Abstract
Ghee and honey has been advocated and used as dressing for infected wounds by Sushruta (600BC) and since 1991 in four Mumbai Hospitals. The gratifying results observed with the dressing have prompted this study which aims to establish its efficacy in five recalcitrant subset of chronic infected wounds over a three year period 2006–2009. A standardized ghee and honey dressing was used to treat: a) Eight cases of fungating malignant lesions. b) Thirteen chronic venous ulcers. c) Twenty nine diabetic foot ulcers. d) Eleven of infected ventral hernia mesh hernioplasty. e) Eleven patient with post-cesarean wound dehiscence. The dressing markedly reduced the foul odour and discharge, significantly improving the quality of life in malignant lesions. The results were equivocal in cases of venous ulcers. The results were uniformly good in the last three groups. In view of our results, as also result of innumerable Randomized Control Trials (RCTs) reported on honey dressing for infected wounds, there is substantial evidence that ghee and honey dressing has at least comparable results to other modes of treatment. The easy availability and low cost of this treatment makes it significant in developing countries. Further trials seem warranted.
Keywords: Sushruta, Ghee and honey dressing, Infected wounds, Developing countries
Introduction
The author was introduced to and convinced of the value of ghee and honey dressing for chronic infected wounds during a visit to Nairobi in September 1991 by Dr. Gadvi, an Indian surgeon and Sanskrit scholar working in a remote part of Kenya [1]. Ghee, clarified butter made from cow’s milk is indigenous to the Indian sub-continent and an integral part of the cuisine in this region. With all the solid constituents of butter removed by heating, ghee in its pure form retains its purity and composition indefinitely and has been used as a medicinal agent, particularly in the treatment of wounds from ancient times. Ghee contains no water, has a very long shelf-life, and according to ayurvedic teaching its quality and healing properties improve with age. Honey is the nectar collected from flowers by bees. In the beehive, worker bees remove the liquid from nectar and with addition of enzymes convert it into syrupy honey which compresses 15% to 20% water and 80% to 85% sugar. Unlike ghee, which is used in specific geographic areas, honey is found all over the world. Honey has been used for its medicinal properties since time immemorial, particularly for its value in wound healing [2]. The use of honey in wound healing is increasing subsequent to the results of several clinical trials [3–5]. Honey has been shown to have an inhibitory effect on most strains of pathogenic bacteria [6]. The emergence of resistant bacteria has given a further impetus to its use in clinical practice [7].
Ayurvedic literature has documented, over the centuries, the healing properties of ghee both systemic and topical. Sushruta in his surgical treatise Sushruta Samhita postulated that the combination of ghee (ghrita) and honey (madhu) for wound healing would have the synergistic healing effect of each one. As this combination is used only where ghee is used, unlike the voluminous clinical literature on honey, there are very few reports of this combination for wound healing in medical literature [1, 8].
Materials and Methods
From November 1991 ghee and honey dressing has been in use to treat infected wounds in four hospitals in Mumbai – the J.J. Hospital., P.D. Hinduja Hospital, Parsee General Hospital, Breach Candy Hospital. Apprehensive of adverse effects and desirous of a comparable study in different hospitals it was decided, as stressed by Sushruta, to use the purest available ingredients. Enquiries convinced us that the ingredients which would maintain standard composition and quality would be Australian honey, (Capilano derived from the nectar of eucalypt and ground flora) and Amul Ghee which are the ingredients used for 19 years. While Indian honey is extensively used for wounds dressing, the only reason Australian honey was used is for its product uniformity for a project covering several years. Ghee is warmed and mixed with honey in a ratio by volume of one to two making a viscous homogenous mixture. Sterile gauze pre-cut to size and requirements of individual patients is impregnated with the thick liquid and stored in an airtight sterile box (Fig. 1). To ensure uniformity, since 1991, dressings used in all hospitals were made under the supervision of the O.R. Superintendent at Parsee General Hospital, at no extra cost to the patient. This dressing has been used with ethics committee approval and informed patient consent for patients in all socio-economic strata for infected wounds as seen in Teaching/General/Tertiary Care Hospitals. Swabs are taken for culture and sensitivity testing before commencing dressing and the wound size and status recorded. The wound is irrigated with saline. Dr. Gadvi in Kenya, out of necessity used tap water with similar results [1]. Depending on the depth of the wound four to six sheets of impregnated gauze are placed over the wound, tucked gently to obliterate dead space and cover the wound edges. Sterile gauze is placed over the dressing and kept in place by bandage or strapping. There is no rule of thumb for frequency of dressing change, which varies in every case. Dressing is changed when the exudate is so profuse that the concentration of ghee and honey on the wound surface is well below the desired Minimum Inhibitory Concentration (MIC), too diluted to be effective. Necrotic tissue and severe infection provoke profuse exudation and require frequent dressings. Once healthy granulation tissue appears frequency of dressing decreases to once in two to four days.
