Abstract
For several decades, lipid biologists have investigated how sphingolipids contribute to physiology, cell biology, and cell fate. Foremost among these discoveries is the finding that the bioactive sphingolipids ceramide, sphingosine, and sphingosine-1-phosphate (S1P) have diverse and often opposing effects on cell fate. Interestingly, these bioactive sphingolipids can be interconverted by just a few enzymatic reactions. Therefore, much attention has been paid to the enzymes which govern these reactions with a disproportionate amount of focus on the enzyme sphingosine kinase 1 (SK1). Several studies have found that tissue expression of SK1 correlates with cancer stage, chemotherapy response, and tumor aggressiveness. In addition, overexpression of SK1 in multiple cancer cell lines increases their resistance to chemotherapy, promotes proliferation, allows for anchorage independent growth, and increases local angiogenesis. Inhibition of SK1 using either pharmacological inhibitors or by crossing SK1 null mice has shown promise in many xenograft models of cancer as well as several genetic and chemically induced mouse models of carcinogenesis. Here we review the majority of the evidence that suggests SK1 is a promising target for the prevention and or treatment of various cancers. Also, we strongly advocate for further research into basic mechanisms of bioactive sphingolipid signaling and an increased focus on the efficacy of SK inhibitors in non-xenograft models of cancer progression.
Keywords: Sphingolipids, Sphingosine-1-phosphate, Ceramide, Chemoresistance, Angiogenesis Oncogene
Introduction
An emerging area of investigation in lipid research has been the role of sphingolipids in cancer biology. Many groups are actively investigating the role of different sphingolipid enzymes, sphingolipid binding proteins, and transmembrane transporters in cancer biology. Among the many contenders, the sphingosine kinase (SK) family has probably received the most attention as an important enzyme in cancer biology since their catalytic activity lies at a critical juncture in regulating bioactive sphingolipid metabolism.
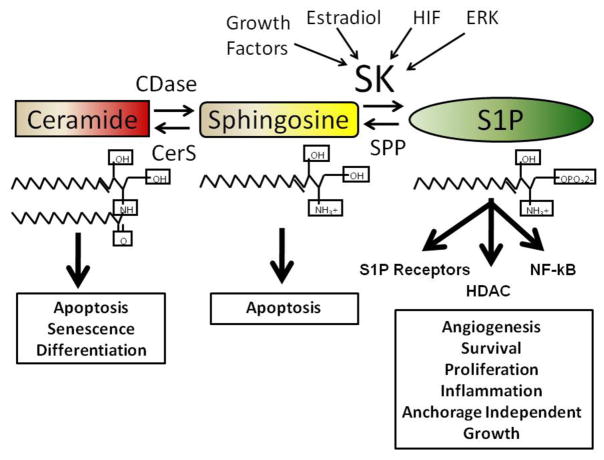
Some of the earliest studies of the biological role of SK brought to attention the idea that sphingosine-1-phosphate (S1P) can act as a mitogen both independently and as a second messenger in response to extracellular inducers. Prior to this discovery, and at present, a substantial amount of evidence that ceramide and sphingosine can act as promoters of apoptosis and senescence has been accumulating (Ahn and Schroeder, 2002), (Venable et al., 2006, Venable and Yin, 2009), (Sakakura et al., 1998). Because these bioactive lipids can be interconverted by only a few metabolic steps, it was hypothesized that the enzymes which regulate this interconversion may regulate apoptosis and proliferation (Spiegel et al., 1998). This model of sphingolipid biology—referred to as the “sphingolipid rheostat”—postulates that regulating relative sphingosine, ceramide, and S1P content consequently influences cellular fate.
The simplicity of the rheostat model, in combination with a significant amount of evidence supporting it in principle, has widespread appeal in the sphingolipid field. Still, the model requires refinement as cellular lipid changes are becoming more accurately measured. For example, this model may not be able to properly account for differences in the subcellular localization of bioactive sphingolipids where, due to their hydrophobicity, they tend to localize to specific membranes and membrane compartments (Hannun and Obeid, 2008, Hannun et al., 2001). In this sense, the rheostat model is likely overly simplistic; however, the model may be applicable within the context of specific membrane compartments. In addition, the diversity of ceramide species produced by at least six different ceramide synthases raises questions about the idea of grouping all ceramide species into a unified group when accounting for their bioactive properties (Levy and Futerman). Although some evidence exists to support this claim, it is currently less clear if these effects are due primarily to differences in affinities to downstream binding partners, differences in subcellular localization, or both (Senkal et al., 2007, White-Gilbertson et al., 2009, Mukhopadhay et. al. 2009). Even so, allure of the rheostat model has lead researchers to focus on the SKs, and to a lesser extent the ceramidases, as major regulators of bioactive sphingolipids.
In humans, and all animals whose genomes have been sequenced to date, there are two SK isoforms: SK1 and SK2. Although both SK isoforms catalyze the same biochemical reaction, these two isoforms differ in their substrate specificities, subcellular localization, and tissue distributions (Liu et al., 2003, Maceyka et al., 2005). Interestingly, several studies have shown that high levels of SK2 can have anti-proliferative effects (Maceyka et al., 2005, Liu et al., 2003). The precise mechanism by which this occurs is still unclear; however, it has been suggested that this effect may be due to SK2 coupling to sphingosine phosphate phosphatase 1 with recycling of sphingosine into ceramide or through distinct subcellular localization (Le Stunff et al., 2007, Strub et al., Hait et al., 2009). Therefore, SK1 and SK2 are not equivalent in their effects on biological activity despite their enzymatic similarities. Because most of the work on SK in cancer has focused on SK1, in this review, we describe the role of SK1 in cancer pathogenesis.
SK1 has been implicated in the regulation of many aspects of cancer progression including the enhancement of cancer cell proliferation or survival, the promotion of angiogenesis or lymphangiogenesis, the migration and invasion of cancer cells during metastasis, and determination of chemotherapy resistance or sensitivity (Shida et al., 2008). In addition, SK1 may play an indirect role in cancer progression by regulating the inflammatory process or altering the adaptive immune response (Snider et al.). That SK1 could be important for various cancer progression steps is appealing; it may be a suitable cancer treatment target. However, additional research may improve cancer progression animal models and better define specific roles for SK1 in different carcinogenic processes, a finding that would be informative for further development of SK1 as an effective oncogenic target. Here, we summarize much of the evidence implicating SK1 in cancer, describing various properties of cancer progression for which SK1 has been implicated, in either in vitro or in animal models. This review also underscores present progress and limitations in our understanding of sphingolipids in cancer biology.
Sphingosine-1-phosphate and Sphingosine Kinase as Regulators of Cell Proliferation and Survival
S1P was identified as an important second messenger in response to fetal calf serum and platelet derived growth factor (Olivera and Spiegel, 1993). On its own, S1P has mitogenic properties, but it can also act synergistically when added to PDGF (Olivera and Spiegel, 1993). When SK activity was inhibited pharmacologically, fetal calf serum and PDGF had reduced effects on the proliferation of NIH 3T3 cells (Edsall et al., 1998). Later it was determined that S1P acted on a G-protein coupled receptor which appeared functionally and perhaps even physically to couple to the PDGF receptor (Lee et al., 1998). Interestingly, PDGF may also regulate the transcription of the S1P1 receptor through the regulation of the kruppel-like factor (KLF) transcription factor (Carlson et al., 2006). The complete absence of KLF leads to embryonic lethality due to hemorrhage similar to that observed in the S1P1 receptor knockout mouse or in the PDGF receptor knockout mouse (Wu et al., 2008).
Overexpression of SK1 increases the proliferative rate of NIH 3T3 cells or HEK293 cells by accelerating the G1-to-S transition (Olivera et al., 1999, Xia et al., 2000), which occurs due to an enhancement of phospholipase D activity, activation of Raf kinase, enhanced AP-1 binding activity, enhanced phosphorylation of the Rb protein, and an increase in intracellular calcium (Olivera and Spiegel, 1993, Wu et al., 1995). SK1 overexpression in MCF-7 cells accelerates the growth of colonies in soft agar and promotes the proliferation of MCF-7 in 10% FBS (Sukocheva et al., 2003). The effects of SK1 overexpression on survival during serum withdrawal and proliferation maintenance in low-serum media depends on phosphorylation at serine 225 (Pitson et al., 2005). In addition, SK1 overexpression in NIH 3T3 cells induces colony formation in a serine 225-dependent manner (Pitson et al., 2005).
