Abstract
Background
Recent reports have suggested a close relationship between education and health, including mortality, in the United States.
Study Design
Observational cohort
Setting and Participants
We studied 61,457 participants enrolled in a national health screening initiative, the National Kidney Foundation’s Kidney Early Evaluation Program (KEEP).
Predictor
Self-reported educational attainment
Outcomes
Chronic diseases (hypertension, diabetes, cardiovascular disease, reduced kidney function, and albuminuria) and mortality
Measurements
We evaluated the cross-sectional associations between self-reported educational attainment with the chronic diseases listed above using logistic regression models adjusted for demographics, access to care, behaviors, and co-morbidities. The association of educational attainment with survival was determined by multivariable Cox proportional hazards regression.
Results
Higher educational attainment was associated with lower prevalence of each of the chronic conditions listed above. In multivariable models, compared with persons not completing high school, college graduates had a lower risk of each chronic condition, ranging from 11% lower odds of reduced kidney function to 37% lower odds of cardiovascular disease. Over a mean follow-up time of 3.9 years (median, 3.7 years), 2,384 (4%) deaths occurred. In the fully adjusted Cox model, those who had completed college had a 24% lower mortality, compared to participants who had completed at least some high school.
Limitations
A lack of income data does not allow us to disentangle the independent effects of education from income.
Conclusions
In this diverse, contemporary cohort, higher educational attainment was independently associated with lower prevalence of chronic diseases and short-term mortality among all age and race/ethnicity groups.
Keywords: education, mortality, chronic kidney disease
Socioeconomic inequalities in health status and life expectancy have been documented for decades in the United States. In a landmark study, Kitagawa and Hauser described educational disparities in mortality beginning in the 1960s; since then a large number of studies have documented educational gaps associated with worse health outcomes.1–3 Recent studies that have examined longitudinal trends in social inequalities have raised the concern that education-related gaps in life expectancy appear to have widened. These reports have provided the basis for national programs to eliminate health disparities in the United States such as Healthy People 2010.4
Whereas the 1980s and 1990s were periods of improvement in overall life expectancy and educational attainment in the general population,5–6 survival improvements did not occur evenly across education groups.7–8 There was little change in median survival among less-educated blacks and whites, compared with substantial increases in life expectancy among the more educated. The widening of these inequalities has occurred largely because of a greater decline in heart disease mortality among higher versus lower socioeconomic groups.9
Although education is generally believed to be associated with improved health, several important gaps in our knowledge exist. The majority of studies in this area have focused on white and black race, while Hispanic and Asian populations have been poorly represented. Hispanics are a rapidly growing segment of the US population, and only 45-75% of Hispanics have completed high school; thus, the health implications of educational attainment in this subgroup require evaluation.5 Furthermore, while the United States government has invested heavily in programs such as the Healthy People 2010 initiative and the expansion of Medicaid to improve the health of disadvantaged populations, no recent studies have provided information to assess the current state of varying levels of educational attainment and health status, and thereby the potential impact of recent efforts to close the gap. Finally, few prior studies accounted for individual-level clinical information, which may confound the association between education and health.
We conducted this study to determine the association between educational attainment with chronic diseases and survival in a national sample of participants of a health screening program. We hypothesized that higher education would be associated with lower mortality risk, particularly among ethnic minorities and younger adults, and that these findings would be mediated by a lower prevalence of chronic diseases.
Methods
Participants
We conducted an analysis among participants of the Kidney Early Evaluation Program (KEEP), a free, nationwide, community-based screening program implemented by the National Kidney Foundation in 2000 to increase awareness of kidney and other chronic diseases and to improve outcomes through early detection and referral for care.10 KEEP targets adults with a history of diabetes or hypertension, or persons with a first-order relative with diabetes, hypertension, or kidney disease; further KEEP recruitment and screening methods have been previously described.11
All individuals aged 18 years or greater participating in KEEP with complete clinical data were eligible for our study. The study enrolled 89,622 individuals in 49 states in the period from August 2000 to December 2007.12 We excluded those with missing education information (n=1,435), individuals with a history of kidney transplant or receipt of chronic dialysis therapy (n=146), participants with missing creatinine or albuminuria testing (n=13,634) or other clinical measurements (n=12,950). The total number of participants included in our study was 61,457.
