Abstract
Hispanics are the fastest growing minority group in the United States and, compared with non-Hispanic whites, have a higher incidence of end-stage renal disease (ESRD). Examining novel factors that may explain this disparity in progression of chronic kidney disease (CKD) in Hispanics is urgently needed. Interpersonal and patient-centered characteristics, including health literacy, acculturation, and social support have been shown to affect health outcomes in other chronic diseases. However, these characteristics have not been well studied in the context of CKD, particularly in relation to disease knowledge, attitudes, and behaviors. In this paper, we examine the potential roles of these factors upon CKD progression in Hispanics and propose targeted therapeutic interventions.
Keywords: Chronic kidney disease, Hispanics, health disparities, health literacy, acculturation, social support
Hispanics are the fastest growing ethnic minority group in the United States. While Hispanics currently compose 15% of the population, they are projected to compose a quarter of the US population by 2050.1 Hispanics with CKD are at increased risk of disease progression compared with non-Hispanic whites.2–4 Accordingly, a better understanding of the factors contributing to the progression of mild to moderate CKD in Hispanics is critical for reducing health disparities and developing therapeutic interventions. While different names have been used to refer to Hispanics, Latinos, and Mexican Americans, for the purpose of this review, the term “Hispanic” refers to the ethnic background of persons of Latin American origin living in the United States.
A number of previous studies have found an increased prevalence of microalbuminuria in Hispanics compared with non-Hispanic whites.5,6 However, an analysis of the National Health and Nutrition Examination Survey (NHANES) found a lower prevalence of moderate kidney disease (eGFR <60 mL/min/1.73 m2) in Mexican Americans compared with non-Hispanic whites (1.0% vs 4.8%, respectively).7 Despite these inconsistent findings, the prevalence of ESRD is almost 2-fold higher in Hispanics than in non-Hispanic whites, and increased by 44% between 1996 and 2006.2 One potential explanation for the discrepancy between the lower prevalence of earlier stages of CKD compared with the higher ESRD prevalence is that Hispanics have a more rapid progression of kidney disease after its onset. Data from Kaiser Permanente of Northern California demonstrated that in patients with stage 3–4 CKD, Hispanic ethnicity was associated with a 1.3-fold increased risk for progression to ESRD when compared with non-Hispanic whites, suggesting that Hispanics may have a more rapid progression of CKD.3 The reasons for the increased prevalence of and risk for ESRD in Hispanics remain unclear and understudied.
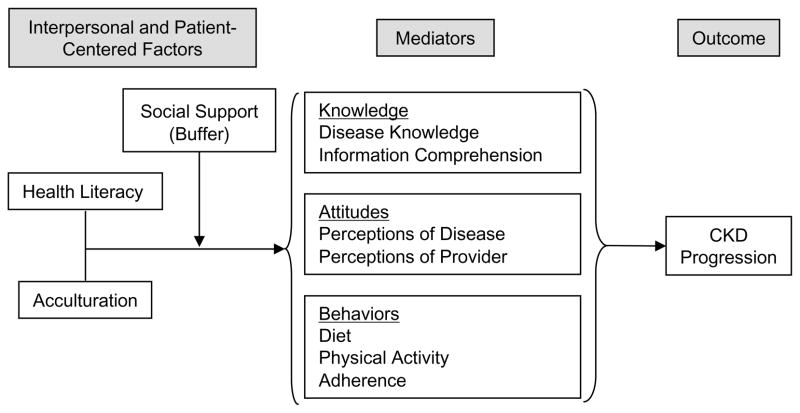
Drawing upon the literature on Hispanic health in other clinical contexts, we suggest several possible interpersonal and patient-centered factors that may influence the progression of CKD among Hispanics: health literacy, acculturation, and social support. In this paper, we present a conceptual model for the role of these patient-centered factors in the progression of CKD in Hispanics (Fig 1). We propose that the relationship of health literacy and acculturation with CKD progression in Hispanics is mediated by other patient-level factors, including knowledge, attitudes, and behaviors (Box 1). More specifically, we hypothesize that lower levels of health literacy and acculturation health literacy and acculturation are associated with poorer understanding of CKD, decreased adherence to prescribed medication therapy, and poorer health behaviors, including diet, physical activity, and tobacco use. These factors have been found to result in worse control of chronic diseases such as diabetes and hypertension, which in turn lead to the progression of CKD.8–10 Furthermore, we propose that social support may buffer the negative effects of low health literacy and low level of acculturation on progression of kidney disease.
Figure 1.
Role of Health Literacy, Acculturation, and Social Support in the Progression of Chronic Kidney Disease in Hispanics.
