Abstract
Pay-for-performance (P4P) strategies improve employee productivity and morale in business settings and are increasingly being implemented in medical care settings. This study investigated whether P4P could improve treatment utilization and retention at a community drug treatment clinic. Counselors had the opportunity to earn cash bonuses based on therapy attendance rates of individual clients as well as the quarterly retention rates of their caseload. Using a pre-post study design, average therapy sessions attended during the first month of treatment increased from 4.6 sessions prior to the intervention to 5.5 sessions per client during the intervention. The 90-day client retention rate increased from 40% to 53%. Additional analyses suggest that the improvement in 90-day retention was mediated by the increase in attendance during the first month of treatment. This project demonstrates that implementing a P4P incentive program in community drug abuse treatment clinics is feasible and effective at improving utilization and retention.
Keywords: Pay-for-performance, contingency management, incentives, treatment utilization, retention
1. Introduction
Pay-for-performance (P4P) incentive strategies are widely used in business settings as motivational tools for enhancing employee performance. Examples of such incentives include profit sharing, cash bonuses, or privileges for employees who individually or collectively meet specific goals. Such programs have been shown to improve employee productivity and morale (Honeywell-Johnson & Dickinson, 1999). Recently, variations on these kinds of incentive programs have been widely applied in medical care settings in the U.S. and abroad (Glickman et al., 2007; Honore, Simoes, Moonesinghe, Kirbey, & Renner, 2004; Meessen, Kashala, & Musango, 2007; Petersen, Woodard, Urech, Daw, & Sookanan, 2006; Rosenthal & Dudley, 2007). P4P incentive programs in medical settings have included bonus payments made each time a specific service is rendered to a patient or for provision of evidence-based services at a minimum rate across patients for a given period of time (Armour et al., 2001; Petersen et al., 2006). Medical P4P programs have also been applied at both the individual physician level and health center level (Armour et al., 2001; Glickman & Peterson, 2009; Petersen et al., 2006). Though the initial success of P4P programs in medical care have been mixed, there is promise that continued development of P4P programs can lead to improvements in the quality and efficiency of medical care for benefit of both patient and provider (Conrad & Perry, 2009; Glickman & Peterson, 2009; Van Herck et al., 2010).
Surprisingly, the adoption of P4P programs for the treatment of drug use disorders is lacking compared with incentive programs for the treatment of other chronic diseases such as diabetes, asthma, and cardiovascular disease. On one hand, Contingency Management (CM), an evidence-based intervention in which drug-users receive incentives for meeting specific treatment goals (e.g. abstinence), has been enormously successful for improving drug abuse treatment outcomes (cf. Higgins & Silverman, 1999; Stitzer & Petry, 2006). However, CM in this application is distinctly different from what is typically considered pay-for-performance because it is a patient-based rather than provider-based intervention (e.g. patient, not service provider, receives incentives for target behaviors/outcomes).
Performance-based contracting programs focusing on drug abuse treatment providers have been established in Delaware and Maine. In Delaware, performance-based contracts were recently developed between the state and state-funded outpatient drug abuse treatment clinics that targeted improved rates of clinic utilization (filled treatment slots) and patient treatment retention. Operating costs for each clinic are reimbursed each month at 50-100% based on patient utilization (i.e. allotted treatment slots filled), and clinics receive a $100 bonus (up to a yearly maximum) for each client that completed treatment. In a recently published study of the first 5 years of this program, clinic utilization improved from 54% to 95% and treatment completion rates improved from 53% to 70% (McLellan, Kemp, Brooks, & Carise, 2008). In Maine, each state-funded drug treatment program receives a yearly evaluation on treatment utilization, efficacy, and inclusion of special populations (e.g. adolescents, poly-drug abusers, IV drug users). Failure to meet minimum requirements on these three aspects of performance results in reduced funding levels. Analysis of data collected following the implementation of this program indicated significant increases over time on all three outcomes (Commons, McGuire, & Riordan, 1997).
One aspect of P4P that is lacking from the Delaware and Maine programs is the provision of incentives at the individual counselor level, rather than at the clinic level. Because counselor behaviors may be directly instrumental in promoting improved outcomes for clients in drug abuse treatment, provision of outcomes-based incentives to counselors could potentially improve client outcomes and could ultimately represent a more cost-effective approach to treatment outcome improvement than would direct reinforcement of client behaviors. One recent study showed that providing incentives directly to counselors based on client retention in treatment significantly improved client outcomes (Shepard et al., 2006). Specifically, retention for at least 5 sessions in an outpatient post-residential aftercare program was increased from 33% to 59% when counselors could earn a $100 bonus for each client that achieved this milestone. In a second study, an intervention consisting of graphical feedback and the opportunity to earn cash prizes was implemented in a drug treatment clinic where counselors were performing poorly in the adoption of a new treatment strategy (Andrzejewski, Kirby, Morral, & Iguchi, 2001). Counselor adherence to the treatment protocol increased from 42% to 81% following implementation of the performance-based incentive program. Of note, a significant increase was also observed (42% to 71% adherence) for counselors that received feedback without the opportunity to earn cash incentives.
