Abstract
Recent research on the epidemiology of substance use disorders (SUDs) has provided important insights into these conditions and their impact on public health. In the United States, annual surveys of drug use in household and school populations serve as one of the primary sources of information about the distribution of illicit drug use. This research has demonstrated continued shifts in trends in illicit drug use in the United States and called attention to rising rates of prescription drug misuse and abuse. Findings have also continued to highlight the substantial comorbidity of SUDs with other psychiatric disorders and with the ongoing HIV epidemic. Building on these foundations, future challenges for research in substance abuse epidemiology will include using novel methodologic approaches to further unravel the complex interrelationships that link individual vulnerabilities for SUDs, including genetic factors, with social and environmental risk factors.
Introduction
Recent progress in the epidemiology of substance use disorders (SUDs) has been substantial and continues to provide important insights into these conditions and their impact on public health. Selected highlights reviewed in this article focus on recent findings and the systematic monitoring of trends in the landscape of drug use in the United States, the examination of the substantial comorbidity between SUDs and other psychiatric disorders, and the association of drug use with other high-risk behaviors and the spread of HIV. In addition, this article highlights important new directions in drug abuse epidemiology research, including the increasing integration of new methodologies into epidemiologic studies that promise to provide major advances in understanding the complex nature of drug use disorders. The future of substance abuse epidemiology depends on the successful application of these integrated approaches to the study of complex human behaviors. These multifactorial models for understanding SUDs build on the foundations of traditional substance abuse research and contemporary trends in epidemiology and increasingly incorporate a broad spectrum of methodologies from molecular genetics and neuroscience to social epidemiology [1,2].
Trends in Substance Use
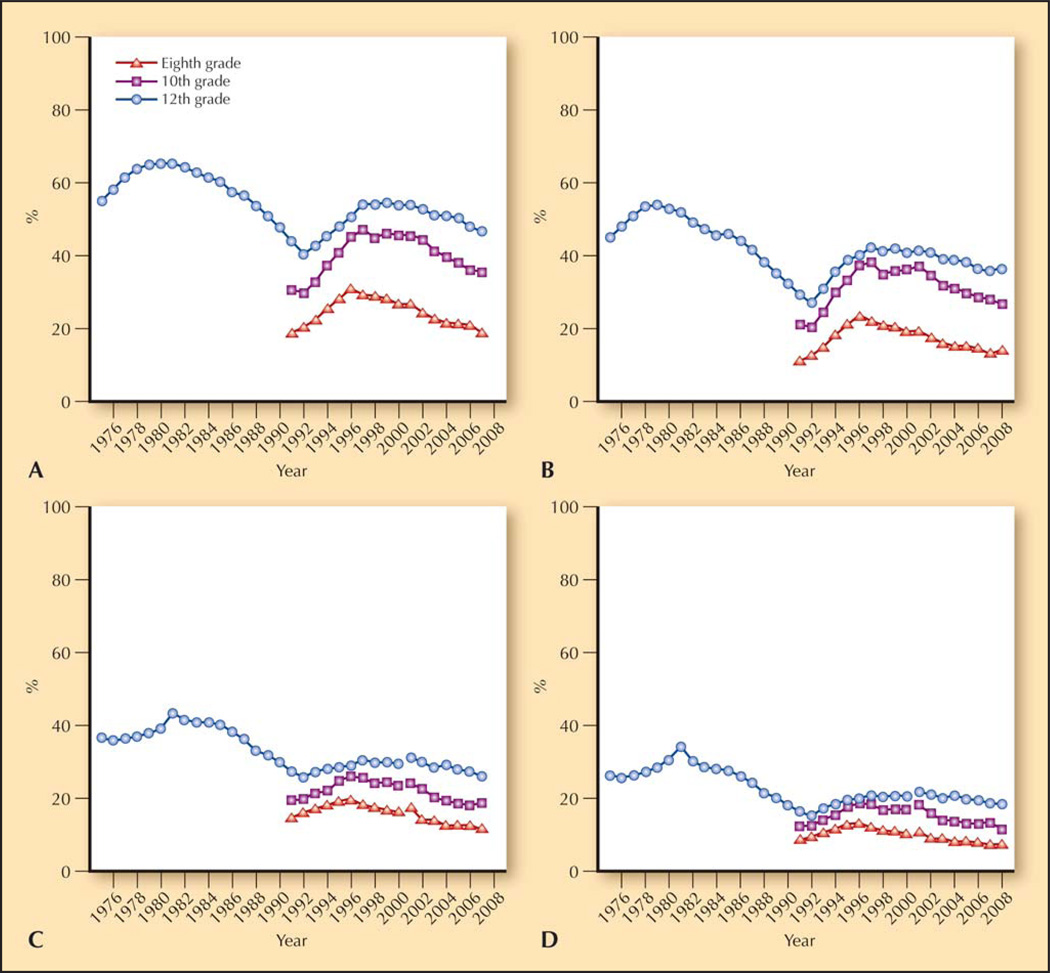
Large-scale population surveys such as the household-based National Survey on Drug Use and Health and the school-based Monitoring the Future (MTF) study have provided rich data on substance use in the United States and pointed out ongoing shifts in trends of illicit drug use [3•,4•]. Overall illicit drug use reached a peak in the late 1970s, declined during the 1980s, rose again in the 1990s, and has remained relatively stable during the past several years (Fig. 1) [3•,4•]. Despite some variation in the absolute rates found in the major surveys of drug use in the United States, these epidemiologic