Variables
The primary predictor variable was the highest level of self-reported educational attainment categorized as: (1) high school or less, (2) high school graduate, (3) some college, (4) college graduate or greater. Covariates such as sociodemographic characteristics and medical information were used for multivariable adjustment, and were obtained by staff- administered screening questionnaires, laboratory testing, and physical examination.11 Health-related behaviors and diagnosed conditions were defined as: family history of kidney disease; insurance coverage (public, private, neither or both); access to a doctor (determined by a response to the question, “Do you have a doctor?”); hypertension (self-reported diagnosis, receiving medication for high blood pressure, or systolic blood pressure ≥140mmHg or diastolic blood pressure ≥90mmHg); diabetes (self-reported diagnosis, a fasting glucose of ≥126 mg/dL, or a non-fasting glucose of ≥200 mg/dL); prevalent cardiovascular disease ([CVD]; heart attack or stroke); smoking (current or past); obesity (body mass index >30kg/m2); reduced kidney function (estimated glomerular filtration rate [eGFR] <60mL/min/1.73m2); and albuminuria (albumin-creatinine ratio [ACR] ≥30mg/g). Kidney function was calculated using the 4-variable, IDMS-traceable Modification of Diet in Renal Disease (MDRD) Study equation.13
Outcomes
Cross-sectional outcomes included hypertension, diabetes, cardiovascular disease, smoking, obesity, reduced kidney function, and albuminuria. The longitudinal outcome was all-cause mortality. Vital status was obtained by linkage to the National Death Index through May 31, 2009. Cause of death information was not available.
StatisticalAnalysis
We compared baseline characteristics by education level using ANOVA for continuous variables and chi-square tests for categorical or dichotomous variables (Table 1). We calculated the prevalence of chronic diseases by category of educational attainment. We next evaluated the cross-sectional associations of education level with the following outcomes: hypertension, diabetes, cardiovascular disease, smoking, obesity, reduced kidney function, and albuminuria. We used multivariate logistic regression models adjusted for demographic information, behaviors, and chronic diseases, with the referent group being “high school or less.”
Table 1.
Baseline Characteristics by Educational Level*
| Educational Level | |||||
|---|---|---|---|---|---|
| High school or less | High school graduate | Some college | 4-year college graduate or greater | P value | |
| No. | 8,540 (14) | 15,969 (26) | 16,216 (26) | 20,732 (34) | |
| Age | 58.3 +/− 17 | 56.2+/− 15 | 52.3 +/− 16 | 52.0 +/− 15 | <0.001 |
| Women | 5,661 (66) | 11,074 (69) | 11,464 (71) | 13,595 (66) | <0.001 |
| Race | <0.001 | ||||
| White | 2,741 (32) | 8,450 (53) | 7,674 (47) | 10,010 (48) | |
| Black | 2,506 (29) | 4,559 (29) | 5,649 (35) | 6,805 (33) | |
| Hispanic | 2,119 (25) | 1,461 (9) | 1,311 (8) | 1,346 (7) | |
| Asian | 415 (5) | 584 (4) | 501 (3) | 1,701 (8) | |
| Other | 759 (9) | 915 (6) | 1,081 (7) | 870 (4) | |
