Abstract
Objective
This study was designed to explore the acceptability, feasibility, and initial efficacy of a new shelter-based treatment for victims of intimate partner violence (IPV; i.e., HOPE).
Method
A phase I randomized clinical trial comparing HOPE (n = 35) to standard shelter services (SSS) (n = 35) was conducted. Primary outcome measures included the Clinician Administered PTSD Scale (CAPS) and the Revised Conflict Tactic Scales. Participants were followed at 1-week, 3- and 6-months post-shelter.
Results
Participants reported HOPE to be credible and indicated a high degree of satisfaction with treatment. Only two women withdrew from treatment. Both intent to treat (ITT) and minimal attendance (MA) analyses found that HOPE treatment relative to SSS was significantly associated with a lower likelihood of re-abuse over the 6-month follow-up period (OR = 5.1, RR = 1.75; OR = 12.6, RR = 3.12, respectively). Results of hierarchical linear model (HLM) analyses found a significant treatment effect for emotional numbing symptom severity in the ITT sample, t (67) = −2.046, p <.05, and significant treatment effects for effortful avoidance symptom severity, t (49) = −2.506, p < .05 and arousal symptom severity, t (49) = −2.04, p <.05, in the MA sample. Significant effects were also found for depression severity, empowerment, and social support.
Conclusions
Results support the acceptability and feasibility of HOPE and suggest that HOPE may be a promising treatment for IPV victims in shelter. However, results also suggest that modifications to HOPE may be required to improve treatment outcomes.
Approximately 1 in 4 women report a history of intimate partner violence (IPV) (Breiding, Black, & Ryan, 2008). Posttraumatic Stress Disorder (PTSD) is one of the most prevalent disorders found in IPV victims (Golding, 1999) and is associated with significant morbidity (Johnson, Zlotnick, & Perez, 2008). IPV victims in shelter tend to present with more severe abuse and related injury and exhibit higher rates of PTSD than do women who do not seek shelter (Jones, Hughes, & Untestaller, 2001). Conservation of resource theory (Hobfoll & Lily, 1993) posits that there is a downward, bidirectional spiral between loss of personal and social resources and PTSD, in which PTSD can then lead to a significant loss of resources, which may contribute to IPV victims’ difficulty in establishing long-term safety.
Consistently, recent research suggests that PTSD symptoms in IPV victims are associated with increased risk of re-abuse (Krause, Kaltman, Goodman, & Dutton, 2006). More specifically, Krause et al. (2006) found the emotional numbing symptoms of PTSD to be associated with the greatest risk for re-abuse. These findings suggest that IPV victims may become numb during dangerous situations, reducing their ability to appropriately perceive situations as unsafe due to numbing, increasing their risk for re-abuse. Given these findings, it is imperative that there are timely interventions that address PTSD. Battered women’s shelters might provide an opportune time to intervene with IPV victims regarding their PTSD, because these women have already instituted a major change in their life. Furthermore, shelters are prevalent throughout the United States (approximately 2,000 community-based shelters throughout the United States, serve 300,000 women and children each year (NCADV, 2008)) and therefore provide access to a difficult-to reach group of women. Few shelters offer evidence-based treatment for PTSD.
Although safety planning is not inconsistent with existing PTSD treatments, neither treatments for the acute aftermath of trauma (e.g., Bryant, Harvey, Dang, Sackville, & Basten, 1998) or PTSD (e.g., Foa et al, 2005.; Resick et al., 2008) offers specific strategies for addressing the unique needs of IPV victims who seek shelter. Exposure-based treatments, which are the first-line recommended treatments for PTSD, target habituation to fear-related stimuli. However, treatment for recent IPV victims should address their most immediate needs which includes establishing safety and accessing resources to improve their ability to cope with the abuse and establish independence from the abuser. The only empirically supported treatment designed specifically for IPV-related PTSD (e.g., Kubany et al., 2004) is intended for women who have permanently left their abuser and established physical safety, and therefore inadequately addresses the specific needs of sheltered IPV victims who face ongoing threats of abuse and have substantial resource needs (e.g., housing, accessing legal remedies, employment). Thus, PTSD treatment that addresses the unique needs of IPV victims in shelter is still needed.
Helping to Overcome PTSD through Empowerment (HOPE), a new cognitive-behavioral treatment (CBT), is designed to address the need for PTSD treatment in sheltered IPV victims. HOPE is informed by Herman’s (1992) multi-stage model of recovery that views recovery from chronic trauma, including IPV, as occurring in three stages: (1) establishing safety, (2) remembrance and mourning, and (3) reconnection. The most urgent clinical need in PTSD treatment is the establishment of physical and emotional safety. IPV victims come to shelters to establish physical safety and access resources to improve the quality of their lives. Thus, a first-stage, present-centered treatment, emphasizing safety and stabilization is most consistent with the treatment needs of IPV victims in shelter.
HOPE incorporates Herman’s stage approach within a cognitive-behavioral framework, including many of the components of traditional CBT for PTSD (e.g., cognitive-restructuring, skill-building). Cognitive-behavioral theories propose that individuals with PTSD process the trauma based on their preexisting beliefs about the self, others, and the world (Ehlers & Clark, 2000; McCann, Sakheim, & Abrahamson, 1988). These idiosyncratic, negative appraisals of the trauma and the trauma sequelae (e.g., overgeneralizations, misinterpretations of PTSD symptoms) can contribute to PTSD by producing an exaggerated sense of current threat. These negative appraisals can sustain PTSD through the production of negative emotions and related dysfunctional coping strategies that enhance and/or maintain PTSD symptoms (Ehlers & Clark, 2000). Recent IPV victims need to realistically appraise their degree of threat and learn how to manage their PTSD symptoms in a manner that does not maintain or intensify PTSD. HOPE targets maladaptive cognitions about self, others, and the world, with a special focus on McCann et al.’s (1988) five schematic areas of dysfunction (i.e., safety, trust, power/control, esteem, intimacy), while simultaneously emphasizing current needs of safety, self-care and protection, the exchange of information on PTSD, and empowerment. Further, HOPE is uniquely suited to IPV victims in shelters because it encourages women to identify how their PTSD symptoms may be interfering with their ability to use resources and establish long-term safety. HOPE also emphasizes the need for collaboration with case managers and other resource providers.
A pilot open-trial of HOPE found that participants who received HOPE experienced less PTSD symptoms, depression, resource loss, and impairment after leaving shelter and these gains were maintained through 6-month follow-up (Johnson & Zlotnick, 2006). The current study was designed to extend these findings and explore the feasibility, acceptability, and initial efficacy of HOPE in a preliminary randomized controlled trial (RCT) with 70 residents of battered women’s shelters. Primary outcomes were PTSD severity and re-abuse after leaving shelter. Secondary outcomes included degree of depressive symptoms, empowerment, resource loss, and social support.