studies indicate that illicit drug use remains very common and typically begins during adolescence. The 2007 National Survey on Drug Use and Health data indicate that about 46.1% of individuals 12 years of age and older in the United States—an estimated 114 million individuals—have tried any illicit drug at least once in their lifetime, 40.6% have used marijuana, and 29.7% have used other illicit drugs [4•]. Reflecting the emergence of substance use in adolescence, the 2008 MTF found that 19.6% of students have tried an illicit drug by eighth grade, 34.1% by 10th grade, and 47.4% by 12th grade (Fig. 1) [3•]. The most recent findings from the MTF study also demonstrated that marijuana remains by far the most commonly used illicit drug, with 14.6% of eighth graders, 29.9% of 10th graders, and 42.6% of 12th graders reporting having tried it [3•]. A nearly universal finding across such studies is that drug use increases from adolescence to young adulthood, and then gradually declines [3•,4•].
Figure 1.
Trends in lifetime and annual illicit drug use among eighth, 10th, and 12th graders. A, Percentage who used any illicit drug in their lifetime. B, Percentage who used any illicit drug during the previous 12 months. C, Percentage who used any illicit drug other than marijuana in their lifetime. D, Percentage who used any illicit drug other than marijuana during the previous 12 months. Note that beginning in 2001, revised sets of questions on other hallucinogen and tranquilizer use were introduced. Thus, data for “any illicit drug other than marijuana” were affected by these changes. (From Johnston et al. [3•]; with permission.)
Another key finding derived from these ongoing surveys is that the number of individuals who report misuse of prescription drugs has been increasing in recent years [5]. In particular, the past few years have seen a marked increase in the misuse of prescription opioid medications, such as oxycodone and hydrocodone, along with a substantial increase in problems associated with such use, including fatal and nonfatal opioid overdose [5–7]. In 2008, marijuana remained the most commonly used category of abused substance among 12th graders (32.4% past year prevalence), but prescription drugs emerged as the second most common category (15.4% past year prevalence) [3•]. Much of the attention paid to this epidemic of prescription drug abuse is a result of the increasing recognition of the problem among teens in the United States [5,8,9]. Other concerning changes in recent years include increases in marijuana use, especially among younger blacks and Hispanics, which may be related to an increase in marijuana potency [10]; shifts in the epidemiology of methamphetamine use, with continued rising rates in the rural United States [4•,11,12]; and increased availability of high-purity heroin and a rise in heroin use via smoking and other noninjection routes [13].
