Abstract
To determine whether African American women expecting their first infant carry a disproportionate burden of posttraumatic stress disorder morbidity, we conducted a comparative analysis of cross-sectional data from the initial psychiatric interview in a prospective cohort study of posttraumatic stress disorder effects on childbearing outcomes. Participants were recruited from maternity clinics in three health systems in the Midwestern USA. Eligibility criteria were being 18 years or older, able to speak English, expecting a first infant, and less than 28 weeks gestation. Telephone interview data was collected from 1,581 women prior to 28 weeks gestation; four declined to answer racial identity items (n =1,577), 709 women self-identified as African American, 868 women did not. Measures included the Life Stressor Checklist, the National Women’s Study Posttraumatic Stress Disorder Module, the Composite International Diagnostic Interview, and the Centers for Disease Control’s Perinatal Risk Assessment Monitoring System survey. The 709 African American pregnant women had more trauma exposure, posttraumatic stress disorder symptoms and diagnosis, comorbidity and pregnancy substance use, and had less mental health treatment than 868 non-African Americans. Lifetime prevalence was 24.0% versus 17.1%, respectively (OR=1.5, p=0.001). Current prevalence was 13.4% versus 3.5% (OR=4.3, p< 0.001). Current prevalence of posttraumatic stress disorder (PTSD) was four times higher among African American women. Their risk for PTSD did not differ by sociodemographic status, but was explained by greater trauma exposure. Traumatic stress may be an additional, addressable stress factor in birth outcome disparities.
Keywords: Posttraumatic stress disorder, African American, Pregnancy, Health disparity
Introduction
Recent reviews of risk for posttraumatic stress disorder (PTSD) by race have, by and large, shown that African Americans are not at increased risk for onset of the disorder, but are at increased risk for persistent disorder (Breslau et al. 2005). PTSD onset in women occurs in relation to the peak incidence of trauma exposure, in the 16–20 year-age range (Breslau 2001). This period of vulnerability generally precedes childbearing, but by less time for African Americans due to their younger mean age at first birth (Mathews and Hamilton 2002). Thus, PTSD may affect pregnant African American women more than others due both to an intersection of their greater risk of chronicity and their decreased time available for remission prior to pregnancy. Other risk factors, including increased risk for trauma exposures and decreased resources for treatment could also play a role. Understanding race-specific risk for PTSD during pregnancy is an important research question not only for the sake of addressing women's mental health, but also because PTSD may be an additional, addressable factor in preterm birth disparities via the HPA axis.
PTSD is associated with physical comorbidity in women across the lifespan (Seng et al. 2006). It also has been associated with some pregnancy complications and with adverse outcomes in preliminary (Seng et al. 2001) and small-sample studies (King et al. 2005; Engel et al. 2005; Rosen et al. 2007). Our on-going study of the effects of PTSD on childbearing outcomes (NIH NR008767, PI Seng) found higher rates of current PTSD among the African American (AA) women, 13.4% versus 3.5% for non-African American (non-AA) women (Seng et al. 2009). This higher risk occurred for the AA women across socioeconomic strata. This parallels the risk pattern for preterm birth, which also affects AA women regardless of income or education levels.
PTSD is a stress-related disorder that is associated with dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis generally and in pregnancy (Shalev et al. 2008; Seng et al. 2008; King et al. 2008). Biologic stress is considered one of the four confirmed pathways to preterm birth (Green et al. 2005) due to the generation of placental and fetal membrane-derived corticotrophin-releasing hormone when stress is elevated. This in turn augments placental estrogen and fetal adrenal cortisol production. Analysis of cortisol data from our sample of pregnant women found an interaction of socio-demographic disadvantage, including African American race, and PTSD to be associated with the highest cortisol levels (King et al. 2008); a finding which suggests that stressful contexts, trauma exposures, and their mental health sequelae may all contribute to adverse outcomes via the HPA axis.
Although there are very consistent findings about African Americans' risk for preterm birth, the accumulating studies of race as a risk factor for PTSD in women have had more mixed results. A US epidemiological study of adolescents found greater risk for PTSD among African American girls (Kilpatrick et al. 2003). Conversely, other studies of young women have found no differences in PTSD rate by race (Vogel and Marshall 2001), or lower rates among African American women in comparison to white women (Seng et al. 2005; Breslau et al. 2006). Three previous studies of PTSD and race among pregnant women show similar rates between groups, including a community sample of low-income pregnant women (Smith et al. 2006), a multi-site sample of Medicaid-eligible pregnant women (Cook et al. 2004), and a sample of pregnant women assessed for PTSD and risk for preterm birth (Rogal et al. 2007). However, the samples in these studies are homogeneously low income, thus the effects of race in relation to differential socioeconomic risk could not be teased out. Therefore, it is currently unclear whether pregnant African American women are at greater, similar, or decreased risk for PTSD in comparison to other women and, importantly, whether risk for PTSD can help explain disparate birth outcomes among African American infants.
The purpose of this paper is to provide detailed race-stratified analysis comparing African American pregnant women and their non-AA counterparts and to examine predictors of lifetime prevalence and pregnancy incidence of PTSD. We will describe our sample's sociodemographic characteristics, trauma histories, and PTSD profiles. We include depression and anxiety disorder diagnoses because these are prevalent comorbidities with PTSD generally (Kessler et al. 1995) and in previous perinatal studies (Cook et al. 2004; Seng et al. 2009; Smith et al. 2006). Furthermore, although there has been considerable attention to prenatal depression in recent years, these studies generally have not considered the extent to which depressed pregnant women may be affected by previous or concurrent trauma exposures or the extent to which depression may be a comorbidity of PTSD, making it a trauma-related secondary disorder. Substance use in pregnancy, the use of PTSD-specific coping strategies, and pre-pregnancy mental health treatment are also described. We will then examine the relative contributions of sociodemographic risk factors and trauma history factors to the risk for developing PTSD (lifetime diagnosis) and for meeting diagnostic criteria in early pregnancy (current diagnosis).
Materials and methods
This study is part of a larger prospective cohort study of effects of PTSD on obstetric and postpartum mental health and attachment outcomes among women expecting their first child (Psychobiology of PTSD & Adverse Outcomes of Childbearing, NIH NR008767; common name “the STACY project”). A convenience sample of participants was recruited from maternity clinics that are a part of three large health systems in the Midwestern USA. One of the systems serves a university town; two serve an urban area. The Institutional Review Boards of the three health systems involved in the study gave approval for this project. Recruitment occurred from August 2005 to July 2008. Follow-up through 6 weeks postpartum concluded in March 2009. Full details of the recruitment process and survey procedures are presented elsewhere (Seng et al. 2009), but a brief description of key information is provided here.