| Family History of Kidney Disease | 1,632 (19) | 3,100 (19) | 3,212 (20) | 3,797 (18) | 0.002 |
| Insurance | <0.001 | ||||
| Public only (Medicare, Medicaid, VA) | 2,604 (31) | 2,987 (19) | 2,146 (14) | 1,876 (9) | |
| Private only | 1,864 (22) | 6,418 (41) | 8,344 (52) | 12,921 (63) | |
| Both public and private | 1,146 (14) | 2,829 (18) | 2,249 (14) | 2,446 (12) | |
| Uninsured | 2,806 (33) | 3,518 (22) | 3,221 (20) | 3,231 (16) | |
| Access to a Doctor | 6,856 (80) | 13,972 (88) | 14,228 (88) | 18,607 (90) | <0.001 |
| Hypertension | 6584 (77) | 11941 (75) | 10984 (68) | 13190 (64) | <0.001 |
| Diabetes | 3228 (38) | 5003 (31) | 4572 (28) | 5154 (25) | <0.001 |
| CVD | 1233 (14) | 1890 (12) | 1512 (9) | 1406 (7) | <0.001 |
| Current or Previous Smoking | 4048 (47) | 7025 (44) | 6995 (43) | 6979 (34) | <0.001 |
| Body Mass Index | 30.4 +/− 7 | 30.5 +/− 7 | 30.7 +/− 7 | 29.5 +/− 7 | <0.001 |
| Reduced Kidney Function | 1823 (21) | 3035 (19) | 2413 (15) | 2789 (14) | <0.001 |
| Albuminuria | 1356 (16) | 2009 (13) | 1788 (11) | 1873 (9) | <0.001 |
Continuous variables are given as mean +/− standard deviation; categorical variables as number (column %). P value represents results of ANOVA test for continuous variables and chi square test for categorical variables.
CVD, cardiovascular disease; VA, Veterans Administration
For longitudinal analyses, we described the proportion of participants surviving over time by education level using Kaplan-Meier methods. We then examined the association between educational attainment and the risk of death using Cox proportional hazards survival analysis, adjusted for demographic characteristics, health behaviors, and the chronic diseases measured at screening. We verified proportionality for all predictors in the analysis by constructing log(-log(survival)) plots. To evaluate the robustness of the mortality findings across subgroups, we conducted stratified analyses by demographic characteristics and co-morbid conditions. We obtained p values for interaction using cross products between education and the subgroup of interest in adjusted models.
Results
Among 89,622 individuals enrolled in KEEP, a total of 61,457 participants were included in this analysis. Compared to those included in this analysis, the 28,165 individuals who were excluded were similar in age (56 versus 54 years, p<0.001), prevalence of diabetes (30% versus 29%, p<0.06), and hypertension (71% versus 70%, p<0.001). Educational attainment was lower for those excluded from this analysis: 21% did not complete high school, and 29% completed college, compared with 14% and 34%, respectively, of persons included in this analysis.
The participants were predominantly female (68%) and white (47%). Approximately one-third of both blacks and whites had completed college or a higher degree, whereas 53% of Asians had completed college (Table 1). Hispanics were the least likely to complete college (22%) and most likely to have not finished high school (34%). Notably, access to a doctor was high (>80%) across education levels. Public insurance and the lack of insurance were more common with lower levels of educational attainment.