Fig. 1.

Ghee and Honey dressing. Gauze size varies with size of infected wound
Dressings are usually done as an outpatient, often by the patient at home. Appropriate antibiotics are used only in fulminant infections till swabs are negative. While ghee and honey has been found effective over a nineteen year experience, results of five recalcitrant subsets of infected wounds, studied in three hospitals (P.D.H.) (B.C.H.) (B.D.P.) over the last three years are presented in this study.
Results and Observations
Malignant ulcers with foul smelling fungation and necrosis, five fungating breast tumors, three fungating inguinal/iliac nodes. In every case treated there was reduction/disappearance of the foul odor within 7 to 12 days greatly improving the quality of life. While there was no change in disease outcome, the dressing ensured the ulcers became cleaner with less odour, discharge, bleeding, especially in the breast lesion making adjuvant therapy more acceptable.
-
Chronic Venous Ulcers: Thirteen cases of large, painful venous ulcers were treated, with duration of ulcers ranging from one to nine years. Venous ulcers are the result of chronic venous hypertension causing necrosis. Compression dressing, elevation as in all reported studies were the mainstay of treatment and were part of the treatment with ghee and honey dressing in all cases. . All RCTs, which show specific benefit of a particular dressing material for venous ulcers have been funded by their manufacturers. Independent study of these and all other products show none to be effective. It was under the shadow of these results that this study was undertaken.
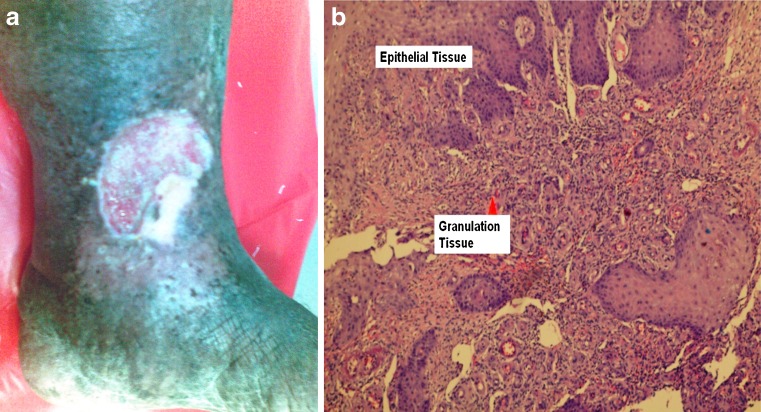
All were large, deep medial ulcers, with fibrotic margins, necrotic floor, weeping discharge, surrounded by deeply pigmented thickened skin not putting on pressure. All cases had undergone treatment, including multiple surgical procedures.. The first effect of this dressing on venous ulcers seen in every case was a dramatic relief from pain. In three cases, there was no improvement in terms of ulcer healing over three weeks and treatment was discontinued. The response was good in nine cases, ulcers were covered with healthy granulation and were skin grafted, but graft broke down on follow-up in four cases within 4–9 months. In one case islands of epithelium appeared spontaneously on the granulation tissue and spread to cover the ulcer. Unsure what these small pale islands were, histology showed epithelialisation Fig. 2. The over all results were not satisfactory. Literature reports varied results of honey in venous ulcers [9, 10].