S1P prevents intranucleosomal fragmentation induced by ceramide by activating ERK and by inhibiting JNK. Overexpression of SK1 reduces apoptosis induced by serum deprivation, exogenous sphingosine, or C2-ceramide (Nava et al., 2002, Olivera et al., 1999). The mechanism by which this occurs is unclear, but appears to be upstream of executioner caspase activation.
Knockdown of SK1 using siRNA or treatment of glioma cells with an SK inhibitor decreases the growth rate of various glioma cell lines. This effect is independent of which SK isoform is predominantly expressed (Van Brocklyn et al., 2005). In addition, knockdown of SK1 increased the number of apoptotic cells in a small, but statistically significant, manner (Taha et al., 2006b). This slight induction of apoptosis is similar to what is observed in MCF-7 cells treated with SK1-specific siRNA (Taha et al., 2006b). In MCF-7, loss of SK1 was shown to initiate the intrinsic apoptotic pathway and induce Bax activation, suggesting that loss of SK1 triggers an apoptotic event upstream of mitochondrial permeabilization (Taha et al., 2006b). This effect could be partially reversed by prolonged treatment with myriocin which depletes sphingolipids, suggesting that the apoptosis observed is a sphingolipid-dependent event. This is significant because loss of SK1 not only leads to a loss of S1P, but also causes significant ceramide accumulation. It has been postulated that ceramide accumulation in response to either SK1 loss or SK1 inhibition through pharmacological means is the major pathway by which SK1 loss leads to apoptosis in cancer cells (Taha et al., 2006b, Pchejetski et al., 2005). Although loss of SK1 by RNAi is a non-physiological mechanism by which apoptosis would occur in cancer, there is evidence that SK1 is lost during cellular stress in response to DNA damaging agents, in response to TNF-α, or in response to the microtubule disrupting agent paclitaxel (Taha et al., 2004, Pchejetski et al., 2005, Taha et al., 2005). There is evidence that p53 mediates SK1 degradation and that this occurs through cathepsin B-mediated degradation of SK1 at His122, followed by Arg 199 (Taha et al., 2006a, Taha et al., 2004). Although the connection between p53 activation and SK1 degradation is unclear, linking DNA damage to sphingolipid metabolism and apoptosis regulation is attractive. In addition, loss of p53 may have important consequences for regulation of sphingolipid metabolism.
Evidence for Sphingosine Kinase 1 Overexpression in Cancer
In several studies, SK1 is reported to be over-expressed in diverse forms of human cancer (French et al., 2003, Johnson et al., 2005, Van Brocklyn et al., 2005, Li et al., 2009a. Liu et al, 2010) such as glioblastoma, uterine, colon, lung, small intestinal, salivary gland, breast, ovarian, renal, rectal, endometrial, and stomach cancer. More recently, high expression of SK1 was associated with resistance to daunorubicin in acute leukemias (Sobue et al., 2006, Knapp et al., 2010, Sobue et al., 2008). That such a variety of cancers share this overexpression suggests that SK1 expression is driven by a common signaling pathway which is disrupted in many forms of cancer. Two candidate pathways which are almost universally dysregulated in cancer are the MAP kinase pathway and the hypoxia/HIF pathway, which would account for the conserved nature of SK1 overexpression. Importantly these two signaling pathways have also been shown to regulate SK1 expression in vitro. The MAP kinase pathway can increase SK1 expression either through AP-2 or Elk-1 transcription factors, or hypoxia within the tumor microenvironment may activate HIF family members which are transcriptional activators of SK1 (Anelli et al., 2008), Schwalm et al., 2008, Cuvillier et. al 2007).
A remaining unaddressed question is whether a 2-fold increase in SK1 expression is significant to cancer biology. In other words, is a doubling of the amount of SK1 biologically relevant or simply an interesting curiosity? Prior to these studies it was shown that SK1 over-expression could imbue non-tumorigenic cell lines with tumorigenic properties. For example, high SK1 expression can protect cells against apoptosis induced by serum starvation, induce proliferation in the absence of serum, promote angiogenesis, and allow for tumor generation in mouse xenograft models (Olivera et al, 1999, Xia et al, 2000, Nava et al, 2002). Therefore, it appears that over-expression of SK1 could be significant to tumor biology because it contributes to cancerous properties. In contrast, the degree of SK1 overexpression reported in studies using cell lines is two or more orders of magnitude greater than that which is reported in human cancer tissues. Therefore, it is not yet evident if a two-fold increase in SK1 expression is comparable to a 200-fold increase in SK1 expression (Xia et. al, 2000, Pitson et. al, 2005). Despite this concern, we have a few biologically relevant stimuli, such as hypoxia which increases SK1 expression ~2-fold in tissue culture models, has a significant effect on sphingolipid metabolism (Anelli et al, 2008). These sphingolipid changes appear to be sufficient to produce biological effects as a result of S1P production (Anelli et al., 2008). Therefore, it is possible that small changes in SK1 activity or expression, as seen in human cancer tissues, have a significant effect on S1P generation to at least produce paracrine effects in cell culture. Because bioactive sphingolipids are assumed to be the ultimate effectors of the SK biological response, we hypothesize that a 2-fold change in SK1 expression is indeed significant for human cancer.
In at least six studies, a correlation between SK1 and cancer progression has been identified. In the first study, SK1 expression correlated with both glioblastoma grade and patient survival (Van Brocklyn et al., 2005). Glioblastomas are highly vascular tumors which are very dependent on the HIF transcription family for their progression. Because SK1 is an HIF-responsive gene, that such a relationship exists is not surprising (Anelli et al., 2008, Oliver et al., 2009, Kaur et al., 2005). Whether S1P plays an essential role in the angiogenic nature of these tumors will be important to establish (Van Brocklyn et al., 2005). More recently, Li et. al. found a similar relationship in astrocytomas with >40% of astrocytomas exhibiting high SK1 expression when compared to adjacent tissues. Similar to Brock et. al, these authors also found that high SK1 expression correlated with astrocytoma tumor grade (Li et. al 2008).
In a second study of SK1 expression and cancer severity, expression of sphingolipid related genes in 171 normal and breast cancer samples were analyzed, and SK1 expression was significantly higher in estrogen-receptor negative breast cancers compared to estrogen-receptor positive breast cancers (Ruckhaberle et al., 2008). Importantly, the authors tested this correlation in five independent publicly available datasets and reported that SK1 expression was significantly higher in all five datasets tested. This analysis validated their original conclusion as well as increased their sample size to 1,269 patients, thereby strengthening the power of the findings. Also, the authors found that higher SK1 expression also correlated with a worse prognosis even when one controlled for the estrogen receptor status of the cancers. Therefore, SK1 expression may have implications for breast cancer treatment regardless of the estrogen receptor status. In several studies, important connections between SKs and estrogen have been demonstrated: SKs are involved in growth, migration, and survival responses due to estrogen. Of particular importance is that SK1 overexpression induces resistance in breast cancer cells to tamoxifen’s growth inhibiting effects (Sukocheva et al., 2003, Sukocheva et al., 2009).
Providing additional evidence of SK1’s role in cancer, a link between SK1 expression and gastric cancer has been reported (Li et al., 2009b). SK1 expression was higher in tumor tissue relative to normal adjacent tissue and an increase in SK1 expression correlated with poorer overall survival (Li et al., 2009b). In a more recent study, endometrial cancer was shown to have higher SK1 activity compared with normal uterine tissue, further reinforcing the idea that SK1 activity is frequently increased in cancer tissues (Knapp et al., 2010). Surprisingly, endometrial cancers also have an increase in SPT activity with multiple sphingolipid species being increased in these tumors. Although tissue S1P is increased, ceramide is also increased in these tissues calling into question the universal nature of the sphingolipid rheostat model. Also plasma S1P is increased in patients with endometrial cancer, suggesting that the presence of endometrial cancer can increase the amount of plasma S1P either directly through tumor production or indirectly through the body’s response to cancer. However, whether these changes in sphingolipid metabolism contribute to the progression of endometrial cancer remains unclear.