Drug Abuse and Dependence
In addition to tracking trends in drug use, several ongoing, large-scale epidemiologic studies, such as the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), have assessed diagnostic categories of drug abuse and dependence as defined in the DSM-IV. Recent findings from the NESARC indicate that about 2.0% of adults living in US households had a DSM-IV drug use disorder in the prior 12 months (1.4% abuse, 0.6% dependence), and 10.3% reported a drug use disorder at any point in their lifetime (7.7% abuse, 2.6% dependence) [14••]. In addition, drug abuse and dependence were associated with significant disability, including missed work days and repeated hospitalizations [14••]. Drug use disorders thus represent a widespread and substantial public health problem in the United States. Of note, rates of drug abuse and dependence were significantly greater among men than women, a finding consistent with results of several previous epidemiologic surveys [4•,14••,15,16]. Several other sociodemographic correlates were also generally associated with greater risk of DSM-IV drug abuse and dependence on a 12-month and lifetime basis, including Native American ethnicity, younger age, having never been married, low income, and residing in the West [14••]. Other correlates were found to be specific for abuse or dependence or for the specific time period examined. For example, rates of 12-month drug dependence, but not 12-month drug abuse, were significantly greater among those with an education level less than a high school degree. These findings highlight the importance of disaggregating drug abuse from drug dependence and lifetime from current disorders. They also showed an especially high prevalence of drug use disorders among Native Americans, with 18.4% reporting a drug use disorder at some point in their lifetime (11.6% abuse, 6.9% dependence) [14••]. These findings are consistent with regional studies among Native Americans [17,18] and highlight the acute need of this community to gain access to substance abuse prevention and treatment services. Further detailed analyses of the NESARC data and other similar data are needed to examine the underlying reasons for these sociodemographic disparities within the context of the multifactorial nature of drug use disorders [14••].
Younger age is consistently associated with drug use disorders [4•,14••,16]. However, data from the NESARC also suggest increased rates among individuals 30 to 44 years of age who grew up in the wake of the 1970s US drug epidemic [14••]. These results indicate the potential for continued increases in rates of drug use disorders among older cohorts as the current baby boomer generation ages [19,20]. Findings from the NESARC also suggested that onset of drug abuse and drug dependence typically occurred during late adolescence or early adulthood, with onset later in life being rare [14••]. Thus, adolescence is a particularly vulnerable period for the onset of drug use disorders and an important target for continued etiologic and prevention research.
Comorbid Psychiatric Disorders
In addition to demonstrating a high prevalence of SUDs, recent epidemiologic research has provided consistent findings demonstrating the substantial comorbidity of SUDs with other psychiatric disorders. Findings from the Epidemiologic Catchment Area Survey [21], the National Comorbidity Survey [22], the National Longitudinal Alcohol Epidemiologic Survey [23], and the NESARC [14••,24] all showed that mood, anxiety, and personality disorders are strongly associated with drug use disorders. Epidemiologic surveys of adults also consistently show that anxiety, mood, and antisocial personality disorders are more strongly associated with drug dependence than drug abuse [25,26]. For example, recent reports from the NESARC found that the odds ratios between lifetime psychiatric and drug use disorders are higher for drug dependence than drug abuse among those with any anxiety disorder (4.9 and 1.7, respectively), mood disorder (7.1 and 2.3, respectively), and antisocial personality disorder (16.7 and 5.4, respectively) [27,28]. Findings from the NESARC also document the importance of controlling for other psychiatric disorders when examining associations between drug use disorders and specific psychiatric disorders [14••]. When analyses controlled for the presence of other comorbid psychiatric disorders, the strength of the associations between individual psychiatric disorders and drug use disorders was reduced but generally remained strong (Table 1). The decreased magnitude of these associations suggests that common causal pathways may underlie drug use disorders and other psychiatric disorders— findings that are consistent with twin and genetic studies [29]. These findings highlight the importance of continued research on both shared and unique risk factors underlying the comorbidity of psychiatric and drug use disorders.
Table 1.