Diabetic ulcers: 29 cases have been treated and evaluated. Established surgical principles-excision of all dead/infected tissue, laying open of infected cavities, control of diabetes were the mainstay of treatment. Fourteen of twenty nine cases were first seen after being treated elsewhere for 17 to 64 days. Dressing continued till the ulcer healed (10 cases) or the wound was healthy and ready for grafting (19 cases). Ulcers healed in 17 to 36 days (mean 21 days), healthy granulation was seen in 11 to 32 days (mean 16 days). Honey was not considered a factor compromising the patient’s diabetes. Seven cases required amputation of one or more toes due to gangrene, three of part of the fore foot due to bone destruction, but in no case did the leg require amputation. One case was lost to follow up, in one case part of the skin graft broke down. Similar results with honey are reported [6, 11].
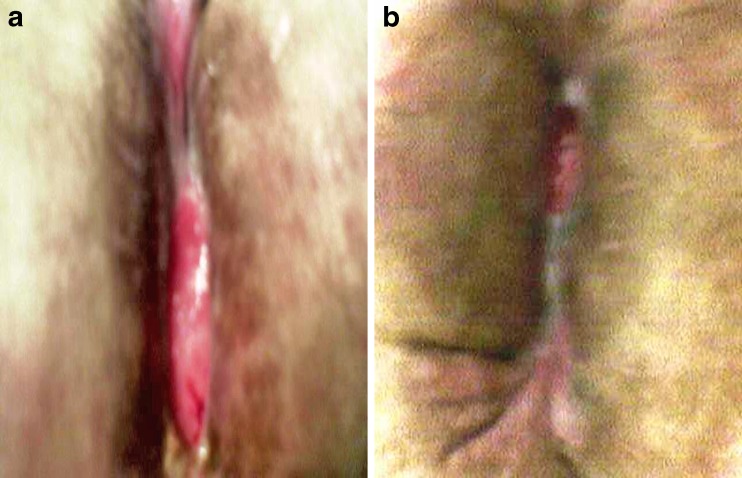
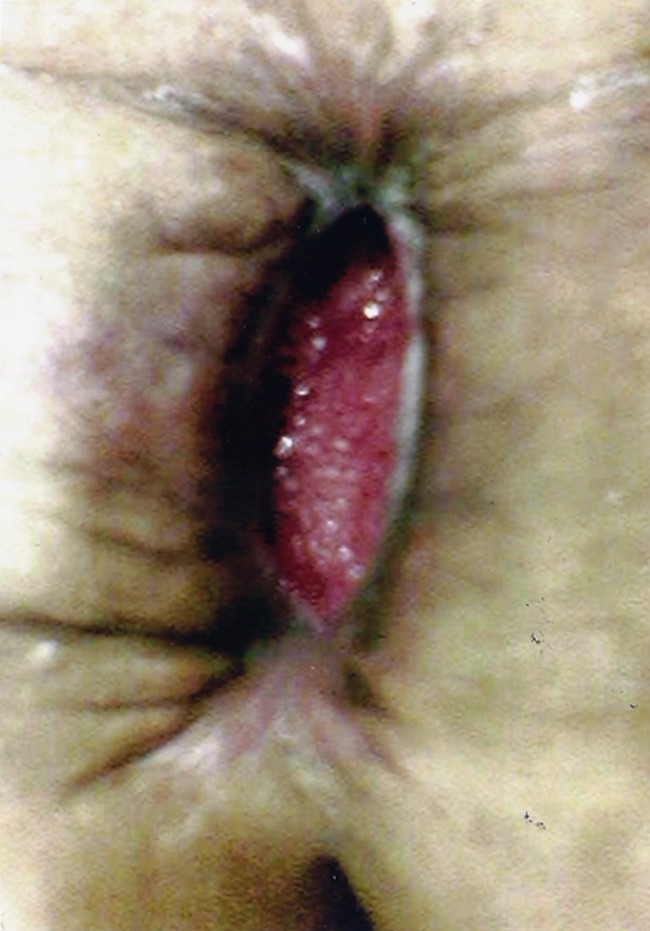
Infected mesh hernioplasties: In developing countries incisional hernia often grow to an enormous, grotesque size, are frequently seen in obese patients, and need a large mesh repair. Wound breakdown is not uncommon, exposing the mesh in the depth of the post operative wound. Eleven such cases with mesh exposed were treated, five of ours and six referred for treatment. In three cases mesh was exposed for the entire extent of the incision, in eight for part of the incision. In every case the exposed mesh was gradually covered with healthy granulation tissue, and the wound healed over a period of three to five weeks with spontaneous apposition of the edges without need for secondary suturing. Serial photographs allay disbelief. Figures 3, 4, 5. In no case did the mesh require removal. The integrity of hernia repair was not compromised. No reference in literature is found to this clinical application of ghee and honey dressing, which could be of use in infected mesh hernioplasty at any site.
-
Post caesarian, Post hysterectomy wound infection: Eleven cases, with infection deep to the sheath/muscle were treated. All healed with a thin scar without secondary suturing within two or three weeks. This finding is supported in literature [12, 13].
Table 1 summarises results.
Fig. 2.
a) Tiny islands of spontaneous epithelialisation coalesce to cover granulation, a phenomenon not previously reported. b) Histopathology of a small island