Liu et. al investigated the correlation between SK1 expression and salivary gland carcinoma. The authors indeed found that SK1 expression was significantly increased in salivary gland carcinoma (Liu et. al 2010). Importantly, high SK1 expression correlated with higher clinical stage and a decrease in overall patient survival. Tumor tissues were found to have greater than 4 fold increase in SK1 expression when compared with non-cancerous adjacent tissue. The authors also found that SK1 expression was an independent predictor of overall prognosis providing further support to the idea that SK1 expression correlates with a more aggressive cancer phenotype.
Most recently Mavaud et. al analyzed prostate tissues from 30 patients who underwent laparoscopic prostatectomies for prostate cancer and compared prostate cancer tissue to histologically normal adjacent tissue (Mavaud et. al 2011). The authors found that the tumor tissue had approximately a 2-fold increase in SK1 activity when compared with adjacent normal tissue. SK1 activity correlated with PSA levels, tumor volume, positive surgical margins, and a higher Gleason score. Importantly, this study is one of the first to look at SK1 activity within tumor samples and how activity relates to tumor aggression rather than SK1 expression alone.
Sphingosine Kinase in Angiogenesis and Lymphangiogenesis
S1P was shown to have an angiogenic effect more than a decade ago (Lee et al., 1999). More recently, we discovered that the SK family is essential for vasculogenesis during embryonic development; a deficit of all four SK alleles ceases vascular maturation, promoting embryonic lethality due to hemorrhage (Mizugishi et al., 2005). Several S1P receptors are also essential for vascular development, suggesting that the production of extracellular S1P is a required function of SKs during development. Mice lacking S1P1, or both S1P2 and S1P3, fail to develop a mature vasculature (Liu et al., 2000, Kono et al., 2004). These studies suggest a complex interplay between the SK genes and the concerted actions of several S1P receptors on the development of the vascular tree. Some functions attributed to S1P during vascular development include recruitment and proliferation of endothelial cells, stabilization of endothelial junctions, promotion of adhesion molecule expression to allow for the adherence of vascular smooth muscles to the endothelium. The development of an endothelial specific S1P1 receptor knockout points to an essential requirement for the expression of the S1P1 receptor only in the endothelium during vasculogenesis; this model reproduces the vascular defects observed in the complete S1P1 receptor knockout mouse (Allende et al., 2003). Because processes and signaling molecules involved in embryonic vascular development are often mimicked by cancer cells, the S1P signaling pathway is thought to be a novel target for an anti-angiogenesis strategy to treat cancer patients. Here, some of the major findings in this regard are summarized.
Several cell models have reinforced the idea that tumor SK1 may be an important source of S1P that leads to enhanced angiogenesis. Overexpression of SK1 in MCF-7 cells transplanted into a nude mouse enhances tumor growth and leads to increased microvessel density around the tumors (Nava et al., 2002). This suggests that increased SK1 expression within a tumor can greatly enhance tumor angiogenesis. Many forms of cancer have increased SK1 expression, so this could be a plausible mechanism by which tumors recruit new blood vessels. More recent studies indicate that U87 glioma cells increase SK1 expression and S1P release in response to hypoxia, thereby providing a physiological mechanism by which SK1 expression can lead to an enhancement of S1P release and neo-vascularization (Anelli et al., 2008). In addition to the better-characterized protein ligands such as VEGF and FGF which regulate angiogenesis, the secretion of S1P into the tumor microenvironment may be an equally significant mechanism by which tumor hypoxia can regulate angiogenesis. In addition, we have recently found that S1P can act as a significant inducer of lymphangiogenesis; human lymphatic endothelial cells are highly responsive to exogenous S1P (Anelli et al., 2010). This increase in S1P release is associated with endothelial migration and aggregation into tubular structures. In a recent study, S1P was shown to play an important role in vascular stabilization, and it had a more potent effect on vascularization when added after VEGF (Tengood et al., 2010). Thus, targeting VEGF in cancer therapy has potential promise, and the addition of an S1P-targeting agent may have an additive effect in anti-angiogenic therapy.
Targeting S1P as a potential therapeutic could be accomplished through multiple mechanisms. Pharmacological targeting of the S1P1 receptor may have a similar effect as inhibiting S1P formation directly. Evidence that S1P receptors are essential for tumor angiogenesis can be found in several studies. The introduction of an S1P1-receptor-specific siRNA into a xenograft model of Lewis lung carcinoma greatly decreased the tumor blood vessel formation and tumor growth, suggesting that S1P signaling is critical for tumor angiogenesis (Chae et al., 2004). Another promising result supporting this strategy was the development of an S1P-specific antibody. The systemic administration of an S1P-specific monoclonal antibody resulted in decreased tumor angiogenesis and decreased tumor volume in xenografts of MDA-MB 231 breast carcinoma, A549 lung adenocarcinoma, SKOV-3 ovarian cancer, and B16-F3 melanoma. That a systemic antibody to S1P can decrease the growth of a local xenograft and reduce tumor angiogenesis is very promising, but this finding is also surprising because serum S1P is very high (Visentin et al., 2006). Also exciting is that this strategy can target xenografts of diverse cancer types, suggesting that this mechanism of angiogenesis is highly conserved, offering a wide therapeutic advantage for multiple tumor types. In a separate study, treatment of macular degeneration with a S1P specific antibody greatly inhibited the formation of blood vessels and improved visual acuity, suggesting that this antibody might have multiple clinical uses for aberrant angiogenesis (Caballero et al., 2009). Therefore, an S1P-specific antibody similar to the monoclonal antibodies currently used to target VEGF may be beneficial for cancer treatment.
Sphingosine Kinase in Chemoresistance
In some of the earliest studies on SK 1, a correlation was identified between SK1 expression and apoptosis resistance (Cuvillier et al., 1996). Because the general strategy of chemotherapy or radiation therapy is to induce cancer cell apoptosis, targeting SK in cancers is a reasonable strategy to pursue. Many separate lines of evidence have converged on the common conclusion that decreasing SK1 activity sensitizes cells to apoptotic-inducing agents and, in fact, SK1 expression often correlates with the sensitivity of a cell line to a chemotherapeutic agent (Cuvillier et al, Sauer et al, 2009, Song et al., 2011, Pchejetski et al, 2008). For example, overexpression of SK1 in HL-60 leukemia cell lines prevents apoptosis induced by doxorubicin or taxotere (Bonhoure et al., 2006). In addition, resistance to doxorubicin correlates with doxorubicin-induced SK1 loss and ceramide accumulation (Bonhoure et al., 2006). In prostate cancer, SK1 expression correlates with chemotherapeutic resistance (Pchejetski et al., 2005). PC3 and LNCaP cells have differential sensitivities to docetaxel and camptothecin with docetaxel being the far more effective agent for PC-3 cells and camptothecin being more effective for LNCaP cells. The efficacy of chemotherapeutics to induce apoptosis in these cell lines strongly correlates with their ability to alter the ceramide:S1P ratio. More ceramide and decreased S1P correlates with an enhanced apoptotic response. The authors developed these ideas in a xenograft model and replicated their original findings: effective docetaxel treatment greatly decreased tumor volume. SK1 knockdown caused sensitization to the chemotherapies whereas overexpression of SK1 enhanced chemotherapeutic resistance (Pchejetski et al., 2005).
Evidence for S1P’s importance in drug resistance can be found in the model organism D. discoideum in which S1P modulation alters cisplatin sensitivity. Deletion of one or both slime mold SKs increases cisplatin sensitivity, whereas overexpression of D. discoideum SgkA increases resistance (Min et al., 2005). Also, deletion of the S1P lyase gene increases cisplatin resistance whereas overexpression of the S1P lyase induces cisplatin sensitivity (Min et al., 2004). Altogether, modulation of enzymes that produce or degrade S1P profoundly affect the ability of cisplatin to kill this organism. Therefore, it is likely that S1P plays an evolutionarily conserved anti-apoptotic role in organisms as distantly related to mammals as slime molds.
Sphingosine Kinase 1 in Mouse Models of Cancer
Although many groups have investigated the role of the SK/S1P pathway in cell cultures and xenograft models, in only a few studies has the role of SK1 been investigated with respect to more representative models of human cancer progression. Cancer is often caused by inherited and acquired mutations in genes which lead to dysregulation of signaling in otherwise healthy tissue. Cancers therefore, arise within the context of a specific microenvironment which depends on the tissue of origin. Animal models in which cancers arise from normal tissue in response to genetic insults or a genetic predisposition for cancer are generally considered more relevant to clinical disease. Although transgenic mice and gene knockout mice have their own set of limitations in terms of closely resembling how the majority of human cancers could be targeted pharmacologically, we believe they are more representative than xenografts in terms of their predictive power for how a specific gene may be involved in cancer progression.