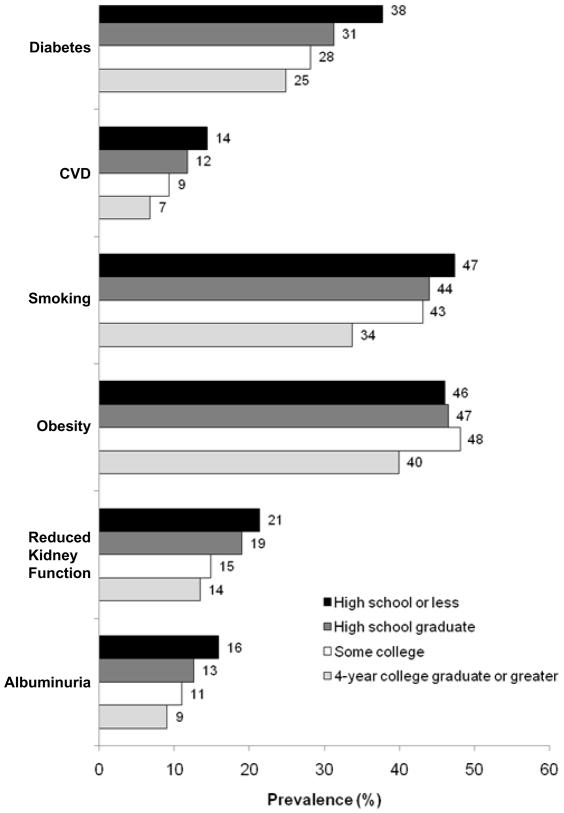
We observed stepwise patterns in the prevalence of all adverse health behaviors and chronic diseases according to educational level (Figure 1). The absolute differences in prevalence between the lowest and highest education groups were: 13% for smoking, diabetes, and hypertension, and 7% for cardiovascular disease, reduced kidney function, and albuminuria. In adjusted analyses, persons who had completed at least some college had a lower risk of chronic diseases; the odds of these prevalent disease conditions appeared to be inversely proportional to educational level, with the exception of obesity. In those who had attained a four-year college degree or greater versus those who completed high school or less, the odds ratios (95% confidence interval (CI)) for the seven outcomes were as follows: hypertension, 0.71 (0.66–0.76); diabetes, 0.77 (0.72–0.81); cardiovascular disease, 0.62 (0.57–0.68); current or previous smoking, 0.57 (0.54–0.60); obesity, 0.83 (0.79–0.88); reduced kidney function, 0.89 (0.82–0.96); and albuminuria, 0.72 (0.67–0.78).
Figure 1. Prevalence of Chronic Disease Conditions by Educational Attainment.
We performed Cochran-Armitage Trend tests for hypertension, diabetes, cardiovascular disease, smoking, obesity, reduced kidney function (eGFR<60 ml/min/1.73 m2), and albuminuria (ACR ≥30 mg/g). All p-values are <0.001.
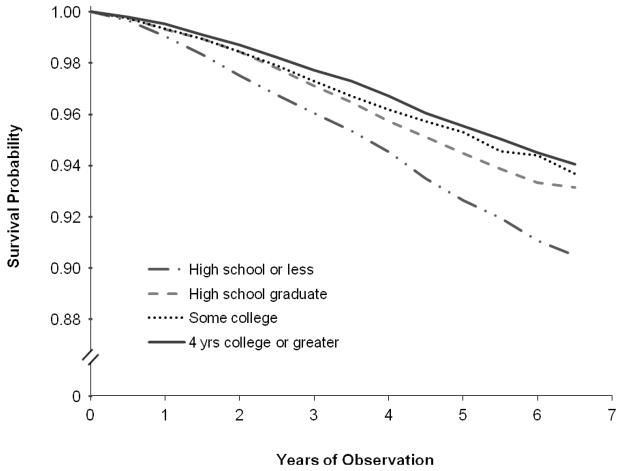
Over a mean follow-up time of 3.9 years (median, 3.7 years), 2,384 deaths occurred (4% of participants). In Kaplan-Meier survival analysis (Figure 2), the proportion surviving over the period of observation increased with higher educational attainment (log-rank test, p<0.001). Similarly, in adjusted analyses, a higher education level was associated with lower mortality (Table 2). In the fully adjusted Cox model, those who had completed college or more had a 24% lower mortality risk compared to participants who had finished high school or less, and the intermediate education groups had 19% lower mortality risk, independent of the baseline prevalence of chronic conditions and access to care. In our subgroup analyses, we found that the association between education and mortality did not differ significantly in any of the subgroups evaluated (P value for interaction >0.05). Interestingly, the effect of education appeared to be attenuated in the younger age group (<50 years), compared to those 50–65, and >65 years; however, heterogeneity across age groups was not statistically significant. Similarly, the intermediate education categories did not appear to be associated with lower mortality in Hispanics, but confidence intervals were wide across education groups. Additionally, education also appeared to have weaker associations with mortality risk among persons without hypertension and those with diabetes, but these subgroup differences did not approach statistical significance.
Figure 2.
Probability of Survival by Educational Attainment
Table 2.