Fig. 3.
Granulation tissue growing into mesh on floor of dehiscent wound. Prolene sutures were removed. (Courtesy Professor H.G. Doctor)
Fig. 4.
Granulation has covered mesh and wound edges are coming closer together (Courtesy Professor H.G. Doctor)
Fig. 5.
a) Progressive healing of wound (Courtesy Professor H.G. Doctor) b) Spontaneous approximation without secondary suturing. (Courtesy Professor H.G. Doctor)
Table 1.
Summarizes results
| Lesion | Cases | Results |
|---|---|---|
| Fungating Malignant Lesions | 8 | Marked reduction in odour and discharge, greatly improving quality of life |
| Chronic Venous ulcers | 13 | Reduction in pain in all cases, but poor overall results |
| Diabetic ulcers | 29 | Overall good results |
| Infected mesh hernioplasty | 11 | Uniformly good results |
| Post-caesarian/hysterectomy wound infection | 11 | Uniformly good results |
| Total | 72 |
Discussion
Several properties of honey are responsible for wound healing. Honey is highly acidic, with a pH of 3.2 to 4.5, inimical to most pathogens [14], and has an osmolarity which inhibits the growth of most organisms [4, 15]. The osmotic action keeps the wound moist by drawing fluid from wound tissue which reduces edema, pain and ensures a constant supply of proteases explaining the desloughing and debridement action of honey [16]. Glucose oxidase present in honey produces hydrogen peroxide (H2O2) and gluconic acid to provide H2O2 in concentration inimical to pathogens but dilute enough not to damage host tissue [17]. Honey stimulates cytokine production [18], and expedites proliferation of B and T lymphocytes [19]. Reduction of wound oedema improves tissue perfusion, oxygenation and free flow of leucocytes and fibroblasts, promotes angiogenesis, granulation and epithelialization [20]
While bacteria cannot survive in honey, spores can and there is a theoretic risk of clostridium spores remaining dormant in honey. Medi-honey is now used in some centers in clinical practice where the honey is sterilized by gamma radiation which destroys the spores without affecting the properties of honey [21]. We have no experience of gamma radiated “medi honey.” However, with use in thousands of cases world-wide over several years in several trials no case of honey transmitted clostridium infection has been reported [22].
