Abstract
Subjects with binge eating disorder (BED) regularly consume large amounts of food in short time periods. The neurobiology of BED is poorly understood. Brain dopamine, which regulates motivation for food intake, is likely to be involved. We assessed the involvement of brain dopamine in the motivation for food consumption in binge eaters. Positron emission tomography (PET) scans with [11C]raclopride were done in 10 obese BED and 8 obese subjects without BED. Changes in extracellular dopamine in the striatum in response to food stimulation in food-deprived subjects were evaluated after placebo and after oral methylphenidate (MPH), a drug that blocks the dopamine reuptake transporter and thus amplifies dopamine signals. Neither the neutral stimuli (with or without MPH) nor the food stimuli when given with placebo increased extracellular dopamine. The food stimuli when given with MPH significantly increased dopamine in the caudate and putamen in the binge eaters but not in the nonbinge eaters. Dopamine increases in the caudate were significantly correlated with the binge eating scores but not with BMI. These results identify dopamine neurotransmission in the caudate as being of relevance to the neurobiology of BED. The lack of correlation between BMI and dopamine changes suggests that dopamine release per se does not predict BMI within a group of obese individuals but that it predicts binge eating.
INTRODUCTION
Binge eating disorder (BED) is characterized by episodes of eating an objectively large amount of food and feelings of loss of control. It occurs in about 0.7–4% of general population and about 30% of obese subjects attending weight control programs (1). Obese binge eaters eat significantly more calories than obese nonbinge eaters when asked to eat until extremely full, to binge eat, or to eat normally (2). Obese binge eaters have high relapse rates during weight control programs and experience their disorder for long periods of time.
Multiple factors regulate food intake including caloric requirements and reinforcing responses to food, which include palatability as well as conditioned responses (3). Dopamine is one of the neurotransmitters involved with feeding behaviors, and its pharmacological manipulation has marked effects on food intake (4). Brain imaging studies with positron emission tomography (PET) and [11C]raclopride showed that the desire for food during presentation of palatable food stimuli, without consumption, was associated with striatal dopamine release (5). The amount of dopamine release was also correlated with the ratings of meal pleasantness following consumption of a favorite food (6). These imaging studies are consistent with dopamine’s role in regulating food consumption through modulation of the rewarding properties of food and the motivation and desire for food consumption (4). It had been postulated that in humans, low dopamine activity could predispose a person to pathological overeating as a way to compensate for decreased dopaminergic activity (7). In fact, in a study done in morbidly obese subjects we reported decreased levels of striatal dopamine D2 receptors, which are predicted to result in an attenuation of dopamine signals (8). Abnormal dopaminergic activity has also been demonstrated in genetically inbred rodents for obesity and has been postulated to underlie overeating (9). Dopamine modulates motivation and reward circuits, and hence dopamine deficiency in obese subjects may perpetuate pathologic eating as a means to compensate for decreased activation of these circuits.
Individuals with BED are characterized by compulsive overeating and impulsivity (10), which shares similarities with compulsive and impulsive drug using behaviors in substance abusers (11). Food is a potent natural reinforcer, and fasting can further enhance its rewarding effects (12). Dopamine plays an important role in signaling the salience for a variety of potential cues that predicts selection of rewards during fasting (13). Some ingredients in palatable food such as sugar and corn oil can result in impulsive ingestion in patterns reminiscent of those seen with drug intake in addiction (4,14). As in the case for drugs of abuse, ingestion of sugar increases dopamine in the nucleus accumbens (14). For example, when rats are given intermittent access to sugar solutions, they drink in a binge-like manner, releasing dopamine in the nucleus accumbens, similar to that observed in animal models of drug dependence (14). The sweet taste of sugar, without the nutrition component, can also induce release of dopamine (15). Using PET and [11C]raclopride, we showed that visual and olfactory exposure to palatable food increased extracellular dopamine in the dorsal striatum in normal-weight healthy controls who had been food deprived for 16 h (5). The dopamine releases were significantly correlated with the increases in self-reports of hunger and desire for food. These results provided evidence of a conditioned-cue response in the dorsal striatum.
Here, we evaluate the hypothesis that obese subjects with BED would show stronger conditioned responses to food stimuli when compared with non-BED obese subjects. To measure changes in dopamine induced by food conditioned stimuli, we used PET and [11C]raclopride with the imaging paradigm that we reported previously (5). Understanding the neurobiological mechanisms underlying food stimulation can provide targets for interventions to help individuals regulate their abnormal eating behaviors.
METHODS AND PROCEDURES
Participants
The institutional review boards at Stony Brook University (Stony Brook, NY)/Brookhaven National Laboratory (Upton, NY), and St. Luke’s–Roosevelt Hospital (New York, NY) approved the protocol. Written informed consent was obtained after the experimental procedure was explained. Ten healthy subjects with BMI (kg/m2) >30 and DSM IV (Diagnostic and Statistical Manual of Mental Disorder-Fourth Edition) diagnosis for BED were recruited for the study. The control group (n = 8) comprised obese subjects (BMI >30) that did not fit into the criteria for BED. Exclusion criteria for both groups were: history of surgical/medical treatment for weight control, dependence on alcohol or other drugs of abuse (except for caffeine <5 cups/day or nicotine <1 pack/day), neurological or psychiatric disorder (other than binge eating for the BED group), use of prescription (nonpsychiatric) medication(s) that can affect brain function, in the past 2 weeks, medical conditions that may alter cerebral function, cardiovascular disease and diabetes, head trauma with loss of consciousness of >30 min. Urine screening tests for psychoactive drugs (including phencyclidine, cocaine, amphetamine, opiates, barbiturates, benzodiazepine and tetrahydrocannabinol) were performed to corroborate lack of drug use.
Psychological diagnosis
Candidates were recruited and screened psychologically at St Luke’s–Roosevelt Hospital for BED using the Eating Disorder Examination, a structured clinical interview which was modified for BED (16). They also completed the Zung Depression Scale (17,18), and the Gormally Binge Eating Scale (19), which reflects binge-eating–related behavior and attitudes.
Study design
The subjects were asked to fill out a questionnaire, which contained the following information on the day of screening: a rating of overall interest in food; list of favorite foods; list of food smells that stimulated appetite; list of food smells that diminished appetite; and a rating of a list of foods for their preferences on a scale from 1 to 10, 10 being the highest. The food items with the highest ratings were presented to the subject during the food stimulation condition.