Box 1. Association of health literacy, social support, and acculturation with knowledge, behaviors and attitudes.
| Health literacy |
| Knowledge |
| Behavior |
| Attitudes |
| Social Support |
| Behavior |
Attitudes
|
| Acculturation |
| Knowledge |
| Behavior |
| Attitudes |
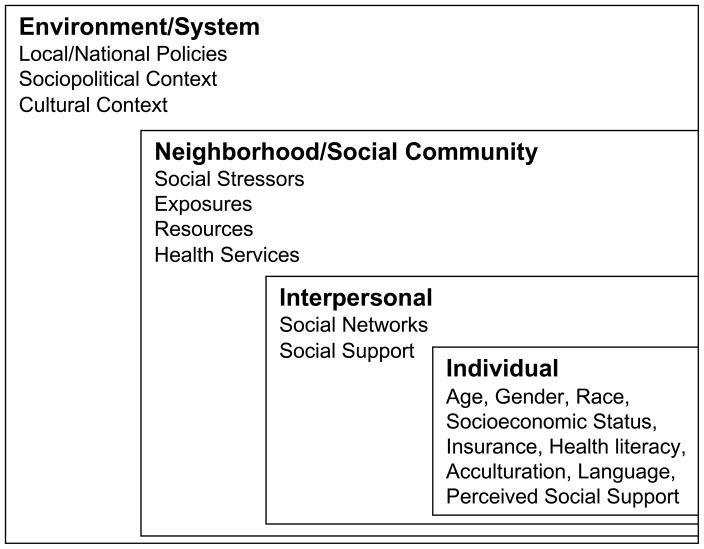
We recognize that Hispanics are a culturally, socioeconomically, and genetically heterogenous group and therefore these relationships may have subtle differences across Hispanic subgroups. Additonally, undocumented immigrants represent a growing and understudied segement of the Hispanic population.4 We speculate that the barriers outlined in our model are amplified for this vulnerable population. Also, since the relationships between these patient-centered factors are likely complex and may be interrelated, we acknowledge that our model may require iterative elaboration pending future research. Lastly, according to the socio-ecological perspective, health outcomes and behaviors result from the interplay between various health determinants including individual and interpersonal factors, the social community and the environment (Fig 2).31 From this perspective, health literacy and acculturation are important issues in Hispanics and need to be addressed in a systematic manner at the level of the individual, health care provider, and health care system.
Figure 2.
Socio-ecological model of factors influencing chronic kidney disease.
Health Literacy
Health literacy is the ability “to obtain, process and understand the basic health information and services needed to make appropriate health decisions.”32 A recent study by the US Department of Education estimated that 93 million US residents (43% of American adults) have limited health literacy skills,33 which may make it difficult for them to understand and act on patient education materials. Patients with low health literacy have decreased use of preventive services,34 knowledge of chronic diseases,11 and medication adherence.16 Additionally, individuals with low health literacy have poorer self-reported health,35 increased hospitalizations,36 and increased mortality.37 Moreover, low health literacy is associated with up to four times higher health care costs.38 The potential for health literacy to affect patients’ chronic disease management has been recognized by the Institute of Medicine, which in 2004, issued a call to action for research in health literacy.39
Examining health literacy in Hispanics is important because minorities and non-English speakers are more likely to have low functional health literacy than non-Hispanic whites.40 Additonally, according to the 2005 American Community Survey, 73% of foreign-born Hispanics speak English “less than very well” as did up to 13% of US born Hispanics.41 Spanish-speaking Hispanics have a nearly two-fold greater likelihood of weak or insufficient health literacy compared with English-speaking Hispanics.40 These lower levels of health literacy may contribute to adverse lifestyles and poorer chronic disease understanding and self-management, as has been demonstrated for conditions such as diabetes and hypertension.11,42
The potential importance of health literacy in CKD has recently received recognition,43 but has not been extensively investigated.44 Educational level, a construct that is correlated with health literacy, has been well studied and found to correlate with poor CKD health outcomes.45–47 However, only a few studies have evaluated health literacy and CKD outcomes.44,48,49 These studies have focused on characterizing literacy levels of dialysis or kidney transplant recipients44,48 or on assessing how literacy explains patients’ access to transplantation.50 More recently, a prospective study of incident dialysis patients demonstrated an association between health literacy and increased mortality.49 Virtually no research has investigated the relationship between literacy and CKD outcomes, albeit, others have conceptualized and called for investigation into such relationships.43
Low health literacy may likely contribute to poor health outcomes in CKD through various mechanisms involving knowledge, attitudes, and behavior (Fig 1). Low health literacy can be problematic because of the need to understand forms, signs, and instructions encountered in navigating the health care system. Understanding of disease and adherence to treatment represent additional challenges for those with limited health literacy.11,16 Low literate individuals with CKD may have difficulty communicating with health care providers, which is essential to process disease information and carry out instructions regarding diet, physical activity, and medication use. For example, a patient with advanced CKD often must adhere to complex medication and dietary regimens, which may include multiple medications for hypertension and diabetes, a phosphate binder, an erythropoiesis stimulating agent, and a low potassium diet. To effectively adhere to such complex regimens, patients must have a clear understanding of the instructions provided, a basic understanding of the importance of these regimens for CKD, and the severity of CKD complications if regimens are not followed. Hyperphosphatemia, for instance, a common complication of advanced CKD, requires adherence to binders which, to be efficacious, must be taken with meals. A patient who has been instructed to take phosphate binders three times a day may believe that they are adherent, but without adequate understanding of when to take the binder and/or of how the binder works, will not receive the therapeutic benefit of the medication.