Method
Participants
Participants were residents of one of two inner-city battered women’s shelters within the same shelter system serving a mid-sized mid-western city. To be eligible, participants had to experience an incident of IPV on the Conflict Tactic Scales-Revised (CTS-2; Straus, Hamby, Boney-McCoy, & Sugarman, 1996) the month prior to shelter admission, and meet diagnostic criteria for IPV-related PTSD or subthreshold PTSD according to the Clinician Administered PTSD Scale (CAPS; Blake et al., 1995). To meet criteria for subthreshold PTSD, participants had to meet criteria A (exposure to IPV), B (re-experiencing symptoms), E (symptom duration of at least one month), and F (significant distress or impairment of functioning) as well as either C (avoidance symptoms) or D (increased arousal) (Stein, Walker, Hazen, & Forde, 1997). We chose to use subthreshold PTSD as the inclusion criteria in an effort to increase the generalizability of findings. Further, subthreshold PTSD is associated with significant impairment and morbidity (Stein et al., 1997) and is frequently used as inclusion criteria in randomized controlled trials of treatments that target PTSD symptoms (e.g., Blanchard et al., 2003; Hien et al., 2009). Participants were excluded from the study if they (a) had symptoms of psychosis on the psychotic screen of the Structured Clinical Interview for Axis I disorders (SCID-I/P; First, Gibbon, Spitzer, Williams, & Benjamin, 1996), (b) met diagnostic criteria for lifetime Bipolar Disorder on the SCID-I/P, (c) endorsed significant suicidal ideation with intent and plan, (d) if on psychotropic medications, have had any change in medication dose or type in the last month, or (e) were in concurrent individual therapy.
Procedures
Design
A randomized, controlled, repeated measures design was used to assess the efficacy of HOPE plus standard shelter services (SSS) (HOPE; n = 35) to SSS alone (control; n = 35). This study is a phase I developmental trial. A power analysis was completed a priori to assure ability to detect large effects (Cohen’s d = .80), with the overall aim of this trial to assess acceptability and feasibility, and to determine estimates of ranges of effect sizes for future larger-scale trials. One week after baseline, the first author randomly assigned participants to one of the conditions using an urn randomization procedure (Stout, Wirtz, Carbonari, & DelBoca, 1994) stratifying participants according to PTSD status (i.e., PTSD and subthreshold PTSD) and medication status (i.e., on psychotropic medications or not). All participants received SSS. Participants randomized to HOPE also received a maximum of 12 sessions approximately twice weekly while in shelter. Participants who left shelter prior to completing HOPE were referred to community resources. This procedure was used in an effort to mirror the reality of SSS as most shelters no longer provide services after discharge. Those randomized to the control condition were provided referrals for treatment in the community. All participants were assessed for follow-up 1-week, 3- and 6-months after leaving shelter. Baseline interviews and therapy sessions occurred in shelter. Follow-up interviews occurred at the participants’ home, local hospitals, or another safe and confidential location (e.g., library). Phone interviews were offered to those who moved out of the region. Participants were paid $50 for each assessment. The trial was stopped once recruitment goals were met.
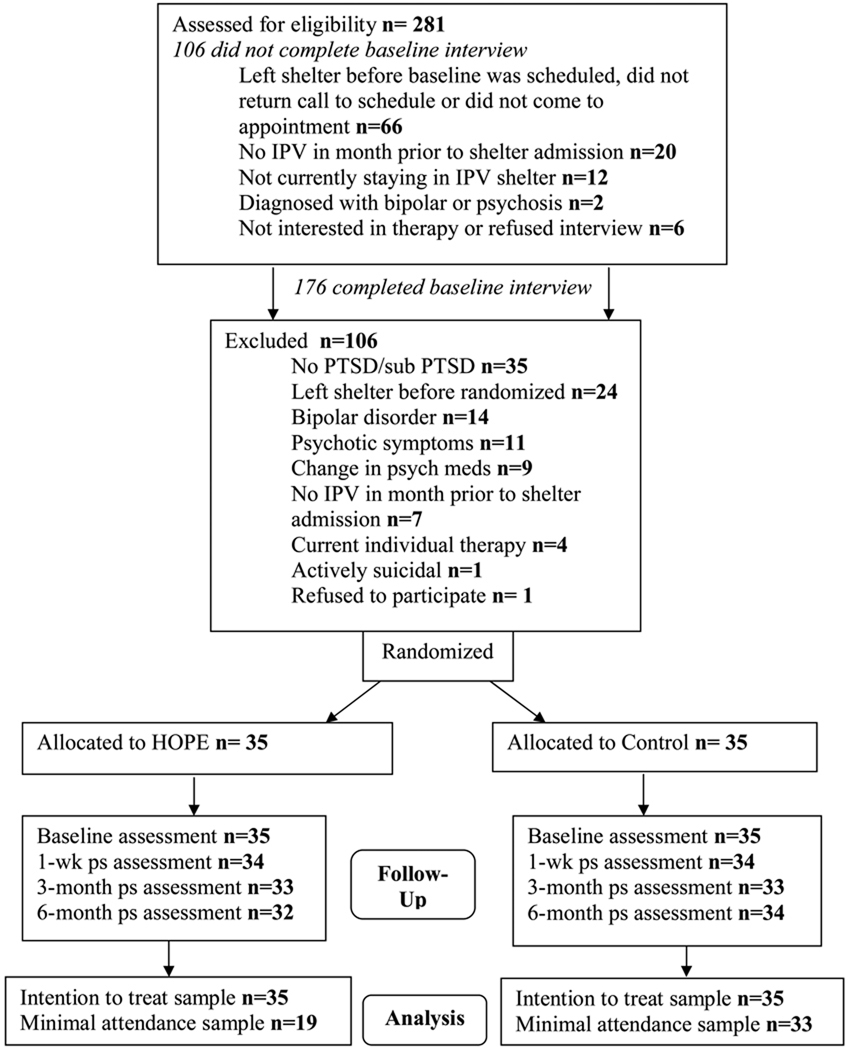
Recruitment occurred from 2004 to 2007. All research procedures were approved by relevant Institutional Review Board and all participants signed an informed consent document. The study was advertised through brochures that described a study evaluating a new counseling program for some of the common reactions to IPV. Shelter staff also referred interested residents to contact HOPE staff. Residents called a confidential research line and completed a screening in which the details of the study were clarified and interest, IPV history, and exclusionary criteria were assessed (see Figure 1). After screening, participants were scheduled for an interview that assessed eligibility. A Certificate of Confidentiality was obtained from the National Institute of Mental Health. Interviews lasted 2–3 hours. Graduate students in psychology or counseling under the direct supervision of the first author conducted interviews. Interview training included detailed instruction on interview procedures, practice with a trained interviewer, and observation of experienced interviewers. Interviewers attended weekly group supervision in which they received feedback about proper administration of assessments to minimize coder drift.
Figure 1.
CONSORT diagram of participant flow through the protocol. IPV= intimate partner violence; PTSD= posttraumatic stress disorder; wk = week; ps = post shelter.
Measures
Inclusion Criteria and Primary Outcomes
PTSD
The CAPS (Blake et al., 1995), a structured interview with established reliability and validity (Weathers, Keane, & Davidson, 2001) was used to assess for IPV-related PTSD diagnosis and past-week symptom severity. In the current study, IPV-related PTSD was assessed for the IPV that led to their shelter admission. Inter-rater reliability was assessed for 21 randomly selected interviews for CAPS-derived PTSD diagnoses (kappa = .83). Total CAPS scores, as well as scores for re-experiencing, arousal, effortful avoidance, and emotional numbing clusters were computed. Total CAPS scores demonstrated strong reliability (α = .91), with each of the CAPS factor scores also demonstrating adequate reliability (α = .66–.84).