There have been relatively few studies which have focused on SK1 in a non-xenograft animal model, however, three studies in the past few years have shown some promise. Two of the non-xenograft models of cancer studied were performed in colon cancer models, and a third study was conducted in an oral squamous cell carcinoma model. In one of the colon cancer studies, azoxymethane was used to induce chemical carcinogenesis. In this study, wildtype, Sphk1 −/−, or Sphk2 −/− mice were given weekly intraperitoneal injections of azoxymethane for three weeks, and then were later analyzed for the presence of aberrant crypt foci (Kawamori et al., 2009). Aberrant crypts are the earliest histologically visible stages of colon adenocarcinoma. Mice that develop aberrant crypts through this model can later develop malignant adenocarcinoma which can be enhanced with the addition of intestinal inflammatory agents such as dextran sulfate sodium. Sphk1 −/−, but not Sphk2 −/− mice had reduced development of aberrant crypt foci in response to AOM when compared to wildtype mice. In addition, Sphk1 −/− mice treated with AOM followed by DSS had dramatically decreased intestinal expression of COX-2, and a marked decrease in progression to adenocarcinoma formation. This phenomenon was attributed to a reduction in inflammation, a decreased rate of proliferation, an enhancement of apoptosis in Sphk1 −/− mice colons. Interestingly, wildtype mice with adenocarcinomas had an elevated tissue and serum S1P which did not occur in Sphk1 −/− mice. SK1 expression increased as the grade of the tumors worsened, with metastases having the highest SK1 expression. Importantly, SK1 expression in human colon adenocarcinomas was also shown to be increased, similar to the mouse model.
The second animal model used to study the effects of SK1 on intestinal carcinogenesis was the APCmin mouse model which develops numerous small intestine polyps. The APC gene is commonly mutated in human colon cancers and is found as a heterozygous mutation in individuals with familial adenomatous polyposis. Loss of heterozygosity of APC leads to the formation of polyps and eventually colonic adenocarcinoma in humans. Therefore, the APCmin mouse serves as a model of FAP with the exception that polyposis occurs primarily in the small intestine in mice rather than in the colon such as occurs in humans. APCmin mice lacking SK1 had smaller intestinal polyps but no difference in polyp number. These effects were attributed to sphingosine accumulation in the adenomas because they had more intracellular sphingosine than their wildtype counterparts. Prolonged treatment of isolated rat intestinal epithelial cells with increased sphingosine induced apoptosis. In addition, SK1 −/− intestinal polyps had reduced expression of c-myc and cdk4, an effect that could be mimicked with exogenous sphingosine treatment. These sphingolipid dependent effects were receptor independent: mice lacking an S1P1 receptor allele, both S1P2 receptor alleles, or both S1P3 receptor alleles were not different with respect to polyp formation in this model (Kohno et al., 2006). In addition, human colon cancer tissue and adenomatous lesions from APCmin mice had decreased S1P lyase expression when compared to normal tissue (Oskouian et al., 2006). Because S1P lyase is primarily responsible for S1P degradation, loss of this enzyme would induce an increase in intracellular S1P. Together, these three studies suggest that intracellular S1P is important for colon cancer progression due to its effects on proliferation and apoptosis. In addition, in a separate study, colon cancers were shown to have reduced ceramide when compared to healthy tissues (Selzner et al., 2001).
More recently, the role SK1 plays in oral squamous cell carcinoma was investigated (Shirai et al.). The authors of this study exposed wildtype and Sphk1 −/− mice to the carcinogen 4-nitroquinolone-1-oxide, a known inducer of tongue cancer in mice. In wildtype mice, SK1 expression was found to be significantly increased in both dysplastic lesions and in squamous cell carcinomas when compared to adjacent normal tissue. Importantly, Sphk1 −/− mice exposed to the carcinogen had less of a chance of developing tongue tumors and those mice that did develop tumors had smaller lesions. These effects were attributed to an increased level of apoptosis and a decreased rate of proliferation in the Sphk1 −/− lesions. Altogether these data provide strong evidence that SK1 plays an important role in both the initiation and progression of squamous cell carcinoma in response to a chemical carcinogen.
Safingol: A Sphingosine Kinase Inhibitor in Phase I Clinical Trials
Safingol, also known as L-Threo-Dihydrosphingosine, is an unnatural isomer of dihydrosphingosine that was originally shown to act as an inhibitor of protein kinase C. Subsequent studies showed that safingol also could act as a competitive inhibitor of SK. Safingol was shown to enhance the cytotoxicity of cancer cells when co-administered with one of several chemotherapeutic agents (Kedderis et. al 1995). Due to safingol’s ability to inhibit multiple kinases, it will be more difficult to tease apart whether any biological effects observed are due to inhibition of SK or to inhibition of protein kinase C. As an anti-cancer agent, this non-specificity of safingol action could actually prove to be an advantage as several protein kinase C family members have been shown to play important roles in cancer promotion (Gonelli et al., 2009).
An early glimpse into the safety of SK inhibitors as anti-cancer agents can be had from the recently published Safingol Phase I clinical trial which enrolled 43 patients with advanced solid tumors and tested the safety of safingol (Dickson et. al 2011). The Safingol Trial was a non-blinded non-randomized dose escalation study in which the authors administered safingol at increasing doses just prior to giving a fixed dose of cisplatin. Therefore, the trial was evaluating the safety of giving safingol in the presence of cisplatin whereby patients were given a 1–2 hour infusion of safingol followed by a 1 hour infusion of cisplatin. Fortunately, the authors found that toxicity was fairly limited with a dose limiting toxicity of elevated liver transaminases which was reversible. In addition, the authors were able to show that three cohorts of patients receiving the top three highest tolerated doses also had a significant reduction in peripheral blood S1P suggesting that safingol was able to inhibit SK activity in patients at the doses given. The efficacy of safingol on tumor responsiveness was difficult to assess since the trial lacked a proper control group. Despite this the authors report that two patients, both with adrenal cortical carcinoma, had positive clinical responses to the safingol and cisplatin treatment. Unfortunately this study was not designed to separate the effects of cisplatin from those of safingol and therefore it is unclear if cisplatin alone could produce these effects. This is understandable since the study was designed to measure safety, future randomized control trials will have to be conducted in order to better evaluate efficacy.
Overall, safingol appears to be well tolerated and the authors have provided some evidence that it has a measurable effect on blood S1P levels. This study paves the way for Phase II clinical trials and provides some guidelines as to which doses should be used to further evaluate clinical responsiveness to this SK inhibitor. As an important aside, data gathered from future trials of safingol will allows us to correlate changes in blood and tumor sphingolipids with clinical responsiveness, thereby providing a practical test of the “sphingolipid rheostat” hypothesis in the context of human cancer therapy.
Conclusion
SK1 has been studied in the context of regulating proliferation for almost two decades. Since these early revelations, several new functions have been assigned to SK1 which may also relate to its involvement in carcinogenesis, such as its ability to regulate cell survival, promote angiogenesis, regulate lymphocyte trafficking, promote inflammation, and control cellular migration. Many of these functions overlap with important functions of classical oncogenes, so it is not surprising that SK1 is of great interest to cancer biologists. Although pharmacologic therapies targeted at SK1 were efficacious in cell culture and in a few animal models, stronger evidence (in the form of clinical trials) is needed to validate SK1 as a legitimate target in human cancer. A role for sphingolipids in cancer progression may first be tested with the S1P receptor antagonist, FTY720, which has already been approved for usage in the US by the FDA for the treatment of multiple sclerosis In addition, the Safingol clinical trials will likely be the first major tests of a competitive SK inhibitor as an anti-cancer agent in humans. It will be exciting to follow the development of this small molecule inhibitor as it moves through early clinical trials since it appears to be well tolerated and has measurable effects on sphingolipid metabolism.
