Answer to the rhythm puzzle
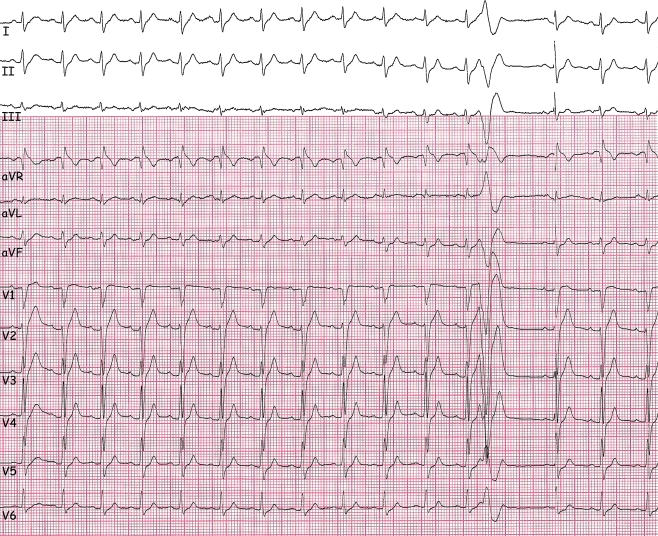
The ECG shows a regular sinus tachycardia at 105 beats/min with an undetermined axis, normal conduction and repolarisation intervals, and normal R-wave progression in the precordial leads (Fig. 1). The notch in the rising portion of the S-wave and the subsequent subtle ST-segment elevation in lead V1 may be noted. The fundamental feature is a very short-coupled (coupling interval: 270 ms) ventricular premature beat (VPB) with a left bundle branch block (LBBB) morphology and superior axis, most probably arising from the right ventricular apex or lower free wall.
Fig. 1.
Twelve-lead electrocardiogram upon presentation (25 mm/s, 10 mm/mV)
The most important question in this young male was his family history. This revealed that multiple family members had suffered from a premature sudden cardiac death; a nephew died suddenly at the age of 26 years and an uncle died suddenly at the age of 48 years.
Our differential diagnosis included arrhythmogenic right ventricular dysplasia/cardiomyopathy, Brugada syndrome and (familial) idiopathic ventricular fibrillation. Other causes of ventricular arrhythmias, such as other cardiomyopathies or primary arrhythmia syndromes, idiopathic ventricular tachycardia, myocardial ischaemia, and myocarditis could not be excluded, but the (family) history or ECG made these last-mentioned causes less likely. The patient was admitted because of the near-syncope and the short-coupled VPB in addition to the malignant family history. Shortly after admission the patient developed non-sustained and sustained episodes of a fast polymorphic ventricular tachycardia and ventricular fibrillation, all initiated by the same very short-coupled VPB with an LBBB morphology and a superior axis (Fig. 2), requiring electrical cardioversion.
Fig. 2.
Twelve-lead electrocardiogram during admission (25 mm/s, 10 mm/mV)
It appeared that this patient carried a haplotype including the DPP6 gene causing familial idiopathic ventricular fibrillation, and he was treated with an ICD. This haplotype is associated with a very high incidence of premature sudden death, up to 50% of its carriers experience ventricular fibrillation or sudden death before 60 years of age [1, 2]. There are no gross structural abnormalities in these patients but very short coupled VPB from the right ventricular lower free wall or apex which start polymorphic ventricular tachycardia or ventricular fibrillation are noted in all DPP6 haplotype carriers with documented arrhythmias. Importantly, most of the family members originate from a defined area in the Netherlands, between Woerden and the Lek. In the sentinel contribution of Haissaguerre et al. on the ablation options for ventricular fibrillation, this type of VPB was identified in 25% of his patients [3]. The exact pathophysiological basis underlying these ventricular arrhythmias is currently being investigated.
Contributor Information
C. van der Werf, Phone: +31-20567731, FAX: +31-206962609, Email: c.vanderwerf@amc.uva.nl
P. G. Postema, Phone: +31-20567731, FAX: +31-206962609
References
- 1.Alders M, Koopmann TT, Christiaans I, et al. Haplotype-sharing analysis implicates chromosome 7q36 harboring DPP6 in familial idiopathic ventricular fibrillation. Am J Hum Genet. 2009;84:468–76. doi: 10.1016/j.ajhg.2009.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Postema PG, Christiaans I, Hofman N, et al. Founder mutations in the Netherlands. Familial idiopathic ventricular fibrillation and DPP6. Neth Heart J. 2011;19:290–96. [DOI] [PMC free article] [PubMed]
- 3.Haïssaguerre M, Shoda M, Jaïs P, et al. Mapping and ablation of idiopathic ventricular fibrillation. Circulation. 2002;106:962–7. doi: 10.1161/01.CIR.0000027564.55739.B1. [DOI] [PubMed] [Google Scholar]