Obstetric clinic nurses in the three health systems identified eligible women after conducting intake patient history clinical interviews. Eligible women were then invited to participate in a telephone survey “about stressful events that happen to women, emotions, and pregnancy.” Eligibility criteria were being 18 years or older, having the ability to speak English without an interpreter, expecting a first infant, and entering prenatal care at less than 28 weeks gestation. Interested eligible women (n=2,689) gave contact information and took a copy of the IRB-approved informed consent information document. A research survey organization (DataStat, Ann Arbor, Michigan) conducted the verbal informed consent process with eligible women they could reach (n=1,653) at the beginning of the 30–40-min structured computer-assisted telephone interview. These interviews were conducted by a small cadre of professional research interviewers who had received project-specific training and were supervised for quality of the interaction and accuracy of data entry in 10% of all interviews across the life of the project. The initial interview included measures of trauma history, lifetime and current PTSD, depression, anxiety, substance use, mental health treatment-seeking, coping strategies, and demographic factors (including race, age, income, educational attainment, and zip code). Among the eligible women who were reached, 96% completed interviews (n= 1,587) and of those, 1,581 interviews were available for analysis (six participants were found to be ineligible after chart abstraction). Participants were reimbursed $20 by mail. Recruitment logs were maintained of those eligible, not eligible, those interested, and those who declined. Analysis of missed opportunities for recruiting across clinic sites was conducted early in the recruitment period by comparing log sheets with the clinic appointment schedule. There were more missed opportunities in the sites where intake was distributed across the entire nursing staff as opposed to clinics with a single intake nurse. These missed opportunities were deemed random, attributable to the heavier work load of the nurses on tightly scheduled clinic days. However, due to the recruitment being conducted in multiple sites by nursing staff in busy clinics, there is no overall record of eligible women missed, nor were we able to compare those who declined the invitation or who were never reached with those who participated.
Analysis presented in this paper is cross-sectional, based on data from the diagnostic interview completed by 1,581 women prior to 28 weeks gestation, of whom four declined to answer racial identity items and were subsequently excluded (n=1,577). The self-identified racial/ethnic make-up of the sample includes 709 African American women (45.0%), 725 self-identified European American women (46.0%), 113 Asian women (7.2%), 67 Hispanic women (4.2%), 23 American Indian/Alaskan Native women (1.5%), seven Native Hawaiian/Pacific Islander women (0.4%), and 51 women identifying as other (3.2%). For data analysis purposes, we divided women into two groups. One group was comprised of women who self-identified as African American (AA, n=709). For the second group, we combined all ethnic groups who did not self-identify as African American and are referred to as non-African American throughout this paper (non-AA, n=868). The rationale for combining non-African American women is based on our primary aim, which is understanding PTSD risk, rates, and profiles among African American women.
Measures
The initial interview established baseline diagnostic status using several measures. Lifetime history of trauma exposure was ascertained using the Life Stressor Checklist (Wolfe and Kimerling 1997). This measure, designed for use with women, included 29 potentially traumatic events and ascertained age, impact at that time, and past-year impact of the woman's “worst” and “second worst” trauma exposures, using behaviorally specific terminology. Lifetime and current (past month) PTSD symptoms and diagnoses were assessed using the National Women's Study PTSD module (NWS-PTSD; Resnick et al. 1993). The NWS-PTSD module is the standardized telephone diagnostic interview that was used in the largest epidemiological study of U.S. women to date. It had a lifetime and current sensitivity of 0.99 and 0.96, respectively, and a specificity of 0.79 and 0.80, respectively, compared with the Structured Clinical Interview for DSM-IV during the PTSD field trial for the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) (Kilpatrick et al. 1994). The NWS measures all 17 symptoms across the re-experiencing, numbing and avoidance, and hyperarousal clusters. Past-year major depressive disorder (MDD) and generalized anxiety disorder (GAD) were assessed using the short form of the Composite International Diagnostic Interview (CIDI). The CIDI also was designed to be conducted by lay interviewers and has been rigorously tested by extensive field trial data indicating cross-national reliability and validity. The CIDI has excellent interrater reliability between lay and clinician interviewers with kappa of 0.97 for major depression and 0.96 for GAD (Wittchen 1994). Demographic and substance use data were gathered using the standardized items from the Center for Disease Control's Pregnancy Risk Assessment Monitoring System (PRAMS; Beck et al. 2002). Lifetime and pregnancy use of psychotherapy, psychiatric medication and coping were queried with items created specifically for the STACY study. Items queried pre-pregnancy use of therapy and psychiatric medications and their use during the current pregnancy. We also asked about engaged and disengaged forms of coping associated with PTSD such as prayer, talking to a friend, distraction with entertainment, sleep, alcohol, tobacco, or drug use.
Several variables were created for regression modeling. First, based on the resiliency literature indicating that cumulative risk is more robust than single risk factors in explaining adverse mental health outcomes (see Garmezy et al. 1984; Luthar et al. 2000; Rutter 1985), we created an index of cumulative sociodemographic factors associated with increased risk for PTSD: young age (<21 years), having an annual income of less than $15,000, having a high school education or less, and living in a postal code area with the FBI uniform crime rate higher than the US average. We defined “less sociodemographic risk” as having zero or one of these and “more sociodemographic risk” as having two or more of these risk factors. Second, to facilitate comparisons between types of exposures, we categorize the woman's self-described “worst” trauma exposure into descriptive categories: family context trauma, event trauma, prior reproductive loss that was traumatic, childhood emotional abuse or physical neglect, childhood sexual or physical abuse, and adult battering or sexual assault. We also considered prior mental health treatment as a likely marker of more severe, unremitting PTSD, and created a variable indicating pre-pregnancy use of either psychotherapy or psychiatric medication. This model is consistent with the model used to predict prenatal PTSD in the entire sample (Seng et al. 2009).
Statistical analyses
The first goal of this analysis was to provide extensive descriptive data, comparing African American to non-African American women. Bivariate tests for differences (chi squared and t test) are presented. Unadjusted odds ratios are presented when the chi squared is calculated in a 2×2 test. Some race-stratified bivariate analyses also were conducted to provide within-race risk data. In comparing the 29 trauma exposure types and 17 PTSD symptoms, we applied a Bonferroni correction for multiple tests.
The second goal was to consider patterns of risk across and within groups. We did two stepwise logistic regressions to model risk for lifetime PTSD. The first one was done on the entire sample, using race and the four-level cumulative index of sociodemographic risk factors associated with PTSD and trauma history variables. The second model of lifetime PTSD stratified the sample into African American and non-AA groups with the same sociodemographic and trauma variables. We then repeated these models to consider risks for still having a PTSD diagnosis in pregnancy. We added pre-pregnancy mental health treatment as a potential additional predictor of current PTSD. We used SPSS 16.0 (SPSS Inc., Chicago, IL, USA) for all analyses. The chi-squared tests comparing conditional risk across strata (Tables 3 and 4) were conducted using an online calculator (Graphpad software accessed 2009). Conditional risk is defined as the risk for PTSD given a history of trauma.
Table 3.