The primary aim of this project was to determine whether implementation of a P4P program at a community drug treatment program could improve 90-day retention rates. The P4P intervention was comprised of cash bonuses paid to counselors based on therapy attendance of individual clients during the first two months of treatment and 90-day retention of their caseload every three months. Though the primary clinical outcome for this intervention was 90-day retention, incentives were provided for early treatment attendance in order to provide more frequent and immediate reinforcement of client treatment engagement. These attendance-centered endpoints were chosen because they are easy and cost effective outcomes. Also, client retention rates are an important metric in the evaluation of treatment programs, and previous research has demonstrated that increased frequency and amount of therapy exposure is positively correlated with desirable treatment outcomes such as drug abstinence (Fiorentine & Anglin, 1996; Fiorentine, 2001). Our hypothesis was that the counselor incentive program would result in improved attendance and retention rates, and that the improvement in 90-day retention would be mediated by improved early treatment engagement.
2. Materials and methods
2.1. Clinical Site
The project was conducted as a quality improvement initiative at an outpatient psychosocial counseling treatment center located in Baltimore, Maryland. The study center has an outpatient census of approximately 150 adult clients whose drug use included alcohol, marijuana, cocaine, opiates or some combination. Most clients were referred from the criminal justice system (about 70%), mainly for DUI, drug possession, or domestic violence offences. The standard treatment plan for the clinic required that all clients attend 1 individual and 1-2 group counseling sessions per week for the first month. During the second and third month, the expectation was 2 group counseling sessions per week and twice monthly individual sessions. Treatment duration was targeted for 180 days, but 90-day client retention was a vital outcome statistic monitored by the clinic's funding agency.
2.2. Participants
During the two-year study period, 11 counselors, 9 masters-level interns and a clinical supervisor worked at the treatment center. Among the counselors, 5 had full and 6 had partial adult caseloads. Full-time caseloads were generally 25-30 clients, part-time caseloads were 12 -18 clients, and interns typically had caseloads of 1-4 clients. The entire clinical staff provided services to a total of 470 clients (196 baseline; 274 intervention) between November of 2007 and August of 2009. The total treated by full and part time counselors was 426 (165 during baseline and 261 during intervention; 90.6% of all clients), with the remainder treated by interns. Seven of the 11 counselors participated during the baseline phase (with > 2 clients) and 10 of 11 during the intervention phase (see Table 1 for counselor characteristics). Five counselors who had full caseloads during both the baseline and intervention periods provided the opportunity for a within-subject analysis. These 5 provided services to a total of 289 clients (117 baseline, 172 intervention; 61.5% of all clients).
Table 1. Counselor Demographics.
| Counselor | Gender | Age | Race | Degree | Years in Field | Adult Caseload | Number of Clients | |
|---|---|---|---|---|---|---|---|---|
| Baseline | Incentives | |||||||
| 1 | Female | 25 | C | Bachelors | 4 | Full | 18 | 54 |
| 2 | Male | 55 | C | Associates | 17 | Full | 40 | 43 |
| 3 | Female | 26 | C | Masters | 2 | Part | 17 | 34 |
| 4 | Female | 33 | C | Masters | 7 | Full | 29 | 29 |
| 5 | Female | 34 | C | Masters | 10 | Part | 13 | 12 |
| 6 | Male | 28 | AA | Masters | 1 | Full | 0 | 27 |
| 7 | Male | 38 | AA | Masters | 8 | Part | 2 | 22 |
| 8 | Female | 48 | C | Associates | 3 | Part | 1 | 17 |
| 9 | Female | 47 | AA | Masters | 3 | Part | 0 | 14 |
| 10 | Female | 63 | C | Masters | 4 | Part | 18 | 9 |
| 11 | Male | 48 | C | Bachelors | 5 | Full | 18 | 0 |
| Total Clients | 165* | 261* | ||||||
Note that student interns accounted for remaining sample
As seen in Table 1, counselors were primarily female (71%) and Caucasian (71%). Ninety percent had earned bachelors-level degrees (BA, BSW, BTPS), 48% had masters-level degrees (MA, MSW), and 67% had attained additional certifications in addictions counseling (CAC-AD, LCADC, LCPC, LGSW).