Patients with limited health literacy may encounter difficulty learning about their CKD from various sources of health information. Although health care providers often rely on written materials for patient education, these materials are frequently created at higher education levels and may not be appropriate for those with low health literacy.51 In 2003, the National Assessment of Adult Literacy (NAAL) found that 44% of Hispanics had below basic prose literacy levels.52 Feelings of shame may prevent patients from informing health care providers about their limited ability to read. Also, providers rarely screen their patients for health literacy level, and frequently overestimate their ability to accurately make this assessment.53 With the increased reliance on technology to deliver health information and services, those with low health literacy are at increased risk of being inadequately educated about their CKD. The internet has increasingly become a source of health information and health empowerment for patients. However, compared with non-Hispanic whites, Hispanics are less likely to search for health information online and are less likely than non-Hispanic whites to use electronic health services.54 Information-seeking opportunities though growth in internet-based technologies may magnify the difference in information access between those with lower and higher health literacy.
Several types of health communication interventions have been successfully utilized in patients with low health literacy and medical conditions including diabetes,55 asthma,56 and cancer.57 Interventions have included pictorial aids, group informational sessions, pharmacists, automated phone calls and the use of media (eg, other nontextual formats, including audiovisual aids and the internet).58–60 These types of interventions have been most successful in improving knowledge and self-efficacy in disease self-management. More recent interventions aimed at individuals with limited health literacy have also been shown to improve pneumococcal vaccination rates and accuracy of self-reported medication adherence. These findings suggest that the effect of health literacy on health outcomes may be modifiable. By understanding the relationship between health literacy and CKD, we may identify a therapeutic target in CKD progression. A health literacy intervention for Hispanics with CKD would need to address not only literacy, but also language and cultural needs. One available educational tool (RenalTouchTM; www.renaltouch.com) provides education on CKD-related topics to predialysis patients through the use of interactive, computer-based modules which do not require computer skills.61 Another potential educational tools for Hispanics with CKD is the fotonovela. A fotonovela is an informational tool that incorporates photographs with simple text bubbles to deliver a message within a captivating, dramatic story.62 Fotonovelas have been used to provide education regarding tuberculosis, depression, and nutrition to Hispanics.62–64 The National Kidney Foundation has developed a fotonovela to educate dialysis patients.65 The effects of RenalTouch and fotonovelas on CKD outcomes in Hispanics need to be evaluated.
Acculturation
Acculturation refers to the manner by which people take on the attitudes, mores, traditions, convictions, and behaviors of another culture.66 A common misunderstanding about acculturation is that individuals select between their own or the mainstream cultural tradition.67 Yet, many choose to adopt multiple cultural traditions to different degrees. Determining where an individual falls along this continuum of acculturation is difficult to ascertain.67 Frequently proxy variables are used to measure acculturation,18 including: primary language, length of residency in the new culture, place of birth, preferred ethnic identity, ethnicity of friends and associates, among others.67 However, these measurements fail to capture values and beliefs, which are fundamental expressions of an individual’s cultural orientation and inform perceptions of health and illness. Logistically, culturally-based values and beliefs are difficult to enumerate and to measure. For this reason, current measurements of acculturation tend to separate culture from the social structure and processes that generate beliefs and behaviors.67 Therefore, some scholars advocate that current measurements of acculturation are incomplete because they are unidimensional and that better measures need to be explored.67 Nonetheless, there is value in the available data regarding acculturation and the health of Hispanics as it may provide clues regarding health disparities in this ethnic group.68
Although it is well documented that level of acculturation is associated with health outcomes, studies report conflicting findings regarding the direction of the relationship between Hispanics’ acculturation and chronic diseases.69,70 For instance, Hispanics with less acculturation have a decreased prevalence of hypertension and diabetes,69,70 however, they have worse control of blood pressure, and an increased prevalence of cardiovascular risk factors.71 Similarly, acculturation has been found to have an impact on health-related behavior (eg, physical activity, diet, and other lifestyle habits) in both positive and negative ways.27,72 Higher levels of acculturation have been associated with unhealthy behaviors such as increased alcohol consumption, increased tobacco use, increased fast food consumption, and lower intake of fruits and vegetables.26 On the other hand, higher acculturation has also been associated with factors that may have a positive impact on health, including increased use of preventive health service,higher rates of health insurance, and higher health literacy.40,73,74
The relationship between acculturation and CKD in Hispanics has not been well studied. A recent analysis of Hispanics enrolled in MESA (the Multi-Ethnic Study of Atherosclerosis) found that more acculturated individuals had lower eGFR compared with less acculturated individuals. This association was not attenuated by traditional risk factors for CKD, but was attenuated by behaviors.75 The relationship between acculturation and CKD progression has never been evaluated. Differences in acculturation level among Hispanic individuals may explain health disparities in CKD progression and understanding this association may help to identify individuals who are at risk of progression. In considering this association, it is important to recognize the close interactions between acculturation, health literacy, and socioeconomic status. Compared with US-born individuals, foreign-born Hispanics tend to have lower educational attainment (a proxy for lower health literacy) and lower median income.63 Lower socioeconomic status is an important predictor of CKD prevalence and progression and may mediate the potential relationship of acculturation with progression of CKD.28,29 However, acculturation may influence progression of CKD in Hispanics through a variety of patient level factors (Fig1).