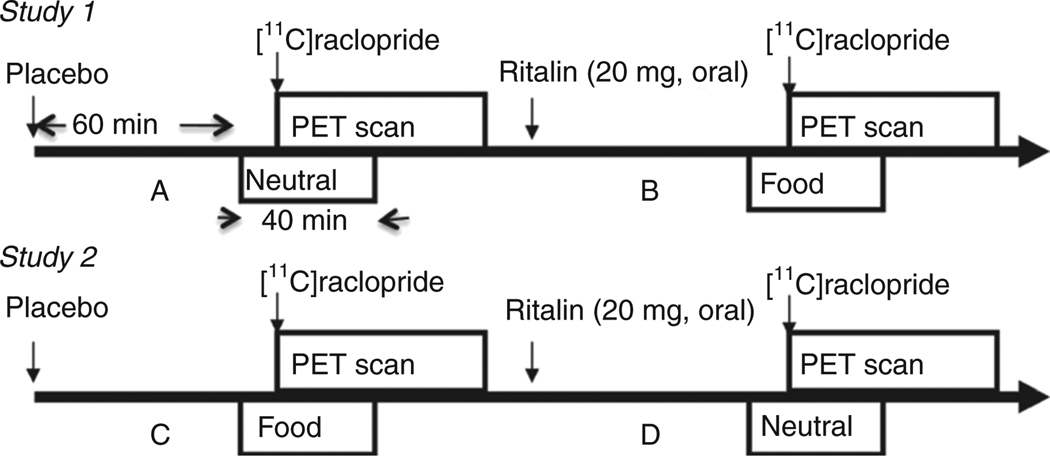
Subjects were scanned four times with [11C]raclopride on two different days under the following conditions (Figure 1): On the first day of study, the first [11C]raclopride scan was started 70 min after oral placebo (dicalcium phosphate tablet) with neutral intervention (neutralplacebo). The second [11C]raclopride scan was started 70 min after oral administration of methylphenidate (MPH: 20 mg) with food intervention (foodMPH) about 2 h and 20 min after the radiotracer injection of the first one. On the second day of study, the first [11C]raclopride scan was started 70 min after oral placebo (dicalcium phosphate tablet) with food intervention (foodplacebo). The second [11C]raclopride scan was started 70 min after oral administration of MPH (20 mg) with neutral intervention (neutralMPH) about 2 hs and 20 min after the radiotracer injection of the first one. We chose a dose of MPH (20 mg oral), which we had previously shown to induce significant increases in striatal dopamine level in normal-weight subjects during food stimulation (5). Both the food and neutral interventions began about 10 min before the radiotracer injection and continued for a total of about 40 min. The subjects did not know whether they received the placebo or MPH. In addition, the order of the study days were varied and counterbalanced across subjects.
Figure 1.
Flow chart of the study. PET, positron emission tomography.
For the food stimulation condition, the food was warmed to enhance the smell, and the subjects were presented with it so that they could view and smell it. A cotton swab impregnated with the food was placed on their tongues so they could taste it. A given food item was presented for 4 min and then exchanged for a new one. The taste, smell, and view of food continued throughout the stimulations. The subjects were asked to describe their favorite foods and how they like to eat them while they were presented with foods that they had reported as their favorite ones. For the neutral stimulation, subjects were presented with pictures, toys, and clothing items so they could view them and smell them and discuss them during the stimulation. We also used a cotton swab impregnated with a neutral taste (such as metallic or plastic), which was placed on their tongues. The food and neutral interventions were started 10 min before radiotracer injection and were continued for a total of 40 min. For both study days, the subjects were asked to have their last meal at 7:00 pm the evening before the day of study and reported to the imaging center at 8:30 am.
Behavior and cardiovascular measures
During the PET studies, participants were instructed to orally respond to each descriptor using a whole number between 1 and 10 for the self-report of “hunger” and “desire of food”, which were obtained prior to the food/neutral stimulation and then at 4-min intervals for a total of 40 min. In addition, pulse rate and blood pressure were obtained before placebo/MPH, 30 min, 60 min (prior to the neutral/food stimulation), then every 3 min during food/neutral stimulation for a total of 42 min.
PET scans
Subjects were scanned with [11C]raclopride using a Siemens HR+ PET scanner. Details on procedures for positioning of the subjects’ arterial and venous catheterization, quantification of radiotracer and transmission and emission scans have been published (5). Briefly, dynamic images were taken immediately after a bolus intravenous injection of 3–7 mCi of [11C]raclopride for a total of 60 min. Blood samples were obtained to measure plasma MPH concentration prior to and at 30, 60, 90, and 120 min after MPH. The plasma concentration of MPH was analyzed at Dr Thomas Cooper’s laboratory (Nathan Kline Institute, Orangeburg, NY).
Image analysis
The regions of interest in dorsal striatum (caudate, putamen), ventral striatum, and cerebellum were outlined by superimposing boundaries from a neuroanatomical atlas using a template, which we had previously published (5). Briefly, regions of interest were initially outlined on the individual’s summed baseline [11C]raclopride image (images obtained between 15 and 54 min) and were then projected into the dynamic [11C] raclopride images to generate time–activity curves for the striatal regions (caudate, putamen, and ventral striatum) and cerebellum. These time–activity curves for tissue concentration, along with the time–activity curves for unchanged tracer in plasma were used to calculate [11C]raclopride’s transfer constant from plasma to brain (K1) and the total tissue distribution volume (VT), which corresponds to the equilibrium measurement of the ratio of tissue concentration to plasma concentration, in striatum and cerebellum using a graphical analysis technique for reversible systems (20). The ratio of VT in striatum to that of VT in cerebellum corresponds to nondisplaceable binding potential (BPND) +1 where BPND is the in vivo binding potential which is proportional to the number available binding sites Bavail/Kd. It is unlikely that BPND for raclopride is affected by changes in blood flow during the scan, but to check for this possibility K1 (which is a function of blood flow) was estimated for the baseline and MPH studies which had arterial blood sampling by fitting the data to a one-compartment model (21). A one-compartment model was used for both cerebellum and the D2 regions of interest.
The response to food stimulation (with placebo or with MPH) was quantified as the difference in Bmax/Kd with respect to the neutralplacebo condition, which was the condition used as baseline. Similarly, the response to MPH with the neutral stimulation (used as a measure of MPH’s effects) was quantified as the difference in BPND with the neutral/placebo condition.