Verbal consent to participate was obtained from clinic counselors and interns, and the procedures followed were approved by the Johns Hopkins University IRB and conducted in accord with the Helsinki Declaration of 1975.
2.3. Study Design
The study was conducted using a pre-post study design, which consisted of two consecutive 9-month periods, an initial baseline period (11/1/07 to 7/31/08) followed by a pay-for-performance intervention period (11/1/08 to 7/31/09). Retention was tracked to 90 days for all clients enrolled during these periods.
2.4. Study Procedures
Baseline
Treatment as usual was in effect during the entire baseline period. Clients were assigned a primary counselor at intake and followed the standard treatment expectations described above.
P4P intervention
The P4P incentive program targeted two distinct endpoints, 1) number of individual and group therapy sessions attended by clients, and 2) rate of client retention for at least 90 days. Although clients were generally expected to attend 2-3 therapy sessions per week, clinic records prior to the study indicated that actual attendance was once per week on average. Based on this information, targeted attendance rate during the first 2 months of treatment for counselor incentives was set at 5 or more therapy sessions per month (any combination of individual and group). Counselors received a bonus of $10 for each client who had attended 5 - 6 therapy sessions in one month and $25 for each client who attended 7 or more therapy sessions (twice weekly attendance would be about 8 sessions per month). Attendance bonuses were paid to counselors during the client's first 2 months in treatment. Thus, counselors had the opportunity to earn up to $50 per client based on attendance. Attendance bonuses were paid out weekly in cash for clients in each counselor's caseload who had reached their 30 or 60 day treatment milestones during the prior week.
In addition to the attendance bonuses, counselors were eligible to earn bonuses based on 90-day retention rates of their caseload. In order to avoid treatment termination and be coded as retained for 90 days, clients needed to attend at least one session in any given 30 day period and to complete one session on or after Day 90 of treatment. Retention criteria for the study was based on 90-day retention benchmarks that had been set at 65% by the local block grant funding agency. Full-time counselors were eligible for quarterly cash bonuses of $100, $150, $175, or $200 if the retention rate of each 3-month cohort of their own clients met target benchmarks of 65%, 75%, 85%, or 95% retention respectively. For counselors with partial adult caseloads, retention bonuses were to be paid at 6-month intervals. Thus, they were eligible for half the bonus amounts available to full time counselors because of smaller caseloads. Interns with very small caseloads (typically 1-4 clients) could earn a $15 bonus for each client retained for 90 days.
During the P4P intervention period, researchers (not employed by the clinic) reviewed the clinic database to update reports detailing client enrollment and attendance, and to determine counselor eligibility for performance bonuses. Researchers then met with counseling staff each week during a regularly scheduled treatment team meeting. At this meeting, each counselor received a report detailing attendance over time (0 - 90 days) for each client in their active caseload and performance-based cash bonuses earned that week. The dispensing of reports and incentives also set the occasion to provide feedback to all counselors regarding attendance and retention at the clinic in general and to stimulate discussion of strategies for improving client engagement. Counselors who had high attendance rates or showed improvement were asked to share strategies they employed to engage clients in treatment with other counselors (e.g. welcome packets, written and telephone appointment reminders, incentives/recognition for attendance or reaching treatment milestones). Similarly, counselors were encouraged to identify clients with sporadic or poor attendance records and to focus treatment engagement efforts on those clients specifically.
Data collection
During each 9-month period, attendance at individual and group therapy sessions was tracked for 90 days for every client admitted to treatment (admission occurred for those who attended at least one therapy session following an initial intake assessment). Early treatment discharges occurred for clients following 30 days with no face-to-face contact or who required referral to a higher level of care (e.g. inpatient or methadone maintenance treatment). Group attendance information was obtained from group sign-in sheets and individual session data from client charts, where counselors recorded each contact and wrote a contact note. With regard to tracking client attendance, there was essentially no change in the day-to-day operation at the clinic during the study.
2.5. Data Analysis
Data analysis was first conducted with all enrolled clients (N = 196) during the 9-month baseline period and all enrolled clients (N=274) during the 9-month pay-for-performance intervention period. Though incentives were provided for attendance during the first 60 days of treatment, analysis of attendance results was limited to the first 30 days due to the increasing impact of client drop out on attendance rates after the first month. Specifically, data from the second month of treatment would suffer from selection bias, whether discharged clients were excluded (attendance inflation) or discharged clients (who had no opportunity to attend) were counted as having not attended (attendance deflation). An independent-samples t-test was conducted to compare days of therapy attendance during the first 30 days of treatment across study conditions and Chi-Square tests were performed to examine client characteristics across the two study cohorts and the distribution of clients attending 1-3, 4-6 and 7 or more sessions. Retention rates at 90-days were compared for client cohorts enrolled during the baseline and intervention periods using Chi Square. The above analyses were also performed for the reduced sample of 5 counselors who provided services during both baseline and incentive phases to ensure that any changes observed were not simply due to changes in clinic personnel.
