Abstract
Background
This study examined whether reductions in depression symptoms at different time points over the course of therapy predict remission for depressed adolescents treated with interpersonal psychotherapy (IPT-A) or treatment as usual (TAU) delivered in school-based health clinics.
Methods
Participants were 63 adolescents (ages 12–18) drawn from a randomized controlled clinical trial examining the effectiveness of IPT-A. [1] Adolescents were randomized to receive IPT-A or TAU delivered by school-based mental health clinicians. Assessments were completed at baseline and weeks 4, 8, 12, and 16 (or at early termination) and included the Hamilton Rating Scale for Depression (HRSD [2]).
Results
Receiver operating characteristic analysis was used to identify the time point and degree of reduction in HRSD that best predicted remission (HRSD < 7) at the end of the trial (week 16). Week 4 was the best time point for classifying adolescents as likely to remit or not likely to remit for both IPT-A and TAU. A 16.2% reduction in HRSD from baseline represented the best combined sensitivity and specificity in predicting week 16 remission status for adolescents treated with IPT-A. A 24.4% reduction in depressive symptoms represented the best combined sensitivity and specificity in predicting remission status for TAU.
Conclusions
These findings provide preliminary evidence of one early marker of remission with IPT-A. Replication with larger samples would suggest that depressed adolescents who have not demonstrated at least a 16.2% reduction in their depressive symptoms after 4 weeks of IPT-A may benefit from a change in the treatment plan.
Keywords: psychotherapy, treatment outcome, depressive disorder, adolescent
In the last two decades, substantial progress has been made in the development of efficacious treatments for adolescent depression. However, even when depressed adolescents receive the best treatments delivered under optimal circumstances, 30–50% still do not achieve remission.[3] In practice, this means that clinicians must continually adapt and readapt adolescents’ treatments by sequencing or combining different treatment approaches until remission is reached. With the exception of the TORDIA study which found that adolescents who had not responded to an initial treatment with an SSRI benefitted most from a switch to a different antidepressant and the addition of cognitive behavioral therapy,[4] there are currently no empirically-derived guidelines to direct clinicians in this process. As a consequence, clinicians often implement treatments in a trial and error fashion that could result in extended time to remission, unnecessary experience of side effects, increased cost or other burdens for adolescents and their families, and prolonged use of scarce clinician resources. The development of evidence-based guidelines for personalizing treatments to increase rates of remission and minimize burden has been identified as a public health priority. [5]
The goal of this study was to determine whether there are early indicators of acute treatment remission for adolescents with mild to moderate depression treated with 12 sessions of interpersonal psychotherapy (IPT-A) [6] or treatment as usual (TAU) delivered over the course of 16 weeks in school-based health clinics. If it were possible to determine early in treatment whether or not a depressed adolescent is likely to achieve remission by the end of the16 week treatment, this could inform clinicians’ decisions to continue the initial treatment past a certain number of weeks or alter the treatment plan.
We focus on early patterns of change in depressive symptoms for two reasons. First, attempts at predicting treatment response from patient demographics or pre-treatment clinical characteristics have yielded mixed results. Most demographic variables have not been found to predict treatment outcome. [7–12] Some studies have found that pre-treatment depression severity and general functioning predict treatment outcome, but the results have not been consistent. [7–9; 11; 12] Second, several previous studies have found early symptom change to predict treatment response. [9; 13–17] A study of cognitive, family, and supportive psychotherapies for adolescent major depressive disorder (MDD) found that adolescents who had demonstrated at least a 50% reduction in self-reported depression symptoms by the second therapy session were significantly more likely to achieve remission at the end of acute treatment and have lower rates of MDD at the 1 year follow-up.[17] Another study found that a 50% reduction in adolescents’ depressive symptoms by week 4 of treatment with fluoxetine predicted remission status at the end of the 12 week treatment.[9] Treatment studies of adult depression have also found that early treatment response predicts treatment outcome, though the time point and criteria for classifying a patient as an early responder have varied.[13; 15; 16]
The majority of the studies that examined early prediction of treatment response used pre-determined and non-empirically-derived criteria for categorizing a patient as an early responder (e.g. a patient is an early rapid responder if he or she demonstrates a 50% reduction in symptoms by week 2 [17]). These studies have provided important information about the ability of early symptom reduction to predict acute treatment outcome. However, there is little empirical data to guide clinicians in knowing how much of a reduction is needed and by what time point to evaluate whether remission by the end of acute treatment is likely. In this study, we use the data from an effectiveness study of IPT-A to empirically determine the optimal depression reduction criterion and time point that best predicts remission at the end of 16 weeks of IPT-A and TAU. We also examined the accuracy of baseline levels of depression for predicting remission status since there have been some studies that have found pre-treatment depression severity to be a significant predictor.