Risk of Mortality Associated with Educational Attainment Overall and by Subgroups*
| Educational Level** | |||||
|---|---|---|---|---|---|
| Group | No. | High school graduate | Some college | college*** graduate or greater | P value for interaction |
| Full model | 0.81 (0.72–0.92) | 0.81 (0.71–0.92) | 0.76 (0.68–0.87) | ||
| Age | 0.1 | ||||
| <50 y | 23,309 | 1.12 (0.83–1.53) | 0.99 (0.73–1.35) | 0.94 (0.69–1.28) | |
| 50–65 y | 23,157 | 0.91 (0.72–1.15) | 0.91 (0.72–1.16) | 0.87 (0.68–1.10) | |
| >65 y | 14,991 | 0.71 (0.60–0.84) | 0.77 (0.65–0.92) | 0.77 (0.65–0.92) | |
| Gender | 0.9 | ||||
| Men | 19,663 | 0.80 (0.65–0.97) | 0.79 (0.64–0.97) | 0.77 (.063–0.93) | |
| Women | 41,794 | 0.82 (0.70–0.95) | 0.81 (0.69–0.95) | 0.76 (0.65–0.89) | |
| Race | 0.4 | ||||
| White | 28,875 | 0.82 (0.68–0.98) | 0.78 (0.64–0.94) | 0.77 (0.64–0.94) | |
| Black | 19,519 | 0.70 (0.55–0.88) | 0.85 (0.68–1.05) | 0.74 (0.59–0.93) | |
| Hispanic | 6,237 | 1.11 (0.75–1.63) | 1.10 (0.74–1.63) | 0.79 (0.51–1.24) | |
| Asian | 3,201 | 0.80 (0.44–1.48) | 0.65 (0.32–1.31) | 0.77 (0.44–1.33) | |
| Other | 3,625 | 0.93 (0.64–1.36) | 0.72 (0.48–1.07) | 0.71 (0.46–1.11) | |
| Hypertension | 0.2 | ||||
| No | 18,758 | 0.98 (0.71–1.36) | 0.90 (0.65–1.24) | 1.01 (0.73–1.38) | |
| Yes | 42,699 | 0.81 (0.71–0.92) | 0.82 (0.72–0.94) | 0.73 (0.64–0.84) | |
| Diabetes | 0.6 | ||||
| No | 43,500 | 0.76 (0.65–0.89) | 0.75 (0.64–0.88) | 0.69 (0.59–0.81) | |
| Yes | 17,957 | 0.91 (0.75–1.10) | 0.94 (0.77–1.15) | 0.93 (0.76–1.14) | |
| CVD | 0.9 | ||||
| No | 55,416 | 0.79 (0.69–0.91) | 0.79 (0.69–0.90) | 0.74 (0.65–0.85) | |
| Yes | 6,041 | 0.91 (0.70–1.20) | 0.92 (0.69–1.23) | 0.89 (0.66–1.21) | |
| Obesity | 0.1 | ||||
| No | 34,018 | 0.92 (0.78–1.09) | 0.89 (0.75–1.05) | 0.82 (0.69–0.97) | |
| Yes | 27,439 | 0.70 (0.59–0.84) | 0.73 (0.61–0.87) | 0.72 (0.60–0.87) | |
| Reduced Kidney Function | 0.08 | ||||
| No | 51,397 | 0.84 (0.72–0.98) | 0.88 (0.76–1.02) | 0.82 (0.70–0.95) | |
| Yes | 10,060 | 0.79 (0.64–0.97) | 0.68 (0.54–0.85) | 0.68 (0.54–0.86) | |
| Albuminuria | 0.5 | ||||
| No | 54,431 | 0.79 (0.69–0.91) | 0.79 (0.69–0.91) | 0.73 (0.63–0.84) | |
| Yes | 7,026 | 0.83 (0.65–1.07) | 0.81 (0.62–1.05) | 0.87 (0.67–1.13) | |
| Region | 0.8 | ||||
| Northeast | 14,062 | 0.93 (0.71–1.21) | 0.97 (0.73–1.28) | 0.82 (0.62–1.08) | |
| Midwest | 9,543 | 0.76 (0.57–1.01) | 0.83 (0.63–1.10) | 0.71 (0.53–0.95) | |
| South | 30,533 | 0.78 (0.66–0.93) | 0.77 (0.64–0.92) | 0.79 (0.66–0.94) | |
| West | 7,307 | 1.03 (0.69–1.54) | 0.82 (0.55–1.24) | 0.83 (0.55–1.25) | |
Note: Results reported as hazard ratio (95% confidence interval) for educational level adjusted for age, sex, race, family history of kidney disease, access to a doctor, insurance, smoking, hypertension, diabetes, cardiovascular disease, body mass index, reduced kidney function, and albuminuria, stratified by the subgroup variable. **reference group is high school or less
4-Year college
CVD, cardiovascular disease
Discussion
In this national sample of 61,457 persons, we observed graded, independent associations between higher educational attainment and lower prevalence of adverse health behaviors and chronic diseases, including hypertension, diabetes, cardiovascular disease, obesity, smoking, reduced kidney function, and albuminuria. Importantly, we also observed an independent association between a higher level of educational attainment and lower mortality rates. In contrast to our hypothesis, gradients in survival by educational level were not increased in ethnic minorities or diminished in elderly participants. Our study extends current understanding of the relationship between education and health by characterizing this association in a large, contemporary, ethnically diverse study population in various stages of chronic disease. It is noteworthy that the association between educational attainment and mortality remained consistent across ethnic minorities, the elderly, and among individuals with established chronic diseases. These findings suggest that the beneficial effects of education and its related impact on socioeconomic status are lifelong and that lower levels of educational attainment may contribute to the exacerbation of prevalent diseases and the development of medical illnesses.