A mediation analysis was conducted to determine if the impact of counselor incentives on 90-day retention was mediated by attendance during the first month. The mediation analysis used the equations from MacKinnon and Dwyer (1993) for the case of mediation with dichotomous variables. The Aroian version of the Sobel test, as popularized by Baron and Kenny (1986), is reported. The mediation analysis was conducted with the full sample and repeated with the subset of clients who were retained in treatment beyond 30 days due to the impact of early drop out on retention at subsequent time points. Data analysis was conducted using SPSS statistical software (Version 16), and α = .05 for all tests of statistical significance.
3. Results
3.1. Client characteristics
Client characteristics across the two study cohorts are provided in Table 2. No significant differences in client demographics were observed for gender, race/ethnicity, treatment referral source, or primary drug of concern entering treatment.
Table 2. Client demographic characteristics by study cohort.
| Baseline (N=196) | P4P Incentive (N=274) | |
|---|---|---|
| Gender (% male) | 79% | 83% |
| Race/Ethnicity | ||
| Caucasian | 18% | 19% |
| African American | 81% | 80% |
| Other | 1% | 1% |
| Referred by Criminal Justice | 79% | 83% |
| Primary Drug Used | ||
| Alcohol | 49% | 52% |
| Marijuana | 22% | 21% |
| Opiates | 13% | 13% |
| Cocaine | 15% | 13% |
| Other Drugs | 1% | 1% |
3.2. Attendance during the first 30 days
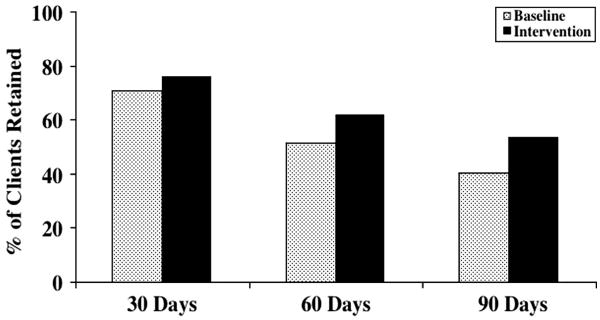
The average number of sessions attended during the first 30 days of treatment for the intent to treat sample increased from 4.6 (SD = 2.7) during baseline to 5.5 (SD = 2.9) during the incentive intervention (t = -3.40, p < .01). A similar outcome was observed when analysis was limited to the 5 counselors who provided full-time therapy services during the baseline and intervention periods, with mean sessions attended increasing from 4.8 (SD = 2.8) during baseline to 6.2 (SD = 2.9) during the P4P intervention (t = -4.05, p < .01). Table 3 shows that an increase in sessions attended was observed for all individual counselors who had at least 5 clients in each study condition except for counselor # 10. Figure 1 shows the distribution of client attendance during the first 30 days of treatment. During baseline, 71% of clients attended 3 or more sessions, 50% of clients attended 5 or more sessions and 25% attended 7 or more sessions. During the intervention attendance increased with 80% of clients attending 3 or more sessions, 61% attending 5 or more and 39% attending 7 or more sessions. A chi square test comparing the distribution of clients attending 1-3, 4-6 and 7 or more sessions showed that this shift in distribution of attendance was significant (χ2 = 12.12, p < .01).
Table 3. Client Attendance and Retention by Counselor.
| Counselor | Baseline | Intervention | ||||
|---|---|---|---|---|---|---|
| Number of clients | Sessions attended first 30 days* | Percent retained 90 days | Number of Clients | Sessions attended first 30 days* | Percent retained 90-days | |
| 1 | 18 | 4.4 (2.2) | 39% | 54 | 6.3 (3.2) | 54% |
| 2 | 40 | 4.7 (2.4) | 48% | 43 | 6.7 (3.1) | 67% |
| 3 | 17 | 3.5 (2.2) | 41% | 34 | 5.4 (2.6) | 56% |
| 4 | 29 | 5.8 (3.4) | 55% | 29 | 6.2 (2.8) | 59% |
| 5 | 13 | 5.2 (3.1) | 39% | 12 | 5.8 (2.3) | 67% |
| 6 | 0 | N/A | N/A | 27 | 5.2 (2.0) | 48% |
| 7 | 2 | 5.5 (0.7) | 100% | 22 | 2.8 (1.9) | 36% |
| 8 | 1 | 2.0 | 0% | 17 | 5.1 (2.1) | 59% |
| 9 | 0 | N/A | N/A | 14 | 5.0 (2.2) | 43% |
| 10 | 18 | 3.6 (2.5) | 33% | 9 | 2.8 (1.9) | 33% |
| 11 | 18 | 4.8 (2.4) | 39% | 0 | N/A | N/A |
Mean (± SD)
Figure 1.