Sushruta taught that ghee apart from its own healing properties blends homogenously and augments the action of honey. Honey becomes watery at body temperature, and it is difficult to maintain honey in contact with the wound at a sufficiently high MIC without very frequent dressings. However, honey when bound with ghee maintains its viscosity at body temperature and is in longer and stronger contact with the wound surface augmenting its activity.
While ghee being derived from one produce is uniformly standardized, it needs to be stressed that honey which is from the nectar of an immense variety of flowers has tremendous variations in its various properties – colour, taste, viscosity, healing properties, which perhaps accounts for differences in clinical results. Honey from specific parts of the world(New Zealand, Australia, Yemen, Sardinia, India, South Africa) has claimed superior healing properties. Hence the use of the same honey in this trial over all these years.
Clinical experience over 19 years shows some distinct benefits of ghee and honey dressing.
Bacteriostatic, anti-microbial even in presence of drug resistant organisms.
Desloughing. Necrotic tissue, slough is separated, ‘digested’, removed.
Provokes rapid proliferation of healthy granulation tissue, of special benefit when preparing large areas, as in burns , for skin grafting.
Deodorant. The most foul smelling wounds lose their mal odour [23].
Maintains a moist, pliable wound, which heals with soft epithelization.
Reduces pain, specially in venous ulcers. Dressings are pain-free, require no anaesthesia, sedation. Being patient friendly, patient compliance is never an issue.
Contractile action. Widely separated wound edges are drawn together and approximated obviating the need for secondary suturing leaving a thin supple scar of special benefit in rural areas in developing countries. A fact most surgeons are reluctant to believe.
No adverse reaction was seen in any case.
-
Cost. Honey dressing is estimated at 4% of the cost of ‘scientifically accepted’, industry manufactured products [24] many of which have had far less stringent and unbiased clinical evaluation then honey dressing. Reducing/removing need for antibiotic cover further reduces the cost of treatment as does early healing. Fortunately both ghee and honey are available in abundance in most parts of the developing world, making this treatment in terms of both availability and cost ideally applicable in these countries.
An incidental observation. In developing countries ghee and honey dressing would be expected to be covered with flies and insects. Surprisingly, ghee and honey dressing acts as an insect repellent, no insects are found on these dressings.
Understandably the use of only honey or ghee and honey to treat infected wounds is viewed with strong skepticism by most , if not all surgeons. An Editorial on “Medical Folklore” tolerantly derided the use of honey as “worthless but harmless” [25]. This should not dishearten those few who are convinced of the clinical value of these wound dressings. In surgery many truths are born as blasphemies. Laparoscopic cholecystectomy which at first was frowned upon by the Surgical Establishment became the “gold standard” without a single RCT.
Evidence Based Medicine mandates an RCT to validate any trial. Several RCTs on use of honey with good results are reported but accepted only as Grade II evidence. This study was started as an RCT but was clearly open to fallacy. Many other workers in the field of wound healing have found similar difficulties to evaluate the effectiveness of comparative treatment in this diverse and complex patient population [26–29]. We felt a factual clinical trial was more honest, less pretentious and perhaps better than a flawed RCT [30].
This study is not meant to be a blanket endorsement for the unquestioned acceptance and use of ghee and honey dressing for infected wounds. It makes a plea that this and several previous studies on honey mandate that more clinical evaluation is merited to develop, in our time of drug resistant organisms, a remedy derived from India’s distant past, which has the potential for safe, pain free, low cost treatment and cure of one of the commonest surgical ailment, the infected wound.