IPV
The CTS2, a self-report measure with established validity and reliability (Straus et al., 1996), which assesses the extent to which 39 acts of negotiation, psychological aggression, physical assault, sexual coercion, and injury were perpetrated against participants, was used to assess for IPV the month prior to shelter admission and in the last month at each follow-up period. The CTS2 was used in two ways for the current study. First, in order to meet study criteria, participants had to endorse at least one item of CTS2 subscales of psychological aggression, physical assault, sexual coercion, or injury the month prior to shelter admission. Second, the CTS-2 was re-administered at each follow-up time point and participants were asked to rate the frequency of each abusive tactic by both their index partner and any new or additional intimate partner. Given that continuous data from the CTS-2 at each of the follow-up periods demonstrated significant skewness (2.16–2.57) and kurtosis (3.61–6.52), a categorical variable classifying participants as experiencing any psychological aggression, physical assault, sexual coercion, or injury by any partner over the 6 month follow-up period was created.
Comorbidity
The mood, anxiety, and substance-use modules of the SCID-I/P (First et al., 2002) were used to assess current (i.e., last month) Axis I comorbidity to PTSD. Inter-rater reliability was calculated for our most frequent comorbid diagnosis, Major Depression, for 16 randomly selected interviews (kappa = .87).
Demographic/Descriptive Variables
Demographic Interview
Demographic information was obtained through a semi-structured interview, and included age, race/ethnicity, education, receipt of public assistance, employment status, number of children, marital/living status, presence of restraining/protective order, presence of prior IPV, length of shelter stay, and contact with abuser.
Trauma History
The Trauma History Questionnaire (THQ; Greene, 1996) was used to assess lifetime history of traumatic events other than IPV. The THQ includes 24 items assessing crime, general disaster/trauma, and sexual and physical assault experiences. For each item the participant indicates whether or not the event occurred, the number of times the event occurred, and the age of first occurrence. In this study, the number of types of events endorsed on the THQ was summed to reflect the degree of prior trauma experienced by participants.
Secondary Outcomes
Depression
The Beck Depression Inventory (BDI; Beck, Rush, Shaw, & Emery, 1979) was used to assess severity of depression symptoms over the past week. The BDI is a 21-item self-report measure of characteristic attitudes and symptoms of depression with established reliability and validity and had excellent internal consistency in the current study (α = .89)
Empowerment
The Personal Progress Scale-Revised (PPS-R) (Johnson et al., 2005) was used to measure women’s empowerment. The PPS-R is a 28 item self-report measure on which participants rated the extent to which they agreed or disagreed with each item on a 7-point Likert scale and then summed to create a total score. The PPS-R assesses 10 broad outcomes of feminist therapies including positive self-evaluation and self-esteem, a favorable comfort distress ratio, gender-role and cultural identity awareness, a sense of personal control/self-efficacy, self-nurturance and self-care, effective problem-solving skills, competent use of assertiveness skills, effective access to multiple economic, social, and community resources, gender and cultural flexibility, and socially constructive activism. Previous research with the PPS-R has shown the measure to have good reliability and validity (Johnson et al., 2005). Further, the measure has shown excellent discriminate validity as it was able to distinguish between victims of IPV with and without PTSD in previous research (Johnson et al., 2005). Alpha in this study was .80.
Resource Loss
The Conservation of Resources–Evaluation (COR-E) (Hobfoll & Lilly, 1993) is a 74 item self-report measure that assesses the degree to which participants experienced loss in material, energy, work, interpersonal, family, and personal resources in the past month. Each item of the COR-E is rated on a 3-point scale ranging from 0 (no threat or loss) to 2 (a great deal of threat or loss). The COR-E has demonstrated excellent validity (Hobfoll & Lilly, 1993; Ironson et al., 1997), and had high reliability in this study (α = .96).
Social Support
The Inventory of Socially Supportive Behaviors (ISSB) (Barrera, Sandler, & Ramsay, 1981) is a 40-item self-report measure that assesses the frequency of material aid, behavioral assistance, intimate interactions, guidance, feedback and positive social interactions over the past month. Items are rated on a 5-point scale. The ISSB has established reliability and validity and excellent reliability within the current sample (α = .95).
Treatment Credibility/Satisfaction with Treatment
Treatment Credibility
The perceived credibility of HOPE was rated on 4-item measure frequently employed in treatment research (Devilly & Borkovec, 2000). Items assessing how logical they found HOPE, how successful they believed HOPE will be in addressing their PTSD and other problems, and their confidence in recommending HOPE were rated on a 9-point scale ranging from 0 to 8. Similar scales have demonstrated high internal consistency and test-retest reliability (Devilly & Borkovec, 2000). Alpha in this instance was .94.
Client Satisfaction
A 14-item version of the Client Satisfaction Questionnaire (CSQ; Attkisson & Zwick, 1982) was used to assess participant overall satisfaction with HOPE. The CSQ is a self-report measure with established reliability and validity that asks participants to rate their degree of satisfaction on a 4-point scale with HOPE on a variety of dimensions (e.g., quality of service, amount of help received, convenience, confidentiality). The CSQ demonstrated sound reliability in the current study (α = .89).
Adherence and Competence
Adherence and competence was rated by study therapists who did not conduct the session being rated. The HOPE Adherence and Competence Scales (HOPE ACS) contains five items assessing therapist general skillfulness (e.g., empathy, efficient use of time) on a 6-point scale ranging from not present (0) to excellent (5). Additionally, for 15 general (e.g., adherence to HOPE hierarchy, discussion of accomplishments) and 18 module specific (i.e., psychoeducation regarding abuse and PTSD, education and application of cognitive restructuring techniques) HOPE strategies, the presence or absence of each strategy, protocol adherence (i.e., not enough (−1) to too much (1)), and quality (i.e., poor (1) to excellent (5)) were rated. Finally, therapist overall adherence and competence were rated on 5 point scales. Internal consistency of both the HOPE adherence scale (α = .95) and HOPE competence scale (α = .80) were excellent. Of the 27 sessions rated for adherence and competence, 13 were rated by a 2nd rater, in order to assess inter-rater reliability. Average measure reliability (intraclass correlation) was also good for adherence (.92) and adequate for competence (.75) ratings.
Treatment
Standard Shelter Services (SSS)
All participants received SSS. SSS included case management, a supportive milieu environment, and attendance of educational groups offered through the shelter (i.e., parenting & support groups). No therapy was offered through SSS.