While public health programs such as Healthy People 2010 have made it a priority to reduce socioeconomic and ethnic disparities in the United States, few studies have examined whether educational differences in mortality have been ameliorated during this past decade. Woolf et al. examined national vital statistics data between 1996 and 2002, and found that educational gradients in survival changed very little over that period. Lantz et al. followed 3,617 U.S. adults from 1986–2005 in the American's Changing Lives study and found that high school or less education, but not other educational levels, was associated with higher mortality when compared to those with ≥16 years education.14 Limitations of that study were its inclusion of only white and black persons and the small number of participants with higher levels of education (n=500); thus, the study may have been underpowered to examine gradients in educational levels.15 In contrast, Willcox et al. conducted a longitudinal study of only Japanese-American men in the Honolulu Heart Program/Asia Aging Study.16 In agreement with the present analysis, these investigators found that higher education (at least high school graduation) was significantly associated with improved survival.16 These findings among Asians are noteworthy as this group has the highest rate of high school graduation among ethnic minorities in the United States, but lower educational attainment was associated with the same adverse health consequences.17
It is controversial whether education affects health decades after schooling has been completed, as in elderly persons. Prior studies have described possible “birth cohort” effects or “survivor bias” which may confound the association between education and survival. In our study, the association between education and mortality was actually accentuated in the older age groups. While our study is unable to determine whether birth cohort effects contribute to this finding, our results are consistent with those of Lauderdale et al. who found that the association between education and mortality increased with age and was not due to cohort or period effects.18 Our results may inform efforts to eliminate health disparities, in that low educational attainment is especially prevalent among the elderly and racial/ethnic minorities; thus, the attributable mortality risk associated with low educational attainment in these groups is likely to be high.
While the causal pathway linking education to mortality is complex, our study and others have found that educational status is linked to several behavioral risk factors and chronic diseases, such as smoking, health illiteracy, poor diet and nutrition, and low levels of physical activity.14,19–20 Prior work in this area has demonstrated that education gives individuals knowledge that enables improved personal health choices and improves earning power, which gives better access to quality health care.21 Education helps individuals access information and recognize the implications of behaviors and healthcare options, to choose actions that optimize their health and that of their children, and to work their way through an increasingly complex healthcare system and manage their illnesses. Although not necessarily caused by education itself, educational attainment, we believe, is a marker for a societal construct that is, in fact, causally related to prognosis.