Importantly, there have only been a few studies utilizing genetic animal cancer models which more closely resemble what we believe are the natural mutational events which give rise to the various stages of cancer progression in humans. In addition, more clarity is required on the exact cancer promoting or inhibiting signaling pathways sphingolipids impinge upon to govern their effects on cellular proliferation and survival. In recent years two potential intracellular targets of S1P, TRAF2 and HDAC, have been identified which may improve our understanding of how bioactive sphingolipids regulate known or unknown signaling pathways to regulate cell survival and growth. Identifying the molecular substrates by which sphingolipids exert their effects is a grand challenge for our field and will likely open up the sphingolipid field to the larger cancer research community. In the meantime, we can continue to make small gains in our understanding of how this important enzyme regulates sphingolipid metabolism in cancerous and normal tissues. There is still much to learn about the mechanisms of cancer formation and the role of sphingolipids in human physiology in general.
Figure 1. The Sphingolipid Rheostat.
Sphingosine Kinase (SK) lies at an important juncture in the metabolic interconversion of the pro-apoptotic sphingolipids ceramide and sphingosine and the proliferative molecule sphingosine-1-phosphate (S1P). Ceramide has been shown to induce apoptosis, senescence, or differentiation in many different experimental systems. Sphingosine also has been shown to exhibit pro-apoptotic properties in multiple experimental systems. S1P, on the other hand, contributes many biological activities that altogether may promote the growth of cancer cells. Ceramidases (CDases), Sphingosine-1-phosphate phosphatases/Lipid phosphate phosphatases (SPP), and Ceramide synthases (CerS) also are important enzymes that regulate the interconversion of bioactive sphingolipids although less is currently known about their contribution to cancer progression. Several upstream activators of SK1 have been shown to contribute to carcinogenesis in cell culture models. These include estradiol, growth factors, phosphorylation by ERK, and increased transcription by hypoxia inducible factor (HIF). The precise mechanism by which SK1 activation/overexpression contributes to carcinogenesis is not clear, but may include S1P receptor activation, stabilization of NF-kB, or through direct interaction of S1P with an intracellular target such as HDAC or TRAF2 (not shown). A color version of the figure is available online.
TABLE 1.
SPHK1 −/− MOUSE MODELS OF CARCINOGENESIS
| Animal Models | Findings | Proposed Mechanism | Reference |
|---|---|---|---|
| APCmin Sphk1 −/− |
Decreased intestinal polyp size, but not number | Increased intracellular sphingosine. Reduced c-myc and CDK4 | (Kohno et al., 2006) |
| AOM-DSS Sphk1 −/− | Decreased aberrant crypt foci | Decreased COX-2 Expression. Increased proliferation. Decreased apoptosis. | (Kawamori et al., 2009) |
| 4-NQO Sphk1 −/− |
Decreased risk of oral SCC with 4-NQO ingestion. Decreased size of lingual tumors when present. | Increased proliferation. Decreased caspase activation. | (Shirai et al.) |
TABLE 2.
XENOGRAFT MODELS OF SK1 IN CARCINOGENESIS
| Xenograft Models | Findings | Proposed Mechanism | Reference |
|---|---|---|---|
| Gastric Cancer | Antisense Sphk1 oligonucleotides decreased xenograft growth by 50% | Increased apoptosis in xenograft | (Fuereder et al.) |
| A-498 kidney carcinoma | Sorafenib acts synergistically with two SK1/SK2 inhibitors to decrease tumor growth | Increased caspase 3/7 activation. Decreased ERK activation. Decreased angiogenesis. | (Beljanski et al.) |
| Bxpc-3 Pancreatic Adenocarcinoma | Sorafenib acts synergistically with two SK1/SK2 inhibitors to decrease tumor growth | Increased caspase 3/7 activation. Decreased ERK activation. Decreased angiogenesis. | (Beljanski et al.) |
| PC-3 - Prostate Cancer | SK inhibitor (B-5354c) and Irinotecan independently and synergistically decrease tumor growth and distant metastases | Decreased survival of tumor cells | (Pchejetski et al., 2008) |
| MCF-7 Breast Cancer | Overexpression of SK1 increases tumor growth | Increased microvessel density | 28 |
| U937-AML cells | SK inhibitor (BML-258) decreased tumor growth. | Increased TUNEL positive cells. Decreased mitotic figures. | (Paugh et al., 2008) |
| NIH 3T3 | Overexpression of SK1 allows for tumor growth in NOD/SCID mice | Allows for anchorage independent growth | 24 |
| MDA MB-231 Breast cancer | A S1P specific antibody decreases xenograft growth | Decreased IL-6, IL-8, and VEGF release from tumors. Increased Caspase-3 activation. | 57 |
| SKOV-3 Ovarian Cancer | A S1P specific antibody decreases xenograft growth | Decreased IL-6, IL-8, and VEGF release from tumors. Increased Caspase-3 activation. | 57 |
| A549 Lung Adenocarcinoma | A S1P specific antibody decreases xenograft growth | Decreased IL-6, IL-8, and VEGF release from tumors. Increased Caspase-3 activation. | 57 |
| JC Breast Cancer | SK specific inhibitor decreases tumor volume | Increased apoptosis. | (French et al., 2003) |
Acknowledgments
The Authors wish to thank Dr. Jennifer Schnellmann for reviewing this paper.
Footnotes
Declaration of Interest
This work was supported in part by: NIH grants R01AG16583, GM062887, and P01 CA097132 (LMO); NIH NRSA 5F3-HL093991 (CRG). VA MERIT Award BX000156-01A1 (LMO).
References
- Ahn Eh, Schroeder JJ. Sphingoid bases and ceramide induce apoptosis in HT-29 and HCT-116 human colon cancer cells. Exp Biol Med (Maywood) 2002;227:345–53. doi: 10.1177/153537020222700507. [DOI] [PubMed] [Google Scholar]
- Allende ML, Yamashita T, Proia RL. G-protein-coupled receptor S1P1 acts within endothelial cells to regulate vascular maturation. Blood. 2003;102:3665–7. doi: 10.1182/blood-2003-02-0460. [DOI] [PubMed] [Google Scholar]
- Anelli V, Gault CR, Cheng AB, Obeid LM. Sphingosine kinase 1 is up-regulated during hypoxia in U87MG glioma cells. Role of hypoxia-inducible factors 1 and 2. J Biol Chem. 2008;283:3365–75. doi: 10.1074/jbc.M708241200. [DOI] [PubMed] [Google Scholar]
- Anelli V, Gault CR, Snider AJ, Obeid LM. Role of sphingosine kinase-1 in paracrine/transcellular angiogenesis and lymphangiogenesis in vitro. Faseb J. 24:2727–38. doi: 10.1096/fj.09-150540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beljanski V, Knaak C, Zhuang Y, Smith CD. Combined anticancer effects of sphingosine kinase inhibitors and sorafenib. Invest New Drugs. doi: 10.1007/s10637-010-9452-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonhoure E, Pchejetski D, Aouali N, Morjani H, Levade T, Kohama T, Cuvillier O. Overcoming MDR-associated chemoresistance in HL-60 acute myeloid leukemia cells by targeting sphingosine kinase-1. Leukemia. 2006;20:95–102. doi: 10.1038/sj.leu.2404023. [DOI] [PubMed] [Google Scholar]