Materials and Methods
Participants
Sixty-three adolescents (ages 12–18 years) participated in a previously published randomized controlled clinical trial examining the effectiveness of IPT-A as compared to treatment as usual in five school-based health clinics in New York City. [1] Inclusion criteria included Hamilton Rating Scale for Depression (HRSD) ≥ 10 [2; 18]; Children’s Global Assessment Scale (CGAS) ≤ 65 [19]; and a DSM-IV diagnosis of major depression, dysthymia, depressive disorder NOS, or adjustment disorder with depressed mood. Adolescents were excluded from participation if they had been diagnosed with mental retardation, were actively suicidal, in current treatment for depression, or taking antidepressant medication. They were also excluded if they had a life-threatening medical illness, psychosis, schizophrenia, or a substance-related disorder. Three schools included only English speaking students, and two schools included both English and monolingual Spanish-speaking students. Informed consent and assent were obtained from parents or legal guardians and adolescents. The institutional review boards for the three hospitals that sponsored the school-based clinics and the New York City Department of Education approved the study. See Mufson et al. [1] for a complete description of the trial and CONSORT flow chart.
Adolescents were 84.1% female and 15.9% male (mean age = 14.7). Adolescents came primarily from low-income families and were 74.6% Latino, 14.3% African American, 1.6% Asian American, and 9.5% other. Depression diagnoses were assessed using the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS) [20]. 50.8% of adolescents were diagnosed with major depressive disorder, 17.5% with dysthymic disorder, 6.3% with double depression, 11.1% with depressive disorder NOS, and 14.3% with adjustment disorder with depressed mood. Comorbid diagnoses were assessed using the Diagnostic Interview Schedule for Children Predictive Scales (DPS) [21] and clinical interview. 32.0% reported symptoms indicative of an anxiety disorder, 8.0% oppositional defiant disorder, and 6.0% attention-deficit/hyperactivity disorder. For a complete sample description and explanation of attrition, see Mufson et al. [1].
Treatment
Adolescents were randomized to receive IPT-A or TAU, both delivered by mental health clinicians in school-based health clinics. Monolingual Spanish-speaking adolescents participated in therapy with a bilingual clinician. IPT-A [6] is a 12 session psychotherapy adapted from IPT for adults.[22] The goal of IPT-A is to decrease depressive symptoms by focusing on current interpersonal difficulties and helping the individual improve his or her relationships and interpersonal interactions. This is accomplished through psychoeducation about the adolescent’s depression and its link to interpersonal relationships, review of the adolescent’s significant relationships, identification of interpersonal problem areas on which to focus the treatment, development of interpersonal problem solving and communication skills, and role-playing. In clinical trials, depressed adolescents treated with IPT-A demonstrated fewer depressive symptoms, better social functioning, and better global functioning at the completion of treatment than adolescents in control conditions. [1; 23; 24] Sessions lasted 35 minutes and were held weekly for 8 weeks, with the remaining 4 sessions scheduled at any frequency over the following 8 weeks.
TAU was whatever psychological treatment the adolescent would have received in the school-based clinic if the study had not occurred. Most adolescents received weekly individual supportive psychotherapy. Eight adolescents also received one to three family/parent sessions, and five adolescents participated in group therapy. The majority of TAU therapists characterized their theoretical orientation as psychodynamic. At the completion of each TAU therapy session, therapists completed the Therapeutic Procedures Inventory [25], a checklist of commonly used psychotherapy techniques. The most common treatment strategies endorsed were gaining a better understanding of the patient, establishing a genuine person-to-person rapport with the patient, and helping the patient talk about feelings and concerns.
Six subjects dropped out prior to study completion (4 in IPT-A and 2 in TAU). Study completers did not significantly differ from study dropouts on any of the baseline measures. For a complete description of attrition, treatment adherence, clinician characteristics, and treatment fidelity, see Mufson et al.[1]
Measures
Assessments were conducted at baseline and weeks 4, 8, 12, and 16 or at early termination by a psychologist or social worker blind to the adolescent’s treatment condition. Monolingual Spanish-speaking adolescents were evaluated by bilingual clinicians and they completed questionnaires that were translated into Spanish by research staff of the same Latino heritage and back translated to insure accuracy. The week 16 assessment was conducted by telephone. A study comparing patients’ responses on the structured interview version of the Hamilton Rating Scale for Depression when administered by telephone as compared to in person found that there were no significant differences in scores based on mode of administration.[26]
Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS)
The K-SADS [20] is a clinician-administered semi-structured interview that assesses current episode and lifetime history of psychiatric diagnoses based on DSM-IV criteria. In this study, only the depression module-child report was used. Inter-rater reliability among the independent evaluators was .76.