Data analysis
Difference in K1 values between placebo and MPH were tested using paired t-test. Differences in BPND between conditions were tested using a 2 × 2 factorial design (drug × cue type) and the group comparison using a mixed design ANOVA. The relative contributions of gender as well as age and BMI were taken into account in the ANOVA model. Post hoc t-tests were then used to determine for which conditions the effects differed from the baseline condition (neutralplacebo). Post hoc power analyses for paired samples t-tests with multiple-test correction and for repeated measures ANOVA were performed. The effects of the food stimulation on the behavioral self-reports were tested by comparing the scores obtained prior to stimulation and the averaged scores obtained between 15 and 40 min after initiation of the intervention using repeated measures ANOVA. The effects of the food stimulation on cardiovascular responses were tested by comparing the measures prior to placebo/MPH, prior to stimulation (60 min after placebo/MPH), and the average measures obtained between 3 and 42 min after initiation of the stimulation using repeat measures ANOVA. Pearson product moment correlations were used to assess the relationship between the food stimulation–induced changes in BPND and parameters such as the behavioral effects of the food stimulation, cardiovascular responses (pulse rate and blood pressure), scores on the binge eating scale, age, and BMI, as well as between MPH-induced changes in BPND and parameters such as cardiovascular responses, age, and BMI. Pearson product moment correlations were also performed between the changes in dopamine induced by MPH when given with the neutral stimulation vs. the changes when given with the food stimulation and parameters such as the behavior effects of the food stimulation, scores on the binge eating scale, cardiovascular responses, age, and BMI.
RESULTS
Ten binge eaters and eight nonbinge eaters were recruited for the study. Both groups were similar in age, BMI, Zung depression scores, years of education and social economic background (Table 1). The binge eaters had significantly higher scores for the Gormally Binge Eating Scale (P < 0.000001).
Table 1.
Characteristics of study participants
| Binge eaters (n = 10) |
Nonbinge eaters (n = 8) |
P value | |
|---|---|---|---|
| Number | 8F + 2M | 5F + 3M | |
| Age (y/o) range | 21–54 | 28–56 | |
| Age (y/o) mean ± s.d. | 38.5 ± 13.3 | 41.8 ± 8.9 | NS |
| Education (years) range | 12–18 | 12–18 | |
| Education (year) mean ± s.d. | 15.3 ± 1.6 | 14.3 ± 2.1 | NS |
| Cigarette use (per day) | 2.2 ± 3.5 | 2.4 ± 6.7 | NS |
| BMI range | 30–65 | 31–59 | |
| BMI mean ± s.d. | 43.4 ± 13.5 | 36.5 ± 9.4 | NS |
| BES range | 19–31 | 0–13 | |
| BES mean ± s.d. | 25.5 ± 4.1 | 4.6 ± 4.9 | 0.000001 |
| Zung depression mean ± s.d. | 53.6 ± 12.5 | 47.4 ± 9.3 | NS |
BES, Gormally Binge Eating Scale; F, female; M, male; NS, not significant; y/o, years old.
Food stimulation increased hunger and desire for food in binge eaters (P < 0.001, P < 0.001, respectively) and nonbinge eaters (P < 0.05, not significant, respectively) in placebo as well as in oral MPH (binge eaters: P < 0.05, not significant; nonbinge eaters: P < 0.05, P < 0.05) conditions, respectively (Table 2). However, the increases in self-report parameters during food stimulation (with or without MPH) did not differ between binge eaters and nonbinge eaters.
Table 2.
Self-report feelings of hunger and desire for food after food stimulation (FS) in the binge eaters and nonbinge eaters
| Binge eaters | Nonbinge eaters | |||
|---|---|---|---|---|
| Conditions | Pre-FS | Post-FS | Pre-FS | Post-FS |
| Hunger | ||||
| Foodplacebo | 4.26 ± 2.51 | 8.90 ± 2.33* | 5.57 ± 3.34 | 9.25 ± 1.39** |
| FoodMPH | 5.84 ± 2.44 | 8.29 ± 2.26** | 4.62 ± 3.54 | 9.43 ± 0.98** |
| Desire for food | ||||
| Foodplacebo | 4.21 ± 2.57 | 9.00 ± 1.70* | 5.83 ± 3.57 | 9.25 ± 1.39 |
| FoodMPH | 6.80 ± 2.27 | 8.76 ± 1.69 | 4.79 ± 3.40 | 9.29 ± 1.25** |
Self-report ratings: 1–10 (1: least, 10: most). Comparisons correspond to repeated ANOVA of pre-to post-FS.
MPH, methylphenidate.
P < 0.001,
P < 0.05.
Food stimulation increased systolic pressure in binge eaters (+6 ± 7%, P = 0.04) and nonbinge eaters (+2 ± 2%, P = 0.02) in placebo condition (Table 3). Comparisons between systolic pressure changes during food stimulation and neutral stimulation did not differ in binge eaters and in nonbinge eaters (measured by stimulation interaction). During food stimulation, pulse rate decreased in nonbinge eaters (P = 0.02) in placebo but not in binge eaters. Blood pressure measured at 60 min (prior to neutral stimulation) after oral MPH in nonbinge eaters showed systolic pressure increases (P = 0.002), which persisted during neutral stimulation (P = 0.004). However, systolic pressure in nonbinge eaters did not change when it was measured prior to food stimulation (60 min after oral MPH), and the systolic pressure was not significantly different between the studies (measured by study interaction).
Table 3.
Group mean measures of pulse rate and blood pressure for the four testing conditions for the baseline, prior to neutral/food stimulation and during neutral/food stimulation
| Pulse rate | Systolic pressure | Diastolic pressure | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | Prior to stimulation |
During stimulation |
Baseline | Prior to stimulation |
During stimulation |
Baseline | Prior to stimulation |
During stimulation |
|
| Binge eaters | |||||||||
| Neutralplacebo | 74.0 ± 11.1 | 71.7 ± 9.4 | 72.8 ± 10.2 | 117.5 ± 12 | 121.4 ± 12 | 121.8 ± 12 | 64.5 ± 6.1 | 65.0 ± 6.3 | 68.7 ± 16.6 |
| NeutralMPH | 76.4 ± 12.3 | 78.9 ± 10.4 | 78.8 ± 11.5 | 125.8 ± 12 | 127.0 ± 14 | 125.7 ± 12 | 66.2 ± 8.3 | 65.5 ± 8.9 | 64.9 ± 7.2 |
| Foodplacebo | 74.5 ± 12.3 | 75.2 ± 12.7 | 76.4 ± 13.5 | 119.6 ± 11 | 123.9 ± 12 | 126.3 ± 12a | 61.7 ± 8.5 | 65.6 ± 8.4 | 64.7 ± 7.9 |
| FoodMPH | 71.3 ± 10.6 | 73.3 ± 10.8 | 76.0 ± 9.9 | 119.1 ± 10 | 124.3 ± 10 | 123.0 ± 10 | 65.2 ± 4.7 | 63.2 ± 5.3 | 64.7 ± 11.4 |
| Nonbinge eaters | |||||||||
| Neutralplacebo | 62.2 ± 9.0 | 63.0 ± 9.7 | 64.1 ± 10.2 | 123.3 ± 11 | 129.3 ± 21 | 128.0 ± 17 | 68.0 ± 13.4 | 68.7 ± 16.6 | 69.0 ± 15.7 |
| NeutralMPH | 64.9 ± 9.9 | 66.7 ± 9.6 | 67.4 ± 11.5 | 124.8 ± 16 | 134.2 ± 17b | 133.1 ± 15b | 68.5 ± 13.2 | 71.6 ± 15.4 | 71.7 ± 17.4 |
| Foodplacebo | 68.3 ± 12.3 | 68.7 ± 12.3 | 66.5 ± 14.2 | 129.3 ± 18 | 131.6 ± 20 | 131.7 ± 18a | 73.5 ± 13.5 | 73.1 ± 15.2 | 71.8 ± 16.4 |
| FoodMPH | 67.7 ± 10.7 | 67.0 ± 11.2 | 68.9 ± 9.9 | 131.9 ± 16 | 138.4 ± 23 | 136.4 ± 20 | 70.7 ± 12.6 | 71.8 ± 16.0 | 73.8 ± 17.4 |
MPH, methylphenidate.
