 0.27 | 0.01 | 0.96 | 0.90 |
* and ^ represent statistical differences among groups. Note significant difference between groups for a mission of 50,000 cycles at 200 N and 300 N.
The surface damage created on the incline of suspended specimens after 150,000 cycles and 600 N of load is shown in Figs. 3a and 3b. The damage on the sliding trail that leads to a more pronounced area of friction-assisted wear as a result of attrition of the porcelain veneer by the indenter is shown in Fig. 3b. The sliding contact step-stress fatigued specimens for group MOD showed smaller fracture size but more extensive fracture into the veneer layer, exposing the Y-TZP modified core surface (Fig. 3c). Wake hackles evidencing fracture originating from the indentation sliding trail are shown in Fig. 3d. Wake hackles are hackle marks that extend from a singularity (porosity in this case) at the crack front in the direction of cracking (Quinn, 2007). For the STD crowns, larger fracture sizes (bulk of the cusp and extended to proximal and cervical regions) were observed, but specimens failed cohesively within the veneer layer (Figs. 3e, 3f). No fracture through the Y-TZP core was observed for either core design.
Figure 3.
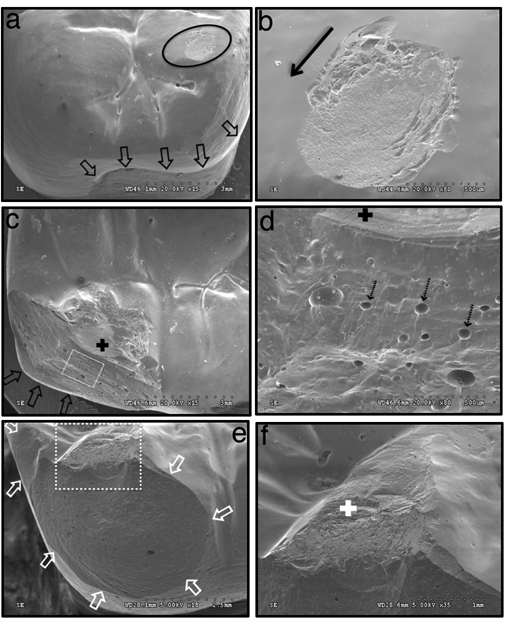
Scanning electron microscopic (SEM) images after mouth motion sliding contact fatigue testing. Images “a” and “b” are SEMs of one MOD of the suspended specimens after 150,000 cycles at 600 N of load. Arrows delimit the core-modified area, and the oval black line indicates the indenter contact area seen in b. The black arrow in b shows the direction of sliding contact. The surface damage created was the result of friction-assisted attrition of the veneer by the indenter. “c” and “d” represent a fractured sample of group MOD after 130,432 cycles at 500 N of load. The black arrow (c) points to the edge of the modified core at the lingual and mesial sides after fracture. The black cross lies on the Y-TZP core exposed by veneer fracture. This was a typical event for failed specimens of group MOD. “d” represents a higher-magnification image of the white dotted box seen in “c”. Segmented arrows show voids in the porcelain veneer followed by wake hackles, demonstrating fracture direction. Images “e” and “f” show a fractured specimen of group STD after 80,000 cycles at 300 N of load. White arrows show the cohesively fractured veneer extending to proximal and cervical areas. The white cross (f) lies on the indentation site. Extensive surface damage can be seen as a result of attrition created by the tungsten carbide ball during sliding contact.
Discussion
The design modification proposed in this study is based on what has been previously proposed for porcelain-fused-to-metal (PFM) crowns (Shelby, 1962; Marker et al., 1986). However, such PFM core design has never been clinically evaluated, since metal core fracture is unlikely because of its ductility, and survival rates are known to be high in such systems (Donovan, 2009).
In contrast, the literature concerning the clinical performance of all-ceramic systems is inconclusive regarding the relative performance of different materials and physical configurations. In addition to an anecdotal positive clinical report on a modified core designed for zirconia crowns (Marchack et al., 2008), clinical studies on zirconia fixed partial dentures with anatomic framework design showed promising survival rates in three- (Tinschert et al., 2008) and five-year (Molin and Karlsson, 2008) mean follow-up studies. Even though a standard design was not evaluated as the control, the authors speculated on the potential of the framework design used in providing better porcelain support during function.