Hamilton Rating Scale for Depression (HRSD)
The HRSD [2; 18] is a clinician-administered semi-structured interview that assesses depression symptom severity. It was originally designed for use with adults, but is widely used with adolescents, as well [27]. It has strong internal reliability and inter-rater reliability when used with adolescents. [28] Inter-rater reliability for the current sample was .84, and internal reliability (Chronbach’s alpha) was .74. Depression remission was defined as HRSD < 7. [2] See Table 1 for descriptive statistics of the HRSD at each time point.
Table 1.
Adolescents’ Mean HRSD Scores and Percent Reduction in HRSD Scores at Each Time Point
| Variable | IPT-A Mean (SD) | TAU Mean (SD) |
|---|---|---|
| Baseline score | 14.18 (4.50) | 13.83 (3.76) |
| Week 4 score | 10.85 (5.35) | 11.41 (5.22) |
| Week 8 score | 8.12 (5.96) | 9.66 (5.09) |
| Week 12 score | 7.15 (6.25) | 9.52 (6.05) |
| Week 16 score | 5.88 (5.96) | 8.28 (5.59) |
| Percent reduction at week 4 | 21.90 (36.47) | 18.31 (34.01) |
| Percent reduction at week 8 | 43.48 (37.92) | 29.50 (33.87) |
| Percent reduction at week 12 | 49.16 (38.49) | 27.31 (49.74) |
| Number of adolescents remitted at week 16 | 22 (64.71%) | 12 (41.1%) |
Note: Remission defined as HRSD < 7. Means differ from those reported in Mufson et al. [1] because this paper reports total scores based on the 17 item HRSD rather than the 24 item HRSD.
Analytic Strategy
All analyses were conducted on the intent-to-treat sample. Missing data was replaced using multiple imputation [29]. Receiver operating characteristic (ROC) analysis was used to identify the time point and degree of reduction in HRSD that best predicts remission at week 16 for each of the treatment conditions. ROC analysis provides plots of the estimates of the probability of a true positive result (sensitivity) and the probability of a true nonresponse (1 – specificity) at different cutoff values of the predictor variable (in this case, baseline HRSD or percent reduction in HRSD at subsequent time points). By examining the plot, it is possible to select a percent reduction in HRSD cutoff value that optimizes sensitivity and specificity. In addition, the ROC analysis includes an estimate of the area under the ROC curve (AUC) which provides an indication of classification accuracy (remitter versus nonremitter) for each assessment week (baseline, 4, 8, and 12). An AUC can range from .50 to 1. An AUC of .50 indicates chance levels of discrimination. An AUC of 1 indicates perfect discrimination of remitters from nonremitters. A ROC analysis was conducted for baseline and weeks 4, 8, and 12. By comparing the AUCs for each time point, it is possible to select the time point that provides the best prediction of remission. Once the time point is selected, the ROC curve for that time point is examined to determine the percent reduction in HRSD that maximizes sensitivity and specificity.
Results
IPT-A
As shown in Table 2, in the IPT-A treatment condition, the AUC for baseline HRSD scores was much smaller than the AUCs for all three of the subsequent time points. This indicates that baseline depression severity is a less accurate classifier of post-treatment remission status than the degree of reduction in symptoms once treatment with IPT-A has started. The AUCs for weeks 4, 8, and 12 were very similar and there was overlap in their confidence intervals. This suggests that waiting until week 8 or week 12 to predict remission rather than predicting remission at week 4 did not meaningfully increase the ability to discriminate remitters from nonremitters. Consequently, week 4 was selected as the time point for classifying adolescents as likely to remit or not likely to remit in order to minimize the time that adolescents who were not likely to remit continued with a treatment plan that was not likely to lead to remission by week 16.
Table 2.
Receiver Operating Characteristic Analysis for IPT-A: Area under the Curve for Baseline HRSD Score and Percent Reduction in HRSD Score at Week 4, 8, and 12 Relative to Week16 Remission Status
| Time Point | AUC | SE | p value | 95% Confidence Interval for AUC |
|---|---|---|---|---|
| Baseline | .34 | .10 | .12 | .14 – .53 |
| Week 4 reduction | .78 | .08 | .01 | .63 – .94 |
| Week 8 reduction | .81 | .08 | .00 | .66 – .97 |
| Week 12 reduction | .89 | .06 | .00 | .78 – 1.00 |
Figure 1 presents the combined sensitivity and specificity of percent reduction in baseline HRSD at week 4 relative to remission status at week 16. The ROC analysis determined that a cutoff of 16.2% reduction in HRSD from baseline represented the best combined sensitivity (72.7%) and specificity (71.4%). That is, 72.7% of the adolescents who remitted by week 16 showed at least a 16.2% reduction in their HRSD scores at week 4, and 71.4% of the adolescents who did not achieve remission by week 16 had less than a 16.2% reduction in HRSD at week 4.