Significantly increased systolic pressure between baseline and during food stimulation in binge eaters (P = 0.04) and nonbinge eaters (P = 0.02).
Significantly increased systolic pressure between baseline and prior to neutral stimulation (P = 0.002) as well as between baseline and during neutral stimulation (P = 0.004) in nonbinge eaters.
Averaged blood MPH concentration did not differ between both groups of subjects during the neutralMPH (binge eaters: 6.75 ± 2.33, nonbinge eaters: 6.07 ± 2.72) and foodMPH (binge eaters: 6.6 ± 2.83, nonbinge eaters: 6.03 ± 2.48) conditions.
K1 values of averaged striatal regions for the placebo and MPH conditions were 0.101 ± 0.02 and 0.11 ± 0.026 (binge eaters—food), 0.09 ± 0.014 and 0.0927 ± 0.02 (binge eaters—neutral), 0.107 ± 0.029 and 0.106 ± 0.03 (nonbinge eaters—food), 0.093 ± 0.012 and 0.098 ± 0.011 (nonbinge eaters—neutral). The average % changes for the groups were +8%, +4%, −0.6%, and +5%, respectively. The differences of K1 values were significant for binge eaters: foodplacebo vs. foodMPH (P < 0.01) and nonbinge eaters: neutral placebo vs. neutralMPH (P < 0.03).
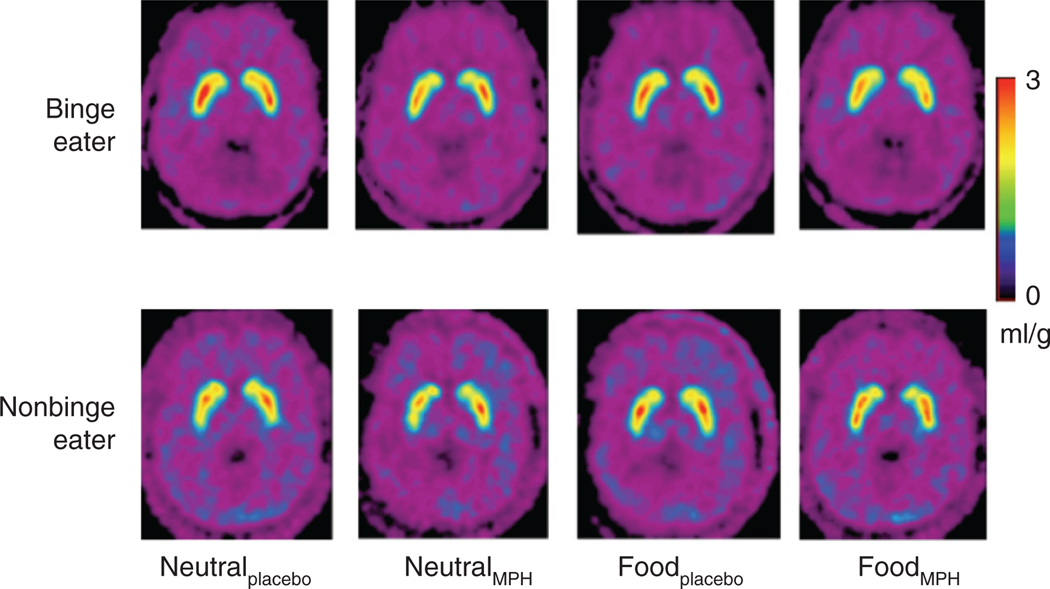
The baseline (neutralplacebo) dopamine D2 receptor availability did not differ between binge eaters and nonbinge eaters and was not correlated with BMI or Zung depression scores. Neither the neutral stimuli nor the food stimuli when given with placebo increased extracellular dopamine in nonbinge eaters. The neutral stimulation given with MPH (neutralMPH, drug by cue interaction, P = 0.003; the estimated effect size Cohen’s d = 1.63 with power = 99.99% at significance level of 0.05, and power = 99.96% at significance level of 0.05/3 with multiple-test correction), but not the food stimuli given with MPH (foodMPH), significantly increased dopamine release in caudate in nonbinge eaters. In binge eaters, neutral stimulation neither with nor without MPH (neutralMPH) significantly increased dopamine release. The food stimuli given with MPH (foodMPH) compared with baseline (neutralplacebo) showed significant dopamine release in binge eaters in caudate (P = 0.003; the estimated effect size, Cohen’s d = 1.30) and putamen (P = 0.05; the estimated effect size = 0.74). The food stimuli given with placebo (foodplacebo) did not induce significant differences between binge eaters and nonbinge eaters (scan by stimuli interaction). Even though MPH with neutral stimulation (neutralMPH) induced significant caudate dopamine release in nonbinge eaters but not in binge eaters, the interaction was not significant (scan by diagnosis interaction). For the comparison of the food stimuli given with MPH (foodMPH) vs. the baseline (neutralplacebo), binge eaters had significantly more dopamine release than nonbinge eater in caudate (scan by diagnosis interaction, P = 0.026, Table 4 and Figure 2 the estimated effect size = 0.79). However, the differences in putamen or in ventral striatum were not significant.
Table 4.