English language proficiency is a prominent marker of acculturation.76 Non-English-speaking individuals may face significant barriers to health care access and effective patient-provider interaction.77 Language barriers have been associated with poorer quality of care77 and dissatisfaction with care.78 However, the concept of acculturation also encompasses beliefs and values which may affect how a person experiences and responds to illness and the type of health care that they seek. For example, some Hispanics may believe in folk illneses or may classify illness as natural (the will of God) or unnatural (arising from an evil force acting on the individual).79 People holding these beliefs may feel they cannot control their illness,79 and may not seek medical help or not follow medical advice. Cultural differences between the health care provider and the patient can inform their communication, which can potentially affect medical care. For instance, patients with CKD are often asked to follow low phosphorus and potassium diets. Less acculturated Hispanics whose diet includes beans, fruits, and tuberous vegetables, which are high in potassium and phosphorus, may not receive culturally-relevant information regarding these foods if their providers are not aware of the typical Hispanic diet. Health care providers whose clinical practices include Hispanic patients should try to be familiar with Hispanic cultural dietary habits to better educate their patients about the effects of such foods on CKD and to help suggest culturally appropriate alternatives.
Although no interventions have been implemented to slow progression of CKD among Hispanic patients with low acculturation, interventions have been used successfully in diabetes. Health promoters (promotoras) have been utilized to improve patients’ knowledge, self-care, and glycemic control in Hispanics with diabetes.80,81 Promotoras are health community workers, who are usually a member of the community, and serve as a liaison between the community and health care providers. As a member of the community, the promotora inspires trust and is aware of underlying cultural beliefs that affect patients’ access to health care, disease understanding, adherence to therapy, and other health behaviors. Accordingly, promotoras are in an ideal position to address patients’ health beliefs in a culturally sensitive manner. Patients who interact with promotoras are more likely to ask questions regarding disease and therapy, which may lead to improved disease understanding and adherence. Furthermore, promotoras can help patients navigate the health system, and translate and simplify provider instructions. Interventions utilizing health promoters for Hispanics with CKD may help overcome barriers related to lower acculturation and health literacy.
Social Support
Social support refers to resources provided by others that “lead the subject to believe that he is cared for and loved, esteemed, and a member of a network of mutual obligations.”82 Members of one’s social network who provide support include: peers, family members, religious groups members, professionals, etc. While social networks overlap with social support, not all members of one’s social network provide support.83 Perceived social support is the extent to which an individual believes that their social support needs are being met by this social network.84 Perceived social support has long been recognized to have an impact on health.85 Higher levels of social support have been shown to associate with enhanced use of preventive services86 and decreased morbidity and mortality.87 Among dialysis patients, greater perceived social support is associated with improved mortality, greater adherence,88 decreased symptoms of depression, improved perception of illness, and increased quality of life.89 The mechanisms by which perceived social support affects chronic disease outcomes such as those relevant to CKD are not well understood.
These mechanisms may include decreased stress through motivational, emotional, or neuroendocrine effects85; as well as alterations in the cardiovascular, endocrine, and immune system.90 According to posited theories, members of social networks provide emotional (intimacy or confiding about emotions), tangible (providing financial assistance, goods, services, or assistance with tasks), informational (providing useful information, guidance), and companionship support (social companionship).91 These types of supports can be instrumental to self-care management of diabetes, hypertension, and other risk factors for progression of CKD. Similarly, greater perceived social support may help buffer the adverse effects of lower levels of health literacy and acculturation on CKD progression (Fig 1). For example, a patient with CKD may not understand their physician’s instructions regarding home blood pressure monitoring, but they may have a partner who does and can help the patient implement the recommendations. Similarly, a partner may help by reading medication labels or, for Spanish speakers, by translating instructions. Many Hispanics have a strong sense of familismo, or strong attachment to nuclear and extended families.92 As such, they have a strong reliance on relatives to provide support and help, and they feel a duty to support their relatives with both material and emotional assistance.92 An analysis of the effect of acculturation on familismo, found that familismo is similar across Hispanic subgroups but changes with increasing acculturation.93 With higher levels of acculturation, the perceived cultural obligation to provide support for family members was found to diminish, however the perception of family support remained the same. Social support represents a modifiable factor and may serve as a therapeutic target for Hispanics with CKD. As discussed earlier, the use of promotoras could be a potential social support intervention.
Conclusions
As the number of Hispanics with CKD continues to grow and disparities among this group remain prominent, it is imperative to examine factors contributing to the problem of CKD progression in Hispanics. We have outlined potential mechanisms by which health literacy, acculturation, and social support may influence the progression of kidney disease in Hispanics. Lower levels of health literacy and acculturation are associated with differences in knowledge, attitudes, and behaviors which may contribute to CKD progression. Higher levels of social support may ameliorate the effects of low health literacy and acculturation on CKD progression. However, these patient-centered factors have not yet been studied in Hispanics with CKD and their effects on CKD progression remain unknown. Future research is needed to needed to elucidate the relationship between these factors and the progression of CKD in Hispanics and could form the basis for targeted interventional trials focused on retarding the progression of CKD in this growing population.