HOPE
(Johnson & Zlotnick, 2006, 2009; Johnson, Zlotnick, & DeLambo, 2004). Participants received a maximum of 12 sessions of HOPE while in shelter over a maximum of 8-weeks. All sessions occurred at shelter and childcare was provided. Sessions were offered bi-weekly and lasted approximately 1–1.5 hours. HOPE session structure is the same for each session: (a) checking in regarding safety and progress on accomplishments (i.e., homework), (b) agenda setting, (c) discussion of module-specific information, and (d) negotiating accomplishments for the next session. A hierarchy of target behaviors (i.e., the HOPE hierarchy) was developed to guide the content of treatment within and across sessions: (a) immediate physical and emotional risks, (b) PTSD symptoms, behaviors, and cognitions that interfere with (b1) achieving shelter and treatment goals and (b2) quality of life, and (c) post-shelter goals and safety. This hierarchy determines the order of specific modules over the course of therapy (e.g., safety discussed before skill specific modules), as well as in prioritizing safety issues within each session (e.g., new material is not presented until safety issues have been addressed).
HOPE clients are provided with an “empowerment tool-box” that includes an exhaustive list of positive coping strategies across three broad areas: (a) establishing safety and empowerment (e.g., take back your power, don’t spin your wheels), (b) managing symptoms (e.g., rethink, self-soothe), and (c) improving their relationships (e.g., give a little trust at a time, focus on safe and healthy relationships). Participants are encouraged to use this toolbox to better cope with their PTSD symptoms. Each empowerment tool is then addressed more specifically in one of the core modules. Core modules cover engagement and goal setting, psychoeducation about abuse and PTSD, safety planning, empowerment, establishing trust, cognitive-restructuring, managing triggers, self-soothing, establishing boundaries, anger management, and establishing long-term support. Throughout HOPE, clients are encouraged to identify the aspects of any threats to their physical and emotional safety that are within their control and to utilize the empowerment toolbox to manage these threats. Participants identify and prioritize their personal goals during the first two sessions, and these goals are used in conjunction with the HOPE hierarchy to individualize treatment and to further engage and empower women in the treatment. Accomplishments (i.e., homework) are assigned between sessions to assist women in applying the empowerment tools to their every-day lives. Beginning sessions (i.e., the first five) tend to focus on psychoeducation regarding interpersonal violence, PTSD, safety planning, and empowerment. Later sessions of HOPE incorporate established CBT skills to manage PTSD and its associated features (e.g., cognitive restructuring, self-soothing, assertiveness training).
Therapist Training
The first author, as well as five additional therapists who held a minimum of a master’s degree in psychology or counseling and had at least one year of prior experience in working with traumatized populations, conducted HOPE. HOPE training included a 12-hour workshop with the first author that provided an overview of the HOPE theoretical approach and specific instructions on how to deliver each module. All therapists were supervised weekly by the first author. Supervision by the first author included discussion of specific HOPE cases, audio-tape review, role-plays, and discussion of adherence and competence ratings.
Statistical Methods
Hierarchical Linear Modeling (HLM) was used to evaluate continuous outcomes. Data were analyzed using HLM 6 (Raudenbush, Bryk, Cheong, Congdon, & duToit, 2004). We chose HLM as our primary analytic strategy because it addresses problems associated with missing data, correlated repeated measures for each participant, and variable measurement in assessment intervals occurring as a result of variable lengths of shelter stay (Raudenbush et al., 2004). For each outcome, two analyses were run. Intent to treat (ITT) analyses included all participants regardless of the number of HOPE sessions completed. Analyses were also conducted with participants who completed a minimal amount of HOPE (≥ 5 sessions) and completed all follow-up assessments (see Figure 1). Attendance of five sessions was chosen for the minimal attendance (MA) analyses because women who completed at least 5 sessions would have completed most of the core and unique components of HOPE (i.e., psychoeducation, safety planning, and empowerment strategies). For each model, time was entered un-centered as the level one predictor. Consistent with previous research (e.g., Monson et al., 2006) and our inspection of data, the variable of time (in days) was log-transformed to represent greatest improvements early in the post-shelter (PS) phase (i.e., curvilinear effects). Both treatment group (i.e., HOPE vs control, dummy coded) and current Major Depression Disorder (MDD) status (MDD vs no MDD, dummy coded, entered as a covariate; see below) were entered un-centered as the level two predictors. In addition to HLM, effect sizes (i.e., Cohen’s d) were computed for each continuous outcome at 1-week PS while controlling for baseline outcome levels. Additionally, using the procedures described by Jacobson and Traux (1991), the reliable change index was computed for CAPS scores at 1-week PS in order to assess whether the change in PTSD symptoms experienced by HOPE participants was indeed meaningful. Finally, chi-squares, odds ratios (OR), and relative risk (RR) values were computed for binary outcomes.
Results
Study Sample
Figure 1 shows the participant flow from phone screen through 6-month PS follow-up. A total of 70 women met study criteria and were randomized into the study. A summary of sample characteristics is found in Table 1. Participants randomized to the control condition had a significantly higher rate of comorbid MDD than did those randomized to HOPE, χ2 (1) = 10.94, p < .01; therefore presence of MDD was controlled for in analyses (see above). No other significant differences emerged between the two treatment groups on any demographic, diagnostic, trauma/IPV characteristics at baseline, nor on the length of shelter stay, occurrence of contact with abuser, or receipt of therapy over the follow-up period (all p’s > .05).
Table 1.
Sample Characteristics by Treatment Group (N= 70)
| Variable | Total (N = 70) | HOPE (n = 35) | Control (n = 35) |
|---|---|---|---|
| Age | 32.55 (8.00) | 31.74 (9.12) | 33.34 (6.74) |
| Race/Ethnicity | |||
| African American | 35 (50.0) | 17 (48.6) | 18 (51.4) |
| Caucasian | 30 (42.9) | 17 (48.6) | 13 (37.1) |
| Other race | 5 (7.1) | 1 (2.9) | 4 (11.4) |
| Hispanic | 3 (4.3) | 1 (2.9) | 3 (5.7) |
| Highest Education Obtained | |||
| Less than high school | 19 (27.1) | 9 (25.7) | 10 (28.6) |
| High school/GED | 16 (22.9) | 7 (20.0) | 9 (25.7) |
| Completed some college | 30 (42.9) | 14 (40.0) | 16 (45.7) |
| Graduated from college | 5 (7.1) | 5 (14.3) | 0 (0) |
| Public Assistance | 46 (65.7) | 20 (57.1) | 26 (74.3) |
| Employed | 19 (27.1) | 13 (37.1) | 6 (17.1) |
| Have children | 63 (90.0) | 30 (85.7) | 33 (94.3) |
| Cohabitated/married to abuser | 53 (75.7) | 25 (71.4) | 28 (80.0) |
| Have restraining order | 26 (37.1) | 14 (40.0) | 12 (34.3) |
| IPV-related PTSD Statusa | |||
| PTSD | 61 (87.1) | 31 (88.6) | 30 (85.7) |
| Subthreshold PTSD | 9 (12.9) | 4 (11.4) | 5 (14.3) |
| Current Comorbid Psychiatric Disorders | |||
| Major Depression**,b | 67.1 (47) | 48.6 (17) | 85.7 (30) |
| Substance Use Disorder | 11.4 (8) | 5.7 (2) | 17.1 (6) |
| Other Anxiety Disorder | 18 (51.4) | 16 (45.7) | 34 (48.6) |
| On Psychotropic Medicationsa | 15 (21.4) | 7 (20.0) | 8 (22.9) |
| IPV in month prior to shelter | |||
| Psychological | 70 (100) | 35 (100) | 35 (100) |
| Physical | 65 (92.9) | 31 (88.6) | 34(97.1) |
| Sexual | 47 (67.1) | 23 (65.7) | 24 (68.6) |
| Prior lifetime IPV | 51 (72.9) | 26 (74.3) | 25 (71.4) |
| No of types of prior lifetime trauma other than index IPV | 6.31 (3.98) | 6.86 (3.96) | 5.77 (3.98) |
| Days in shelter at baseline | 15.00 (9.73) | 15.60 (6.24) | 14.40 (12.35) |
| Length of shelter stayc | 73.18 (60.80) | 79.12 (62.74) | 67.24 (59.12) |
| Contact with abuser over study periodd | 59 (90.77) | 30 (93.75) | 29(87.88) |
| Received psychotherapy post-shelterd | 27 (41.5) | 14 (43.8) | 13 (39.4) |
Note. Values are either reported as M (SD) or n (%).
used in randomization stratification.
used as covariate in analyses.
n = 69.
n = 65.
p < .01.