Client therapy attendance during the first 30 days of treatment during 9-month baseline and intervention study phases.
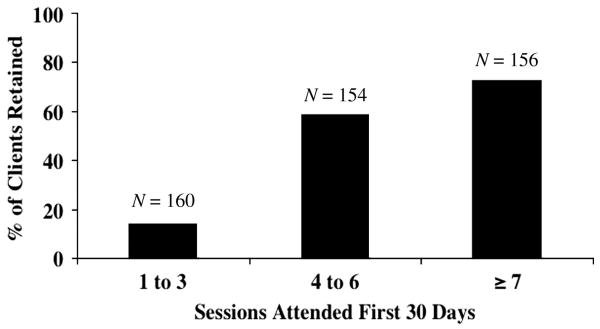
3.3. Treatment retention
Figure 2 shows treatment retention in the two study periods at 30, 60 and 90-day milestone time points. Data analysis indicated that 90-day retention significantly increased from 40% during baseline to 53% during the P4P intervention (χ2 = 4.846, p < .05). In addition, Table 3 shows that 90-day retention rates improved from baseline to intervention for all but one (#10) counselor who had caseloads in both study conditions.
Figure 2.
Client 90-day retention rates during 9-month baseline and intervention study phases.
3.4. Money earned
During the incentive intervention, at total of $7590 was paid out to counselors and interns. Of this, $7020 (93% of total) was paid for attendance bonuses and the remainder for retention bonuses. Each counselor, and all but 2 interns, earned a bonus during the program. A majority of the bonus money (97%) was paid to counselors. The average amount earned per counselor during the 9-month intervention was $738.50 (range = $75 - $1765; median = $535).
3.5. Mediation analysis
Our hypothesis was that any increase in 90-day retention would be mediated by increased early treatment attendance rates of individual clients. As described above, both attendance and retention improved during the intervention. In the mediation model conducted with the intent to treat sample (N = 470), the P4P intervention was significantly associated with attendance during the first 30 days (a = 0.887, SE(a) = 0.261, p < .01), attendance during the first 30 days was significantly associated with 90-day retention controlling for the P4P intervention (b = 0.428, SE(b) = 0.045, p < .01), and the P4P intervention was significantly associated with 90-day retention without controlling for attendance during the first 30 days (c = 0.524, SE(c) = 0.189, p < .01), but not when attendance during the first 30 days was controlled for (c' = 0.287, SE(c') = 0.217, p = .186). The Sobel test was also significant for the intent to treat sample (Sobel = 3.18, p < .01). The mediating relationship between attendance and retention was similarly significant with those who left treatment prior to 30 days excluded (N = 348; Sobel = 2.22, p < .05), and when only data from the 5 counselors providing services during both study phases were considered (all clients, N = 289, Sobel = 3.59, p < .01; excluding those who left treatment prior to 30 days, N = 221, Sobel = 2.91, p < .01). Figure 3 depicts the relationship between attendance during the first 30 days and retention at 90 days for the full sample. The same relationship was seen when analysis was conducted excluding those who left treatment prior to 30 days. In that sample, 33% of those who attended 1-3 sessions in the first 30 days (N = 67) were retained for 90 days compared with 69% of those who attended 4-7 sessions (N = 130) and 75% of those who attended >7 sessions (N = 151).
Figure 3.
Client 90-day retention rates as a function of therapy attendance rates during the first 30 days of treatment.
4. Discussion
In the present study we assessed rates of clinic attendance during the first 30 days of treatment and its relationship to 90-day retention rates at a community substance abuse treatment clinic. These rates were examined during a baseline period of usual care and during a period when counselors were able to earn cash bonuses based on client attendance early in treatment as well as bonuses based on caseload retention. Compared with the baseline period, client therapy attendance during the first 30 days of treatment and 90-day retention rates were both significantly improved when clinic counselors could earn pay-for-performance incentives.
The mean number of sessions attended during baseline reflected historical trends at this particular clinic, where clients, who are expected to attend twice per week, in fact attend about once per week on average. The mean number of therapy sessions attended was increased by 1 session per month by the counselor incentive intervention. At face value this is not a dramatic increase. However, it may nevertheless represent an important improvement both in terms of opportunities to strengthen early engagement of clients and in terms of billing opportunities in clinics where fee-for-service billing models are operative.