Group mean measures of binding potential (BPND) for the four testing conditions and percent changes to the neutralplacebo condition for the caudate nucleus, putamen, and ventral striatum
| Caudate nucleus | Putamen | Ventral striatum | ||||
|---|---|---|---|---|---|---|
| BPND | % Change | BPND | % Change | BPND | % Change | |
| Binge eaters | ||||||
| Neutralplacebo | 2.79 ± 0.49 | 3.38 ± 0.54 | 2.64 ± 0.52 | |||
| NeutralMPH | 2.55 ± 0.54 | +7.8 ± 16.2 | 3.36 ± 0.66 | +0.7 ± 9.5 | 2.81 ± 0.54 | −8.1 ± 18.6 |
| Foodplacebo | 2.80 ± 0.55 | −0.7 ± 11.9 | 3.46 ± 0.63 | −2.3 ± 10.3 | 2.99 ± 0.67 | −14.8 ± 21.6 |
| FoodMPH | 2.53 ± 0.4a | +8.8 ± 6.7 | 3.17 ± 0.5 | +5.8 ± 7.8 | 2.54 ± 0.43 | +1.4 ± 20.4 |
| Nonbinge eaters | ||||||
| Neutralplacebo | 2.50 ± 0.31 | 3.07 ± 0.39 | 2.28 ± 0.47 | |||
| NeutralMPH | 2.22 ± 0.4b | +11.9 ± 9.8 | 2.75 ± 0.55 | +10.6 ± 14.4 | 2.22 ± 0.51 | +0.8 ± 24.7 |
| Foodplacebo | 2.41 ± 0.56 | +4.6 ± 15.1 | 2.95 ± 0.62 | +4.0 ± 17.5 | 2.45 ± 0.54 | −9.6 ± 15.2 |
| FoodMPH | 2.47 ± 0.4a | +1.1 ± 6.7 | 3.06 ± 0.48 | +0.2 ± 10.2 | 2.41 ± 0.28 | −8.2 ± 18.9 |
Percent changes are calculated with respected to neutralplacebo, which served as baseline condition.
MPH, methylphenidate.
Comparison of foodMPH with neutralplacebo, binge eaters had greater change than nonbinge eater (scan × diagnosis, P = 0.026).
Significant between neutralplacebo and neutralMPH in nonbinge eaters (P = 0.003).
Figure 2.
Distribution volume ratio image [11C]raclopride at level of striatum for one of the binge eaters and one of the nonbinge eaters for four scanning conditions: neutral stimulation with oral placebo, neutral stimulation with oral methylphenidate (MPH), food stimulation with oral placebo and food stimulation with oral MPH. The images are scaled with respect to the maximum distribution volume ratio value of the binge eater obtained on neutral stimulation with oral placebo. The images are presented by using the rainbow scale, where red represents the highest value and violet represents the lowest value. Binding of [11C]raclopride is lowest during the food stimulation with oral MPH in the binge eater.
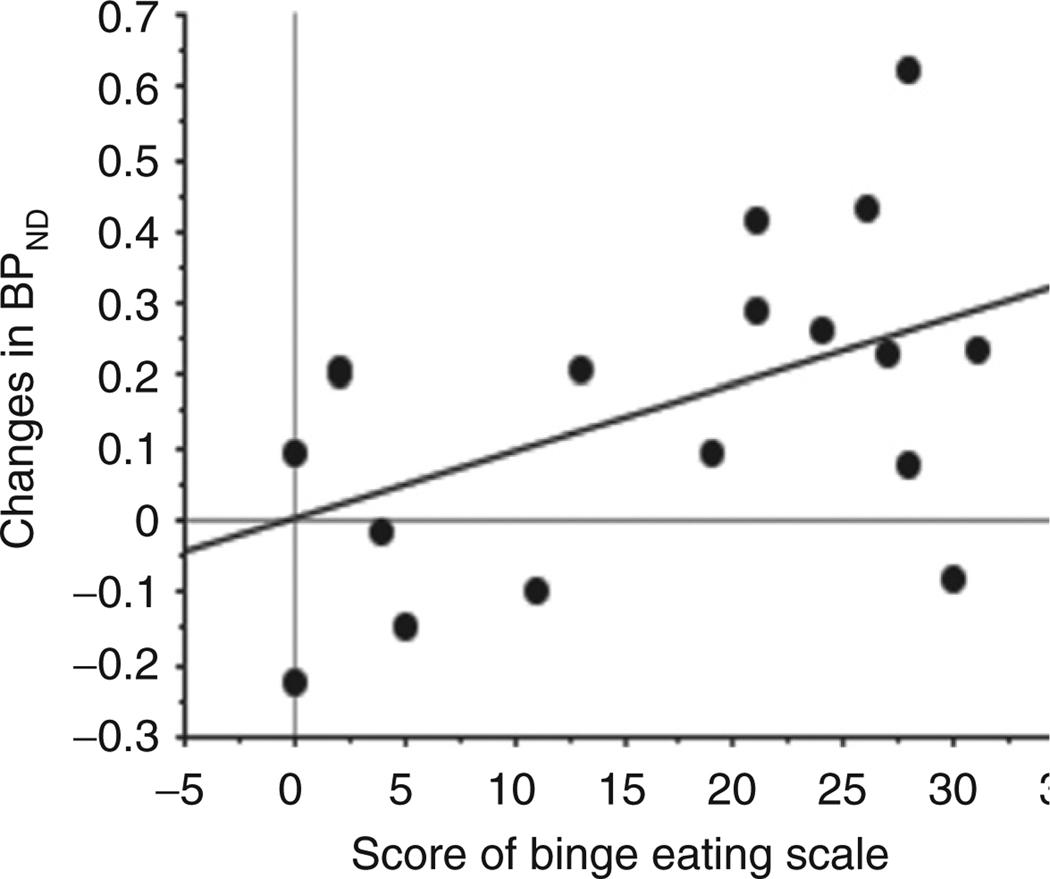
There were no correlations between foodplacebo condition and self-report parameters, cardiovascular responses, scores on the binge eating scale, age or BMI. Compared across all subjects, the subjects with larger BMI had lower plasma MPH concentration (n = 18, r = 0.57, P < 0.01). The increases in striatal dopamine release across all subjects for the neutralMPH condition were not correlated with self-report scores, cardiovascular responses, scores on the binge eating scale, plasma MPH concentration, age, and BMI. The increases of dopamine release across all subjects in caudate under foodMPH condition were correlated with severity in the Gormally Binge Eating Scale (n = 18, r = 0.49, P < 0.03, Figure 3) but not with BMI, plasma MPH concentration, self-report parameters, cardiovascular responses, and age. No gender effects were observed in these parameters.
Figure 3.
Correlation between dopamine release (changes in nondisplaceable binding potential (BPND)) in the caudate nucleus of all subjects under foodMPH condition with scores of the Gormally Binge Eating Scale (n = 18, r = 0.49, P < 0.03). MPH, methylphenidate.