Psychiatric profile of African American and non-African American participants
| African American 45% (n=709) |
Non-African Americans 55% (n=868) |
Test statistic | p value | |
|---|---|---|---|---|
| Lifetime PTSD symptoms, mean (SD) | 5.0 (4.5) | 3.5 (4.0) | t=−7.2 | <0.001 |
| Lifetime PTSD diagnosis rate 20.2% (n=318) | 24.0 | 17.1 | Χ2= 11.6 | 0.001 |
| School impairment | 41.9% | 50.8% | Χ2=2.1 | 0.355 |
| Work impairment | 37.1% | 45.2% | Χ2=1.9 | 0.378 |
| Family role impairment | 77.4% | 65.3% | Χ2=4.4 | 0.035 |
| Very distressing | 49.2% | 61.3% | Χ2=5.6 | 0.135 |
| Current PTSD symptoms, mean (SD) | 3.3 (3.7) | 1.4 (2.3) | t=−12.3 | <0.001 |
| Current PTSD diagnosis rate 7.9% (n=125) | 13.4% | 3.5% | Χ2=52.9 | <0.001 |
| Depression rate 12.3% (n=194) | 15.1% | 10.0% | Χ2=9.3 | 0.002 |
| Conditional risk of depression comorbid with PTSD | 34.7% Χ2=67.1 OR=5.4 |
25.7% Χ2=48.5 OR=4.7 |
Χ2 for difference across strata in conditional risk is 2.632, p=0.105 |
|
| p<0.001 | p<0.001 | |||
| Anxiety rate 4.4% (n=69) | 3.7% | 5.0% | Χ2=1.5 | 0.214 |
| Conditional risk of anxiety comorbid with PTSD | 10.0% Χ2=25.4 OR=6.5 |
16.9% Χ2=54 OR=7.9 |
Χ2 for difference across strata in conditional risk is 2.705, p=0.100 |
|
| p<0.001 | p<0.001 | |||
| Substance use rate 25.9% (n=408) | 27.6% | 24.4% | Χ2=2.1 | 0.146 |
| Conditional risk of pregnancy substance use comorbid with PTSD | 42.9% Χ2=26.2 OR=2.5 |
29.7% Χ2=2.7 OR=1.4 |
Χ2 for difference across strata in conditional risk is 5.384, p=0.020 |
|
| p<0.001 | p=0.099 | |||
Table 4.
Comparison of rates of reporting current PTSD symptoms organized by DSM-IV symptom clusters (APA, 1994)
| African American 45% (n=709) |
Non-African Americans 55% (n=868) |
Bivariate odds ratio* |
|
|---|---|---|---|
| B cluster: intrusive re-experiencing | |||
| Unpleasant memories | 24.3 | 6.1 | 5.0 |
| Nightmares | 15.1 | 6.0 | 2.8 |
| Flashbacks | 9.9 | 3.0 | 3.5 |
| Intense distress at exposure to cues | 11.3 | 3.8 | 3.2 |
| Physiological reactivity | 18.3 | 7.8 | 2.6 |
| C cluster: avoidance and numbing | |||
| Avoiding thoughts/feelings | 26.8 | 7.7 | 4.4 |
| Avoiding places/activities | 9.4 | 2.8 | 3.7 |
| Could not remember aspects of trauma | 11.5 | 15.2 | 0.7 |
| Lost interest in activities | 22.3 | 6.1 | 4.4 |
| Detached feeling | 21.6 | 6.9 | 4.0 |
| Numb/less emotion | 14.1 | 2.8 | 5.8 |
| Foreshortened future | 14.4 | 7.3 | 2.1 |
| D cluster: arousal | |||
| Difficulty sleeping | 28.9 | 14.2 | 2.5 |
| Irritability/anger | 41.5 | 13.2 | 4.6 |
| Trouble concentrating | 18.9 | 8.3 | 2.6 |
| Hypervigilence | 16.2 | 3.7 | 5.1 |
| Exaggerated startle | 15.9 | 4.4 | 4.1 |
All p values<0.001 except for the amnesia symptom, which AA women reported less frequently, with p=0.030.
Results
Demographics
African Americans in this sample of pregnant women were an average of 7 years younger than non-AA women (22 versus 29 years). They also had many more sociodemographic risk factors, as only 6.8% had none of the four risk factors in the index (age<21 years, living on less than $15,000, having a high school education or less, and living in a higher than average crime rate neighborhood). Their mean number of these risk factors was 2.5 out of 4, versus a mean of 0.4 among non-AA women.
Trauma history
There is a disparity in the extent of trauma exposure across these groups (Table 1). We queried 29 potentially traumatic life events using the Life Stressor Checklist. After Bonferroni correction for 29 tests, African American women reported 16 exposures significantly more frequently (OR from 1.5 for sudden, unexpected death of a loved one, to 8.9 for family member jailed). There were 11 exposures reported at similar rates. Only two exposures were reported more frequently by non-AA women; death of a loved one (neither sudden nor unexpected) and personally being separated or divorced.
Table 1.
Comparison of trauma exposure disclosure rates in rank order by highest and lowest disparity in odds
| Type of potentially traumatic event | African American 45% (n=709) |
Non-African Americans 55% (n=868) |
OR* |
|---|---|---|---|
| Family member jailed | 57.5 | 13.2 | 8.9 |
| Serious money problems | 33.6 | 10.0 | 4.5 |
| Was fostered/adopted | 7.8 | 2.3 | 3.6 |
| Jailed (you) | 10.4 | 3.6 | 3.1 |
| Witnessed domestic violence | 47.7 | 23.0 | 3.0 |
| Physically abused as child | 6.1 | 2.5 | 2.5 |
| Saw robbery or attack | 22.1 | 11.4 | 2.2 |
| Saw accident | 37.5 | 22.7 | 2.0 |
| Child sexual abuse—penetration | 8.2 | 4.3 | 2.0 |
| Parents separated/divorced | 44.9 | 28.7 | 2.0 |
This table displays the 10 most disparately reported of all 29 trauma types
All p values≤0.001
As Table 2 shows, African American women had experienced more cumulative types of trauma exposure (5.7 versus 3.8 mean types of exposure). These were also more recent, with the “worst” trauma an average of 6.5 years (versus an average of 11.3 years) prior to the survey. This recentness, however, was more a function of the African American group's younger mean age than a function of difference in age at the time of the worst trauma exposure, as that difference is smaller (17.4 years for African American women and 18.9 years for non-AA women). Rates of childhood abuse trauma and worst trauma exposure occurring during childhood were slightly higher among African American women. However, the conditional risk of having PTSD in pregnancy given the risk factor of childhood abuse was 56.8% for AA women and 60.0% for non-AA women, a difference across strata that was not statistically significant (Χ2=0.009, p=0.926).
Table 2.