Acknowledgements
Dr. Gadvi a scholarly surgeon working in Kenya with missionary zeal, who inspired this study. Dr. Rushad T. Udwadia, MS, FCPS, DNAB, FRCS Hon. Professor of Surgery J.J. Hospital, Consultant Surgeon Breach Candy Hospital, Parsee General Hospital, Mumbai who helped in this study. He declined the request to be a joint author as he felt his contribution did not merit it. Resident Surgeons in all the hospitals, who over several years, have helped in these trials with interest and perseverance. Ms. J. Bode, Ms. S. Konkrawala O.R. Superintendents, Parsee General Hospital who since 1991 have maintained gratis, a uniform product. Professor H.G. Doctor M.S., FRCSEd Emeritus Professor of Surgery J.J. Hospital, Senior Consultant Surgeon, Jain Clinic, Mumbai, who accepted the suggestion and used this dressing made at Parsee General Hospital for treatment of his patients with mesh exposed in the wound, documented, photographed and reported good results. Dr. Anita S. Bhaduri, M.D., Consultant Histopathologist, P.D.Hinduja Hospital for histopathology studies of spontaneous epithelialisation.
Funding
No source of funding
Conflict of interest
No conflict of interest
References
- 1.Udwadia TE. Ghee and honey dressing. Rural Surg. 2008;4:1–3. doi: 10.1007/s12262-011-0240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grover SK, Prasad GC. Uses of Madhu in Ayurveda. J NIMA. 1985;10:7–10. doi: 10.1016/0168-583X(85)90191-0. [DOI] [Google Scholar]
- 3.Subrahmanyam M. Topical application of honey for burn wound treatment – an overview. Ann Burns Fire Disasters. 2007;20:137–140. [PMC free article] [PubMed] [Google Scholar]
- 4.White RJ, Molan P (2005) A summary of published clinical research on honey in wound management. In White RJ, Cooper A, Molan P (Eds). Honey: a modern wound management product. Nurs Stand 20:130–143.
- 5.Ahmed AK, Hoekstra MJ, Hage J, et al. Honey medicated dressing: transformation of an ancient remedy into modern therapy. Ann Plast Surg. 2003;50:143–148. doi: 10.1097/01.SAP.0000032306.44107.C1. [DOI] [PubMed] [Google Scholar]
- 6.Cooper RA, Molan PC, Harding KG (1999) Antibacterial activity of honey against strains of Staphylococcus aureus from infected wounds. J Roy Soc Med 283–285 [DOI] [PMC free article] [PubMed]
- 7.Allen KL, Hutchinson G, Molan PC. The potential for using honey to treat wounds infected with MRSA and VRE. Melbourne : First World Wound Healing Congress; 2000. [Google Scholar]
- 8.Charde MS, Fulzele SV, Satturwar PM, et al. Wound healing and anti-inflammatory potential of madhu-ghrita. Indian J Pharm Sci. 2006;68:26–31. doi: 10.4103/0250-474X.22959. [DOI] [Google Scholar]
- 9.Wood B, Rademaker M, Molan P. Manuka honey, a low cost leg ulcer dressing. N Z Med J. 1997;110(1040):107. [PubMed] [Google Scholar]
- 10.Jull N, Walker VP, et al. Randomized clinical trial of honey-impregnated dressings for venous leg ulcers. Br J Surg. 2008;95:175–182. doi: 10.1002/bjs.6059. [DOI] [PubMed] [Google Scholar]
- 11.Eddy JJ, Gideonsen MD. Topical honey for diabetic foot ulcers. J Fam Pract. 2005;54:533–535. [PubMed] [Google Scholar]
- 12.Al-Waili NS, Saloom KY. Effects of topical honey on post-operative wound infections due to gram positive and gram negative bacteria following caesarian sections and hysterectomies. Eur J Med Res. 1999;4:126–130. [PubMed] [Google Scholar]