Treatment Attendance and Study Retention
Participants in HOPE attended 0–12 sessions (M = 6.8, SD = 4.3). All but one participant (97.1%) attended at least one session of HOPE, with 22 (62.9%) attending ≥ 5 sessions, and 9 (25.7%) attending all 12 sessions. Two (6.7%) participants withdrew from the treatment phase (i.e., refused further treatment while still in shelter), but were still followed post-shelter. The remaining 24 participants who did not complete all 12 sessions (68.6%) left shelter prior to completing HOPE. Participants who stayed in shelter long enough to complete HOPE tended to receive a significant dose of HOPE (M = 10.31, SD = 2.66). Participants cancelled between 0 and 3 sessions (M = 0.60, SD = 0.77) and no-showed between 0 and 11 sessions (M = 1.91, SD = 2.48). No significant demographic differences were found between participants who completed a minimal dose of treatment (i.e., ≥5 sessions) and those who did not (all p’s >.05).
Retention rates for each follow-up time point are as follows: 97.1% at one-week PS (n = 68), 94.3% at 3-months PS (n = 66), and 94.6% at 6-months PS (n = 66). Data for all follow-up periods was completed for 92.9% of participants (n = 65). See Figure 1 for retention numbers by treatment group. Participants lost to follow-up were less likely to receive public assistance (20% of those lost) than were participants retained through 6-month follow-up (69.2% of those retained) (χ2 (1) = 4.99, p < .05). No other differences were found between participants lost to follow-up and those retained throughout the entire follow-up period.
Treatment Delivery
Dichotomous adherence ratings across the 15 general and 18 module specific items on the HOPE ACS were summed to compute the average percentage of adherence to specific HOPE strategies. As such, adherence was good, with an average of 90.8% of HOPE strategies delivered as prescribed by the manual. Ratings on the item measuring overall therapist adherence on a 5-point scale was also strong 4.28 (SD = .84). The average quality rating (5-point scale) for each HOPE strategy was summed across each of the 15 general and 18 module specific items on HOPE ACS to assess competence. Competence in delivering HOPE was good, with an average quality rating of 3.92 (SD = .57). Ratings on the item measuring overall therapist competence on a 5-point scale was also good, with an average rating of 4.2 (SD = .87). Therapist general skillfulness was also rated high, with an average rating of 4.42 (SD = .53) on a rating scale from 0–5.
Adverse Events
There were no unanticipated-research-related serious adverse events (SAE’s) that required participants to be removed from the trial. There were 7 hospitalizations (5 medical, 2 substance related), and 4 life-threatening traumatic experiences (2 abuse-related) reported over the course of the 6-month follow-up period.
Treatment Outcomes
PTSD
No significant differences were found for PTSD diagnostic status in the ITT sample (p > .05). Descriptive analyses and effect sizes for CAPS scores in the ITT sample are found in Table 2. HLM analyses with the ITT sample yielded a significant effect for time, χ2 (67) = 118.75, p <.0001, on total CAPS scores in which PTSD severity decreased over time. No significant treatment effect was found (p > .05). When looking at PTSD symptoms by factors (i.e., re-experiencing, effortful avoidance, emotional numbing, and arousal), a significant treatment effect was found for emotional numbing symptoms, t (67) = −2.046, p <.05, in which participants in HOPE experienced less severe emotional numbing symptoms over follow-up than did participants in the control group. No significant treatment effects were found for re-experiencing, effortful avoidance, or arousal symptoms (all p’s > .05).
Table 2.
Descriptive analyses for Primary and Secondary Outcomes for Intent to Treat Sample (n = 70)
| HOPE | Control | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline M (SD) n=35 |
1-wk PS M (SD) n=34 |
3-mo PS M (SD) n=33 |
6-mo PS M (SD) n=32 |
Baseline M (SD) n=35 |
1-wk PS M (SD) n=34 |
3-mo PS M (SD) n=33 |
6-mo PS M (SD) n=34 |
Effect Size1 (95% CI) n=68 |
|
| CAPS | 53.34 (24.29) |
24.76 (18.47) |
21.15 (24.79) |
18.62 (18.84) |
62.69 (25.38) |
42.38 (29.33) |
31.27 (22.01) |
26.56 (25.83) |
.59 (−6.57, 7.76) |
| CAPS Re-experiencing |
15.94 (9.00) |
6.79 (7.75) |
5.27 (7.69) |
4.44 (7.50) |
20.60 (7.89) |
9.79 (9.56) |
7.03 (7.22) |
6.38 (8.67) |
.17 (−2.65, 2.99) |
| CAPS-Effortful Avoidance |
7.71 (3.90) |
3.09 (3.48) |
2.85 (4.03) |
2.19 (3.08) |
8.54 (4.40) |
6.15 (5.31) |
4.12 (4.20) |
3.15 (3.39) |
.67 (−1.57, 2.92) |
| CAPS-Emotional Numbing* |
11.51 (9.05) |
6.65 (6.96) |
5.12 (7.98) |
3.81 (5.32) |
14.11 (9.37) |
10.71 (8.91) |
8.94 (8.20) |
8.68 (9.71) |
.41 (−3.26, 4.08) |
| CAPS Arousal |
18.17 (8.75) |
8.24 (7.19) |
7.91 (9.13) |
8.19 (8.18) |
19.43 (9.73) |
15.74 (10.57) |
11.18 (8.11) |
8.35 (10.26) |
.84 (−1.87, 3.56) |
| BDI** | 24.17 (9.10) |
10.68 (8.80) |
11.61 (10.69) |
8.16 (8.62) |
21.89 (11.54) |
18.53 (12.12) |
15.73 (10.90) |
12.85 (11.87) |
.94 (−2.21, 4.10) |
| PPS* | 120.23 (20.34) |
133.32 (22.16) |
136.15 (22.25) |
138.84 (24.32) |
115.97 (19.19) |
121.35 (12.12) |
125.06 (21.65) |
127.09 (23.12) |
.49 (−7.04, 6.06) |
| COR | 63.97 (28.72) |
37.18 (38.07) |
33.06 (29.09) |
29.63 (33.34) |
68.83 (33.98) |
44.82 (37.13) |
54.09 (36.22) |
39.00 (34.95) |
.16 (−12.10, 12.42) |
| ISSB* | 94.34 (29.46) |
101.38 (27.86) |
90.79 (37.15) |
88.66 (36.38) |
87.57 (27.77) |
81.44 (29.42) |
76.52 (29.06) |
78.77 (31.06) |
.65 (−7.67, 8.96) |
Note. Mo=month; PS=post-shelter.