Adjusted odds ratios for 12-month DSM-IV drug use disorders and other psychiatric disorders (controlling for demographic characteristics and comorbid psychiatric disorders) in the NESARC study
| ORs adjusted for demographic characteristics* | ORs adjusted for demographic characteristics and other psychiatric disorders† |
|||||
|---|---|---|---|---|---|---|
| Comorbid disorder | Drug use disorder (99% CI) |
Drug abuse (99% CI) |
Drug dependence (99% CI) |
Drug use disorder (99% CI) |
Drug abuse (99% CI) |
Drug dependence (99% CI) |
| Alcohol use disorder | 9.0 (6.94–11.70) | 6.4 (4.75–8.65) | 15.0 (8.57–26.59) | 5.6 (4.28–7.42) | 4.5 (3.25–6.25) | 7.0 (3.89–12.48) |
| Alcohol abuse | 2.7 (1.98–3.71) | 3.1 (2.18–4.50) | 1.6 (0.88–3.01) | 4.2 (3.03–5.85) | 4.2 (2.87–6.13) | 3.7 (1.79–7.58) |
| Alcohol dependence | 9.7 (7.13–13.10) | 5.7 (3.95–8.27) | 18.7 (10.83–32.34) | 6.8 (4.86–9.63) | 4.8 (3.11–7.31) | 9.0 (4.66–17.16) |
| Nicotine dependence | 5.8 (4.41–7.63) | 4.0 (2.86–5.69) | 11.0 (6.89–17.56) | 3.2 (2.38–4.38) | 2.6 (1.76–3.79) | 4.4 (2.63–7.42) |
| Any mood disorder | 3.5 (2.66–4.53) | 1.9 (1.34–2.70) | 8.5 (5.27–13.64) | 1.8 (1.33–2.41) | 1.1 (0.73–1.67) | 3.3 (1.92–5.56) |
| Major depressive disorder | 2.2 (1.56–3.07) | 1.4 (0.88–2.32) | 3.8 (2.18–6.48) | 1.4 (0.97–1.96) | 1.0 (0.63–1.69) | 2.2 (1.20–4.10) |
| Bipolar I disorder | 5.1 (3.35–7.80) | 2.4 (1.38–4.21) | 10.3 (5.75–18.62) | 2.3 (1.49–3.67) | 1.2 (0.61–2.24) | 4.2 (2.14–8.35) |
| Bipolar II disorder | 2.4 (1.23–4.49) | 2.1 (1.02–4.32) | 2.6 (0.92–7.33) | 1.2 (0.58–2.63) | 1.2 (0.50–2.68) | 1.4 (0.40–4.59) |
| Dysthymia | 4.0 (2.17–7.20) | 2.1 (0.85–5.25) | 6.9 (3.28–14.67) | 2.1 (1.15–3.84) | 1.5 (0.62–3.76) | 2.8 (1.16–6.67) |
| Any anxiety disorder | 2.7 (2.05–3.67) | 1.6 (1.15–2.25) | 6.0 (3.74–9.55) | 1.2 (0.88–1.73) | 0.9 (0.62–1.34) | 1.9 (1.07–3.24) |
| Any panic disorder | 3.9 (2.58–5.87) | 1.9 (1.02–3.62) | 7.8 (4.31–14.05) | 1.5 (0.91–2.39) | 1.0 (0.49–2.10) | 1.8 (0.85–3.81) |
| Panic with agoraphobia | 5.6 (3.01–10.34) | 3.2 (1.20–8.33) | 9.2 (3.98–21.24) | 1.7 (0.80–3.57) | 1.4 (0.51–4.03) | 1.5 (0.44–4.93) |
| Panic without agoraphobia | 3.1 (1.87–5.14) | 1.4 (0.62–3.32) | 6.4 (3.21–12.58) | 1.3 (0.75–2.28) | 0.8 (0.32–2.13) | 1.8 (0.85–3.94) |
| Social phobia | 2.6 (1.69–4.15) | 1.7 (0.94–3.00) | 4.5 (2.53–8.16) | 1.2 (0.71–1.93) | 1.1 (0.58–2.04) | 1.2 (0.58–2.48) |
| Specific phobia | 2.3 (1.65–3.21) | 1.6 (1.06–2.47) | 3.8 (2.14–6.73) | 1.0 (0.68–1.41) | 0.9 (0.58–1.46) | 1.0 (0.53–2.00) |
| Generalized anxiety | 4.5 (2.80–7.09) | 2.0 (0.98–4.00) | 9.5 (4.82–18.83) | 1.7 (0.97–2.92) | 1.1 (0.51–2.28) | 2.5 (1.02–5.88) |
| Any personality disorder | 4.1 (3.27–5.15) | 2.6 (1.94–3.49) | 9.6 (6.44–14.43) | 2.2 (1.71–2.91) | 1.8 (1.26–2.48) | 3.3 (2.00–5.33) |
| Avoidant | 3.4 (2.25–5.12) | 2.0 (1.05–3.69) | 6.0 (3.19–11.34) | 1.3 (0.85–2.05) | 1.1 (0.56–2.30) | 1.3 (0.63–2.60) |
| Dependent | 7.3 (3.65–14.54) | 2.4 (0.89–6.67) | 14.9 (6.36–34.71) | 2.2 (1.02–4.80) | 1.1 (0.37–3.20) | 2.4 (0.75–7.77) |
| Obsessive-compulsive | 2.3 (1.65–3.15) | 1.4 (0.87–2.17) | 4.6 (2.91–7.34) | 0.9 (0.57–1.33) | 0.7 (0.40–1.23) | 1.2 (0.69–2.10) |
| Paranoid | 3.5 (2.49–4.86) | 2.0 (1.28–3.00) | 6.7 (4.09–11.07) | 1.1 (0.66–1.68) | 0.9 (0.48–1.50) | 1.1 (0.59–2.22) |
| Schizoid | 3.4 (2.33–5.03) | 2.1 (1.26–3.56) | 5.8 (3.35–10.11) | 1.5 (0.88–2.44) | 1.2 (0.66–2.32) | 1.5 (0.74–3.21) |
| Histrionic | 4.5 (2.98–6.77) | 2.5 (1.45–4.21) | 8.4 (4.69–14.92) | 1.3 (0.79–2.20) | 1.0 (0.58–1.86) | 1.4 (0.63–3.03) |
| Antisocial | 6.4 (4.77–8.56) | 4.3 (2.84–6.50) | 9.7 (6.29–15.10) | 2.9 (2.08–4.12) | 2.5 (1.57–3.99) | 2.6 (1.45–4.53) |
Adjusted for age, race/ethnicity, sex, education, income, marital status, urbanicity, and geographic region; significant ORs are highlighted in boldface.