Another study (Bonfante et al., 2009) evaluated the characteristic strength and failure modes of glass-infiltrated alumina (In-Ceram) compared with porcelain-fused-to-metal premolar crowns. They compared a standard (even 0.5-mm core thickness) and a modified core design (cervical margin increased to 2.0 mm height and 1 mm thick at the lingual, connected to proximal strut of 3.5 mm height). Although the porcelain-fused-to-metal group had significantly higher strength in all instances compared with the In-Ceram group, the modified core design for the latter group significantly increased the characteristic strength. Both groups were cemented on high elastic modulus (stainless steel) “preparations.”
In our investigation, we used a mandibular first molar, and the core for group MOD had an even 2.5-mm height of cervical margin at the lingual and proximal sites. Both groups, STD and MOD, were cemented to resin composite “preparations” (dies) with a modulus of elasticity similar to that of dentin (from 16 to 18 GPa), presenting a clinically realistic scenario for fatigue testing.
The SSALT approach used in this study consists of testing the samples at increasing levels of stress, which become higher than use stress, to accumulate damage while facilitating failures in a timely manner. The results of these tests are then analyzed so that a profile of the failure behavior specimens at use stresses can be determined. The SSALT testing was conducted in water with translation of the indenter 0.5-0.7 mm along the buccal incline of the mesio-lingual cusp toward the central fossa, simulating approximating tooth surfaces during mastication. Such translation has been shown to be highly deleterious due to a stress field extension and water magnification of partial cone cracks in flat-layer studies (B Kim et al., 2007; JW Kim et al., 2007, 2008; JH Kim et al., 2008). The veneer cohesive failure found beneath the indenter path suggests that this hydraulically magnified damage mode is operational in these anatomical crowns. The high hardness of the tungsten carbide indenter only slightly changes the rate of crack initiation and evolution for the veneering porcelain when compared with a glass indenter with an elastic modulus slightly lower (70 GPa) than that of tooth enamel (80-90 GPa) (Bhowmick et al., 2007).
The proposed Y-TZP core design modification for group MOD improved the reliability compared with that of group STD. Whereas this result is in contrast to the higher SLF mean value observed for the STD compared with the MOD, limited conclusions should be drawn from these results, since they do not simulate damage accumulation occurring during function (Kelly, 1999). The SLF test was used in the present study only to design step-stress profiles for mouth-motion fatigue testing. The reason for such fatigue response improvement might be attributed not only to the higher ceramic support created, but also to the thermal expansion and cooling responses of the different core designs. Porcelain-veneered zirconia failures have led to concerns regarding differences in coefficient of thermal expansion between the core and veneering porcelain and their respective processing techniques (Raigrodski et al., 2006), or due to the low thermal diffusivity of zirconia compared with that of alumina or metal (Swain, 2009).
All SSALT specimens for group STD failed within the veneer layer. The more confined failure mode for group MOD included, in addition to cohesive veneer fracture, Y-TZP core exposure. Wake hackles observed in the SEM indicate that failure progressed from the contact area through the body of the porcelain, as noted in clinical replicas (Scherrer et al., 2008), suggesting that the methodology used was successful in simulating clinical scenarios. Hence, core design modification resulted in a significantly higher reliability at both 200- and 300-N loads (50,000-cycle mission) when compared with STD, and, since the chips are smaller, they may be repaired chairside.
The testing scenario used was able to mimic clinical failure observed with uniform-thickness core designs. The modified design showed the benefits of additional porcelain support compared with a standard design by improving the reliability of this all-ceramic crown system. Thus, the study hypothesis was accepted. Because the proposed design improved the reliability of the lingual cusp only, further studies of design modifications involving additional support on the buccal cusps as well are warranted.
Acknowledgments
Hitachi S3500N SEM imaging was made possible by cooperative agreement with NIH/NIDCR. Support was provided by NIDCR P01-DE10976.