- Caballero S, Swaney J, Moreno K, Afzal A, Kielczewski J, Stoller G, Cavalli A, Garland W, Hansen G, Sabbadini R, Grant MB. Anti-sphingosine-1-phosphate monoclonal antibodies inhibit angiogenesis and sub-retinal fibrosis in a murine model of laser-induced choroidal neovascularization. Exp Eye Res. 2009;88:367–77. doi: 10.1016/j.exer.2008.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson Cm, Endrizzi Bt, Wu J, Ding X, Weinreich MA, Walsh ER, Wani MA, Lingrel JB, Hogquist KA, Jameson SC. Kruppel-like factor 2 regulates thymocyte and T-cell migration. Nature. 2006;442:299–302. doi: 10.1038/nature04882. [DOI] [PubMed] [Google Scholar]
- Chae SS, Paik JH, Furneaux H, Hla T. Requirement for sphingosine 1-phosphate receptor-1 in tumor angiogenesis demonstrated by in vivo RNA interference. J Clin Invest. 2004;114:1082–9. doi: 10.1172/JCI22716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuvillier O. Sphingosine kinase-1--a potential therapeutic target in cancer. Anticancer Drugs. 2007;18:105–10. doi: 10.1097/CAD.0b013e328011334d. [DOI] [PubMed] [Google Scholar]
- Cuvillier O, Pirianov G, Kleuser B, Vanek PG, Coso OA, Gutkind S, Spiegel S. Suppression of ceramide-mediated programmed cell death by sphingosine-1-phosphate. Nature. 1996;381:800–3. doi: 10.1038/381800a0. [DOI] [PubMed] [Google Scholar]
- Dickson MA, Carvajal RD, Merrill AH, Jr, Gonen M, Cane LM, Schwartz GK. A phase I clinical trial of safingol in combination with cisplatin in advanced solid tumors. Clin Cancer Res. 2011;17(8):2484–2492. doi: 10.1158/1078-0432.CCR-10-2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edsall LC, Van Brocklyn, JR, Cuvillier O, Kleuser B, Spiegel S. N,N-Dimethylsphingosine is a potent competitive inhibitor of sphingosine kinase but not of protein kinase C: modulation of cellular levels of sphingosine 1-phosphate and ceramide. Biochemistry. 1998;37:12892–8. doi: 10.1021/bi980744d. [DOI] [PubMed] [Google Scholar]
- French KJ, Schrecengost RS, Lee BD, Zhuang Y, Smith SN, Eberly JL, Yun JK, Smith CD. Discovery and evaluation of inhibitors of human sphingosine kinase. Cancer Res. 2003;63:5962–9. [PubMed] [Google Scholar]
- Fuereder T, Hoeflmayer D, Jaeger-Lansky A, Rasin-Streden D, Strommer S, Fisker N, Hansen BJ, Crevenna R, Wacheck V. Sphingosine kinase 1 is a relevant molecular target in gastric cancer. Anticancer Drugs. 22:245–52. doi: 10.1097/cad.0b013e328340bd95. [DOI] [PubMed] [Google Scholar]
- Gonelli A, Mischiati C, Guerrini R, Voltan R, Salvadori S, Zauli G. Perspectives of protein kinase C (PKC) inhibitors as anti-cancer agents. Mini Rev Med Chem. 2009;9(4):498–509. doi: 10.2174/138955709787847967. [DOI] [PubMed] [Google Scholar]
- Hait NC, Allegood J, Maceyka M, Strub GM, Harikumar KB, Singh SK, Luo C, Marmorstein R, Kordula T, Milstien S, Spiegel S. Regulation of histone acetylation in the nucleus by sphingosine-1-phosphate. Science. 2009;325:1254–7. doi: 10.1126/science.1176709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannun YA, Luberto C, Argraves KM. Enzymes of sphingolipid metabolism: from modular to integrative signaling. Biochemistry. 2001;40:4893–903. doi: 10.1021/bi002836k. [DOI] [PubMed] [Google Scholar]
- Hannun YA, Obeid LM. Principles of bioactive lipid signalling: lessons from sphingolipids. Nat Rev Mol Cell Biol. 2008;9:139–50. doi: 10.1038/nrm2329. [DOI] [PubMed] [Google Scholar]
- Johnson KR, Johnson KY, Crellin HG, Ogretmen B, Boylan AM, Harley RA, Obeid LM. Immunohistochemical distribution of sphingosine kinase 1 in normal and tumor lung tissue. J Histochem Cytochem. 2005;53:1159–66. doi: 10.1369/jhc.4A6606.2005. [DOI] [PubMed] [Google Scholar]
- Kaur B, Khwaja FW, Severson EA, Matheny SL, Brat DJ, Van Meir EG. Hypoxia and the hypoxia-inducible-factor pathway in glioma growth and angiogenesis. Neuro Oncol. 2005;7:134–53. doi: 10.1215/S1152851704001115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawamori T, Kaneshiro T, Okumura M, Maalouf S, Uflacker A, Bielawski J, Hannun YA, Obeid LM. Role for sphingosine kinase 1 in colon carcinogenesis. Faseb J. 2009;23:405–14. doi: 10.1096/fj.08-117572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kedderis LB, Bozigian HP, Kleeman JM, Hall RL, Palmer TE, Harrison SD, Jr, Susick RL., Jr Toxicity of the protein kinase C inhibitor safingol administered alone and in combination with chemotherapeutic agents. Fundam Appl Toxicol. 1995;25(2):201–217. doi: 10.1006/faat.1995.1056. [DOI] [PubMed] [Google Scholar]
- Knapp P, Baranowski M, Knapp M, Zabielski P, Blachnio-Zabielska AU, Gorski J. Altered sphingolipid metabolism in human endometrial cancer. Prostaglandins Other Lipid Mediat. 2010;92:62–6. doi: 10.1016/j.prostaglandins.2010.03.002. [DOI] [PubMed] [Google Scholar]
- Kohno M, Momoi M, OOMl, Paik JH, Lee YM, Venkataraman K, AIY, Ristimaki AP, Fyrst H, Sano H, Rosenberg D, Saba JD, Proia RL, Hla T. Intracellular role for sphingosine kinase 1 in intestinal adenoma cell proliferation. Mol Cell Biol. 2006;26:7211–23. doi: 10.1128/MCB.02341-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kono M, Mi Y, Liu Y, Sasaki T, Allende ML, Wu YP, Yamashita T, Proia RL. The sphingosine-1-phosphate receptors S1P1, S1P2, and S1P3 function coordinately during embryonic angiogenesis. J Biol Chem. 2004;279:29367–73. doi: 10.1074/jbc.M403937200. [DOI] [PubMed] [Google Scholar]
- Le Stunff H, Giussani P, Maceyka M, Lepine S, Milstien S, Spiegel S. Recycling of sphingosine is regulated by the concerted actions of sphingosine-1-phosphate phosphohydrolase 1 and sphingosine kinase 2. J Biol Chem. 2007;282:34372–80. doi: 10.1074/jbc.M703329200. [DOI] [PubMed] [Google Scholar]
- Lee MJ, Van Brocklyn, JR, Thangada S, Liu Ch, Hand AR, Menzeleev R, Spiegel S, Hla T. Sphingosine-1-phosphate as a ligand for the G protein-coupled receptor EDG-1. Science. 1998;279:1552–5. doi: 10.1126/science.279.5356.1552. [DOI] [PubMed] [Google Scholar]
- Lee OH, Kim YM, Lee YM, Moon EJ, Lee DJ, Kim JH, Kim KW, Kwon YG. Sphingosine 1-phosphate induces angiogenesis: its angiogenic action and signaling mechanism in human umbilical vein endothelial cells. Biochem Biophys Res Commun. 1999;264:743–50. doi: 10.1006/bbrc.1999.1586. [DOI] [PubMed] [Google Scholar]
- Levy M, Futerman AH. Mammalian ceramide synthases. IUBMB Life. 2010;62:347–56. doi: 10.1002/iub.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Guan HY, Gong LY, Song LB, Zhang N, Wu J, Yuan J, Zheng YJ, Huang ZS, Li M. Clinical significance of sphingosine kinase-1 expression in human astrocytomas progression and overall patient survival. Clin Cancer Res. 2008;14(21):6996–7003. doi: 10.1158/1078-0432.CCR-08-0754. [DOI] [PubMed] [Google Scholar]
- Li Mh, Sanchez T, Yamase H, Hla T, OOMl, Pappalardo A, Lynch Kr, Lin CY, Ferrer F. S1P/S1P1 signaling stimulates cell migration and invasion in Wilms tumor. Cancer Lett. 2009a;276:171–9. doi: 10.1016/j.canlet.2008.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Yu Cp, Xia JT, Zhang L, Weng GX, Zheng HQ, Kong QL, Hu LJ, Zeng MS, Zeng YX, Li M, Li J, Song LB. Sphingosine kinase 1 is associated with gastric cancer progression and poor survival of patients. Clin Cancer Res. 2009b;15:1393–9. doi: 10.1158/1078-0432.CCR-08-1158. [DOI] [PubMed] [Google Scholar]