Several other possible mechanisms link educational attainment to mortality. Education is closely linked to income (and thus health care access), which is also strongly associated with mortality; those with lower incomes (and therefore lower-level occupations) and less education have higher mortality rates than individuals with higher levels of education and pay.14,19–20,22–23 Educated individuals have jobs that provide better resources for health care coverage, access to care, and out-of-pocket expenses. Furthermore, Zimmer and House found that education has the greatest impact on the prevention of disease, while income plays a greater role in the management of health problems. Among those with a critical health problem, individuals with a higher income will be better able to pay for care and to improve than those with a lower income.23 Prior studies concerning socioeconomic status and mortality have focused primarily on other predictors for socioeconomic status such as income or employment status as opposed to education, citing colinearity with income that influences results.7,14,18,20 Although we were able to account for access to care, insurance status, behavioral factors, and medical conditions, the lack of income data is a weakness of our study that does not allow us to disentangle the independent effects of education from income.
Another limitation is the study population chosen for this analysis. We studied participants of a health screening program targeting individuals at high risk for hypertension, diabetes, or kidney disease. The sampling design was not probabilistic in nature, the population included an oversampling of ethnic minority groups, and participants were volunteers, leading to probable selection bias. In addition, roughly one-fourth of persons screened in KEEP were excluded from analysis, and we cannot determine whether or not this may have biased our analysis. Because of these limitations, our study population was enriched with participants who are susceptible to medical illness, which may limit the generalizability of findings.
Our results suggest but do not prove that interventions to reduce educational disparities could have a broad and long-lasting impact across a range of sociodemographic and clinical subgroups. Furthermore, our results will help to guide future longitudinal studies that define mediators of the associations between educational attainment and mortality, such as health literacy or neighborhood-level factors, and health system based interventions to reduce health disparities related to the educational gradient. Clinical trials in this area could help to inform the allocation of educational resources.
Acknowledgments
Support: KEEP is a program of the National Kidney Foundation and is supported by Amgen, Abbott, Novartis, Siemens, Genentech, Genzyme, Nephroceuticals, Pfizer, LifecSan, and Suplena. These funding sources were not involved in the design or conduct of the study. Dr Norris is supported by National Institutes of Health grants MD00148 and 1U54RR026138.
Financial Disclosure: Dr Norris has consulted with Amgen, King Pharmaceuticals, and Abbott. The remaining authors declare that they have no relevant financial interests.
Footnotes
N section: Because the Editor-in-Chief recused himself from consideration of this manuscript, the Deputy Editor (Daniel E. Weiner, MD, MS) served as Acting Editor-in-Chief. Details of the journal’s procedures for potential editor conflicts are given in the Editorial Policies section of the AJKD website.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003 Jan 13;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 2.Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006 May–Jun;121(3):245–254. doi: 10.1177/003335490612100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kitagawa EM. In: Differential mortality in the United States: a study in socioeconomic epidemiology. Kitagawa Evelyn M, Hauser Philip M., editors. Cambridge, Mass: Harvard University Press; 1973. [Google Scholar]
- 4.Healthy People 2010. 2. Washington, DC: Department of Health and Human Services; 2000. [Google Scholar]
- 5. [Accessed March 1, 2008];Educational Attainment in the United States: 2003. 2004 http://www.census.gov/prod/2004pubs/p20-550.pdf.