Trauma history profile of African American and non-African American participants
| African American 45% (n=709) |
Non-African Americans 55% (n=868) |
Test statistic |
p value | |
|---|---|---|---|---|
| Mean number reported exposures (SD) | 5.7 (3.7) | 3.8 (3.2) | t=−10.8 | <0.001 |
| Mean age at worst trauma exposurea(SD) | 17.4 (12.9) | 18.9 (11.6) | t=2.3 | 0.021 |
| Mean years elapsed since worst traumaa(SD) | 6.5 (5.9) | 11.3 (8.0) | t=13.0 | <0.001 |
| Past-year impact of worst traumaa | Χ2=40.2 | <0.001 | ||
| Not at all affected | 41.0% | 52.1% | ||
| Moderately affected | 42.3% | 40.9% | ||
| Extremely affected | 16.0% | 6.6% | ||
| Worst exposure in childhood (age<16 years) | 49.4% | 38.7% | Χ2=35.0 | <0.001 |
| Experienced child physical, sexual, emotional abuse, or physical neglect | 24.1% | 19.0% | Χ2=6.1 | 0.014 |
| Conditional risk of PTSD diagnosis in early pregnancy, given the trauma exposure of childhood abuse | 56.8% | 60.0% | OR=1.4 | |
| Χ2=64.2 OR=5.6 p<0.001 |
Χ2=33.9 OR=7.1 p<0.001 |
Χ2 for difference across strata in conditional risk is 0.009, p=0.926 |
||
7.8% of women (n=123) women did not report a trauma exposure so they are excluded from analyses related to “worst trauma”
PTSD prevalence and incidence
AA women reported an average of 1.5 more lifetime PTSD symptoms. They had a 50% increased odds of meeting lifetime PTSD diagnostic criteria (24.0% prevalence versus 17.1%, Χ2=11.6, p= 0.001; see Table 3). Distress and impairment related to lifetime PTSD did not differ between groups except that African American women reported family role impairment slightly more (77.4% versus 65.3%, Χ2=4.4, p=0.035). The disparity in meeting diagnostic criteria for current (chronic or recurrent PTSD, active in early pregnancy) was much larger. The incidence in pregnancy for African American women was 13.4% versus 3.5% among non-AA women (Χ2 =52.9, p<0.001). This conveys a threefold increased risk (OR=4.3, 95%, p<0.001) for current PTSD among AA expecting their first infant.
Comorbidity
The overall rate of past-year MDD diagnosis in this sample was 12.3%, with African American women having higher point prevalence (15.1% versus 10.0%, Χ2= 9.3, OR=1.6, p=0.002; Table 3). Although the prevalence of comorbid MDD diagnosis was higher for African American women (34.7% versus 25.7% among non-AA women), the conditional risk for MDD given a lifetime history of PTSD was similar (Χ2=2.632, ORs=5.4 and 4.7, respectively, p=0.105). Conditional risk for generalized anxiety disorder diagnosis, given lifetime PTSD also was similar across race strata. Conditional risk for use of any substances in pregnancy was higher in the African American group, primarily due to more use of marijuana.
Effect of cumulative sociodemographic risk factors for PTSD
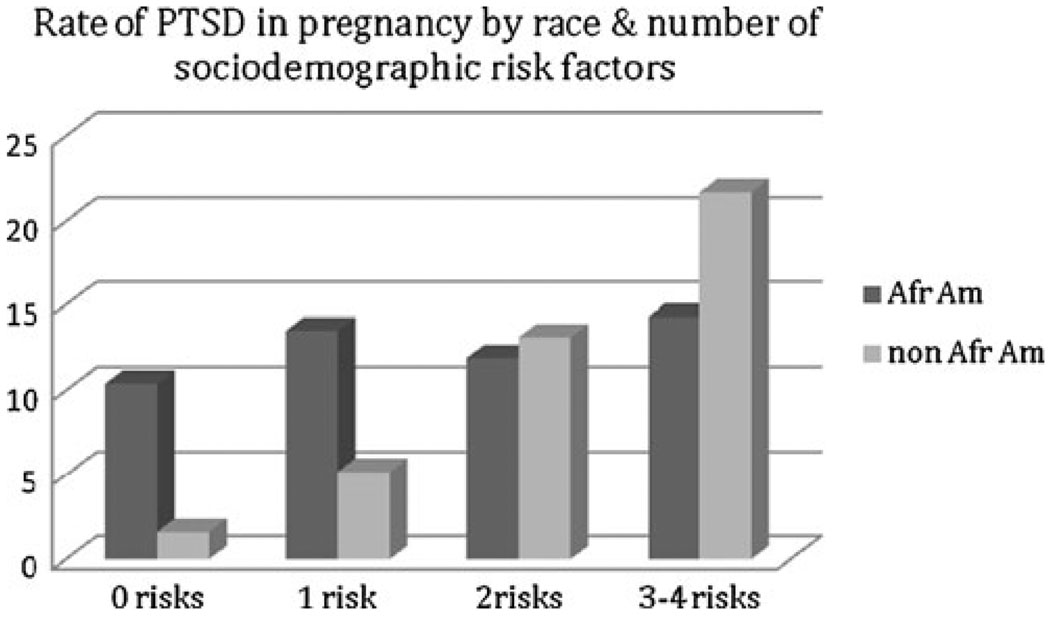
Sociodemographic risk factors associated with PTSD in the literature (young age, poverty, low education, residing in a high crime area) were not associated with PTSD rates for African American women in this sample (see Fig. 1). We assessed this relationship within race groups two ways. Using the cumulative sociodemographic risk variable in its ordinal form (zero, one, two, three to four risks), the association with PTSD in pregnancy for non-AA women was strong (Χ2=47.7, p<0.001), but was weak for African American women (Χ2=1.0, p=0.802; see bar graph). When dividing the two race strata by relative level of sociodemographic risk factors, defined as lower number of risks (zero or one) versus higher number of risks (two, three, or four), again distinctly different patterns were evident. For non-AA women, more risk factors were associated with higher rates of both lifetime (32.1% versus 15.4%, Χ2=15.0, OR=2.6, p<0.001) and current PTSD diagnoses (15.5% versus 2.2%, Χ2=40.3, OR=8.3, p< 0.001). For AA women, however, more risk factors were not associated with higher rates of either lifetime (22.8% versus 29.5%, Χ2=2.5, OR=2.6, p=0.116) or current PTSD (13.6% versus 12.3%, Χ2=0.2, OR=1.1, p=0.694).
Fig. 1.
Rate of PTSD in pregnancy by race and number of sociodemographic risk factors
Symptom profile
In terms of lifetime PTSD symptom profiles (data not shown), after Bonferroni correction for 17 tests, African American women reported symptoms at greater rates for 11 of 17 symptoms across all three PTSD symptom clusters. The significant odds ratios ranged from a low of 1.5 (i.e., psychological distress at reminders of the trauma, detachment) to 3.0 (i.e., anger and irritability). In relation to current PTSD symptoms, except for amnesia, the African American women reported more symptoms across the board, ranging from a significant odds ratio of 2.1 (i.e., foreshortened sense of future) to 5.8 (i.e., emotional numbing). The most common symptoms for African American women were irritability/anger (41.5%), difficulty sleeping (28.9%), avoiding thoughts/feelings (26.8%), and having unpleasant memories (24.3%; Table 4).