Adjusted for age, race/ethnicity, sex, education, income, marital status, urbanicity, geographic region, and other psychiatric disorders; significant ORs are highlighted in boldface.
NESARC—National Epidemiologic Survey on Alcohol and Related Conditions; OR—odds ratio.
(Data from Compton et al. [14••].)
Comorbid HIV Infection
Drug abuse epidemiology research continues to explore the role of substance use and SUDs in contributing to the HIV epidemic. Injection drug use continues to be a substantial category of risk for HIV infection, with an estimated 16% of individuals with newly diagnosed HIV infections in the United States in 2006 reporting this as a contributing risk factor [30]. In addition to the risk of HIV infection through sharing injection equipment among injection drug users, noninjection drug use is associated with increased likelihood to engage in other HIV risk behaviors [31]. For example, drugs such as methamphetamine and related stimulants can simultaneously increase libido, lower inhibitions, and cloud judgment, raising the risk of individuals engaging in unsafe sexual behaviors in which they might not have otherwise engaged [32,33]. In growing recognition of the substantial combined comorbidity of SUDs, HIV, and psychiatric illness, epidemiologic research has focused increasingly on the importance of understanding these conditions as part of a “syndemic” of multiple, linked epidemics that are powerfully influenced by social context [34–36]. This research promises to provide a better understanding of the interrelationships among drug abuse, HIV, other illnesses, and social conditions such as poverty and structural violence in order to better explain the disproportionate burden of these illnesses experienced by some communities [34,37].
Genetic Epidemiology
Family history is one of the most consistently and strongly associated risk factors for drug use disorders. Results from family studies show that drug use disorders tend to cluster within families [38]; twin and adoption studies suggest that much of the familial clustering of drug use disorders can be explained by genetic factors [29]. Several controlled family studies demonstrated that substance abuse or dependence in probands (ie, the index case in genetically informative designs) is associated with a substantial increase in risk for these disorders among first-degree adult relatives and offspring [39,40]. Furthermore, risk is conferred generally across the various classes of illicit drugs and within specific drug classes [41]. Genetic epidemiologic studies of drug use disorders have yielded consistent results indicating clearly that drug use disorders have genetic and environmental underpinnings in need of further explication.
Of note, genetic factors appear to be more strongly associated with drug use disorders than with drug use in and of itself [29]. This finding suggests that genetic factors may be important for identifying individuals at risk for drug use disorders, whereas the prevention of onset of drug use is much more likely to be based on efforts to change environmental risk factors. As with many other relatively common diseases, the risk for drug use disorders is believed to emerge from a combination of factors, including multiple possible genes exerting small effects, gene–gene interactions, gene–environment interactions, and a host of environmental factors and individual riskconferring behaviors [29,41–43]. Because identifying gene–environment interactions is likely to prove key to understanding the etiology of drug use disorders [42,43], advances in this important area will benefit from large, prospective, genetically informed studies drawn from large, representative populations.