DISCUSSION
This study showed that obese binge eaters had greater increases of extracellular dopamine levels in the caudate nucleus during the food stimulation when dopamine transporters were blocked by the administration of MPH, than the nonbinge eaters. In contrast, the ventral striatum where the nucleus accumbens is located did not differ between the groups. Dopamine in the nucleus accumbens has been found to influence the motivation for behavioral output toward drugs and drug-associated stimuli (22). Animal studies showed that anticipating an impending reward from food intake activated mesotelencephalic dopamine neurons, and the dopamine activation in the nucleus accumbens was greater in the presence of conditioned stimuli that signaled food receipt than after actual delivery of an unexpected meal (23). The nucleus accumbens integrates converging input from limbic sites related to appetite and rewards to initiate approach behavior (24). Its activation predicts an immediate reward. In contrast, the dorsal striatum is important for the formation of behavioral habits and has been shown to a be major mediator in drug abuse behaviors (25). The dorsal striatum contributes to stimulus response habit learning, where behavior becomes automatic and no longer driven by an action outcome relationship (26). When conditioned stimuli predict an upcoming reward, the firing of dopamine neurons occurs after reward-predicting stimulus, rather than after the reward itself (27). Electrophysiological recordings in monkeys in the caudate nucleus, suggest that its activity may be dependent on the anticipated consequence of performance (28). However, the caudate nucleus is believed to be involved in reinforcement of action potentially leading to reward but not in processing of the reward per se (29).
In this study, BMI did not differ between the nonbinge eaters and binge eaters. However, scores on the binge eating scale were higher for the binge eaters as expected. The Gormally Binge Eating Scale scores were associated with extracellular dopamine increases in the caudate during food stimulation. Subjects with higher binge eating scores had greater extracellular dopamine increases in caudate during the food stimulation than those with lower scores. Prior imaging studies have shown that obese binge eaters had more activation in the frontal and prefrontal cortical areas than obese nonbinge eaters during food cue stimulation (30,31). Binge eaters showed greater responses in medial orbitofrontal cortex while viewing food pictures, which was correlated with their reward sensitivity (30). In a prior study using PET-18F-fluorodeoxyglucose and the same food stimulation paradigm, we showed that in normal weight fasting subjects, orbitofrontal activation was associated with an increased desire for food (32). The mesoaccumbens/mesocortical dopamine fibers, which mostly originate in the ventral tegmental area, innervate limbic and cortical regions including prefrontal and orbitofrontal cortices (33). Thus, the activation in these frontal regions could reflect downstream effects of dopaminergic striatal activation.
Unlike the obese binge eaters, the obese nonbinge eaters did not increase extracellular dopamine levels in striatum during food stimulation. Using PET-[11C]raclopride with the same food stimulation paradigm to evaluate changes in striatal extracellular dopamine in food-deprived normal-weight subjects, we showed significant increases (+12%) in extracellular dopamine in the dorsal striatum (5). It is possible that obese subjects might have a downregulated dopamine system (+8% in obese binge eaters and +1% in obese nonbinge eaters). Imaging studies in humans and animals from our laboratory and others, showed enhanced activation in brain regions related to sensory processing of food in obese individuals. Specifically using PET and 18F-fluorodeoxyglucose, we showed that morbidly obese subjects had higher than normal baseline glucose metabolism (without stimulation) in the gustatory somatosensory cortex than nonobese subjects (34). A functional magnetic resonance imaging study of adolescent girls showed that obese girls had greater activation in insula and gustatory somatosensory cortex in response to anticipated food intake and to actual consumption of food than lean girls (35). Preclinical studies from our group showed that food stimulation (viewing and smelling without consumption) enhanced thalamic activation in obese Zucker rats more than in lean littermates (36). These activated/enhanced regions are implicated in sensory (somatosensory, visual cortices, thalamus) and hedonic (insula) aspects of food cues. Dopamine stimulation signals saliency and facilitates conditioning (37). Dopamine’s modulation of neural processing of food cues in the sensory cortices and thalamus to food stimuli might enhance their saliency, which is likely to play a role in the formation of conditioned associations between food and food-related environmental cues. The functional magnetic resonance imaging study of adolescent girls (35) showed that obese girls had greater activation in the brain regions that relate to sensory and hedonic aspects of the food. However, these obese girls also showed decreased activation in the caudate in response to food consumption, which might indicate a dysfunctional dopamine system that could increase their risk of overeating (35).
Here, we show that a therapeutic dose of oral MPH (20 mg) significantly increased extracellular dopamine in caudate in nonbinge eaters but not in binge eaters. However, the dopamine increases was not significantly different between the groups. Our prior finding in healthy normal-weight subjects showed that MPH did not induce significant cardiovascular effects, similar to the findings of this study, and MPH-induced striatal dopamine increases were larger when MPH was given with a salient stimulation (visual food stimulation when food deprived, money) than when given with a neutral stimulus (5,38). These results might reflect the context-dependent effects of MPH (dopamine increases result from dopamine transporter blockade and spontaneous dopamine releases). The greater dopamine increases occurred when exposed to a salient stimulus that presumably increases dopamine cell firing in the binge eaters. The finding is similar to our study in the cocaine-dependent subjects in which MPH-induced craving only when given with exposure to cocaine cues (39). The reason why we did not observe dopamine increases when MPH was given with salient stimuli (food cues) in nonbinge eaters is not clear. It is possible that when MPH amplifies the effects of relatively weak reinforcing stimuli (as in binge eaters) it may not do so for stronger ones (as in normal-weight subjects). It is also possible that the slow and small dopamine increases induced by MPH could be sufficient to inhibit dopamine release via dopamine D2 autoreceptors and attenuate the phasic dopamine cell firing associated with food stimulation.
The use of MPH introduces the possibility of blood flow changes occurring during the scan. This is only a potential problem in the estimation of BPND if the changes occur in the scan after oral MPH. If the flow is greater but constant during the scan, there will be no effect on the VT. Slifstein et al. has shown that the greatest error in VT estimation will occur with large rapid changes in flow during the first several minutes after tracer injection (21). However, they have shown that for kinetic parameters characteristic of fallypride, a 60% change in flow occurring abruptly results in only small differences in VT. Since the K1 for raclopride is smaller than for fallypride, flow changes will have less effect on uptake. Also the dose of MPH is given orally and not by injection, so that any changes in flow would be expected to be continuous. Since the change in K1 was in binge eaters, comparing foodplacebo and foodMPH, we would conclude that the change in K1 had no effect on the VT since it didn’t change. For nonbinge eaters, comparing neutralplacebo and neutralMPH, the average change in K1 was 5%, which is unlikely to be responsible for any change seen in VT. Given the small differences in K1 observed in this study, we conclude that any changes in BPND were not due to changes in blood flow.