Mental health treatment seeking and coping strategies
Reported mental health service use for their lifetime prior to pregnancy and in pregnancy indicated that despite greater burden of PTSD and comorbidity, African American women sought or received less treatment (Table 5). Coping strategies also differed by race, with AA women using prayer more and alcohol less “to cope with emotions or problems,” similar rates of using tobacco, illicit drugs, or sleep to cope, and lower rates of other engaged (e.g., talking to a friend) and disengaged (e.g., distraction with entertainment) strategies than non-AA women.
Table 5.
Use of mental health services, self-help strategies, and coping
| African American 45% (n=709) % |
Non-African Americans 55% (n=868) % |
p value | OR | |
|---|---|---|---|---|
| Mental health services used | ||||
| Individual psychotherapy | 17.5 | 39.7 | <0.001 | 0.3 |
| Group therapy | 7.9 | 8.4 | 0.712 | 0.9 |
| Marital/family therapy | 9.0 | 19.2 | <0.001 | 0.4 |
| Support group | 3.9 | 7.7 | 0.002 | 0.5 |
| Medication | 4.4 | 21.3 | <0.001 | 0.2 |
| Mental health services used in pregnancy | ||||
| Pregnancy psychotherapy | 1.7 | 6.3 | <0.001 | 0.3 |
| Pregnancy medication | 0.1 | 4.4 | <0.001 | 0.0 |
| Self-help strategies | ||||
| Herbals | 1.6 | 8.2 | <0.001 | 0.2 |
| Self-help books or materials | 9.2 | 24.9 | <0.001 | 0.3 |
| Coping strategies useda | ||||
| Alcohol | 8.9 | 21.5 | <0.001 | 0.4 |
| Tobacco | 15.9 | 17.4 | 0.440 | 0.9 |
| Drugs | 11.8 | 9.4 | 0.122 | 1.3 |
| Sleep | 65.6 | 63.7 | 0.439 | 1.1 |
| Distracting with entertainment | 60.2 | 79.1 | <0.001 | 0.4 |
| Distracting with work | 40.1 | 54.0 | <0.001 | 0.6 |
| Light exercise | 61.6 | 79.6 | <0.001 | 0.4 |
| Strenuous exercise | 7.6 | 28.0 | <0.001 | 0.2 |
| Talking with friend | 84.5 | 97.2 | <0.001 | 0.2 |
| Crying | 76.6 | 86.9 | <0.001 | 0.5 |
| Praying | 88.6 | 65.7 | <0.001 | 4.1 |
“Which, if any, of these ways have you EVER used to cope with emotions or problems?”
Lifetime PTSD risk
When lifetime PTSD diagnosis was modeled with all participants together in a first step that included only race, African American race was a significant independent predictor (OR=1.534, p=0.001), but when the categorical cumulative sociodemographic risk factor was added, neither race nor sociodemographic risk were significant predictors (Table 6). All of the six trauma exposure types (i.e., family context, events, prior reproductive loss, childhood emotional abuse or neglect, childhood sexual or physical abuse, adult sexual or physical abuse) were independently predictive, each with odds ratios of 2.1 to 3.0. In the parallel model, stratified by race, sociodemographic risk is not significantly associated with lifetime PTSD among the African American women. However, sociodemographic risk is predictive of lifetime PTSD among non-AA women, in a dose–response pattern.
Table 6.
Stepwise logistic regression of predictors of lifetime PTSD diagnosis (n=1,577)
| Model steps and variable names | Combined analysis |
Race-stratified analyses |
||||
|---|---|---|---|---|---|---|
| All participants n=1, 577 |
African Americans n=709a |
Non-African Americans n=868b |
||||
| OR | p value | OR | p value | OR | p value | |
| Step 1 | ||||||
| African American | 0.001 | 1.534 | – | – | – | – |
| Step 2 | ||||||
| African American | 0.430 | 1.167 | – | – | – | – |
| Cumulative sociodemographic risk factorsc | 0.159 | – | 0.378 | – | 0.001 | – |
| 1 risk factor, n=190 | 0.044 | 1.528 | 0.734 | 0.872 | 0.158 | 1.438 |
| 2 risk factors, n=229 | 0.106 | 1.448 | 0.134 | 0.579 | 0.003 | 2.435 |
| 3–4 risk factors, n=442 | 0.074 | 1.506 | 0.246 | 0.681 | 0.003 | 3.739 |
| Step 3d | ||||||
| African American | 0.825 | 0.953 | – | – | – | – |
| Cumulative sociodemographic risk factorsa | 0.706 | – | 0.422 | – | 0.045 | – |
| 1 risk factor, n=190 | 0.344 | 1.253 | 0.683 | 0.827 | 0.574 | 1.178 |
| 2 risk factors, n=229 | 0.543 | 1.168 | 0.137 | 0.534 | 0.076 | 1.847 |
| 3–4 risk factors, n=442 | 0.298 | 1.297 | 0.281 | 0.661 | 0.019 | 3.096 |
| Any family context trauma | 0.037 | 2.139 | 0.443 | 1.789 | 0.055 | 2.223 |
| Any event trauma | <0.001 | 2.477 | <0.001 | 2.776 | <0.001 | 2.238 |
| Any reproductive trauma | <0.001 | 2.915 | <0.001 | 2.988 | <0.001 | 2.735 |
| Child emotional abuse or physical neglect | 0.001 | 2.733 | 0.085 | 2.071 | 0.002 | 3.488 |
| Childhood sexual or physical abuse | <0.001 | 2.989 | <0.001 | 3.402 | <0.001 | 2.702 |
| Adult sexual or physical abuse | <0.001 | 2.613 | <0.001 | 2.672 | <0.001 | 2.502 |
AA model evaluation: model chi-squared, p<0.001, Nagelkerke R2 =0.290, predicted correctly, 79.7%
Non-AA model evaluation: model chi squared, p<0.001, Nagelkerke R2 =0.238, predicted correctly, 84.2%
Reference group for categorical sociodemographic variable=0 risk factors, n=716.
Combined model evaluation: model chi-squared, p<0.001, Nagelkerke R2 =0.263, predicted correctly, 82.2%
Current PTSD risk
When current PTSD diagnosis was modeled with all participants, race was a significant predictor (OR=4.322, p=<.001), but sociodemographic risk factors mediated the association of between race and current PTSD when all women are considered together (OR=1.619, p= 0.111; Table 7). In the third step of the model, we added the six types of trauma exposure and a variable indicating whether the woman had used mental health treatment (psychotherapy or medication) prior to pregnancy. African American race approached significance (OR=1.737, p= 0.084), and each additional sociodemographic risk increased odds (from 2.7 to 4.8).
Table 7.