Future Directions
The future of substance abuse epidemiology depends on the successful application of integrated approaches to the study of complex human behaviors. Such a goal of studying multifactorial models is consistent with current trends in epidemiology [2] and builds on the rich history of drug abuse epidemiology by incorporating perspectives from molecular genetics and neuroscience into individual and social epidemiology. By integrating these diverse transdisciplinary approaches, prevention and treatment of drug use and drug use disorders will be enhanced [1]. Novel conceptualizations and measurements of social and cultural contexts within theoretically grounded research are suggested because increased understanding of how genetic, biological, social, and contextual phenomena interact to influence behavior will better inform prevention and treatment for individuals at risk for drug use and drug use disorders [44]. Recent research has begun to focus on the complex interactions among a range of such factors, including norms established by family members and public figures, peer group influences, and social and institutional processes [45,46]. Neighborhood and community level factors, such as residential instability, community cohesion, or other aspects of local environments, also likely serve as potential risk or protective factors for drug use behaviors [47•]. Epidemiologic studies of drug use and drug use disorders increasingly will need to examine the complex interaction of these individual and social environmental factors, including immediate individual factors and cumulative intergenerational effects [47•].
One of the key challenges for epidemiology will be harnessing selected measures from a range of disciplines, such as sociology and neurobiology, that can be applied to large-scale, population-based studies. Measurement technologies that are already increasingly feasible for use in epidemiologic studies include neuroimaging, serum samples for metabolic studies [48], and specimens for genetic association studies. For example, as the technology for obtaining genetic specimens through mouthwashes and cheek swabs improves, applying such techniques in broad, population-based samples becomes more feasible in terms of cost and acceptability to study participants [49]. Additional promising new epidemiologic techniques include ecological momentary assessment tools that can capture information from cohorts nearly at the time of its occurrence through participants’ use of novel recording devices (eg, personal digital assistants or cellular phones) [50]. Moving into the study of interactions across domains of risk—individual susceptibility, social environment, gene–environment interactions—provides great promise for the next generation of drug abuse epidemiology research.
Conclusions
Epidemiology provides the foundation for understanding drug use, abuse, and dependence by demonstrating the distribution and determinants of these disorders. Through population-based studies, key clues as to etiologic risk factors for these disorders are identified for detailed exploration in more refined epidemiologic and nonepidemiologic studies. As the field of epidemiology moves into an integrative era [1,2,47•], the epidemiology of drug use and drug use disorders must remain at the forefront. The goal will increasingly be to develop integrated models that improve understanding of the complex interrelationships among social factors, environmental agents, genetic predisposition, and other individual factors contributing to the risk of drug use disorders. Achieving this goal will require continued refinement of existing methods and development of new techniques for understanding the individual and the environment. The knowledge obtained from such studies will improve the nation’s public health by promoting integrated approaches to preventing and treating drug abuse and dependence.
Acknowledgment
The views and opinions expressed in this article are those of the authors and should not be construed necessarily to represent the views of any of the sponsoring agencies or the US government.
Footnotes
Disclosure
No potential conflicts of interest relevant to this article were reported.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Fishbein D. The importance of neurobiological research to the prevention of psychopathology. Prev Sci. 2000;1:89–106. doi: 10.1023/a:1010090114858. [DOI] [PubMed] [Google Scholar]
- 2.Susser E, Bresnahan M. Origins of epidemiology. Ann N Y Acad Sci. 2001;954:6–18. doi: 10.1111/j.1749-6632.2001.tb02743.x. [DOI] [PubMed] [Google Scholar]
- 3. Johnston LD, O’Malley PM, Bachman JG, et al. Bethesda, MD: National Institute on Drug Abuse; 2009. Monitoring the Future: National Survey Results on Drug Use, 1975–2008.. This is an excellent source of epidemiologic data on drug use among a school-based cohort.
- 4. Substance Abuse and Mental Health Services Administration. Results From the 2007 National Survey on Drug Use and Health: National Findings. Rockville, MD: US Department of Health and Human Services; 2008. . This is an excellent source of epidemiologic data on drug use among a household-based cohort.