- Liu H, Toman Re, Goparaju Sk, Maceyka M, Nava Ve, Sankala H, Payne Sg, Bektas M, Ishii I, Chun J, Milstien S, Spiegel S. Sphingosine kinase type 2 is a putative BH3-only protein that induces apoptosis. J Biol Chem. 2003;278:40330–6. doi: 10.1074/jbc.M304455200. [DOI] [PubMed] [Google Scholar]
- Liu Y, Wada R, Yamashita T, Mi Y, Deng Cx, Hobson Jp, Rosenfeldt Hm, Nava Ve, Chae Ss, Lee Mj, Liu Ch, Hla T, Spiegel S, Proia Rl. Edg-1, the G protein-coupled receptor for sphingosine-1-phosphate, is essential for vascular maturation. J Clin Invest. 2000;106:951–61. doi: 10.1172/JCI10905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu G, Zheng H, Zhang Z, Wu Z, Xiong H, Li J, Song L. Overexpression of sphingosine kinase 1 is associated with salivary gland carcinoma progression and might be a novel predictive marker for adjuvant therapy. BMC Cancer. 2010;10:495. doi: 10.1186/1471-2407-10-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maceyka M, Sankala H, Hait Nc, Le Stunff H, Liu H, Toman R, Collier C, Zhang M, Satin Ls, Merrill Ah, Jr, Milstien S, Spiegel S. SphK1 and SphK2, sphingosine kinase isoenzymes with opposing functions in sphingolipid metabolism. J Biol Chem. 2005;280:37118–29. doi: 10.1074/jbc.M502207200. [DOI] [PubMed] [Google Scholar]
- Malavaud B, Pchejetski D, Mazerolles C, de Paiva GR, Calvet C, Doumerc N, Pitson S, Rischmann P, Cuvillier O. Sphingosine kinase-1 activity and expression in human prostate cancer resection specimens. Eur J Cancer. 2010;46(18):3417–3424. doi: 10.1016/j.ejca.2010.07.053. [DOI] [PubMed] [Google Scholar]
- Min J, Stegner Al, Alexander H, Alexander S. Overexpression of sphingosine-1-phosphate lyase or inhibition of sphingosine kinase in Dictyostelium discoideum results in a selective increase in sensitivity to platinum-based chemotherapy drugs. Eukaryot Cell. 2004;3:795–805. doi: 10.1128/EC.3.3.795-805.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min J, Traynor D, Stegner Al, Zhang L, Hanigan Mh, Alexander H, Alexander S. Sphingosine kinase regulates the sensitivity of Dictyostelium discoideum cells to the anticancer drug cisplatin. Eukaryot Cell. 2005;4:178–89. doi: 10.1128/EC.4.1.178-189.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizugishi K, Yamashita T, Olivera A, Miller Gf, Spiegel S, Proia Rl. Essential role for sphingosine kinases in neural and vascular development. Mol Cell Biol. 2005;25:11113–21. doi: 10.1128/MCB.25.24.11113-11121.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukhopadhyay A, Saddoughi SA, Song P, Sultan I, Ponnusamy S, Senkal CE, Snook CF, Arnold HK, Sears RC, Hannun YA, Ogretmen B. Direct interaction between the inhibitor 2 and ceramide via sphingolipid-protein binding is involved in the regulation of protein phosphatase 2A activity and signaling. Faseb J. 2009;23(3):751–763. doi: 10.1096/fj.08-120550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nava VE, Hobson Jp, Murthy S, Milstien S, Spiegel S. Sphingosine kinase type 1 promotes estrogen-dependent tumorigenesis of breast cancer MCF-7 cells. Exp Cell Res. 2002;281:115–27. doi: 10.1006/excr.2002.5658. [DOI] [PubMed] [Google Scholar]
- Oliver L, Olivier C, Marhuenda FB, Campone M, Vallette FM. Hypoxia and the malignant glioma microenvironment: regulation and implications for therapy. Curr Mol Pharmacol. 2009;2:263–84. doi: 10.2174/1874467210902030263. [DOI] [PubMed] [Google Scholar]
- Olivera A, Kohama T, Edsall L, Nava V, Cuvillier O, Poulton S, Spiegel S. Sphingosine kinase expression increases intracellular sphingosine-1-phosphate and promotes cell growth and survival. J Cell Biol. 1999;147:545–58. doi: 10.1083/jcb.147.3.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivera A, Spiegel S. Sphingosine-1-phosphate as second messenger in cell proliferation induced by PDGF and FCS mitogens. Nature. 1993;365:557–60. doi: 10.1038/365557a0. [DOI] [PubMed] [Google Scholar]
- Oskouian B, Sooriyakumaran P, Borowsky Ad, Crans A, Dillard-Telm L, Tam YY, Bandhuvula P, Saba JD. Sphingosine-1-phosphate lyase potentiates apoptosis via p53- and p38-dependent pathways and is down-regulated in colon cancer. Proc Natl Acad Sci U S A. 2006;103:17384–9. doi: 10.1073/pnas.0600050103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paugh SW, Paugh BS, Rahmani M, Kapitonov D, Almenara JA, Kordula T, Milstien S, Adams JK, Zipkin RE, Grant S, Spiegel S. A selective sphingosine kinase 1 inhibitor integrates multiple molecular therapeutic targets in human leukemia. Blood. 2008;112:1382–91. doi: 10.1182/blood-2008-02-138958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pchejetski D, Doumerc N, Golzio M, Naymark M, Teissie J, Kohama T, Waxman J, Malavaud B, Cuvillier O. Chemosensitizing effects of sphingosine kinase-1 inhibition in prostate cancer cell and animal models. Mol Cancer Ther. 2008;7:1836–45. doi: 10.1158/1535-7163.MCT-07-2322. [DOI] [PubMed] [Google Scholar]
- Pchejetski D, Golzio M, Bonhoure E, Calvet C, Doumerc N, Garcia V, Mazerolles C, Rischmann P, Teissie J, Malavaud B, Cuvillier O. Sphingosine kinase-1 as a chemotherapy sensor in prostate adenocarcinoma cell and mouse models. Cancer Res. 2005;65:11667–75. doi: 10.1158/0008-5472.CAN-05-2702. [DOI] [PubMed] [Google Scholar]
- Pitson Sm, Xia P, Leclercq Tm, Moretti Pa, Zebol, Lynn He, Wattenberg Bw, Vadas Ma. Phosphorylation-dependent translocation of sphingosine kinase to the plasma membrane drives its oncogenic signalling. J Exp Med. 2005;201:49–54. doi: 10.1084/jem.20040559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruckhaberle E, Rody A, Engels K, Gaetje R, Von Minckwitz G, Schiffmann S, Grosch S, Geisslinger G, Holtrich U, Karn T, Kaufmann M. Microarray analysis of altered sphingolipid metabolism reveals prognostic significance of sphingosine kinase 1 in breast cancer. Breast Cancer Res Treat. 2008;112:41–52. doi: 10.1007/s10549-007-9836-9. [DOI] [PubMed] [Google Scholar]
- Sakakura C, Sweeney Ea, Shirahama T, Hagiwara A, Yamaguchi T, Takahashi T, Hakomori S, Igarashi Y. Selectivity of sphingosine-induced apoptosis. Lack of activity of DL-erythyro-dihydrosphingosine. Biochem Biophys Res Commun. 1998;246:827–30. doi: 10.1006/bbrc.1998.8719. [DOI] [PubMed] [Google Scholar]
- Sauer L, Nunes J, Salunkhe V, Skalska L, Kohama T, Cuvillier O, Waxman J, Pchejetski D. Sphingosine kinase 1 inhibition sensitizes hormone-resistant prostate cancer to docetaxel. Int J Cancer. 2009;125(11):2728–2736. doi: 10.1002/ijc.24640. [DOI] [PubMed] [Google Scholar]
- Schwalm S, Doll F, Romer I, Bubnova S, Pfeilschifter J, Huwiler A. Sphingosine kinase-1 is a hypoxia-regulated gene that stimulates migration of human endothelial cells. Biochem Biophys Res Commun. 2008;368:1020–5. doi: 10.1016/j.bbrc.2008.01.132. [DOI] [PubMed] [Google Scholar]
- Selzner M, Bielawska A, Morse Ma, Rudiger Ha, Sindram D, Hannun Ya, Clavien Pa. Induction of apoptotic cell death and prevention of tumor growth by ceramide analogues in metastatic human colon cancer. Cancer Res. 2001;61:1233–40. [PubMed] [Google Scholar]