This study has some limitations. First, the effects of food stimulation by itself were insufficient to elicit responses that could be detected with the PET-[11C]raclopride method. We had to use a low dose of MPH, which blocks dopamine transporters, to enhance the detection of dopamine (5). Thus, we cannot rule out the possibility of a pharmacological interaction between MPH and the response to food stimulation. However, the failure to see an association between the dopamine changes induced by MPH between the two groups when given with the neutral stimulation provides evidence that the MPH effects were driven by the food stimulation condition. Second, since all the subjects received the same oral dose of MPH, the subjects with greater BMI had lower plasma MPH concentrations. However, the subjects with greater BMI did not show lower dopamine release neither for the neutral MPH nor for the food MPH conditions, which provides evidence that MPH effects were driven by the food stimulation. Third, to avoid additional arterial lines insertion, the studies were completed in 2 days, which introduces potential confounds from order effects. Fourth, the changes in the ventral striatum did not differ among the conditions, which could reflect the decreased reactivity of these subjects to the food cues that they knew they could not eat. However, the magnitude of changes in ventral striatal regions had great variability, which might result from movement during food/MPH stimulation and the structure of the region beyond the spatial resolution of the PET scanner. Since the study was done in a small number of heterogeneous subjects (different in age, gender, and BMI) we cannot rule out the possibility that the lack of a group effect in the reactivity of the ventral striatum was due to low statistical power. Another limitation was that neither did we control the time of the menstrual cycle at which the studies were performed nor did we measure gonadal hormones. The menstrual cycle could influence brain responses to food since the pattern of estradiol secretion during the ovarian cycle has been shown to affect eating behavior; e.g., women eat more during the luteal and menstrual phases than the follicular and periovulatory phases (40).
In summary, this is the first study using PET to measure brain dopamine changes during food stimulation in binge eaters. These results provide evidence of involvement of the caudate nucleus in the pathophysiology of BED. Inasmuch as binge eating is not exclusively found in obese individuals, further studies are warranted to assess the neurobiological factors that may differentiate obese and nonobese binge eaters.
ACKNOWLEDGMENTS
The positron emission tomography (PET) study was carried out at Brookhaven National Laboratory with infrastructure support from the U.S. Department of Energy OBER (DE-ACO2-76CH00016) and under support in part by the National Institute of Health: R01DA6278 (G.-J.W.), R01DA06891 (G.-J.W), Intramural Research Program of the National Institute on Alcoholism and Alcohol Abuse, Z01AA000550 (N.D.V., F.T., M.J.) and M01RR10710 (the General Clinical Research Center of Stony Brook University). The study components at St Luke’s–Roosevelt Hospital were supported in part by R01DK068603 (A.G.) and R001DK074046 (A.G.). The recruitment and psychological screening were at St Luke’s–Roosevelt Hospital. We thank David Schlyer and Michael Schueller for cyclotron operations; Donald Warner, David Alexoff and Paul Vaska for PET operations; Richard Ferrieri, Colleen Shea, Youwen Xu, Lisa Muench and Payton King for radiotracer preparation and analysis, Karen Apelskog-Torres for study protocol preparation, and Barbara Hubbard and Pauline Carter for patient care.
Footnotes
DISCLOSURE
G.-J.W. reports having received lecture fees from and research funding from Orexigen Therapeutics Inc.; J.S.F., A.G., K.G., H.H., M.J., J.L., P.S., F.T., N.D.V., C.T.W., W.Z. declared no conflict of interest.
REFERENCES
- 1.Dymek-Valentine M, Rienecke-Hoste R, Alverdy J. Assessment of binge eating disorder in morbidly obese patients evaluated for gastric bypass: SCID versus QEWP-R. Eat Weight Disord. 2004;9:211–216. doi: 10.1007/BF03325069. [DOI] [PubMed] [Google Scholar]
- 2.Geliebter A, Hassid G, Hashim SA. Test meal intake in obese binge eaters in relation to mood and gender. Int J Eat Disord. 2001;29:488–494. doi: 10.1002/eat.1047. [DOI] [PubMed] [Google Scholar]
- 3.Mietus-Snyder ML, Lustig RH. Childhood obesity: adrift in the “limbic triangle”. Annu Rev Med. 2008;59:147–162. doi: 10.1146/annurev.med.59.103106.105628. [DOI] [PubMed] [Google Scholar]
- 4.Bello NT, Hajnal A. Dopamine and binge eating behaviors. Pharmacol Biochem Behav. 2010;97:25–33. doi: 10.1016/j.pbb.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Volkow ND, Wang GJ, Fowler JS, et al. “Nonhedonic” food motivation in humans involves dopamine in the dorsal striatum and methylphenidate amplifies this effect. Synapse. 2002;44:175–180. doi: 10.1002/syn.10075. [DOI] [PubMed] [Google Scholar]
- 6.Small DM, Jones-Gotman M, Dagher A. Feeding-induced dopamine release in dorsal striatum correlates with meal pleasantness ratings in healthy human volunteers. Neuroimage. 2003;19:1709–1715. doi: 10.1016/s1053-8119(03)00253-2. [DOI] [PubMed] [Google Scholar]
- 7.Blum K, Sheridan PJ, Wood RC, et al. The D2 dopamine receptor gene as a determinant of reward deficiency syndrome. J R Soc Med. 1996;89:396–400. doi: 10.1177/014107689608900711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Volkow ND, Chang L, Wang GJ, et al. Low level of brain dopamine D2 receptors in methamphetamine abusers: association with metabolism in the orbitofrontal cortex. Am J Psychiatry. 2001;158:2015–2021. doi: 10.1176/appi.ajp.158.12.2015. [DOI] [PubMed] [Google Scholar]
- 9.Thanos PK, Michaelides M, Piyis YK, Wang GJ, Volkow ND. Food restriction markedly increases dopamine D2 receptor (D2R) in a rat model of obesity as assessed with in-vivo muPET imaging ([11C] raclopride) and in-vitro ([3H] spiperone) autoradiography. Synapse. 2008;62:50–61. doi: 10.1002/syn.20468. [DOI] [PubMed] [Google Scholar]
- 10.Galanti K, Gluck ME, Geliebter A. Test meal intake in obese binge eaters in relation to impulsivity and compulsivity. Int J Eat Disord. 2007;40:727–732. doi: 10.1002/eat.20441. [DOI] [PubMed] [Google Scholar]
- 11.Wang GJ, Volkow ND, Thanos PK, Fowler JS. Similarity between obesity and drug addiction as assessed by neurofunctional imaging: a concept review. J Addict Dis. 2004;23:39–53. doi: 10.1300/J069v23n03_04. [DOI] [PubMed] [Google Scholar]