- 5.Compton WM, Volkow ND. Major increases in opioid analgesic abuse: concerns and strategies. Drug Alcohol Depend. 2006;81:103–107. doi: 10.1016/j.drugalcdep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 6.Ballesteros MF, Budnitz DS, Sanford CP, et al. Increase in deaths due to methadone in North Carolina. JAMA. 2003;290:40. doi: 10.1001/jama.290.1.40. [DOI] [PubMed] [Google Scholar]
- 7.Hall AJ, Logan JE, Toblin RL, et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300:2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- 8.Boyd CJ, McCabe SE, Cranford JA, et al. Adolescents’ motivations to abuse prescription medications. Pediatrics. 2006;118:2472–2480. doi: 10.1542/peds.2006-1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCabe SE, Boyd CJ, Young A. Medical and nonmedical use of prescription drugs among secondary school students. J Adolesc Health. 2007;40:76–83. doi: 10.1016/j.jadohealth.2006.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Compton WM, Grant BF, Colliver JD, et al. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- 11.Thomas YF, Compton WM. Rural populations are not protected from drug use and abuse. J Rural Health. 2007;23:1–3. doi: 10.1111/j.1748-0361.2007.00116.x. [DOI] [PubMed] [Google Scholar]
- 12.Gfroerer JC, Larson SL, Colliver JD. Drug use patterns and trends in rural communities. J Rural Health. 2007;23:10–15. doi: 10.1111/j.1748-0361.2007.00118.x. [DOI] [PubMed] [Google Scholar]
- 13.Community Epidemiology Work Group. Epidemiological Trends in Drug Abuse. Washington, DC: National Institute on Drug Abuse; 2004. [Google Scholar]
- 14. Compton WM, Thomas YF, Stinson FS, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566.. These were detailed analyses of drug abuse and dependence prevalence, correlates, and comorbidity with other Axis I and II disorders.
- 15.Grant BF. Prevalence and correlates of drug use and DSM-IV drug dependence in the United States: results of the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse. 1996;8:195–210. doi: 10.1016/s0899-3289(96)90249-7. [DOI] [PubMed] [Google Scholar]
- 16.Teesson M, Baillie A, Lynskey M, et al. Substance use, dependence and treatment seeking in the United States and Australia: a cross-national comparison. Drug Alcohol Depend. 2006;81:149–155. doi: 10.1016/j.drugalcdep.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 17.Beals J, Novins DK, Whitesell NR, et al. Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: mental health disparities in a national context. Am J Psychiatry. 2005;162:1723–1732. doi: 10.1176/appi.ajp.162.9.1723. [DOI] [PubMed] [Google Scholar]
- 18.Gilder DA, Wall TL, Ehlers CL. Comorbidity of select anxiety and affective disorders with alcohol dependence in southwest California Indians. Alcohol Clin Exp Res. 2004;28:1805–1813. doi: 10.1097/01.alc.0000148116.27875.b0. [DOI] [PubMed] [Google Scholar]
- 19.Gfroerer J, Penne M, Pemberton M, et al. Substance abuse treatment need among older adults in 2020: the impact of the aging baby-boom cohort. Drug Alcohol Depend. 2003;69:127–135. doi: 10.1016/s0376-8716(02)00307-1. [DOI] [PubMed] [Google Scholar]
- 20.Colliver JD, Compton WM, Gfroerer JC, et al. Projecting drug use among aging baby boomers in 2020. Ann Epidemiol. 2006;16:257–265. doi: 10.1016/j.annepidem.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 21.Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 22.Warner LA, Kessler RC, Hughes M, et al. Prevalence and correlates of drug use and dependence in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:219–229. doi: 10.1001/archpsyc.1995.03950150051010. [DOI] [PubMed] [Google Scholar]
- 23.Grant BF. Comorbidity between DSM-IV drug use disorders and major depression: results of a national survey of adults. J Subst Abuse. 1995;7:481–497. doi: 10.1016/0899-3289(95)90017-9. [DOI] [PubMed] [Google Scholar]
- 24.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 25.Merikangas KR, Mehta RL, Molnar BE, et al. Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict Behav. 1998;23:893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- 26.Swendsen JD, Merikangas KR. The comorbidity of depression and substance use disorders. Clin Psychol Rev. 2000;20:173–189. doi: 10.1016/s0272-7358(99)00026-4. [DOI] [PubMed] [Google Scholar]
- 27.Conway KP, Compton W, Stinson FS, et al. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67:247–257. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- 28.Compton WM, Conway KP, Stinson FS, et al. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66:677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- 29.Kendler KS, Prescott CA, Myers J, et al. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. [Accessed March 27, 2009];Cases of HIV infection and AIDS in the United States and dependent areas, 2007. Available at http://cdc.gov/hiv/topics/surveillance/resources/reports/2007report/default.htm.