Figure 1.
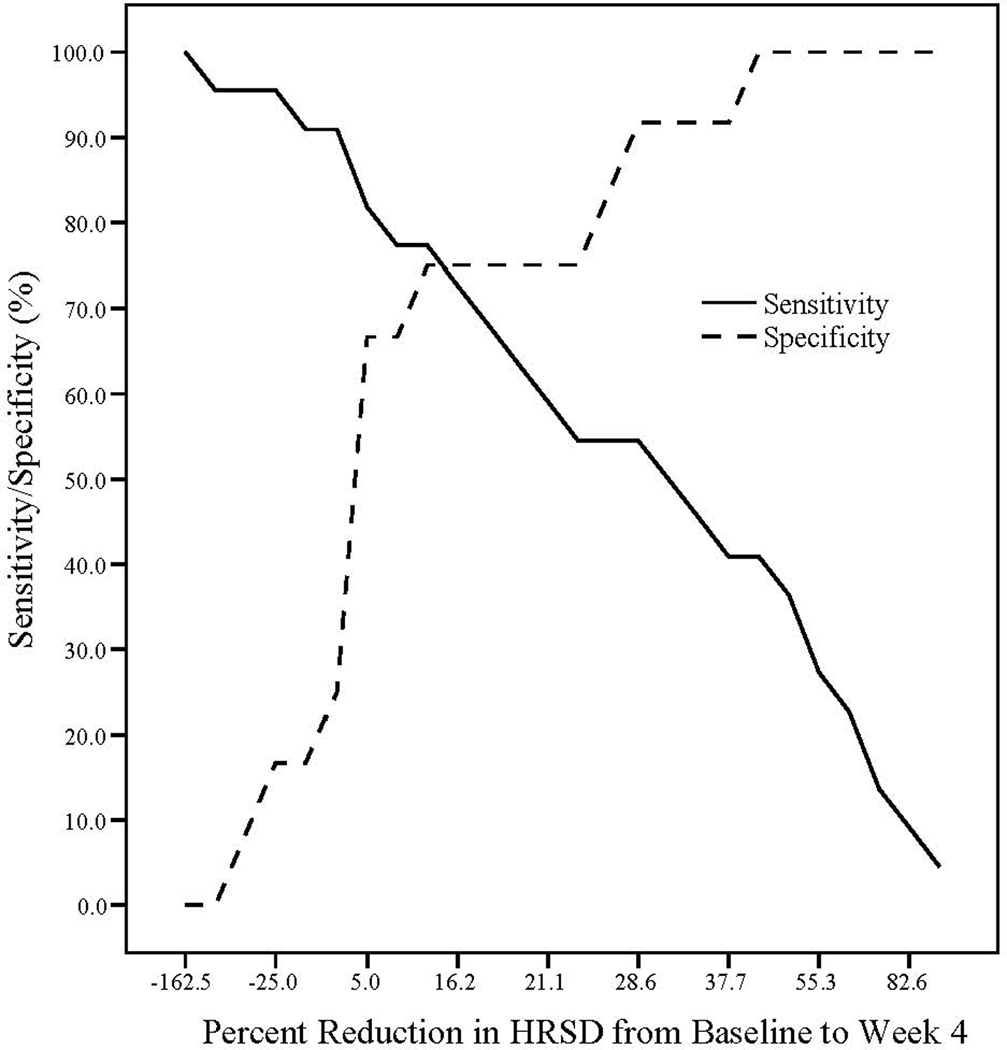
IPT-A: Sensitivity and Specificity Associated with Percent Reduction in HRSD at week 4 Relative to Remission status at Week 16.
Note. A negative percent indicates an increase in HRSD from baseline to week 4.
TAU
The results of the ROC analyses for the TAU condition are shown in Table 3. As with IPT-A, baseline HRSD was not an accurate classifier of post-treatment remission status for adolescents treated with TAU. The most accurate predictor of remission was improvement in depression symptoms at week 12. However, given that this time point was just 4 weeks away from the end of treatment, it did not seem to be a useful classifier. The AUCs for week 4 and week 8 both approached statistical significance and were comparable in magnitude. Week 4 was selected as the best time point for classifying an adolescent as likely to remit or not likely to remit with TAU in order to minimize the time that adolescents continued with a treatment plan that was not likely to lead to remission. As illustrated in Figure 2, a cutoff of 24.4% reduction in HRSD from baseline to week 4 represented the best combined sensitivity (66.7%) and specificity (64.7%). That is, 66.7% of the adolescents who remitted by week 16 showed at least a 24.4% reduction in their HRSD scores at week 4, and 64.7% of the adolescents who did not achieve remission by week 16 had less than a 24.4% reduction in HRSD at week 4.