Acknowledgments
Support: Dr. Lora’s work is support by the Research Supplent to Promote Diversity in Health-Related Research (R01 DK72231). Dr. Fischer is supported by the Department of Veterans Affairs Health Service Research Development (HSR&D) Career Development Award. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Footnotes
Financial Disclosure: The authors declare they have no relevant financial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.U.S.Census. [Accessed February 26, 2009];Nation's population one-third minority. 2008 http://www.census.gov/Press-Release/www/releases/archives/population/006808.html [serial online]
- 2.Collins AJ, Foley RN, Herzog C, et al. United States Renal Data System 2008 Annual Data Report Abstract. Am J Kidney Dis. 2009;53:vi–374. doi: 10.1053/j.ajkd.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Peralta CA, Shlipak MG, Fan D, et al. Risks for end-stage renal disease, cardiovascular events, and death in Hispanic versus non-Hispanic white adults with chronic kidney disease. J Am Soc Nephrol. 2006;17:2892–2899. doi: 10.1681/ASN.2005101122. [DOI] [PubMed] [Google Scholar]
- 4.Lora CM, Daviglus ML, Kusek JW, et al. Chronic kidney disease in United States Hispanics: a growing public health problem. Ethn Dis. 2009;19:466–472. [PMC free article] [PubMed] [Google Scholar]
- 5.Bryson CL, Ross HJ, Boyko EJ, Young BA. Racial and ethnic variations in albuminuria in the US Third National Health and Nutrition Examination Survey (NHANES III) population: associations with diabetes and level of CKD. Am J Kidney Dis. 2006;48:720–726. doi: 10.1053/j.ajkd.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 6.Jones CA, Francis ME, Eberhardt MS, et al. Microalbuminuria in the US population: third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2002;39:445–459. doi: 10.1053/ajkd.2002.31388. [DOI] [PubMed] [Google Scholar]
- 7.Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41:1–12. doi: 10.1053/ajkd.2003.50007. [DOI] [PubMed] [Google Scholar]
- 8.McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87:443–494. doi: 10.1111/j.1468-0009.2009.00564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sclar DA, Chin A, Skaer TL, Okamoto MP, Nakahiro RK, Gill MA. Effect of health education in promoting prescription refill compliance among patients with hypertension. Clin Ther. 1991;13:489–495. [PubMed] [Google Scholar]
- 10.Sacks FM, Campos H. Dietary therapy in hypertension. N Engl J Med. 2010;362:2102–2112. doi: 10.1056/NEJMct0911013. [DOI] [PubMed] [Google Scholar]
- 11.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 12.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 13.Longo DR, Schubert SL, Wright BA, Lemaster J, Williams CD, Clore JN. Health information seeking, receipt, and use in diabetes self-management. Ann Fam Med. 2010;8:334–340. doi: 10.1370/afm.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shigaki C, Kruse RL, Mehr D, et al. Motivation and diabetes self-management. Chronic Illn. 2010;6:202–214. doi: 10.1177/1742395310375630. [DOI] [PubMed] [Google Scholar]
- 15.Kripalani S, Gatti ME, Jacobson TA. Association of age, health literacy, and medication management strategies with cardiovascular medication adherence. Patient Educ Couns. 2010;81:177–181. doi: 10.1016/j.pec.2010.04.030. [DOI] [PubMed] [Google Scholar]
- 16.Kalichman SC, Ramachandran B, Catz S. Adherence to combination antiretroviral therapies in HIV patients of low health literacy. J Gen Intern Med. 1999;14:267–273. doi: 10.1046/j.1525-1497.1999.00334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hirsh JM, Boyle DJ, Collier DH, Oxenfeld AJ, Caplan L. Health literacy predicts the discrepancy between patient and provider global assessments of rheumatoid arthritis activity at a public urban rheumatology clinic. J Rheumatol. 2010;37:961–966. doi: 10.3899/jrheum.090964. [DOI] [PubMed] [Google Scholar]
- 18.Ciampa PJ, Osborn CY, Peterson NB, Rothman RL. Patient numeracy, perceptions of provider communication, and colorectal cancer screening utilization. J Health Commun. 2010;15 (Suppl 3):157–168. doi: 10.1080/10810730.2010.522699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Briggs AM, Jordan JE, Buchbinder R, et al. Health literacy and beliefs among a community cohort with and without chronic low back pain. Pain. 2010;150:275–283. doi: 10.1016/j.pain.2010.04.031. [DOI] [PubMed] [Google Scholar]
- 20.Emmons KM, Barbeau EM, Gutheil C, Stryker JE, Stoddard AM. Social influences, social context, and health behaviors among working-class, multi-ethnic adults. Health Educ Behav. 2007;34:315–334. doi: 10.1177/1090198106288011. [DOI] [PubMed] [Google Scholar]