Retention to 90-days was also improved in this study from 40% to 53% for all clients entering treatment. It is questionable, however, whether the 90-day caseload retention bonus offered as an incentive to counselors had a direct impact on client retention since few counselors earned the retention bonus. In hindsight, the retention benchmark (65% at 90-days) was not a realistic goal, though it was endorsed by the clinic director and counselors at the beginning of the study. It is possible that an independent impact of retention bonuses might be seen if the benchmark goal had been set at a lower level. A study by Sheppard et al. (2006) had previously shown that client retention bonuses could be an effective intervention in an outpatient post-residential aftercare program. In that study, counselors could earn a $100 bonus for each client who stayed in treatment for 5 sessions. The two protocols have some overlap in that a 5-session attendance benchmark was also used in the present study. The difference was the time constraint in our study whereby these sessions had to be attended within a 30-day window for the counselor to qualify for a bonus payment. Interestingly, outcomes from the two studies were similar in that the percentage of clients attending 5 sessions increased (33% to 59% in Sheppard et al. study, versus 50% to 61% in this study; see Figure 1), despite marked differences in the payment protocols and in baseline rates of clients attending 5 or more sessions.
That retention was improved despite the low rate at which retention bonuses were earned is consistent with our hypothesis that there would be a strong association between early treatment attendance and later treatment retention. This relationship was demonstrated for the full sample (Figure 3) and remained significant when clients discharged within the first 30 days of treatment (which would limit therapy attendance opportunity) were omitted from the analysis. Further, we were able to conclude that frequency of attendance early in treatment mediated the effect of the P4P intervention on retention at 90-days. This outcome suggests that therapy attendance, particularly early in treatment, may be a more optimal target for intervention than is retention per se. This makes sense from a theoretical standpoint because attendance is a more frequent, observable, and proximal outcome than retention. Further, the data in Figure 3 suggest that a week without clinical contact early in treatment (i.e. 1-3 contacts during the first 30 days) indicates a high risk of treatment dropout and should be addressed by the clinic team for enhanced intervention.
Counselors appreciated the opportunity to earn incentives during the study and became actively engaged in discussing the strategies they employed to encourage client engagement. Strategies included providing welcome packets for clients at intake, engaging in more outreach efforts (phone calls; letters) both before appointments and after missed appointments, and scheduling more individual appointments with clients. Identifying and promoting effective strategies for early client engagement is an on-going challenge for substance abuse treatment programs (Capoccia et al., 2007; McCarty, Gustafson, Capoccia, & Cotter, 2009). It would be possible to provide incentives to counselors for performing these activities rather than for client attendance outcomes. However, the latter strategy is clearly more complex and challenging to implement. P4P in this case would appear to be a more straightforward means to an end, but an assessment of the relative efficacy of that more complex approach, compared with the more simplistic approach used in this study, would need to be investigated.
The costs of any P4P program will depend on the size and frequency of bonuses offered. In the present study, $7590 was paid in performance bonuses to achieve a one-session increase in attendance among 274 clients. This averaged to a cost of $28 per session. In this clinic, the reimbursement rate for a therapy session exceeded $28, thus the intervention was cost-effective. It is possible that an incentive program with smaller bonuses would be effective, as has been the case when lower value abstinence incentive programs have been offered to substance abuse clients (Petry & Martin, 2002), but it is important to ensure that incentives remain salient and attractive or they will no longer affect behavior. Clearly, more research will be needed to determine optimal strategies (counselor versus program wide bonuses), schedules of reinforcement, and performance targets for P4P programs in substance use treatment settings. Not only should retention and attendance be considered (both separately and combined) as targets for future research, but also the possibility of directly reinforcing counselor behaviors such as phone calls to clients that may result in improved appointment keeping should be considered. Finally, the costs and benefits of reinforcing counselors for client behavior as compared with reinforcing clients directly for desired behavior change will need to be evaluated in future work on this topic.
In this study, incentive bonuses were paid to counselors based on their individual performance, rather than to the treatment team or clinic as a whole. This decision was made primarily because there was concern that a group approach could result in diffusion of responsibility among counselors, or that missed incentive benchmarks due to poor performance by one counselor could strain relations with others. Future research could compare individual versus group-based approaches to determine comparative efficacy and whether any of these concerns are legitimate.