Table 3.
Receiver Operating Characteristic Analysis for TAU: Area under the Curve for Baseline HRSD Score and Percent Reduction in HRSD Score at Week 4, 8, and 12 Relative to Week16 Remission Status
| Time Point | AUC | SE | p value | 95% Confidence Interval for AUC |
|---|---|---|---|---|
| Baseline | .42 | .11 | .49 | .21 – .64 |
| Week 4 reduction | .71 | .10 | .06 | .51 – .90 |
| Week 8 reduction | .70 | .10 | .07 | .50 – .91 |
| Week 12 reduction | .91 | .06 | .00 | .00 – 1.00 |
Figure 2.
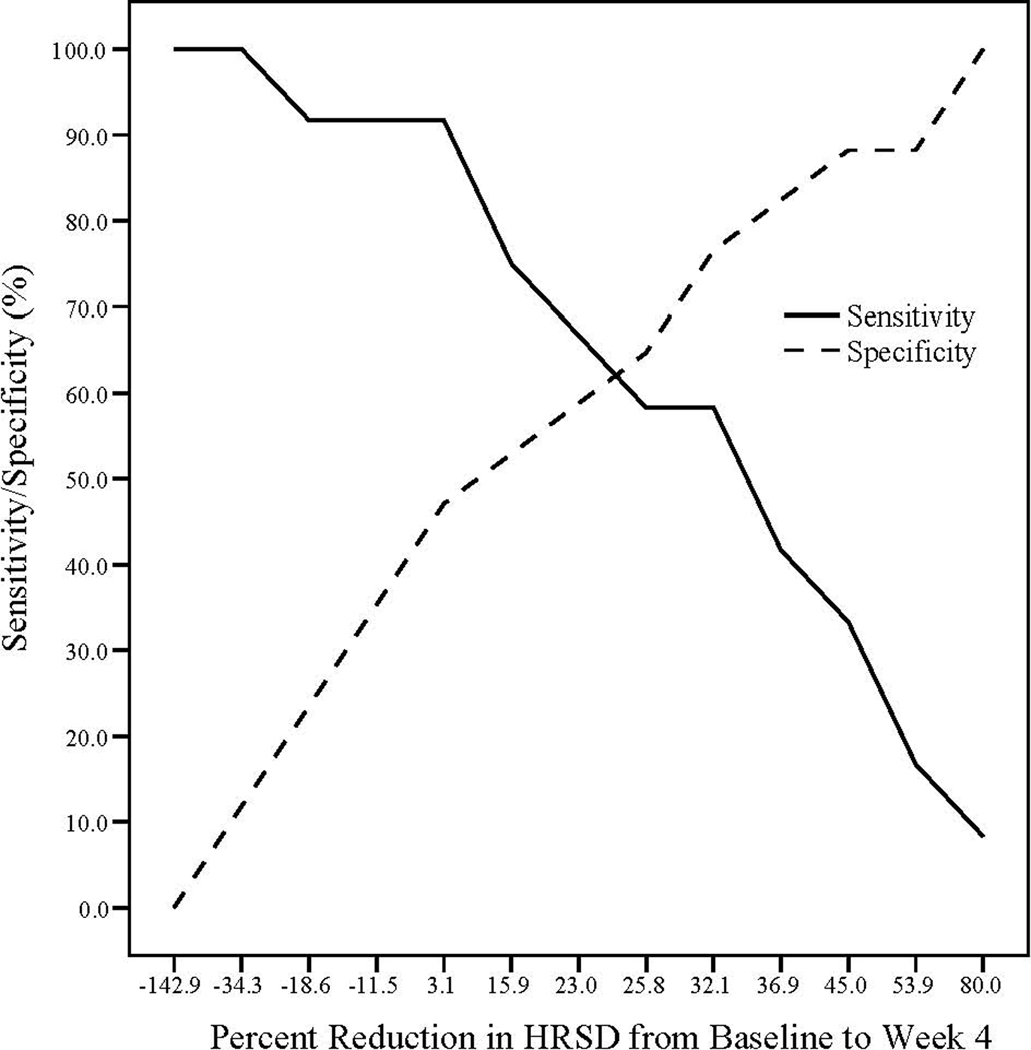
TAU: Sensitivity and Specificity Associated with Percent Reduction in HRSD at week 4 Relative to Remission status at Week 16.
Note. A negative percent indicates an increase in HRSD from baseline to week 4.