- 6.Harper S, Lynch J, Burris S, Davey Smith G. Trends in the black-white life expectancy gap in the United States, 1983–2003. Jama. 2007 Mar 21;297(11):1224–1232. doi: 10.1001/jama.297.11.1224. [DOI] [PubMed] [Google Scholar]
- 7.Meara ER, Richards S, Cutler DM. The gap gets bigger: changes in mortality and life expectancy, by education, 1981–2000. Health Aff (Millwood) 2008 Mar–Apr;27(2):350–360. doi: 10.1377/hlthaff.27.2.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jemal A, Ward E, Anderson RN, Murray T, Thun MJ. Widening of socioeconomic inequalities in U.S. death rates, 1993–2001. PLoS One. 2008;3(5):e2181. doi: 10.1371/journal.pone.0002181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. N Engl J Med. 1993 Jul 8;329(2):103–109. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- 10.Ohmit SE, Flack JM, Peters RM, Brown WW, Grimm R. Longitudinal Study of the National Kidney Foundation's (NKF) Kidney Early Evaluation Program (KEEP) J Am Soc Nephrol. 2003 Jul;14(7 Suppl 2):S117–121. doi: 10.1097/01.asn.0000070155.63971.b2. [DOI] [PubMed] [Google Scholar]
- 11.Vassalotti JA, Li S, Chen SC, Collins AJ. Screening populations at increased risk of CKD: the Kidney Early Evaluation Program (KEEP) and the public health problem. Am J Kidney Dis. 2009 Mar;53(3 Suppl 3):S107–114. doi: 10.1053/j.ajkd.2008.07.049. [DOI] [PubMed] [Google Scholar]
- 12.Vassalotti JA, Li S, McCullough PA, Bakris GL. Kidney early evaluation program: a community-based screening approach to address disparities in chronic kidney disease. Semin Nephrol. 2010 Jan;30(1):66–73. doi: 10.1016/j.semnephrol.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999 Mar 16;130(6):461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 14.Lantz PM, Golberstein E, House JS, Morenoff J. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of U.S. adults. Soc Sci Med. 2010 Feb 20; doi: 10.1016/j.socscimed.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health. 2010 Apr 1;100( Suppl 1):S186–196. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Willcox BJ, He Q, Chen R, et al. Midlife risk factors and healthy survival in men. Jama. 2006 Nov 15;296(19):2343–2350. doi: 10.1001/jama.296.19.2343. [DOI] [PubMed] [Google Scholar]
- 17.Chapman C, Laird J, KewalRamani A. Education USDo. Trends in High School Dropout and Completion Rates in the United States: 1972–2008. Washington, D.C: National Center for Education Statistics, Institute of Education Sciences; 2010. [Google Scholar]
- 18.Lauderdale DS. Education and survival: birth cohort, period, and age effects. Demography. 2001 Nov;38(4):551–561. doi: 10.1353/dem.2001.0035. [DOI] [PubMed] [Google Scholar]
- 19.Rask K, O'Malley E, Druss B. Impact of socioeconomic, behavioral and clinical risk factors on mortality. J Public Health (Oxf) 2009 Jun;31(2):231–238. doi: 10.1093/pubmed/fdp015. [DOI] [PubMed] [Google Scholar]
- 20.Feinglass J, Lin S, Thompson J, et al. Baseline health, socioeconomic status, and 10-year mortality among older middle-aged Americans: findings from the Health and Retirement Study, 1992 2002. J Gerontol B Psychol Sci Soc Sci. 2007 Jul;62(4):S209–217. doi: 10.1093/geronb/62.4.s209. [DOI] [PubMed] [Google Scholar]
- 21.Cutler DM, Lleras-Muney A. Education and Health: Evaluating Theories and Evidence. In: Schoeni RF, House JS, Kaplan GA, editors. Making Americans Healthier: Social and Economic Policy as Health Policy. Russell Sage Foundation; 2008. pp. 29–59. [Google Scholar]
- 22.Sorlie PD, Backlund E, Keller JB. US mortality by economic, demographic, and social characteristics: the National Longitudinal Mortality Study. Am J Public Health. 1995 Jul;85(7):949–956. doi: 10.2105/ajph.85.7.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zimmer Z, House JS. Education, income, and functional limitation transitions among American adults: contrasting onset and progression. Int J Epidemiol. 2003 Dec;32(6):1089–1097. doi: 10.1093/ije/dyg254. [DOI] [PubMed] [Google Scholar]