Cohen’s d calculated with adjusted means at 1-week post-shelter controlling for baseline scores. Positive values reflect greater improvement in HOPE relative to Control.
p<.05.
p<.01.
Chi-Square analyses evaluating PTSD diagnostic status in the MA sample were only significant at 3-months PS, χ2 (1) = 4.69, p <.05, in which participants in HOPE (15.8%) were significantly less likely to meet criteria for PTSD relative to controls (45.5%), OR = 4.44, 95% CIs [1.08–18.22], RR = 2.88, 95% CIs [.95–8.68]. Descriptive analyses and effect sizes for CAPS scores in the MA sample are found in Table 3. HLM analyses with the MA sample yielded a significant effect for time, χ2 (49) = 73.54, p <.05, in that participants experienced less severe PTSD symptoms over time. The treatment effect approached significance, t (49) −1.70, p = .094, in which participants who attended a minimal number of sessions of HOPE reported less severe PTSD symptoms over follow-up than did participants in the control group. Further analyses with specific PTSD factors yielded significant treatment effects for effortful avoidance symptom severity, t (49) = −2.50, p < .05 and arousal symptom severity, t (49) = −2.04, p <.05, in which participants who received a minimum dose of HOPE experienced less severe effortful avoidance and arousal symptoms over the follow-up period relative to women in the control group. The treatment effect for emotional numbing symptom severity approached significance, t(49) = −1.810, p = .076. No significant effect was found for re-experiencing symptom severity (p >.05).
Table 3.
Descriptive analyses for Primary and Secondary Outcomes for Minimal Attendance (i.e. ≥5 sessions) Sample (n=52)
| HOPE | Control | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline M (SD) n=19 |
1-wk PS M (SD) n=19 |
3-mo PS M (SD) n=19 |
6-mo PS M (SD) n=19 |
Baseline M (SD) n=33 |
1-wk PS M (SD) n=33 |
3-mo PS M (SD) n=33 |
6-mo PS M (SD) n=33 |
Effect Size1 (95% CI) n=52 |
|
| CAPS | 50.00 (22.61) |
21.16 (17.17) |
16.32 (20.20) |
14.79 (16.63) |
61.85 (25.66) |
40.97 (28.59) |
31.27 (22.01) |
26.82 (26.18) |
.63 (−6.79, 10.48) |
| CAPS Re-experiencing |
14.32 (7.37) |
5.68 (7.99) |
4.05 (6.98) |
3.63 (6.54) |
20.30 (8.03) |
9.00 (8.50) |
7.03 (7.22) |
6.55 (8.75) |
.12 (−2.61, 3.78) |
| CAPS-Effortful Avoidance* |
8.68 (3.94) |
2.37 (3.64) |
1.89 (3.73) |
1.63 (2.17) |
8.42 (4.42) |
6.15 (5.39) |
4.12 (4.20) |
3.03 (3.37) |
.83 (−1.59, 3.25) |
| CAPS-Emotional Numbing |
8.74 (7.91) |
6.58 (7.80) |
3.89 (7.05) |
2.00 (3.21) |
13.91 (9.38) |
10.55 (9.00) |
8.94 (8.20) |
8.79 (9.84) |
.19 (−3.63, 4.06) |
| CAPS Arousal** |
18.26 (9.11) |
6.53 (5.75) |
6.47 (8.26) |
7.53 (9.03) |
19.21 (9.73) |
15.27 (10.38) |
11.18 (8.11) |
8.45 (10.40) |
1.05 (−1.72, 4.70) |
| BDI* | 20.79 (6.65) |
8.89 (8.45) |
11.95 (10.11) |
7.21 (8.59) |
21.82 (11.62) |
18.67 (12.28) |
15.73 (10.90) |
13.24 (11.83) |
.96 (−2.40, 5.38) |
| PPS | 122.95 (16.98) |
131.68 (25.56) |
135.74 (20.75) |
140.95 (26.79) |
117.06 (18.70) |
121.03 (21.77) |
125.06 (21.65) |
127.42 (23.40) |
.34 (−7.34, 8.90) |
| COR | 56.58 (27.49) |
30.26 (41.13) |
31.74 (29.76) |
23.53 (25.52) |
68.30 (32.97) |
43.67 (37.08) |
54.09 (36.22) |
40.12 (34.87) |
.24 (−12.43, 17.01) |
| ISSB | 106.47 (27.68) |
102.16 (31.94) |
83.21 (33.17) |
79.16 (35.07) |
86.48 (28.08) |
80.39 (29.22) |
76.52 (29.06) |
79.16 (35.07) |
.35 (−8.75, 10.90) |
Note. Mo=month; PS=post-shelter.
Cohen’s d calculated with adjusted means at 1-week PS controlling for baseline scores. Positive values reflect greater improvement in HOPE relative to Control.
p<.05.
p<.01.
The reliable change index as outlined by Jacobson and Truax (1991) was calculated for CAPS scores at 1-week PS for both the ITT and MA samples. Using a 95% confidence interval, a change of more than 21 points on the CAPS is required to indicate reliable change in the ITT sample. Using this criterion, 63.2% of participants randomized to HOPE achieved reliable change. For the MA sample, a change of 22 points on the CAPS is required to indicate reliable change. Of the MA participants, 64.7% achieved reliable change.
Re-abuse
In both the ITT and MA samples, Chi-Square analyses found significant differences in re-abuse rates over the 6-month follow-up period, χ2 (1) = 8.68, p < .01 & χ2 (1) = 15.70, p < .0001, respectively. In the ITT sample, participants in HOPE (46.9%) were significantly less likely to report re-abuse than were control participants (81.8%), OR = 5.1, 95% CIs [1.66–15.70], RR = 1.75, 95% CIs [1.17–2.61]. In the MA sample, participants in HOPE (26.3%) were also significantly less likely to report re-abuse than were control participants (81.8%), OR= 12.6, 95% CIs [3.26–48.65], RR = 3.11, 95% CIs [1.44–6.71].
Secondary Outcomes
Descriptive analyses and effect sizes for all secondary outcomes can be found in Table 2 for the ITT sample and Table 3 for the MA sample. HLM analyses with the BDI for the ITT sample yielded a significant effect of time, in which participants reported fewer depressive symptoms over the course of the follow-up, χ2 (67) = 117.71, p < .0001. A significant treatment effect was also found, t (67) = −3.13, p <.01, in which participants in HOPE reported fewer depression symptoms over follow-up relative to participants in the control group (see Table 2). Analyses with the MA sample were similar in that a significant treatment effect was also found, t (49) = −2.510, p < .05, in which MA participants reported fewer depression symptoms over follow-up relative to participants in the control condition.