- 21.Thompson HS, Littles M, Jacob S, Coker C. Posttreatment breast cancer surveillance and follow-up care experiences of breast cancer survivors of African descent: an exploratory qualitative study. Cancer Nurs. 2006;29:478–487. doi: 10.1097/00002820-200611000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Alfonso V, Geller J, Bermbach N, Drummond A, Montaner JS. Becoming a “treatment success”: what helps and what hinders patients from achieving and sustaining undetectable viral loads. AIDS Patient Care STDS. 2006;20:326–334. doi: 10.1089/apc.2006.20.326. [DOI] [PubMed] [Google Scholar]
- 23.Guzman SJ, Nicassio PM. The contribution of negative and positive illness schemas to depression in patients with end-stage renal disease. J Behav Med. 2003;26:517–534. doi: 10.1023/a:1026249702054. [DOI] [PubMed] [Google Scholar]
- 24.Constantine ML, Rockwood TH, Schillo BA, Castellanos JW, Foldes SS, Saul JE. The relationship between acculturation and knowledge of health harms and benefits associated with smoking in the Latino population of Minnesota. Addict Behav. 2009;34:980–983. doi: 10.1016/j.addbeh.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 25.Vega WA, Sallis JF, Patterson T, Rupp J, Atkins C, Nader PR. Assessing knowledge of cardiovascular health-related diet and exercise behaviors in Anglo- and Mexican-Americans. Prev Med. 1987;16:696–709. doi: 10.1016/0091-7435(87)90052-1. [DOI] [PubMed] [Google Scholar]
- 26.Ayala GX, Baquero B, Klinger S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. J Am Diet Assoc. 2008;108:1330–1344. doi: 10.1016/j.jada.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu J, Probst JC, Harun N, Bennett KJ, Torres ME. Acculturation, physical activity, and obesity among Hispanic adolescents. Ethn Health. 2009;14:509–525. doi: 10.1080/13557850902890209. [DOI] [PubMed] [Google Scholar]
- 28.Barron F, Hunter A, Mayo R, Willoughby D. Acculturation and adherence: issues for health care providers working with clients of Mexican origin. J Transcult Nurs. 2004;15:331–337. doi: 10.1177/1043659604268950. [DOI] [PubMed] [Google Scholar]
- 29.Wallace LS, DeVoe JE, Heintzman JD, Fryer GE. Language preference and perceptions of healthcare providers' communication and autonomy making behaviors among Hispanics. J Immigr Minor Health. 2009;11:453–459. doi: 10.1007/s10903-008-9192-9. [DOI] [PubMed] [Google Scholar]
- 30.Hubbell FA, Chavez LR, Mishra SI, Valdez RB. Beliefs about sexual behavior and other predictors of Papanicolaou smear screening among Latinas and Anglo women. Arch Intern Med. 1996;156:2353–2358. [PubMed] [Google Scholar]
- 31.Bronfenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1997;32:513–531. [Google Scholar]
- 32.Committee on Health Literacy BoNaMH. Health literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press; 2010. [Google Scholar]
- 33.Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America's Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006-483) Washington, DC: US Department of Education; 2006. [Google Scholar]
- 34.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 35.Guerra CE, Shea JA. Health literacy and perceived health status in Latinos and African Americans. Ethn Dis. 2007;17:305–312. [PubMed] [Google Scholar]
- 36.Baker DW, Gazmararian JA, Williams MV, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. 2002;92:1278–1283. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167:1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 38.Weiss BD, Palmer R. Relationship between health care costs and very low literacy skills in a medically needy and indigent Medicaid population. J Am Board Fam Pract. 2004;17:44–47. doi: 10.3122/jabfm.17.1.44. [DOI] [PubMed] [Google Scholar]
- 39.Glassman P. Health literacy. National Network of Libraries of Medicine New England Region; 2010. [Accessed November 15, 2009]. http://nnlm.gov/outreach/consumer/hlthlit.html [serial online] [Google Scholar]
- 40.Williams MV, Parker RM, Baker DW, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274:1677–1682. [PubMed] [Google Scholar]
- 41.Pew Hispanic Center. [Accessed May 25, 2010];A statistical portrait of Hispanic at mid-decade. 2006 http://pewhispanicorg/reports/middecade/ [serial online]
- 42.Osborn CY, Cavanaugh K, Wallston KA, Rothman RL. Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun. 2010;15 (Suppl 2):146–158. doi: 10.1080/10810730.2010.499980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Devraj R, Gordon EJ. Health literacy and kidney disease: toward a new line of research. Am J Kidney Dis. 2009;53:884–889. doi: 10.1053/j.ajkd.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 44.Gordon EJ, Wolf MS. Health literacy skills of kidney transplant recipients. Prog Transplant. 2009;19:25–34. doi: 10.1177/152692480901900104. [DOI] [PubMed] [Google Scholar]
- 45.Fored CM, Ejerblad E, Fryzek JP, et al. Socio-economic status and chronic renal failure: a population-based case-control study in Sweden. Nephrol Dial Transplant. 2003;18:82–88. doi: 10.1093/ndt/18.1.82. [DOI] [PubMed] [Google Scholar]