Stepwise logistic regression of predictors of current PTSD diagnosis (n=1,577)
| Model steps and variable names | Combined analysis |
Race-stratified analyses |
||||
|---|---|---|---|---|---|---|
| All participants n=1, 577 |
African Americans n=709a |
Non-African Americans n=868b |
||||
| OR | p value | OR | p value | OR | p value | |
| Step 1 | ||||||
| African American | <0.001 | 4.322 | – | – | – | – |
| Step 2 | ||||||
| African American | 0.111 | 1.619 | – | – | – | – |
| Cumulative sociodemographic risk factorsc | <0.001 | – | 0.803 | – | <0.001 | – |
| 1 risk factor, n=190 | 0.001 | 3.390 | 0.612 | 1.344 | 0.023 | 3.258 |
| 2 risk factors, n=229 | <0.001 | 4.382 | 0.776 | 1.162 | <0.001 | 9.015 |
| 3–4 risk factors, n=442 | <0.001 | 4.953 | 0.461 | 1.437 | <0.001 | 16.591 |
| Step 3d | ||||||
| African American | 0.084 | 1.737 | – | – | – | – |
| Cumulative sociodemographic risk factorsc | 0.001 | – | 0.654 | – | <0.001 | – |
| 1 risk factor, n=190 | 0.017 | 2.662 | 0.616 | 1.383 | 0.082 | 2.638 |
| 2 risk factors, n=229 | 0.001 | 3.981 | 0.607 | 1.354 | <0.001 | 8.781 |
| 3–4 risk factors, n=442 | <0.001 | 4.782 | 0.309 | 1.746 | <0.001 | 16.100 |
| Any family context trauma | 0.932 | 0.955 | 0.524 | 1.941 | 0.298 | 0.492 |
| Any event trauma | 0.085 | 1.577 | 0.218 | 1.471 | 0.290 | 1.700 |
| Any reproductive trauma | 0.001 | 2.199 | <0.001 | 2.600 | 0.834 | 1.118 |
| Child emotional abuse or physical neglect | 0.035 | 2.132 | 0.075 | 2.153 | 0.219 | 2.256 |
| Childhood sexual or physical abuse | <0.001 | 3.498 | <0.001 | 3.727 | 0.007 | 3.353 |
| Adult sexual or physical abuse | <0.001 | 2.475 | 0.001 | 2.340 | 0.021 | 2.828 |
| Pre-pregnancy mental health treatment | 0.049 | 1.599 | 0.384 | 1.286 | 0.047 | 2.525 |
AA final model evaluation: model chi-squared, p<0.001, Nagelkerke R2 =0.231, predicted correctly, 86.9%
Non-AA final model evaluation: model chi-squared, p<0.001, Nagelkerke R2 =0.276, predicted correctly, 96.3%
Reference group for categorical sociodemographic variable=0 risk factors, n=716.
Combined final model evaluation: model chi-squared, p<0.001, Nagelkerke R2 =0.282, predicted correctly, 92.0%
Reproductive loss, both childhood trauma variables, and adult abuse each increased risk. Previous mental health treatment also was a predictor of having a PTSD diagnosis in pregnancy. In the stratified analyses, the patterns differed by race. The strongest predictor of current PTSD was among non-AA women in the final adjusted model with accumulated sociodemographic risk factors, where the odds ratios were 8.8 with two risk factors and 16.1 with three risk factors (p<0.001 in both instances). Child and adult abuse and prior treatment were also predictive for non-AA women. Pre-pregnancy mental health treatment was significantly associated with risk for current PTSD among non-AA women, but not among African American women.
Discussion and conclusion
In conclusion, in this study of pregnant women, African American gravidas had slightly higher rates of lifetime PTSD (24%) and fourfold higher rates of current PTSD (13.4%) compared with non-African Americans (17.1% lifetime, 3.5% current). Race alone was not a significant risk factor after trauma history was taken into account. Sociodemographic risk was not predictive for African Americans, but was highly predictive for non-AA women. History of childhood sexual or physical abuse was a major risk factor for both groups. Conditional risk for PTSD given a childhood abuse history did not differ by race. However the overall burden of trauma for African Americans was greater. Mean number of trauma exposures, rating of strong past-year impact of the index trauma, likelihood the index trauma occurred in childhood, and likelihood of having experienced childhood abuse trauma in particular all were higher among African Americans. The rate of pre-pregnancy use of mental health treatment among African American women was lower. In stratified models, African American women's higher rates of lifetime PTSD were accounted for by greater trauma exposure generally. Their higher rates of current PTSD were accounted for by child and adult abuse trauma in particular. Risk within the African American group did not differ by sociodemographic status. Among non-AA women, sociodemographic status was associated with lifetime PTSD risk and very strongly predictive of current PTSD diagnosis, over and above the risk conveyed by trauma exposures. For non-AA women, accessing treatment prior to pregnancy was associated with unremitted (i.e., more severe, chronic, or recent PTSD). For African American women, however, having accessed previous treatment was not predictive of current PTSD status.
Interestingly, group differences in self-reported coping strategies were found to be both similar and dissimilar with that in previous literature. African American women's greater reliance on prayer is reflective of robust findings of race differences in the use of religious resources (Taylor et al. 2004). African American women's decreased reliance on alcohol mirrors the decreased risk among African Americans in national prevalence rates for alcohol abuse and dependence in comparison to non-African Americans (see Breslau et al. 2005). While not entirely consistent with previous studies comparing the use of tobacco, illicit drugs and sleep, the racially similar rates found here may be due to the shared pregnant status of the sample. African American women's lower rates of both engaged and disengaged coping strategies implies that increasing the use of these strategies may be fruitful areas for intervention.
This finding of greater risk for PTSD among African American women compared to other women, regardless of sociodemographic risk, parallels the consistent finding in the public health and obstetric literature that African American women are at risk for the worst perinatal outcomes, also regardless of sociodemographic status (Green et al. 2005; Paul et al. 2008). The threefold disparity by race in risk for PTSD diagnosis during pregnancy in this sociodemographically diverse sample appears due to differential exposure to trauma and possibly also to differential use of or access to treatment prior to pregnancy. This increased risk raises the question of whether PTSD might be an addressable contributory factor in racial disparities in birth outcomes, above and beyond the explanatory factor of greater trauma exposure.
There are limitations to bear in mind. Findings from this study may not generalize to non-pregnant women, multi-gravid women, or males. Also, the focus on African American women in this study precluded analysis of other minority groups; this is an area for future research. We do not know how recent trauma exposures were, so we do not know if it is cumulative load of exposure, recency, or both that contribute to the higher risk of PTSD for African Americans. Despite the use of telephone surveys to avoid potential biases in clinical judgments and hesitancy to discuss sensitive information, we acknowledge that the trauma assessments may underestimate the rates of interpersonal trauma experienced by participants due to disclosure concerns. We did not conduct in-depth inquiry on treatment seeking and therefore do not know what accounts for the lower rates of treatment among African Americans in this sample. Limitations of the recruitment process preclude comparing participants with those who declined to participate, so this should be viewed as a convenience sample. Finally, although women were recruited from diverse contexts (university town and large urban center) this analysis only considered effect of local crime rate, not effect of minority versus majority status; findings might differ in more integrated contexts.