- Senkal Ce, Ponnusamy S, Rossi Mj, Bialewski J, Sinha D, Jiang Jc, Jazwinski Sm, Hannun Ya, Ogretmen B. Role of human longevity assurance gene 1 and C18-ceramide in chemotherapy-induced cell death in human head and neck squamous cell carcinomas. Mol Cancer Ther. 2007;6:712–22. doi: 10.1158/1535-7163.MCT-06-0558. [DOI] [PubMed] [Google Scholar]
- Shida D, Takabe K, Kapitonov D, Milstien S, Spiegel S. Targeting SphK1 as a new strategy against cancer. Curr Drug Targets. 2008;9:662–73. doi: 10.2174/138945008785132402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirai K, Kaneshiro T, Wada M, Furuya H, Bielawski J, Hannun Ya, Obeid Lm, Ogretmen B, Kawamori T. A role of sphingosine kinase 1 in head and neck carcinogenesis. Cancer Prev Res (Phila) 2011;4:454–62. doi: 10.1158/1940-6207.CAPR-10-0299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha UK, Schorn VJ, Hochstim C, Chinn SB, Zhu S, Masood R. Increased radiation sensitivity of head and neck squamous cell carcinoma with sphingosine kinase 1 inhibition. Head Neck. 2011;33(2):178–188. doi: 10.1002/hed.21418. [DOI] [PubMed] [Google Scholar]
- Snider Aj, Orr Gandy Ka, Obeid LM. Sphingosine kinase: Role in regulation of bioactive sphingolipid mediators in inflammation. Biochimie. 2010;92:707–15. doi: 10.1016/j.biochi.2010.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobue S, Iwasaki T, Sugisaki C, Nagata K, Kikuchi R, Murakami M, Takagi A, Kojima T, Banno Y, Akao Y, Nozawa Y, Kannagi R, Suzuki M, Abe A, Naoe T, Murate T. Quantitative RT-PCR analysis of sphingolipid metabolic enzymes in acute leukemia and myelodysplastic syndromes. Leukemia. 2006;20:2042–6. doi: 10.1038/sj.leu.2404386. [DOI] [PubMed] [Google Scholar]
- Sobue S, Murakami M, Banno Y, Ito H, Kimura A, Gao S, Furuhata A, Takagi A, Kojima T, Suzuki M, Nozawa Y, Murate T. v-Src oncogene product increases sphingosine kinase 1 expression through mRNA stabilization: alteration of AU-rich element-binding proteins. Oncogene. 2008;27:6023–33. doi: 10.1038/onc.2008.198. [DOI] [PubMed] [Google Scholar]
- Song L, Xiong H, Li J, Liao W, Wang L, Wu J, Li M. Sphingosine kinase-1 enhances resistance to apoptosis through activation of PI3K/Akt/NF-kappaB pathway in human non-small cell lung cancer. Clin Cancer Res. 2011;17(7):1839–1849. doi: 10.1158/1078-0432.CCR-10-0720. [DOI] [PubMed] [Google Scholar]
- Spiegel S, Cuvillier O, Edsall LC, Kohama T, Menzeleev R, Olah Z, Olivera A, Pirianov G, Thomas DM, Tu Z, Van Brocklyn Jr, Wang F. Sphingosine-1-phosphate in cell growth and cell death. Ann N Y Acad Sci. 1998;845:11–8. doi: 10.1111/j.1749-6632.1998.tb09658.x. [DOI] [PubMed] [Google Scholar]
- Strub GM, Paillard M, Liang J, Gomez L, Allegood JC, Hait NC, Maceyka M, Price MM, Chen Q, Simpson DC, Kordula T, Milstien S, Lesnefsky EJ, Spiegel S. Sphingosine-1-phosphate produced by sphingosine kinase 2 in mitochondria interacts with prohibitin 2 to regulate complex IV assembly and respiration. Faseb J. 25:600–12. doi: 10.1096/fj.10-167502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sukocheva O, Wang L, Verrier E, Vadas MA, Xia P. Restoring endocrine response in breast cancer cells by inhibition of the sphingosine kinase-1 signaling pathway. Endocrinology. 2009;150:4484–92. doi: 10.1210/en.2009-0391. [DOI] [PubMed] [Google Scholar]
- Sukocheva OA, Wang L, Albanese N, Pitson SM, Vadas MA, Xia P. Sphingosine kinase transmits estrogen signaling in human breast cancer cells. Mol Endocrinol. 2003;17:2002–12. doi: 10.1210/me.2003-0119. [DOI] [PubMed] [Google Scholar]
- Taha TA, El-Alwani M, Hannun YA, Obeid LM. Sphingosine kinase-1 is cleaved by cathepsin B in vitro: identification of the initial cleavage sites for the protease. FEBS Lett. 2006a;580:6047–54. doi: 10.1016/j.febslet.2006.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taha TA, Kitatani K, Bielawski J, Cho W, Hannun YA, Obeid LM. Tumor necrosis factor induces the loss of sphingosine kinase-1 by a cathepsin B-dependent mechanism. J Biol Chem. 2005;280:17196–202. doi: 10.1074/jbc.M413744200. [DOI] [PubMed] [Google Scholar]
- Taha TA, Kitatani K, El-Alwani M, Bielawski J, Hannun YA, Obeid LM. Loss of sphingosine kinase-1 activates the intrinsic pathway of programmed cell death: modulation of sphingolipid levels and the induction of apoptosis. Faseb J. 2006b;20:482–4. doi: 10.1096/fj.05-4412fje. [DOI] [PubMed] [Google Scholar]
- Taha TA, Osta W, Kozhaya L, Bielawski J, Johnson KR, Gillanders We, Dbaibo Gs, Hannun YA, Obeid LM. Down-regulation of sphingosine kinase-1 by DNA damage: dependence on proteases and p53. J Biol Chem. 2004;279:20546–54. doi: 10.1074/jbc.M401259200. [DOI] [PubMed] [Google Scholar]
- Tengood JE, Kovach KM, Vescovi PE, Russell AJ, Little SR. Sequential delivery of vascular endothelial growth factor and sphingosine 1-phosphate for angiogenesis. Biomaterials. 2010 doi: 10.1016/j.biomaterials.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Brocklyn, JR, Jackson CA, Pearl DK, Kotur MS, Snyder PJ, Prior TW. Sphingosine kinase-1 expression correlates with poor survival of patients with glioblastoma multiforme: roles of sphingosine kinase isoforms in growth of glioblastoma cell lines. J Neuropathol Exp Neurol. 2005;64:695–705. doi: 10.1097/01.jnen.0000175329.59092.2c. [DOI] [PubMed] [Google Scholar]
- Venable ME, Webb-Froehlich LM, Sloan EF, Thomley JE. Shift in sphingolipid metabolism leads to an accumulation of ceramide in senescence. Mech Ageing Dev. 2006;127:473–80. doi: 10.1016/j.mad.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Venable ME, Yin X. Ceramide induces endothelial cell senescence. Cell Biochem Funct. 2009;27:547–51. doi: 10.1002/cbf.1605. [DOI] [PubMed] [Google Scholar]
- Visentin B, Vekich JA, Sibbald BJ, Cavalli AL, Moreno KM, Matteo RG, Garland WA, Lu Y, Yu S, Hall HS, Kundra V, Mills GB, Sabbadini RA. Validation of an anti-sphingosine-1-phosphate antibody as a potential therapeutic in reducing growth, invasion, and angiogenesis in multiple tumor lineages. Cancer Cell. 2006;9:225–38. doi: 10.1016/j.ccr.2006.02.023. [DOI] [PubMed] [Google Scholar]
- White-Gilbertson S, Mullen T, Senkal C, Lu P, Ogretmen B, Obeid L, Voelkel-Johnson C. Ceramide synthase 6 modulates TRAIL sensitivity and nuclear translocation of active caspase-3 in colon cancer cells. Oncogene. 2009;28:1132–41. doi: 10.1038/onc.2008.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J, Bohanan CS, Neumann JC, Lingrel JB. KLF2 transcription factor modulates blood vessel maturation through smooth muscle cell migration. J Biol Chem. 2008;283:3942–50. doi: 10.1074/jbc.M707882200. [DOI] [PubMed] [Google Scholar]
- Wu J, Spiegel S, Sturgill TW. Sphingosine 1-phosphate rapidly activates the mitogen-activated protein kinase pathway by a G protein-dependent mechanism. J Biol Chem. 1995;270:11484–8. doi: 10.1074/jbc.270.19.11484. [DOI] [PubMed] [Google Scholar]
- Xia P, Gamble JR, Wang L, Pitson SM, Moretti PA, Wattenberg BW, D'Andrea RJ, Vadas MA. An oncogenic role of sphingosine kinase. Curr Biol. 2000;10:1527–30. doi: 10.1016/s0960-9822(00)00834-4. [DOI] [PubMed] [Google Scholar]