HLM analyses with the ITT sample and PPS scores revealed a significant effect of time, χ2 (67) = 99.96, p < .01, in which participants scored higher on empowerment over the follow-up period. A significant treatment effect was also found, t (67) = 2.09, p < .05, in which women randomized to HOPE reported higher levels of empowerment relative to controls over the follow-up period. No significant treatment effect was found for empowerment in the MA sample. HLM analyses with both the ITT sample and the MA sample with scores on the COR-E found no significant effect of time or treatment group (all p’s > .05). HLM analyses with the ITT sample and scores on the ISSB revealed a significant effect of time, χ2 (67) = 95.19, p < .05, in which participants reported greater degree of social support over the follow-up period. A significant treatment effect was also found, t (67) = 2.11, p < .05, in which women in HOPE reported more social support over the follow-up period than did women in the control group. However, no significant effect of time or treatment group was found in the MA sample (all p’s > .05).
Treatment Credibility and Satisfaction with Treatment
Average credibility rating (n = 29) on an 8-point scale was 6.78 (SD = 1.42). Average satisfaction ratings on the 4-point scale of the CSQ (Attkisson & Zwick, 1983) was 3.4 at 1-week PS (n = 32), 3.5 at 3-month PS (n = 31), and 3.4 at 6-month PS (n = 30).
Discussion
This study represents the first RCT of residents of battered women shelters with PTSD or subthreshold PTSD. Results suggest that HOPE may be a promising treatment for recent IPV victims in shelter, but that some modifications may be required to improve HOPE’s impact on PTSD. Results support the initial feasibility and acceptability of a first-stage, present-centered, structured, CBT for sheltered women with IPV-related PTSD. Participants in HOPE found the treatment credible, expressed a high degree of satisfaction with treatment, and the treatment drop-out rate was low (6.67%). However, most participants left shelter prior to completing HOPE (62.9%), with many participants leaving before receiving a minimal dose (33.3%). We attempted to offer treatment more frequently to increase the likelihood of participants receiving an adequate dose, however, residents’ competing demands made more frequent sessions impossible. Therefore, treatment may need to continue after shelter in order for women to receive a therapeutic dose of treatment.
Findings suggest that HOPE may be significantly associated with victims’ increased safety after leaving shelter. Women who only received SSS were 12 times more likely to be re-abused relative to participants who received a minimal dose of HOPE. Targeting PTSD symptoms may be one useful strategy in reducing the risk of re-abuse in IPV victims with PTSD (Krause et al., 2006). However, other components of HOPE (e.g., emphasis on empowerment and resource acquisition) may also explain findings of reduced re-abuse in HOPE participants. Future research is needed to confirm these findings, examine if they are sustained beyond 6-months post shelter, and determine if this apparent reduced risk of re-abuse is a result of reductions in PTSD symptoms and/or depression, increased empowerment, and/or more effective use of resources. Further, future research should investigate whether the reduced risk for re-abuse varies for different types of violence (e.g., physical, sexual, emotional).
Although the present study did not find that HOPE reduced overall PTSD severity, initial findings suggest that HOPE relative to the control condition significantly reduced effortful avoidance, emotional numbing, and arousal symptom severity. Specifically, participants randomized to HOPE experienced a significant decline in emotional numbing symptoms after leaving shelter relative to control participants. Further, participants who completed a minimal dose of HOPE experienced significantly less severe effortful avoidance and arousal symptoms over the 6-month follow-up relative to control participants. HOPE’s lack of effect on PTSD re-experiencing symptoms may be attributable to the large number of women in HOPE who still have contact with their abuser (87.9%; see Table 1) and the likelihood that such contact may trigger re-experiencing symptoms. HOPE participants may have, however, learnt more effective coping strategies (i.e., rather than avoidance strategies) to manage these re-experiencing symptoms, as well as their symptoms of arousal.
Although participants who received a minimal dose of HOPE were significantly less likely to meet criteria for PTSD three months PS than were control participants and medium effect sizes were found for severity of PTSD symptoms 1-week PS, with women in HOPE experiencing less severe PTSD, these improvements relative to the control were not statistically significant over time. The lack of significant findings in PTSD symptom severity may be a result of participants’ ongoing re-experiencing symptoms, continued safety concerns and contact with their abuser, and inability to complete a significant dose of HOPE prior to leaving shelter. Further, most participants reported a significant trauma history prior to their IPV (see Table 1), and HOPE may not have generalized to address PTSD symptoms from these events. Alternatively, the CBT components of HOPE specifically targeting PTSD symptoms may need to be expanded in order for HOPE to have a greater impact on IPV-related PTSD. Consistent with Herman’s (1992) model this first stage treatment may help to stabilize IPV victims, preparing them for the next stage of treatment in which exposure-based treatments may be warranted. Further research is needed to fully understand the impact of HOPE on IPV victims’ PTSD and examine if extending HOPE after shelter departure improves outcomes.
Although HOPE was not designed to specifically target depressive symptoms, this study found that HOPE participants reported significantly less depressive symptoms over the follow-up period than did controls, regardless of the number of sessions received. A large effect size was found for depression severity, even when controlling for MDD status. Since HOPE addresses maladaptive cognitions, a well-known treatment intervention for depression, it is possible that the cognitive strategies used in HOPE are efficacious for comorbid depression. Consistent with the treatment goals of HOPE, this study found that HOPE participants reported higher levels of empowerment and more social support over the course of the follow-up than did women in the control group. Taken together, these findings suggest that participation in HOPE is associated with significant treatment gains, in that women who receive HOPE are more likely to establish long-term safety, experience fewer depressive symptoms, and increased access to personal (e.g., empowerment) and social (e.g., social support) resources. Future research is obviously needed to confirm these findings.
Although preliminary data suggest that residents of battered women shelters with full or sub-threshold PTSD fair generally better when participating in HOPE than standard shelter services alone, findings also clearly suggest that HOPE participants continue to have significant symptoms and ongoing concerns after leaving shelter. Almost all women (90.77%; see Table 1) had contact with their abuser during the course of the study, and nearly half (46.9%) of the women in HOPE reported incidents of further abuse after leaving shelter. Moreover, nearly 40% of HOPE participants still met diagnostic criteria for PTSD one-week after leaving shelter. Taken together, these findings strongly suggest that IPV victims who seek shelter require services, including mental health treatment, after leaving shelter. Perhaps, an expanded version of HOPE that includes sessions after leaving shelter may maximize treatment benefits.
Results of this study are preliminary and obviously must be viewed with caution. Strengths of this study include the use of a RCT design with an ethnically diverse sample, excellent retention rate, and use of reliable and valid measures of PTSD and IPV. Further, HOPE was manualized (Johnson et al., 2004) and measures were included to assure that the treatment protocol was delivered in an adherent and competent manner. Weaknesses of this study include the relatively small sample size and resulting high variability in effect size estimates that can result in small pilot studies (Kraemer, Mintz, Noda, Tinklenberg, & Yesa, 2006). Also, since subthreshold PTSD was used as inclusion criteria, our population may not be representative of that used in other clinical trials of PTSD. Further, given funding restrictions, we were unable to assure that interviewers were masked to participants’ treatment condition and study therapists were used to rate adherence and competence rather than outside raters, which could significantly bias findings. Additionally, future research is needed comparing HOPE to a credible attention control condition in order to determine whether “active ingredients” specific to HOPE are responsible for observed treatment effects over factors common to psychotherapy in general. Further, research with a longer follow-up period is needed to evaluate the durability of treatment effects. It is also unknown whether findings generalize to IPV victims who do not seek shelter. Regardless, results of this study are promising, suggesting that supplementing standard shelter services with HOPE may improve the safety and psychological outcomes of victims of IPV who seek shelter.