The limitations of this study include the single clinic site and the pre-post design, which does not allow for control of extraneous time-related variables. That similar findings were observed in both the between group and within-subjects (5 counselors present during both study phases) analyses helps to support validity of the conclusions. Nonetheless, because there was no control group for which attendance was tracked during the same time period, it is not certain if other unrelated variables could have contributed to the differences observed. The relative impact of incentives versus other components of the intervention is also not known. Counselors received regular feedback about their clients' attendance during the incentive period that was not delivered consistently during the baseline period. Previous research has demonstrated that providing feedback to counselors on behavior adherence can result in improved counselor performance (Andrzejewski et al., 2001). In addition to feedback, counselors attended brainstorming sessions about methods of improving client attendance and shared strategies with one another. In the present study, it was not possible to individually assess the impact of the monetary incentives, feedback, or brainstorming sessions on attendance or retention outcomes. A final limitation is that no systematic measures were obtained over time of either counselor attitudes or specific counselor behaviors that may have resulted in improved attendance of clients during the intervention. One unlikely adverse behavior would be counselors inappropriately discharging clients early in order to earn more money from newly admitted clients. This is unlikely because all client discharges were subject to review by the clinic director or supervisor. It will be interesting and important to include counselor-based process measures in future studies of this type.
In conclusion, this is one of the first studies to demonstrate an improvement in desirable client behavior as a result of a P4P intervention with substance abuse counselors. The intervention targeted increased early attendance of clients and was effective in increasing the average number of sessions attended during the first 30 days of treatment. Further, a strong relationship was demonstrated between improved early attendance and subsequent 90-day retention. This suggests that reinforcement of early attendance, either through counselor or client directed incentive programs, will result in improved long-term treatment retention, and possibly better long-term clinical outcomes. In conjunction with the recent study by Sheppard et al. (Shepard et al., 2006), the present research suggests that providing performance-based incentives to drug abuse treatment counselors can improve client treatment engagement. This approach to improving drug treatment utilization is desirable because it is based on established behavioral principles, provides a mechanism to encourage the adoption of evidence-based practices (EBP's) by counselors, and may improve the traditionally high rate of staff turnover in publicly funded substance abuse treatment clinics. Future studies on the impact of performance-based incentive interventions targeting drug treatment providers need to include control conditions to isolate the effect of incentives and measures of counselor behavior change that result from the interventions. Studies are also needed to characterize the effects of different performance milestones and incentive magnitudes, the use of a single benchmark versus a graduated incentive scale, and the use of various schedules of incentive delivery. Finally, studies need to ascertain the relative cost effectiveness of incentive programs directed to staff versus clients. Such studies will help ascertain the relative cost-benefit outcomes of different approaches and will inform clinical use based on the variety of budgetary constraints encountered by treatment providers.
Acknowledgments
This research was supported by National Institute on Drug Abuse (NIDA) grants U10-DA13034 and T32-07209. The authors would like to thank Jeannie Fry and Maggie Klinedinst for valuable research support, Linda Felch for statistical consulting, and the staff and clients of the Harbel Prevention & Recovery Center.
References
- Andrzejewski ME, Kirby KC, Morral AR, Iguchi MY. Technology transfer through performance management: the effects of graphical feedback and positive reinforcement on drug treatment counselors' behavior. Drug and Alcohol Dependence. 2001;63(2):179–186. doi: 10.1016/s0376-8716(00)00207-6. [DOI] [PubMed] [Google Scholar]
- Armour BS, Pitts MM, Maclean R, Cangialose C, Kishel M, Imai H, et al. The effect of explicit financial incentives on physician behavior. Archives of Internal Medicine. 2001;161(10):1261–1266. doi: 10.1001/archinte.161.10.1261. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Capoccia VA, Cotter F, Gustafson DH, Cassidy EF, Ford JH, 2nd, Madden L, et al. Making “stone soup”: improvements in clinic access and retention in addiction treatment. Joint Commission Journal on Quality and Patient Safety. 2007;33(2):95–103. doi: 10.1016/s1553-7250(07)33011-0. [DOI] [PubMed] [Google Scholar]
- Commons M, McGuire TG, Riordan MH. Performance contracting for substance abuse treatment. Health Services Research. 1997;32(5):631–650. [PMC free article] [PubMed] [Google Scholar]