- 46.Bruce MA, Beech BM, Crook ED, et al. Association of socioeconomic status and CKD among African Americans: the Jackson Heart Study. Am J Kidney Dis. 2010;55:1001–1008. doi: 10.1053/j.ajkd.2010.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shoham DA, Vupputuri S, Diez Roux AV, et al. Kidney disease in life-course socioeconomic context: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis. 2007;49:217–226. doi: 10.1053/j.ajkd.2006.11.031. [DOI] [PubMed] [Google Scholar]
- 48.Chisholm MA, Fair J, Spivey CA. Health literacy and transplant patients and practitioners. Public Health. 2007;121:800–803. doi: 10.1016/j.puhe.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 49.Cavanaugh KL, Wingard RL, Hakim RM, et al. Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol. 2010;21:1979–1985. doi: 10.1681/ASN.2009111163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grubbs V, Gregorich SE, Perez-Stable EJ, Hsu CY. Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol. 2009;4:195–200. doi: 10.2215/CJN.03290708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilson M. Readability and patient education materials used for low-income populations. Clin Nurse Spec. 2009;23:33–40. doi: 10.1097/01.NUR.0000343079.50214.31. [DOI] [PubMed] [Google Scholar]
- 52.National Center for Education Statistics. National Assesment of Adult Literacy (NAAL): A first look at the literacy of America's adults in the 21st century. 2006. 5–25–0010. Ref Type: Report. [Google Scholar]
- 53.Kelly PA, Haidet P. Physician overestimation of patient literacy: a potential source of health care disparities. Patient Educ Couns. 2007;66:119–122. doi: 10.1016/j.pec.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 54.Hsu J, Huang J, Kinsman J, et al. Use of e-Health services between 1999 and 2002: a growing digital divide. J Am Med Inform Assoc. 2005;12:164–171. doi: 10.1197/jamia.M1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rothman RL, DeWalt DA, Malone R, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;292:1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 56.Sobel RM, Paasche-Orlow MK, Waite KR, Rittner SS, Wilson EA, Wolf MS. Asthma 1-2-3: a low literacy multimedia tool to educate African American adults about asthma. J Community Health. 2009;34:321–327. doi: 10.1007/s10900-009-9153-9. [DOI] [PubMed] [Google Scholar]
- 57.Wydra EW. The effectiveness of a self-care management interactive multimedia module. Oncol Nurs Forum. 2001;28:1399–1407. [PubMed] [Google Scholar]
- 58.Schaefer CT. Integrated review of health literacy interventions. Orthop Nurs. 2008;27:302–317. doi: 10.1097/01.NOR.0000337283.55670.75. [DOI] [PubMed] [Google Scholar]
- 59.Clement S, Ibrahim S, Crichton N, Wolf M, Rowlands G. Complex interventions to improve the health of people with limited literacy: A systematic review. Patient Educ Couns. 2009;75:340–351. doi: 10.1016/j.pec.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 60.Glasgow RE, Boles SM, McKay HG, Feil EG, Barrera M., Jr The D-Net diabetes self-management program: long-term implementation, outcomes, and generalization results. Prev Med. 2003;36:410–419. doi: 10.1016/s0091-7435(02)00056-7. [DOI] [PubMed] [Google Scholar]
- 61.Kleinman K. An Article on CKD by Dr Kleinman. 2005. Ref Type: Online Source. [Google Scholar]
- 62.Cabassa LJ, Molina GB, Baron M. Depression Fotonovela: Development of a Depression Literacy Tool for Latinos With Limited English Proficiency. Health Promot Pract. 2010 doi: 10.1177/1524839910367578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cabrera DM, Morisky DE, Chin S. Development of a tuberculosis education booklet for Latino immigrant patients. Patient Educ Couns. 2002;46:117–124. doi: 10.1016/s0738-3991(01)00156-2. [DOI] [PubMed] [Google Scholar]
- 64.Sberna HM, Hinojosa R, Nelson DA, et al. Salud de la mujer: using fotonovelas to increase health literacy among Latinas. Prog Community Health Partnersh. 2010;4:25–30. doi: 10.1353/cpr.0.0106. [DOI] [PubMed] [Google Scholar]
- 65.National Kidney Foundation. 2011 http://www.kidney.org/professionals/kls/novella/index.html [serial online]
- 66.Lafromboise T, Coleman HLK, Gerton J. Psychological Impact of Biculturalism - Evidence and Theory. Psychological Bulletin. 1993;114:395–412. doi: 10.1037/0033-2909.114.3.395. [DOI] [PubMed] [Google Scholar]
- 67.Hunt LM, Schneider S, Comer B. Should “acculturation” be a variable in health research? A critical review of research on US Hispanics. Soc Sci Med. 2004;59:973–986. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 68.Siatkowski AA. Hispanic acculturation: a concept analysis. J Transcult Nurs. 2007;18:316–323. doi: 10.1177/1043659607305193. [DOI] [PubMed] [Google Scholar]