Discussion
We examined whether early patterns of improvement in depression symptoms predicted remission at the end of acute treatment with IPT-A and TAU. Baseline levels of depression did not accurately distinguish the adolescents who remitted from those who did not in either treatment condition. However, adolescents’ remission status was predicted from symptom reductions during the early weeks of treatment. Depressed adolescents treated with IPT-A who demonstrated at least a 16.2% reduction in HRSD scores at week 4 had a strong chance of achieving remission at the end of 16 weeks of treatment. Adolescents who did not demonstrate at least a 16.2% reduction in their depressive symptoms were unlikely to reach remission by week 16 and therefore may have benefitted from a change in the treatment plan. Week 4 was also the most useful time point for predicting remission status for adolescents treated with TAU, though the findings were less robust. A greater degree of reduction in depression symptoms was needed by week 4 for adolescents receiving TAU than for adolescents treated with IPT-A. Adolescents treated with TAU who did not demonstrate at least a 24.4% reduction in their depressive symptoms were less likely to reach remission by the end of treatment. The results of this study should be considered preliminary, given the small sample size. However, the AUC for the week 4 time point for IPT-A was relatively robust, despite the small sample size, which suggests that it is worth investigation in larger prospective studies.
The findings from this study are consistent with previous studies that have found that early improvements in depression symptoms predict treatment outcome. [9; 13–17] Our study found that only a relatively small improvement in depression symptoms is needed to signal that remission will be likely. This differs from much of the current literature that has documented that remission is predicted by a 50–60% reduction in symptoms. This may be at least in part due to the fact that many of the previous studies used predefined criteria for characterizing an early treatment response rather than letting the data indicate the percent reduction in symptoms that best predicts remission. While a 16% reduction in symptoms at week 4 of IPT-A treatment is probably not sufficient improvement to be classified as a treatment response, we suggest that it may be a signal that remission with the full course of IPT-A is likely. For a patient with moderate depression, a 16% reduction in HRSD scores represents a decrease of 3–4 points. If the therapist is using the most recent version of the Hamilton (GRID-HAMD [30]) which provides good rating anchors that take into account both the severity and frequency of each symptom, and has strong interrater reliability and concurrent validity, therapists should be able to feel confident about their assessment of a decrease of 3–4 points.
As clinician investigators, we do not yet know what the change in treatment plan should be for depressed adolescents who have not shown sufficient improvement with 4 weeks of psychotherapy. Options include increasing the number of psychotherapy sessions, switching to a different psychotherapy, or adding medication. Two previous studies have found that increasing the number of psychotherapy sessions increases response rates for patients receiving only psychotherapy. [31; 32] Three out of five randomized controlled trials of psychotherapy plus medication versus psychotherapy alone and/or medication alone found that depressed adolescents who received the combined treatment had the greatest reductions in depressive symptoms. [4; 33–36] Future studies are needed to examine the efficacy of increasing the number of psychotherapy sessions, adding antidepressant medication, or switching to a different psychotherapeutic modality for depressed adolescents who have shown an insufficient response to an initial dose of psychotherapy.
The primary limitation of this study is the small sample size. Future studies with larger samples are needed to determine if the findings are replicable. Larger samples would also permit the assessment of the predictive value of early patterns of symptom change for subgroups of depressed adolescents receiving IPT-A. Our sample was of insufficient size to determine if the decrease in HRSD needed to predict remission differs based on patient characteristics such as the severity of pre-treatment depression symptoms or the presence of a comorbid diagnosis. Future studies are also needed to assess whether this early marker of treatment remission generalizes to adolescents receiving other kinds of treatments for depression.
The study’s sample consisted primarily of low-income Hispanic females living in an urban setting. The number of male adolescents in the sample is smaller than what might be expected based on the prevalence rates documented in epidemiological studies [37]. We understand our sample characteristics to be primarily due to patterns in treatment-seeking behavior. Adolescent girls have more positive help-seeking attitudes and lower perceived barriers to initiating treatment than male adolescents. [38; 39] Our study extends the treatment literature to an understudied, underserved population; however, we do not know if the results are generalizable to other populations of depressed adolescents.
Conclusion
If replicated with larger samples, the results of this study have the potential to have significant implications for clinical practice. First, they provide an impetus for thinking about treatment response early on in clinical practice with a depressed adolescent, as early patterns of symptom change may signal whether a modification in the treatment plan may be warranted. An early signal that a change in treatment approach is needed could increase chances of reaching remission and minimize time spent in a treatment that is not likely to have the desired clinical outcome. It could also potentially lead to lower rates of treatment drop-out, given that many families discontinue treatment because they perceive a lack of benefit with treatment. [40]
Second, the findings have implications for the use of standardized and validated depression measures during the treatment process. Clinicians’ predictions of patients’ ultimate treatment outcomes tend to be quite inaccurate when based on clinical judgment alone. [41; 42] Change in depression symptoms, as assessed with the HRSD predicted treatment remission with a relatively high level of accuracy. The newest version of the HRSD, the GRID-HAMD [30], is a free and relatively brief instrument that has strong interrater reliability and concurrent validity, and with training, can be administered reliably in community settings. [26] Future studies may identify other additional instruments that may be used to predict treatment response.