- 31.Woody GE, Donnell D, Seage GR, et al. Non-injection substance use correlates with risky sex among men having sex with men: data from HIVNET. Drug Alcohol Depend. 1999;53:197–205. doi: 10.1016/s0376-8716(98)00134-3. [DOI] [PubMed] [Google Scholar]
- 32.Mansergh G, Purcell DW, Stall R, et al. CDC consultation on methamphetamine use and sexual risk behavior for HIV/STD infection: summary and suggestions. Public Health Rep. 2006;121:127–132. doi: 10.1177/003335490612100205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krawczyk CS, Molitor F, Ruiz J, et al. Methamphetamine use and HIV risk behaviors among heterosexual men—preliminary results from five northern California counties, December 2001–November 2003. MMWR Morb Mortal Wkly Rep. 2006;55:273–277. [PubMed] [Google Scholar]
- 34.Walkup J, Blank MB, Gonzalez JS, et al. The impact of mental health and substance abuse factors on HIV prevention and treatment. J Acquir Immune Defic Syndr. 2008;47 Suppl 1:S15–S19. doi: 10.1097/QAI.0b013e3181605b26. [DOI] [PubMed] [Google Scholar]
- 35.Des Jarlais DC, Semaan S. HIV prevention for injecting drug users: the first 25 years and counting. Psychosom Med. 2008;70:606–611. doi: 10.1097/PSY.0b013e3181772157. [DOI] [PubMed] [Google Scholar]
- 36.Mustanski B, Garofalo R, Herrick A, et al. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34:37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Friedman SR, Tempalski B, Cooper H, et al. Metropolitan area characteristics, injection drug use and HIV among injectors. In: Thomas YF, Richardson D, Cheung I, editors. Geography and Drug Addiction. Washington, DC: Springer; 2008. pp. 255–265. [Google Scholar]
- 38.Bierut LJ, Dinwiddie SH, Begleiter H, et al. Familial transmission of substance dependence: alcohol, marijuana, cocaine, and habitual smoking: a report from the Collaborative Study on the Genetics of Alcoholism. Arch Gen Psychiatry. 1998;55:982–988. doi: 10.1001/archpsyc.55.11.982. [DOI] [PubMed] [Google Scholar]
- 39.Chassin L, Pitts SC, Prost J. Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: predictors and substance abuse outcomes. J Consult Clin Psychol. 2002;70:67–78. [PubMed] [Google Scholar]
- 40.Moss HB, Lynch KG, Hardie TL, et al. Family functioning and peer affiliation in children of fathers with antisocial personality disorder and substance dependence: associations with problem behaviors. Am J Psychiatry. 2002;159:607–614. doi: 10.1176/appi.ajp.159.4.607. [DOI] [PubMed] [Google Scholar]
- 41.Compton WM, Cottler LB, Ridenour T, et al. The specificity of family history of alcohol and drug abuse in cocaine abusers. Am J Addict. 2002;11:85–94. doi: 10.1080/10550490290087866. [DOI] [PubMed] [Google Scholar]
- 42.Caspi A, McClay J, Moffitt TE, et al. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297:851–854. doi: 10.1126/science.1072290. [DOI] [PubMed] [Google Scholar]
- 43.Foley DL, Eaves LJ, Wormley B, et al. Childhood adversity, monoamine oxidase a genotype, and risk for conduct disorder. Arch Gen Psychiatry. 2004;61:738–744. doi: 10.1001/archpsyc.61.7.738. [DOI] [PubMed] [Google Scholar]
- 44.Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiol Rev. 2004;26:36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- 45.Burton LM, Jarrett RL. In the mix, yet on the margins: the place of families in urban neighborhood and child development research. J Marriage Fam. 2000;62:444–465. [Google Scholar]
- 46.Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing “neighborhood effects:” social processes and new directions in research. Ann Rev Sociol. 2002;28:443–478. [Google Scholar]
- 47. Galea S, Hall C, Kaplan GA. Social epidemiology and complex system dynamic modelling as applied to health behavior and drug use research. Int J Drug Policy. 2009;20:209–216. doi: 10.1016/j.drugpo.2008.08.005.. This article discusses approaches to complex system dynamic modeling in drug abuse epidemiology.
- 48.Young EA, Breslau N. Cortisol and catecholamines in posttraumatic stress disorder: an epidemiologic community study. Arch Gen Psychiatry. 2004;61:394–401. doi: 10.1001/archpsyc.61.4.394. [DOI] [PubMed] [Google Scholar]
- 49.Cozier YC, Palmer JR, Rosenberg L. Comparison of methods for collection of DNA samples by mail in the Black Women’s Health Study. Ann Epidemiol. 2004;14:117–122. doi: 10.1016/S1047-2797(03)00132-7. [DOI] [PubMed] [Google Scholar]
- 50.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]