Despite limitations, the strengths of this study are considerable. This is the first large study of PTSD in pregnant women that includes sufficient sociodemographic diversity in the sample, including approximately half privately and half publicly insured women, such that race and socioeconomic status are not entirely confounded. The use of the standardized National Women's Study PTSD module for diagnosis provided comparable, valid, and well-characterized data on PTSD. The trauma assessment tool we used is considered to be highly sensitive to trauma exposure experienced by women (Cusak et al. 2002). It also was conducted in standardized form by telephone and included behavior-specific definitions; these strategies are known to reduce rater bias and disclosure concerns. The sample size was large enough to permit stringent correction for multiple tests in the bivariate analyses of the 29 trauma exposures and 17 PTSD symptoms. The findings from this study are of significant importance given the relevant potential for early detection procedures through the assessment of trauma, PTSD, and risk factors that disproportionately and negatively affect childbirth among African Americans.
There are clinical implications from this analysis. First, screening for PTSD should be added to screening for past and current abuse in perinatal settings, especially those serving African Americans and poor women. For African American women especially past and current abuse may be only one or two among an average of six types of trauma exposure, and not necessarily the worst they experienced. More expansive trauma history checklists may be warranted in high-risk settings. Screening for both PTSD and depression is warranted. In this study, 50% of cases of pregnancy depression were comorbid with PTSD. When comorbid with PTSD, depression is usually the secondary disorder (Breslau 2001), therefore depression screening alone may miss cases of PTSD by finding only the secondary disorder. Screening for both depression and PTSD would likely make the underlying traumatic stress etiology evident when it exists, and would permit tailoring of treatment and stress-reduction strategies. Evidence-based treatments for PTSD exist, but research to verify their efficacy and safety in pregnancy are needed. Qualitative research done with women whose childbearing experience was affected by PTSD suggested that trauma-informed education and support services were desired, including anticipatory guidance about parenting (Seng et al. 2002; Sperlich and Seng 2008).
Our finding of greater risk for PTSD is somewhat at odds with the literature on race and PTSD prevalence. Epidemiological, clinical, and service use studies all have generally found lower rates of PTSD among African Americans (Breslau et al. 2006; Seng et al. 2005). When a finding of higher prevalence among African Americans was subjected to multivariate analysis, poverty and urban residence accounted for their greater risk (Breslau et al. 1998). However, studies that have analyzed risk by race for both lifetime and current PTSD have come to the similar conclusion that, while risk for lifetime PTSD may not differ, odds of recovery are lower for African Americans, as evidenced by greater risk for meeting current diagnostic criteria (Breslau et al. 2006). It is not yet known whether risk for current PTSD among African American women is more attributable to lack of treatment or to more recent and greater cumulative number of trauma exposures. Age may be an additional important factor. We assessed the effect of time elapsed since the worst trauma as a risk factor and found it not to be a significant predictor of current PTSD. However, we do not have data regarding the time elapsed since the most recent traumatic event. Trauma exposure peaks in the 16–20 year age range for women, so the younger mean age of the African American group (22 years versus 29 years for the non-AA group) suggests that recency may be an additional important predictor (Breslau 2001). In our own previous study of Medicaid claims data, rates of PTSD diagnosis in African American adult women were lower than in African American adolescent girls (Seng et al. 2005) a finding which would support this conjecture and suggests that careful analysis across age cohorts is warranted in future studies.
Our findings also are at odds with two other U.S. studies of PTSD incidence in pregnancy where African American participants were included. Cook et al. (2004) reported a current PTSD rate of 7.7% among low-income women that did not differ by race. Smith et al. (2006) reported a rate of 3.5% across a racially diverse sample which mirrors the current PTSD prevalence rate for non-African American women in our study. The inconsistency may be due to the low-income and Medicaid clinic settings used in those studies. In our economically diverse sample, which includes privately and publicly insured women from urban and non-urban settings, sociodemographic risk factors were most predictive for non-African American women. In fact, the very highest risk for PTSD in our study was among the 84 non-AA women who were the most disadvantaged. Thus, if samples include only poor women in urban settings, the risk of PTSD may be equally high for all. But a disparity in rates by race may become evident if the reference group in the risk models are affluent, non-AA pregnant women, as is the case in our sample.
More research is needed among African American women to know the mechanism underlying higher risk for meeting diagnostic criteria during pregnancy regardless of sociodemographic risk. Future research should use ecological and multi-level methods to model neighborhood and social network factors to better understand risk for PTSD by race and socioeconomic status and to inform planning for effective social service supports and interventions. It is important to learn whether triggers for PTSD re-experiencing symptoms that are inherent in pregnancy and maternity care differ in quantity or quality by race, increasing symptomatology among African American women. It also is critical to learn what is differentially preventing PTSD recovery for African American young women prior to pregnancy. If PTSD turns out to be associated with preterm birth via psychosocial and biological pathways, we will have a new avenue for primary, secondary, and tertiary prevention of obstetric outcome disparities—over and above the risk conveyed by disparities in trauma exposure.
Acknowledgment
The project described was supported by Grant Number R01NR008767 from the National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Footnotes
The authors declare that they have no conflict of interest.
Contributor Information
Julia S. Seng, Email: jseng@umich.edu, Institute for Research on Women and Gender, University of Michigan, G120 Lane Hall, 204 S. State St, Ann Arbor, MI 48109, USA; School of Nursing, University of Michigan, G120 Lane Hall, 204 S. State St, Ann Arbor, MI 48109, USA; Department of Obstetrics and Gynecology, University of Michigan, G120 Lane Hall, 204 S. State St, Ann Arbor, MI 48109, USA; Department of Women’s Studies, University of Michigan, G120 Lane Hall, 204 S. State St, Ann Arbor, MI 48109, USA.
Laura P. Kohn-Wood, University of Miami Department of Educational and Psychological Studies, 5202 University Drive, Coral Gables, FL 33124, USA
Melnee D. McPherson, University of Michigan School of Social Work, 1080 S. University Dr, Ann Arbor, MI 48109, USA
Mickey Sperlich, University of Michigan Institute for Research on Women and Gender, G120 Lane Hall, 204 S. State St, Ann Arbor, MI 48109, USA.