Acknowledgements
This research was supported by grants 6HS5SM52671-02-1 (L. Mufson, P.I.) from the Substance Abuse and Mental Health Services Administration, K23MH090216 (M. Gunlicks-Stoessel, P.I.) from the National Institute of Mental Health, and a Research Associate Award (M. Gunlicks-Stoessel, P.I.) from Research Foundation for Mental Hygiene, Inc.
References
- 1.Mufson L, Dorta KP, Wickramaratne P, et al. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry. 2004;61:577–584. doi: 10.1001/archpsyc.61.6.577. [DOI] [PubMed] [Google Scholar]
- 2.Hamilton M. Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 3.TADS Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents with Depression Study (TADS) randomized controlled trial. Journal of the American Medical Association. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- 4.Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: The TORDIA randomized controlled clinical trial. Journal of the American Medical Association. 2008;299:901–913. doi: 10.1001/jama.299.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Insel TR. Translating scientific opportunity Into public health impact: A strategic plan for research on mental illness. Archives of General Psychiatry. 2009;66:128–133. doi: 10.1001/archgenpsychiatry.2008.540. [DOI] [PubMed] [Google Scholar]
- 6.Mufson L, Dorta KP, Moreau D, Weissman MM. Interpersonal psychotherapy for depressed adolescents. New York: Guilford Press; 2004. [Google Scholar]
- 7.Asarnow JR, Emslie G, Clarke G, et al. Treatment of selective serotonin reuptake inhibitor-resistant depression in adolescents: Predictors and moderators of treatment response. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:330–339. doi: 10.1097/CHI.0b013e3181977476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brent DA, Kolko DJ, Birmaher B, et al. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:906–914. doi: 10.1097/00004583-199809000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Tao R, Emslie G, Mayes T, et al. Early prediction of acute antidepressant treatment response and remission in pediatric major depressive disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:71–78. doi: 10.1097/CHI.0b013e318190043e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin. 2006;132:132–149. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curry J, Rohde P, Simons A, et al. Predictors and moderators of acute outcome in the Treatment for Adolescents with Depression Study (TADS) Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:1427–1439. doi: 10.1097/01.chi.0000240838.78984.e2. [DOI] [PubMed] [Google Scholar]
- 12.Kowatch RA, Carmody TJ, Emslie GJ, et al. Prediction of response to fluoxetine and placebo in children and adolescents with major depression: A hypothesis generating study. Journal of Affective Disorders. 1999;54:269–276. doi: 10.1016/s0165-0327(98)00205-5. [DOI] [PubMed] [Google Scholar]
- 13.Crits-Christoph P, Connolly M, Gallop R, et al. Early improvement during manual-guided cognitive and dynamic psychotherapies predicts 16-week remission status. Journal of Psychotherapy Practice and Research. 2001;10:145–154. [PMC free article] [PubMed] [Google Scholar]
- 14.Emslie GJ, Mayes T, Porta G, et al. Treatment of Resistant Depression in Adolescents (TORDIA): Week 24 outcome. American Journal of Psychiatry. 2010;167:782–791. doi: 10.1176/appi.ajp.2010.09040552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hayes AM, Feldman GC, Beevers CG, et al. Discontinuities and cognitive changes in an exposure-based cognitive therapy for depression. Journal of Consulting and Clinical Psychology. 2007;75:409–421. doi: 10.1037/0022-006X.75.3.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Papakostas GI, Petersen T, Sklarsky KG, et al. Timing of clinical improvement and symptom resolution in the treatment of major depressive disorder. Psychiatry Research. 2007;149:195–200. doi: 10.1016/j.psychres.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 17.Renaud J, Brent DA, Baugher M, et al. Rapid response to psychosocial treatment for adolescent depression: A two-year follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1184–1190. doi: 10.1097/00004583-199811000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Williams JB. A structured interview guide for the Hamilton Depression Rating Scales. Archives of General Psychiatry. 1988;45:742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- 19.Shaffer D, Gould MS, Brasic J, et al. A children's Global Assessment Scale (CGAS) Archives of General Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 20.Chaput F, Fisher P, Klein R, et al. Columbia K-SADS (Schedule for Affective Disorders and Schizophrenia for School-aged Children) New York: Child Psychiatry Intervention Research Center, New York State Psychiatric Institute; 1999. [Google Scholar]