- 69.Moran A, Roux AV, Jackson SA, et al. Acculturation is associated with hypertension in a multiethnic sample. Am J Hypertens. 2007;20:354–363. doi: 10.1016/j.amjhyper.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 70.Kandula NR, Diez-Roux AV, Chan C, et al. Association of acculturation levels and prevalence of diabetes in the multi-ethnic study of atherosclerosis (MESA) Diabetes Care. 2008;31:1621–1628. doi: 10.2337/dc07-2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Eamranond PP, Legedza AT, Diez-Roux AV, et al. Association between language and risk factor levels among Hispanic adults with hypertension, hypercholesterolemia, or diabetes. Am Heart J. 2009;157:53–59. doi: 10.1016/j.ahj.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Perez-Escamilla R. Dietary quality among Latinos: is acculturation making us sick? J Am Diet Assoc. 2009;109:988–991. doi: 10.1016/j.jada.2009.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Thamer M, Richard C, Casebeer AW, Ray NF. Health insurance coverage among foreign-born US residents: the impact of race, ethnicity, and length of residence. Am J Public Health. 1997;87:96–102. doi: 10.2105/ajph.87.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hu DJ, Covell RM. Health care usage by Hispanic outpatients as function of primary language. West J Med. 1986;144:490–493. [PMC free article] [PubMed] [Google Scholar]
- 75.Day EC, Li Y, Diez-Roux A, et al. Associations of acculturation and kidney dysfunction among Hispanics and Chinese from the Multi-Ethnic Study of Atherosclerosis (MESA) Nephrol Dial Transplant. 2010 doi: 10.1093/ndt/gfq676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Marín G, Sabogal F, Marín B, Otero-Sabogal R, Perez-Stable E. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9:183–205. [Google Scholar]
- 77.Timmins CL. The impact of language barriers on the health care of Latinos in the United States: a review of the literature and guidelines for practice. J Midwifery Womens Health. 2002;47:80–96. doi: 10.1016/s1526-9523(02)00218-0. [DOI] [PubMed] [Google Scholar]
- 78.Carrasquillo O, Orav EJ, Brennan TA, Burstin HR. Impact of language barriers on patient satisfaction in an emergency department. J Gen Intern Med. 1999;14:82–87. doi: 10.1046/j.1525-1497.1999.00293.x. [DOI] [PubMed] [Google Scholar]
- 79.Otero-Sabogal R, Sabogal F, Perez-Stable EJ, Hiatt RA. Dietary practices, alcohol consumption, and smoking behavior: ethnic, sex, and acculturation differences. J Natl Cancer Inst Monogr. 1995:73–82. [PubMed] [Google Scholar]
- 80.Norris SL, Chowdhury FM, Van LK, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006;23:544–556. doi: 10.1111/j.1464-5491.2006.01845.x. [DOI] [PubMed] [Google Scholar]
- 81.Gerber BS, Cano AI, Caceres ML, et al. A pharmacist and health promoter team to improve medication adherence among Latinos with diabetes. Ann Pharmacother. 2010;44:70–79. doi: 10.1345/aph.1M389. [DOI] [PubMed] [Google Scholar]
- 82.Cobb S. Presidential Address-1976. Social support as a moderator of life stress. Psychosom Med. 1976;38:300–314. doi: 10.1097/00006842-197609000-00003. [DOI] [PubMed] [Google Scholar]
- 83.Israel BA. Social networks and health status: Linking theory, research, and practice. Patient Counselling and Health Education. 1982;4:65–79. doi: 10.1016/s0190-2040(82)80002-5. [DOI] [PubMed] [Google Scholar]
- 84.Procidano ME, Heller K. Measures of perceived social support from friends and from family: three validation studies. Am J Community Psychol. 1983;11:1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- 85.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 86.Kang SH, Bloom JR. Social support and cancer screening among older black Americans. J Natl Cancer Inst. 1993;85:737–742. doi: 10.1093/jnci/85.9.737. [DOI] [PubMed] [Google Scholar]
- 87.Waxler-Morrison N, Hislop TG, Mears B, Kan L. Effects of social relationships on survival for women with breast cancer: a prospective study. Soc Sci Med. 1991;33:177–183. doi: 10.1016/0277-9536(91)90178-f. [DOI] [PubMed] [Google Scholar]
- 88.Lamping D&CK. Hemodialysis compliance: Assesment, prediciton, and intervention. Vol. 3. Semin Dial; 1990. pp. 52–56.pp. 105–111. Ref Type: Report. [Google Scholar]
- 89.Patel SS, Peterson RA, Kimmel PL. The impact of social support on end-stage renal disease. Semin Dial. 2005;18:98–102. doi: 10.1111/j.1525-139X.2005.18203.x. [DOI] [PubMed] [Google Scholar]
- 90.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996;119:488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- 91.DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23:207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 92.Marin G, Marin BV. Research with Hispanic Populations. Newbury Park: Sage Publications; 1991. [Google Scholar]
- 93.Sabogal F, Marín G, Otero-Sabogal R, Marín BV, Perez-Stable EJ. Hispanic Familism and Acculturation: What Changes and What Doesn't? Hispanic Journal of Behavioral Sciences. 1987;9:397–412. [Google Scholar]