- Conrad DA, Perry L. Quality-based financial incentives in health care: can we improve quality by paying for it? Annual Review of Public Health. 2009;30:357–371. doi: 10.1146/annurev.publhealth.031308.100243. [DOI] [PubMed] [Google Scholar]
- Fiorentine R. Counseling frequency and the effectiveness of outpatient drug treatment: revisiting the conclusion that “more is better”. American Journal on Drug and Alcohol Abuse. 2001;27(4):617–631. doi: 10.1081/ada-100107659. [DOI] [PubMed] [Google Scholar]
- Fiorentine R, Anglin MD. More is better: counseling participation and the effectiveness of outpatient drug treatment. Journal of Substance Abuse Treatment. 1996;13(4):341–348. doi: 10.1016/s0740-5472(96)00109-2. [DOI] [PubMed] [Google Scholar]
- Glickman SW, Ou FS, DeLong ER, Roe MT, Lytle BL, Mulgund J, et al. Pay for performance, quality of care, and outcomes in acute myocardial infarction. Journal of the American Medical Association. 2007;297(21):2373–2380. doi: 10.1001/jama.297.21.2373. [DOI] [PubMed] [Google Scholar]
- Glickman SW, Peterson ED. Innovative health reform models: pay-for-performance initiatives. American Journal of Managed Care. 2009;15(10 Suppl):S300–305. [PubMed] [Google Scholar]
- Higgins ST, Silverman K. Motivating behavior change among illicit-drug abusers: Research on contingency-management Interventions. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- Honeywell-Johnson JA, Dickinson AM. Small group incentives: A review of the literature. Journal of Organizational Behavior Management. 1999;19:89–120. [Google Scholar]
- Honore PA, Simoes EJ, Moonesinghe R, Kirbey HC, Renner M. Applying principles for outcomes-based contracting in a public health program. Journal of Public Health Management and Practice. 2004;10(5):451–457. doi: 10.1097/00124784-200409000-00013. [DOI] [PubMed] [Google Scholar]
- Kirby KC, Benishek LA, Dugosh KL, Kerwin ME. Substance abuse treatment providers' beliefs and objections regarding contingency management: Implications for dissemination. Drug and Alcohol Dependence. 2006;85:19–27. doi: 10.1016/j.drugalcdep.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Lamb RJ, Morral AR, Kirby KC, Iguchi MY, Galbicka G. Shaping smoking cessation using percentile schedules. Drug and Alcohol Dependence. 2004;76:247–259. doi: 10.1016/j.drugalcdep.2004.05.008. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17:144–158. [Google Scholar]
- McCarty D, Gustafson D, Capoccia VA, Cotter F. Improving care for the treatment of alcohol and drug disorders. Journal of Behavioral Health Services and Research. 2009;36(1):52–60. doi: 10.1007/s11414-008-9108-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Kemp J, Brooks A, Carise D. Improving public addiction treatment through performance contracting: the Delaware experiment. Health Policy. 2008;87(3):296–308. doi: 10.1016/j.healthpol.2008.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meessen B, Kashala JP, Musango L. Output-based payment to boost staff productivity in public health centres: contracting in Kabutare district, Rwanda. Bulletin of the World Health Organization. 2007;85(2):108–115. doi: 10.2471/BLT.06.032110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen LA, Woodard LD, Urech T, Daw C, Sookanan S. Does pay-for-performance improve the quality of health care? Annals of Internal Medicine. 2006;145(4):265–272. doi: 10.7326/0003-4819-145-4-200608150-00006. [DOI] [PubMed] [Google Scholar]
- Petry N, Martin B. Lower-cost contingency management for treating cocaine and opioid abusing methadone patients. Journal of Consulting and Clinical Psychology. 2002;70(2):398–405. doi: 10.1037//0022-006x.70.2.398. [DOI] [PubMed] [Google Scholar]
- Rosenthal MB, Dudley RA. Pay-for-performance: will the latest payment trend improve care? Journal of the American Medical Association. 2007;297(7):740–744. doi: 10.1001/jama.297.7.740. [DOI] [PubMed] [Google Scholar]
- Shepard DS, Calabro JA, Love CT, McKay JR, Tetreault J, Yeom HS. Counselor incentives to improve client retention in an outpatient substance abuse aftercare program. Administration and Policy in Mental Health. 2006;33(6):629–635. doi: 10.1007/s10488-006-0054-2. [DOI] [PubMed] [Google Scholar]
- Silverman KS, Chutuape MAD, Bigelow GE, Stitzer ML. Voucher-based reinforcement of cocaine abstinence in treatment-resistant methadone patients: Effects of reinforcement magnitude. Psychopharmacology. 1999;146:128–138. doi: 10.1007/s002130051098. [DOI] [PubMed] [Google Scholar]
- Stitzer M, Petry N. Contingency management for treatment of substance abuse. Annual Review of Clinical Psychology. 2006;2:411–434. doi: 10.1146/annurev.clinpsy.2.022305.095219. [DOI] [PubMed] [Google Scholar]
- Vandrey R, Bigelow GE, Stitzer ML. Contingency management in cocaine abusers: a dose-effect comparison of goods-based versus cash-based incentives. Experimental and Clinical Psychopharmacology. 2007;15(4):338–343. doi: 10.1037/1064-1297.15.4.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Herck P, De Smedt D, Annemans L, Remmen R, Rosenthal MB, Sermeus W. Systematic review: Effects, design choices, and context of pay-for-performance in health care. BMC Health Services Research. 2010;10:247:1–13. doi: 10.1186/1472-6963-10-247. [DOI] [PMC free article] [PubMed] [Google Scholar]