References
- Ash MM. (2003). Occlusion: reflections on science and clinical reality. J Prosthet Dent 90:373-384 [DOI] [PubMed] [Google Scholar]
- Beuer F, Edelhoff D, Gernet W, Sorensen JA. (2009). Three-year clinical prospective evaluation of zirconia-based posterior fixed dental prostheses (FDPs). Clin Oral Investig 13:445-451 [DOI] [PubMed] [Google Scholar]
- Bhowmick S, Melendez-Martinez JJ, Hermann I, Zhang Y, Lawn BR. (2007). Role of indenter material and size in veneer failure of brittle layer structures. J Biomed Mater Res B Appl Biomater 82:253-259 [DOI] [PubMed] [Google Scholar]
- Bonfante EA, Silva NR, Coelho PG, Bayardo-Gonzalez DE, Thompson VP, Bonfante G. (2009). Effect of framework design on crown failure. Eur J Oral Sci 117:194-199 [DOI] [PubMed] [Google Scholar]
- Chevalier J, Gremillard L. (2009). Ceramics for medical applications: a picture for the next 20 years. J Eur Ceram Soc 29:1245-1255 [Google Scholar]
- Coelho PG, Bonfante EA, Silva NR, Rekow ED, Thompson VP. (2009a). Laboratory simulation of Y-TZP all-ceramic crown clinical failures. J Dent Res 88:382-386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coelho PG, Silva NR, Bonfante EA, Guess PC, Rekow ED, Thompson VP. (2009b). Fatigue testing of two porcelain-zirconia all-ceramic crown systems. Dent Mater 25:1122-1127 [DOI] [PubMed] [Google Scholar]
- Della Bona A, Kelly JR. (2008). The clinical success of all-ceramic restorations. J Am Dent Assoc 139(Suppl):8S-13S [DOI] [PubMed] [Google Scholar]
- DeLong R, Douglas WH. (1983). Development of an artificial oral environment for the testing of dental restoratives: bi-axial force and movement control. J Dent Res 62:32-36 [DOI] [PubMed] [Google Scholar]
- Deng Y, Lawn BR, Lloyd IK. (2002). Characterization of damage modes in dental ceramic bilayer structures. J Biomed Mater Res 63:137-145 [DOI] [PubMed] [Google Scholar]
- Donovan TE. (2009). Porcelain-fused-to-metal (PFM) alternatives. J Esthet Restor Dent 21:4-6 [DOI] [PubMed] [Google Scholar]
- Guess PC, Strub JR, Steinhart N, Wolkewitz M, Stappert CF. (2009). All-ceramic partial coverage restorations—Midterm results of a 5-year prospective clinical splitmouth study. J Dent 37:627-637 [DOI] [PubMed] [Google Scholar]
- Huang M, Thompson VP, Rekow ED, Soboyejo WO. (2007). Modeling of water absorption induced cracks in resin-based composite supported ceramic layer structures. J Biomed Mater Res 84:124-130 [DOI] [PubMed] [Google Scholar]
- Kelly JR. (1999). Clinically relevant approach to failure testing of all-ceramic restorations. J Prosthet Dent 81:652-661 [DOI] [PubMed] [Google Scholar]
- Kim B, Zhang Y, Pines M, Thompson VP. (2007). Fracture of porcelain-veneered structures in fatigue. J Dent Res 86:142-146 [DOI] [PubMed] [Google Scholar]
- Kim JH, Kim JW, Myoung SW, Pines M, Zhang Y. (2008). Damage maps for layered ceramics under simulated mastication. J Dent Res 87:671-675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JW, Kim JH, Thompson V, Zhang Y. (2007). Sliding contact damage in layered ceramic structures. J Dent Res 86:1046-1050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JW, Kim JH, Janal MN, Zhang Y. (2008). Damage maps of veneered zirconia under simulated mastication. J Dent Res 87:1127-1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohal RJ, Klaus G. (2004). A zirconia implant-crown system: a case report. Int J Periodontics Restorative Dent 24:147-153 [PubMed] [Google Scholar]
- Kohal RJ, Klaus G, Strub JR. (2006). Zirconia-implant-supported all-ceramic crowns withstand long-term load: a pilot investigation. Clin Oral Implants Res 17:565-571 [DOI] [PubMed] [Google Scholar]
- Larsson C, Vult von Steyern P, Sunzel B, Nilner K. (2006). All-ceramic two- to five-unit implant-supported reconstructions. A randomized, prospective clinical trial. Swed Dent J 30:45-53 [PubMed] [Google Scholar]