References
- Beck LF, Morrow B, Lipscomb LD, Johnson CH, Gaffield ME, Rogers M, Gilvert BC. Prevalence of selected maternal behaviors and experiences, Pregnancy Risk Assessment Monitoring System (PRAMS), 1999. Morbidity & Mortality Weekly Reports. 2002;51(SS02):1–26. [PubMed] [Google Scholar]
- Breslau N. Outcomes of posttraumatic stress disorder. J Clin Psychiatry. 2001;62 suppl 17:55–59. [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 detroit area survey of trauma. Arch Gen Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Breslau J, Kendler KS, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med. 2005;35:317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Aguilar-Gaxiola S, Kendler KS, Su M, Williams D, Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med. 2006;36(1):57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook CAL, Flick LH, Homan SM, Campbell C, McSweeney M, Gallagher ME. Posttraumatic stress disorder in pregnancy: prevalence, risk factors, and treatment. Obstet Gynecol. 2004;103:710–717. doi: 10.1097/01.AOG.0000119222.40241.fb. [DOI] [PubMed] [Google Scholar]
- Cusak K, Falsetti S, de Arellano M. Gender considerations in the psychometric assessment of PTSD. In: Kimerling R, Ouimette P, Wolfe J, editors. Gender and PTSD. New York: Guilford Press; 2002. pp. 15–176. [Google Scholar]
- Engel SM, Berkowitz GS, Wolff MS, Yehuda R. Psychological trauma associated with the World Trade Center attacks and its effect on pregnancy outcome. Paediatr Perinat Epidemiol. 2005;19(5):334–341. doi: 10.1111/j.1365-3016.2005.00676.x. [DOI] [PubMed] [Google Scholar]
- Garmezy N, Masten AS, Tellegen A. The study of stress and competence in children: a building block for developmental psychology. Child Dev. 1984;55:97–111. [PubMed] [Google Scholar]
- Graphpad software. [Accessed 5 Jan 2009];QuickCalcs: Online calculators for scientists. www.graphpad.com/quickcalc/Contingency1.cfm.
- Green NS, Damus K, Simpson JL, et al. Research agenda for preterm birth: recommendations from the March of Dimes. Am J Obstet Gynecol. 2005;193:626–635. doi: 10.1016/j.ajog.2005.02.106. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Heghes M, Nelson C. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Freedy JR, Pelcovitz D, Resick P, Roth S, van der Kolk B. DSM-IV Sourcebook. Washington, DC: American Psychiatric Press; 1994. The posttraumatic stress disorder field trial: emphasis on criterion a and overall PTSD diagnosis. [Google Scholar]
- Kilpatrick DG, Ruggerio KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the national survey of adolescents. J Cons Clin Psych. 2003;71(4):692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- King S, Walker CD, Brunet A, Meaney MJ, Laplante DP. Project Ice Storm: Effect of prenatal cortisol levels on obstetric complications; International Society for Psychoneuroendocrinology Annual Meeting; Montreal, Quebec, Canada. 2005. Nov, [Google Scholar]
- King AP, Leichtman JN, Abelson JL, Liberzon I, Seng JS. Ecological salivary cortisol analysis—Part 2: relative impact of trauma history, posttraumatic stress, comorbidity, chronic stress, and known confounds on hormone levels. J Am Psychiatr Nurses Assoc. 2008;14:285–296. doi: 10.1177/1078390308321939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 2000;71:543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews TJ, Hamilton BE. Mean age of mother, 1970–2000. CDC Natl Vital Stat Rep. 2002;51:1–14. [PubMed] [Google Scholar]
- Paul K, Boutain D, Agnew K, Thomas J, Hitti J. The relationship between racial identity, income, stress, and c-reactive protein among parous women: implications for preterm birth disparity research. J Nat Med Assoc. 2008;100:540–546. doi: 10.1016/s0027-9684(15)31300-6. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Rogal SS, Poschman K, Belanger K, Howell HB, Smith MV, Medina J, Yonkers KA. Effects of posttraumatic stress disorder on pregnancy outcomes. J Affect Disord. 2007;102:137–143. doi: 10.1016/j.jad.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen D, Seng JS, Tolman RM, Mallinger G. Intimate partner violence, depression, and posttraumatic stress disorder as additional predictors of low birth weight infants among low-income mothers. J Interpers Violence. 2007;22:1305–1314. doi: 10.1177/0886260507304551. [DOI] [PubMed] [Google Scholar]
- Rutter M. Resilience in the face of adversity. Protective factors and resistance to psychiatric disorder. Br J Psychiatry. 1985;147:598–611. doi: 10.1192/bjp.147.6.598. [DOI] [PubMed] [Google Scholar]
- Seng JS, Oakley DJ, Sampselle CM, Killion C, Graham-Bermann S, Liberzon I. Association of posttraumatic stress disorder with pregnancy complications. Obstet Gynecol. 2001;97:17–22. doi: 10.1016/s0029-7844(00)01097-8. [DOI] [PubMed] [Google Scholar]
- Seng JS, Sparbel KJH, Kane Low LM, Killion C. Abuse-related posttraumatic stress and desired maternity care practices: women's perspectives. J Midwifery Womens Health. 2002;47:360–370. doi: 10.1016/s1526-9523(02)00284-2. [DOI] [PubMed] [Google Scholar]
- Seng JS, Kohn-Wood LP, Odera L. Exploring racial disparity in posttraumatic stress disorder diagnosis: implications for care of African American women. J Obstet Gynecol Neonatal Nurs. 2005;34:521–530. doi: 10.1177/0884217505278296. [DOI] [PubMed] [Google Scholar]
- Seng JS, Clark MK, McCarthy AM, Ronis DL. PTSD and physical co-morbidity among women: results from service use data. J Trauma Stress. 2006;19:45–56. doi: 10.1002/jts.20097. [DOI] [PubMed] [Google Scholar]
- Seng JS, King AP, Gabriel C, Reed CD, Sperlich M, Dunbar S, Fraker E, Ronis DL. Ecological salivary cortisol specimen collection—Part 1: methodological consideration of yield, error, and effects of sampling decisions in a perinatal mental health study. J Am Psychiatr Nurses Assoc. 2008;14:273–284. doi: 10.1177/1078390308322944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Kane Low LM, Sperlich MI, Ronis DL, Liberzon I. Trauma history and risk for PTSD among nulliparous women in maternity care. Obstet Gynecol. 2009;114(4):839–847. doi: 10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shalev AY, Videlock EJ, Peleg T, Segman R, Pitman RK, Yehuda R. Stress hormones and post-traumatic stress disorder in civilian trauma victims: a longitudinal study. Part I: HPA axis responses. Int J Neuropsychopharmacol. 2008;11(3):365–372. doi: 10.1017/S1461145707008127. [DOI] [PubMed] [Google Scholar]
- Smith MV, Poschman K, Cavaleri MA, Howell HB, Yonkers KA. Symptoms of posttraumatic stress disorder in a community sample of low-income pregnant women. Am J Psychiatry. 2006;163:881–884. doi: 10.1176/ajp.2006.163.5.881. [DOI] [PubMed] [Google Scholar]
- Sperlich M, Seng JS. Survivor moms: women's stories of birthing, mothering, and healing after sexual abuse. Eugene: Motherbaby Press; 2008. [Google Scholar]
- Taylor RJ, Chatters LM, Levin JS. Religion in the lives of African Americans: social, psychological, and health perspectives. Thousand Oaks: Sage Publications; 2004. [Google Scholar]
- Vogel LCM, Marshall LL. PTSD symptoms and partner abuse: low income women at risk. J Trauma Stress. 2001;14(3):569–584. doi: 10.1023/A:1011116824613. [DOI] [PubMed] [Google Scholar]
- Wittchen HU. Reliability and validity of the WHO-composite international diagnostic interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Wolfe J, Kimerling R. Gender issues in the assessment of posttraumatic stress disorder. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford Press; 1997. pp. 192–238. [Google Scholar]