- 12.Cameron JD, Goldfield GS, Cyr MJ, Doucet E. The effects of prolonged caloric restriction leading to weight-loss on food hedonics and reinforcement. Physiol Behav. 2008;94:474–480. doi: 10.1016/j.physbeh.2008.02.014. [DOI] [PubMed] [Google Scholar]
- 13.Carr KD. Chronic food restriction: enhancing effects on drug reward and striatal cell signaling. Physiol Behav. 2007;91:459–472. doi: 10.1016/j.physbeh.2006.09.021. [DOI] [PubMed] [Google Scholar]
- 14.Avena NM, Rada P, Hoebel BG. Sugar and fat bingeing have notable differences in addictive-like behavior. J Nutr. 2009;139:623–628. doi: 10.3945/jn.108.097584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Avena NM, Rada P, Moise N, Hoebel BG. Sucrose sham feeding on a binge schedule releases accumbens dopamine repeatedly and eliminates the acetylcholine satiety response. Neuroscience. 2006;139:813–820. doi: 10.1016/j.neuroscience.2005.12.037. [DOI] [PubMed] [Google Scholar]
- 16.Cooper Z, Cooper PJ, Fairburn CG. The validity of the eating disorder examination and its subscales. Br J Psychiatry. 1989;154:807–812. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- 17.Zung WW, Richards CB, Short MJ. Self-rating depression scale in an outpatient clinic. Further validation of the SDS. Arch Gen Psychiatry. 1965;13:508–515. doi: 10.1001/archpsyc.1965.01730060026004. [DOI] [PubMed] [Google Scholar]
- 18.Schaefer A, Brown J, Watson CG, et al. Comparison of the validities of the Beck, Zung, and MMPI Depression Scales. J Consult Clin Psychol. 1985;53:415–418. doi: 10.1037//0022-006x.53.3.415. [DOI] [PubMed] [Google Scholar]
- 19.Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7:47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- 20.Logan J, Fowler JS, Volkow ND, et al. Graphical analysis of reversible radioligand binding from time-activity measurements applied to [N-11C-methyl]-(−)-cocaine PET studies in human subjects. J Cereb Blood Flow Metab. 1990;10:740–747. doi: 10.1038/jcbfm.1990.127. [DOI] [PubMed] [Google Scholar]
- 21.Slifstein M, Narendran R, Hwang DR, et al. Effect of amphetamine on [(18)F] fallypride in vivo binding to D(2) receptors in striatal and extrastriatal regions of the primate brain: Single bolus and bolus plus constant infusion studies. Synapse. 2004;54:46–63. doi: 10.1002/syn.20062. [DOI] [PubMed] [Google Scholar]
- 22.Peciña S, Smith KS, Berridge KC. Hedonic hot spots in the brain. Neuroscientist. 2006;12:500–511. doi: 10.1177/1073858406293154. [DOI] [PubMed] [Google Scholar]
- 23.Schultz W. Neural coding of basic reward terms of animal learning theory, game theory, microeconomics and behavioural ecology. Curr Opin Neurobiol. 2004;14:139–147. doi: 10.1016/j.conb.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 24.Weiss F. Neurobiology of craving, conditioned reward and relapse. Curr Opin Pharmacol. 2005;5:9–19. doi: 10.1016/j.coph.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 25.Gerdeman GL, Partridge JG, Lupica CR, Lovinger DM. It could be habit forming: drugs of abuse and striatal synaptic plasticity. Trends Neurosci. 2003;26:184–192. doi: 10.1016/S0166-2236(03)00065-1. [DOI] [PubMed] [Google Scholar]
- 26.Vanderschuren LJ, Di Ciano P, Everitt BJ. Involvement of the dorsal striatum in cue-controlled cocaine seeking. J Neurosci. 2005;25:8665–8670. doi: 10.1523/JNEUROSCI.0925-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schultz W, Preuschoff K, Camerer C, et al. Explicit neural signals reflecting reward uncertainty. Philos Trans R Soc Lond, B, Biol Sci. 2008;363:3801–3811. doi: 10.1098/rstb.2008.0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schultz W, Tremblay L, Hollerman JR. Reward processing in primate orbitofrontal cortex and basal ganglia. Cereb Cortex. 2000;10:272–284. doi: 10.1093/cercor/10.3.272. [DOI] [PubMed] [Google Scholar]
- 29.Tricomi EM, Delgado MR, Fiez JA. Modulation of caudate activity by action contingency. Neuron. 2004;41:281–292. doi: 10.1016/s0896-6273(03)00848-1. [DOI] [PubMed] [Google Scholar]
- 30.Schienle A, Schäfer A, Hermann A, Vaitl D. Binge-eating disorder: reward sensitivity and brain activation to images of food. Biol Psychiatry. 2009;65:654–661. doi: 10.1016/j.biopsych.2008.09.028. [DOI] [PubMed] [Google Scholar]
- 31.Geliebter A, Ladell T, Logan M, et al. Responsivity to food stimuli in obese and lean binge eaters using functional MRI. Appetite. 2006;46:31–35. doi: 10.1016/j.appet.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 32.Wang GJ, Volkow ND, Telang F, et al. Exposure to appetitive food stimuli markedly activates the human brain. Neuroimage. 2004;21:1790–1797. doi: 10.1016/j.neuroimage.2003.11.026. [DOI] [PubMed] [Google Scholar]
- 33.Swanson LW. The projections of the ventral tegmental area and adjacent regions: a combined fluorescent retrograde tracer and immunofluorescence study in the rat. Brain Res Bull. 1982;9:321–353. doi: 10.1016/0361-9230(82)90145-9. [DOI] [PubMed] [Google Scholar]
- 34.Wang GJ, Volkow ND, Felder C, et al. Enhanced resting activity of the oral somatosensory cortex in obese subjects. Neuroreport. 2002;13:1151–1155. doi: 10.1097/00001756-200207020-00016. [DOI] [PubMed] [Google Scholar]
- 35.Stice E, Spoor S, Bohon C, Veldhuizen MG, Small DM. Relation of reward from food intake and anticipated food intake to obesity: a functional magnetic resonance imaging study. J Abnorm Psychol. 2008;117:924–935. doi: 10.1037/a0013600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thanos PK, Michaelides M, Gispert JD, et al. Differences in response to food stimuli in a rat model of obesity: in-vivo assessment of brain glucose metabolism. Int J Obes (Lond) 2008;32:1171–1179. doi: 10.1038/ijo.2008.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zink CF, Pagnoni G, Martin ME, Dhamala M, Berns GS. Human striatal response to salient nonrewarding stimuli. J Neurosci. 2003;23:8092–8097. doi: 10.1523/JNEUROSCI.23-22-08092.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Volkow ND, Wang GJ, Fowler JS, et al. Evidence that methylphenidate enhances the saliency of a mathematical task by increasing dopamine in the human brain. Am J Psychiatry. 2004;161:1173–1180. doi: 10.1176/appi.ajp.161.7.1173. [DOI] [PubMed] [Google Scholar]
- 39.Volkow ND, Wang GJ, Telang F, et al. Dopamine increases in striatum do not elicit craving in cocaine abusers unless they are coupled with cocaine cues. Neuroimage. 2008;39:1266–1273. doi: 10.1016/j.neuroimage.2007.09.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reed SC, Levin FR, Evans SM. Changes in mood, cognitive performance and appetite in the late luteal and follicular phases of the menstrual cycle in women with and without PMDD (premenstrual dysphoric disorder) Horm Behav. 2008;54:185–193. doi: 10.1016/j.yhbeh.2008.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]