- Manicone PF, Rossi Iommetti P, Raffaelli L. (2007). An overview of zirconia ceramics: basic properties and clinical applications. J Dent 35:819-826 [DOI] [PubMed] [Google Scholar]
- Marchack BW, Futatsuki Y, Marchack CB, White SN. (2008). Customization of milled zirconia copings for all-ceramic crowns: a clinical report. J Prosthet Dent 99:169-173 [DOI] [PubMed] [Google Scholar]
- Marker JC, Goodkind RJ, Gerberich WW. (1986). The compressive strength of nonprecious versus precious ceramometal restorations with various frame designs. J Prosthet Dent 55:560-567 [DOI] [PubMed] [Google Scholar]
- McLaren EA, White SN. (1999). Glass-infiltrated zirconia/alumina-based ceramic for crowns and fixed partial dentures. Pract Periodontics Aesthet Dent 11:985-994 [PubMed] [Google Scholar]
- Molin MK, Karlsson SL. (2008). Five-year clinical prospective evaluation of zirconia-based Denzir 3-unit FPDs. Int J Prosthodont 21:223-227 [PubMed] [Google Scholar]
- Nelson W. (1990). Accelerated testing: statistical models, test plans, and data analysis. New York: John Wiley & Sons, Chapter 10, pp. 493-520 [Google Scholar]
- Okeson JP. (1998). Alignment and occlusion of the dentition. In: Management of temporomandibular disorders and occlusion. St. Louis, MO: CV Mosby, pp. 67-92 [Google Scholar]
- Panek H, Matthews-Brzozowska T, Nowakowska D, Panek B, Bielicki G, Makacewicz S, et al. (2008). Dynamic occlusions in natural permanent dentition. Quintessence Int 39:337-342 [PubMed] [Google Scholar]
- Quinn G. (2007). Fractography of ceramics and glasses. A NIST recommended practice guide; Special Publication 960-16. Washington, DC: National Institute of Standards and Technology; May 2007. http://www.ceramics.nist.gov/pubs/practice.htm (URL accessed 6/16/10). [Google Scholar]
- Raigrodski AJ, Chiche GJ, Potiket N, Hochstedler JL, Mohamed SE, Billiot S, et al. (2006). The efficacy of posterior three-unit zirconium-oxide-based ceramic fixed partial dental prostheses: a prospective clinical pilot study. J Prosthet Dent 96:237-244 [DOI] [PubMed] [Google Scholar]
- Rekow D, Thompson VP. (2007). Engineering long term clinical success of advanced ceramic prostheses. J Mater Sci Mater Med 18:47-56 [DOI] [PubMed] [Google Scholar]
- Rekow D, Zhang Y, Thompson V. (2007). Can material properties predict survival of all-ceramic posterior crowns? Compend Contin Educ Dent 28:362-368 [PubMed] [Google Scholar]
- Sailer I, Feher A, Filser F, Gauckler LJ, Luthy H, Hammerle CH. (2007a). Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont 20:383-388 [PubMed] [Google Scholar]
- Sailer I, Pjetursson BE, Zwahlen M, Hammerle CH. (2007b). A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part II: Fixed dental prostheses. Clin Oral Implants Res 18(Suppl 3):86-96 Erratum in Clin Oral Implants Res 19:326-328, 2008 [DOI] [PubMed] [Google Scholar]
- Scherrer SS, Quinn GD, Quinn JB. (2008). Fractographic failure analysis of a Procera AllCeram crown using stereo and scanning electron microscopy. Dent Mater 24:1107-1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelby DS. (1962). Practical considerations and design of the porcelain fused to metal. J Prosthet Dent 12:542-548 [Google Scholar]
- Silva NRFA, Sailer I, Zhang Y, Coelho PG, Guess PC, Zembic A, et al. (2010). Performance of Zirconia for Dental Healthcare. Materials 3:863-896 [Google Scholar]
- Swain MV. (2009). Unstable cracking (chipping) of veneering porcelain on all-ceramic dental crowns and fixed partial dentures. Acta Biomater 5:1668-1677 [DOI] [PubMed] [Google Scholar]
- Tinschert J, Schulze KA, Natt G, Latzke P, Heussen N, Spiekermann H. (2008). Clinical behavior of zirconia-based fixed partial dentures made of DC-Zirkon: 3-year results. Int J Prosthodont 21:217-222 [PubMed] [Google Scholar]
- Zhao W, Elsayed E. (2005). A general accelerated life model for step-stress testing. IEEE Trans Reliability 37:1059-1069 [Google Scholar]