- 21.Lucas CP, Zhangh H, Fisher PW, et al. The DISC Predictive Scales (DPS): efficiently screening for diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:443–449. doi: 10.1097/00004583-200104000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Weissman MM, Markowitz JC, Klerman GL. Comprehensive guide to interpersonal psychotherapy. New York: Basic Books; 2000. [Google Scholar]
- 23.Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry. 1999;56:573–579. doi: 10.1001/archpsyc.56.6.573. [DOI] [PubMed] [Google Scholar]
- 24.Rossello Jb, Bernal G. The efficacy of cognitive-behavioral and interpersonal treatments for depression in Puerto Rican adolescents. Journal of Consulting and Clinical Psychology. 1999;67:734–745. doi: 10.1037//0022-006x.67.5.734. [DOI] [PubMed] [Google Scholar]
- 25.McNeilly CL, Howard KI. The Therapeutic Procedures Inventory: Psychometric properties and relationship to phase of treatment. Journal of Psychotherapy Integration. 1991;1:223–234. [Google Scholar]
- 26.Potts MK, Daniels M, Burnam MA, Wells KB. A structured interview version of the Hamilton Depression Rating Scale: Evidence of reliability and versatility of administration. Journal of Psychiatric Research. 1990;24:335–350. doi: 10.1016/0022-3956(90)90005-b. [DOI] [PubMed] [Google Scholar]
- 27.Meyers K, Winters NC. Ten-year review of rating scales II: Scales for internalizing disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:634–659. doi: 10.1097/00004583-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Robbins DR, Alessi NE, Colfer MV, Yanchyshyn GW. Use of the Hamilton Rating Scale for Depression and the Carroll Self-Rating Scale in adolescents. Psychiatry Research. 1985;14:123–129. doi: 10.1016/0165-1781(85)90056-3. [DOI] [PubMed] [Google Scholar]
- 29.Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. [Google Scholar]
- 30.Williams JB, Kobak KA, Bechg P, et al. The GRID-HAMD: Standardization of the Hamilton Depression Rating Scale. International Clinical Psychopharmacology. 2008;23:120–129. doi: 10.1097/YIC.0b013e3282f948f5. [DOI] [PubMed] [Google Scholar]
- 31.Clarke G, Rohde P, Lewinsohn P, et al. Cognitive-behavioral treatment of adolescent depression: Efficacy of acute group treatment and booster sessions. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:272–279. doi: 10.1097/00004583-199903000-00014. [DOI] [PubMed] [Google Scholar]
- 32.TADS Team. The Treatment for Adolescents with Depression Study (TADS): Long-term effectiveness and safety outcomes. Archives of General Psychiatry. 2007;64:1132–1144. doi: 10.1001/archpsyc.64.10.1132. [DOI] [PubMed] [Google Scholar]
- 33.Clarke GN, Debar L, Lynch F, et al. A randomized effectiveness trial of brief cognitive-behavioral therapy for depressed adolescents receiving antidepressant medication. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:888–898. [PubMed] [Google Scholar]
- 34.Goodyer IM, Dubicka B, Wilkinson P, et al. Selective serotonin reuptake inhibitors (SSRIs) and routine specialist care with and without cognitive behaviour therapy in adolescents with major depression: Randomised controlled trial. British Medical Journal. 2007 doi: 10.1136/bmj.39224.494340.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Melvin GA, Tonge BJ, King NJ, et al. A comparison of cognitive-behavioral therapy, sertraline, and their combination for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:1151–1161. doi: 10.1097/01.chi.0000233157.21925.71. [DOI] [PubMed] [Google Scholar]
- 36.TADS Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression. Journal of the American Medical Association. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- 37.Lewinsohn PM, Hops H, Roberts RE, et al. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- 38.Sen B. Adolescent propensity for depressed mood and help seeking: Race and gender differences. Journal of Mental Health Policy and Economics. 2004;7:133–145. [PubMed] [Google Scholar]
- 39.Kuhl J, Jarkon-Horlick L, Morrissey RF. Measuring barriers to help-seeking behavior in adolescents. Journal of Youth and Adolescence. 1997;26:637–650. [Google Scholar]
- 40.Kazdin AE. Dropping out of child therapy: Issues for research and implications for practice. Clinical Child Psychology and Psychiatry. 1996;1:133–156. [Google Scholar]
- 41.Hannan C, Lambert MJ, Harmon C, et al. A lab test and algorithms for identifying cases at risk for treatment failure. Journal of Clinical Psychology. 2005;61:155–163. doi: 10.1002/jclp.20108. [DOI] [PubMed] [Google Scholar]
- 42.Grove WM, Meehl PE. Comparative efficiency of informal (subjective, impressionistic) and formal (mechanical, algorithmic) prediction procedures: The clinical-statistical controversy. Psychology, Public Policy, and Law. 1996;2:293–323. [Google Scholar]