Acknowledgments
This work was supported by NIMH grant K23 MH067648. We would like to thank Cynthia Cluster, Keri Pinna, Kristen Walter, Kirsten DeLambo, Holly Harris, Michelle Taylor, Christina Kraft, Brigette Shy, and the staff and residents of the Battered Women’s Shelter of Summit and Medina Counties for their assistance in data collection and/or provision of therapy. We would also like to thank Patrick Palmieri for his statistical assistance on this study.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
Contributor Information
Dawn M. Johnson, University of Akron, Department of Psychology, University of Akron, Akron, Ohio
Caron Zlotnick, Butler Hospital and Brown University, Department of Psychiatry and Human Behavior, Providence, Rhode Island.
Sara Perez, Cleveland Veteran’s Administration Hospital, Department of Psychology, Brecksville, Ohio.
References
- Attkisson CC, Zwick R. The client satisfaction questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning. 1982;5:233–237. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- Barrera M, Sandler IN, Ramsay TB. Preliminary development of a scale of social support: Studies on college students. American Journal of Community Psychology. 1981;9:435–447. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York: Guildford Publications; 1979. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloeupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Hickling EJ, Devineni T, veazey CH, Galovski TE, Mundy E, Malta LS, Buckley TC. A controlled evaluation of cognitive behavioral therapy for posttraumatic stress in motor vehicle accident survivors. Behaviour Research and Therapy. 2003;41:79–96. doi: 10.1016/s0005-7967(01)00131-0. [DOI] [PubMed] [Google Scholar]
- Breiding MJ, Black MC, Ryan GW. Prevalence and risk factors of intimate partner violence in eighteen U.S. states/territories, 2005. American Journal of Preventative Medicine. 2008;34:112–118. doi: 10.1016/j.amepre.2007.10.001. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Harvey AG, Dang ST, Sackville T, Basten C. Treatment of acute stress disorder: A comparison of cognitive-behavioral therapy and supportive counseling. Journal of Consulting and Clinical Psychology. 1998;66:862–866. doi: 10.1037//0022-006x.66.5.862. [DOI] [PubMed] [Google Scholar]
- Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavior Therapy. 2000;31:73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38:319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, Feeny NC, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73:953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JB, Benjamin LS. User’s guide for the structured clinical interview for DSM-IV axis I disorders, research version. NY: New York State Psychiatric Institute, Biometrics Research Department, NY; 1996. [Google Scholar]
- Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. Journal of Family Violence. 1999;14:99–132. [Google Scholar]
- Green BL. Psychometric review of Trauma History Questionnaire (self-report) In: Stamm BH, Varra EM, editors. Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran; 1996. [Google Scholar]
- Herman JL. Trauma and recovery. New York: Basic Books; 1992. [Google Scholar]
- Hien DA, Wells EA, Jiang H, Suarez-Morales L, Campbell ANC, Cohen LR, Miele GM, et al. Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. Journal of Consulting and Clinical Psychology. 2009;77:607–619. doi: 10.1037/a0016227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobfoll SE, Lilly RS. Resource conservation as a strategy for community psychology. Journal of Community Psychology. 1993;21:128–148. [Google Scholar]
- Ironson G, Wynings C, Schneiderman N, Baum A, Rodriguez M, Greenwood D, Benight C, Antoni M, LaPierre P, Huang H, Klimas N, Fletcher MA. Posttraumatic stress symptoms, intrusive thoughts, loss, and immune function after Hurricane Andrew. Psychosomatic Medicine. 1997;59:129–141. doi: 10.1097/00006842-199703000-00003. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Johnson DM, Worell J, Chandler RK. Assessing psychological health and empowerment in women: The Personal Progress Scale Revised. Women and Health. 2005;41:109–129. doi: 10.1300/J013v41n01_07. [DOI] [PubMed] [Google Scholar]
- Johnson DM, Zlotnick C. HOPE for battered women with PTSD in domestic violence shelters. Professional Psychology: Research and Practice. 2009;40:234–241. doi: 10.1037/a0012519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson DM, Zlotnick C. A cognitive-behavioral treatment for battered women with PTSD in shelters: Findings from a pilot study. Journal of Traumatic Stress. 2006;19:1. doi: 10.1002/jts.20148. 6559-564. [DOI] [PubMed] [Google Scholar]
- Johnson DM, Zlotnick C, DeLambo K. Helping to Overcome PTSD through Empowerment (HOPE): Treatment manual. 2004 Unpublished manuscript. [Google Scholar]
- Johnson DM, Zlotnick C, Perez S. The relative contribution of abuse severity and PTSD severity on the psychiatric and social morbidity of battered women in shelters. Behavior Therapy. 2008;39:232–241. doi: 10.1016/j.beth.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Jones L, Hughes M, Unterstaller U. Post-traumatic stress disorder (PTSD) in victims of domestic violence: A review of the research. Trauma, Violence, and Abuse. 2001;2:99–119. [Google Scholar]
- Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry. 2006;63:484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- Krause ED, Kaltman S, Goodman LA, Dutton MA. Role of distinct PTSD symptoms in intimate partner reabuse: A prospective study. Journal of Traumatic Stress. 2006;19:507–516. doi: 10.1002/jts.20136. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Hill EE, Owens JA, Iannce-Spencer C, McCaig MA, Tremayne KJ, Williams P. Cognitive trauma therapy for battered women with PTSD (CTT-BW) Journal of Consulting and Clinical Psychology. 2004;72:3–18. doi: 10.1037/0022-006X.72.1.3. [DOI] [PubMed] [Google Scholar]
- McCann L, Sakheim DK, Abrahamson DJ. Trauma and victimization: A model of psychological adaptation. Counseling Psychologist. 1988;39:1–17. [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2006;74:898–907. doi: 10.1037/0022-006X.74.5.898. [DOI] [PubMed] [Google Scholar]
- National Coalition Against Domestic Violence. Family Violence Prevention and Services Act: Funding need: $175 million. 2008 Retrieved June 18, 2008, from http://www.ncadv.org/files/statecomparisonFVPSA.pdf. [Google Scholar]
- Raudenbush S, Bryk A, Cheong YF, Congdon R, du Toit M. HLM6: Linear and Nonlinear Modeling. Lincolnwood, IL: Scientific Software International, Inc; 2006. [Google Scholar]
- Resick PA, Uhlmansiek MO, Clum GA, Galovski TE, Scher CD, Young-Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology. 2008;76:243–258. doi: 10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein M, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: Findings from a community survey. American Journal of Psychiatry. 1997;154:1114–1119. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, DelBoca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol, Supplement no. 12. 1994:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Weathers FW, Keane T, Davidson JRT. Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]