- 13.Phuapradit W, Saropala N. Topical application of honey in treatment of abdominal wound disruption. Aust N Z J Obstet Gynaecol. 1992;32:381–384. doi: 10.1111/j.1479-828X.1992.tb02861.x. [DOI] [PubMed] [Google Scholar]
- 14.Subrahmanyam M. Honey as a topical antibacterial agent for treatment of infected wounds. A prospective randomized clinical and histological study of superficial burn wound healing with honey and silver sulphadiazine. Burns. 1998;24(2):157–161. doi: 10.1016/S0305-4179(97)00113-7. [DOI] [PubMed] [Google Scholar]
- 15.Green AE. Wound healing properties of honey. Br J Surg. 1988;75:1278. doi: 10.1002/bjs.1800751236. [DOI] [PubMed] [Google Scholar]
- 16.Stephen-Haynes J. (2005). Implications of honey dressing within primary care. In: White RJ, Cooper A, Molan P (Eds) Honey: a modern wound management product. Wounds UK, Aberdeen. Nurs Stand 20:33–53
- 17.Hyslop PA, Hinshaw DB, Scraufstatter IU, et al. Hydrogen peroxide as a patent Bacteriostatic antibiotic implications for host defense. Free Radic Biol Med. 1995;19:31–37. doi: 10.1016/0891-5849(95)00005-I. [DOI] [PubMed] [Google Scholar]
- 18.Tonks AJ, Cooper RA, Jones KP, et al. Honey stimulates inflammatory cytokine production from monocytes. Cytokine. 2003;21:242–247. doi: 10.1016/S1043-4666(03)00092-9. [DOI] [PubMed] [Google Scholar]
- 19.Tonks AJ, Cooper RA, Price AJ, et al. Stimulation of the tnf-alpha release in monocytes by honey. Cytokine. 2001;14:240–242. doi: 10.1006/cyto.2001.0868. [DOI] [PubMed] [Google Scholar]
- 20.Stephen-Haynes J (2005). Implications of honey dressing within primary care. In: White RJ, Cooper A, Molan P (Eds) Honey: a modern wound management product. Wounds UK, Aberdeen, Nurs Stand 20:33–53
- 21.Molan PC, Allen KL. The effect of gamma-irridation on the antibacterial activity of honey. J Pharm Pharmacol. 1996;48:1206–1209. doi: 10.1111/j.2042-7158.1996.tb03922.x. [DOI] [PubMed] [Google Scholar]
- 22.Bell SG. The therapeutic use of honey. Neonatal. 2007;26:247–251. doi: 10.1891/0730-0832.26.4.247. [DOI] [PubMed] [Google Scholar]
- 23.Cooper RA, Gray D (2005) The control of wound malodour with honey based wound dressing and ointments. Wounds UK. Aberdeen 26–32
- 24.Ingle R, Levin J, Polinder K. Wound healing with honey- a randomized controlled trial. S Afr Med J. 2006;96:831–835. [PubMed] [Google Scholar]
- 25.Soffer A. Editorial: chinuahuas and laetrile, chelation therapy, and honey. Arch Intern Med. 1976;136:865–866. doi: 10.1001/archinte.1976.03630080007003. [DOI] [PubMed] [Google Scholar]
- 26.Gottrup F, Apelqvist J (2010) The challenge of using Randomised Trials in wound healing B.J.S. 97:303–304 [DOI] [PubMed]
- 27.Horkan L, Stansfield G, Miller M. An Analysis of systemic Reviews undertaken on standardized advanced wound dressings in the last ten years. J. wound Care. 2009;18:298–304. doi: 10.12968/jowc.2009.18.7.43113. [DOI] [PubMed] [Google Scholar]
- 28.Gottrup F. Evidence is a challenge in wound management. Int J Low extreme Wounds. 2006;5:74–75. doi: 10.1177/1534734606288412. [DOI] [PubMed] [Google Scholar]
- 29.Sultan MJ, Mccollum C. Don’t wast money when dressing leg ulcers. Br J Surg. 2009;96:1099–1100. doi: 10.1002/bjs.6801. [DOI] [PubMed] [Google Scholar]
- 30.Balasubramnina SP, Weiner M, Alshameeri Z, et al. Standards of reporting of randomised controlled trials in general surgery. Can we do better? Ann Surg. 2006;244:663–667. doi: 10.1097/01.sla.0000217640.11224.05. [DOI] [PMC free article] [PubMed] [Google Scholar]