Abstract
Objective:
The objective of the present study was to examine sudden gains during developmentally adjusted prolonged exposure (PE) for posttraumatic stress disorder (PTSD) among children and adolescents. We hypothesized that sudden gains would be detected and would be predictive of treatment outcome and follow-up.
Method:
Sixty three youngsters (age 8 to 17) completed a developmentally adjusted protocol for the treatment of pediatric PTSD (Foa, Chrestman, & Gilboa-Schechtman, 2008). Participants’ posttraumatic and depressive symptoms were assessed before each treatment session, as well as at approximately 3 and 12 months after treatment termination. We measured posttraumatic symptoms using the Child PTSD Symptom Scale (CPSS – Foa et al., 2001), and depressive symptoms using the Beck Depression Inventory (BDI - Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) and the Children’s Depression Inventory (Kovacs, 1981, 1982).
Results:
Sudden gains were found among 49.2% of participants, and constituted 48.6% of the total reduction in posttraumatic symptoms. Compared to individuals who did not experience sudden gains, individuals who experienced sudden gains reported lower levels of posttraumatic symptoms, F(1, 61) = 14.4, p < 0.001, and depressive symptoms, F(1, 61) = 7.9, p < 0.01 at treatment termination. Differences in posttraumatic symptoms were maintained during both follow-up periods.
Conclusions:
Sudden gains are common in pediatric PE for PTSD and are predictive of long-term outcome. Treatment planning can benefit from considering the intra-individual course of improvement, and treatment development may be enriched by understanding the mechanisms responsible for sudden gains.
Keywords: Posttraumatic Stress Disorder, Prolonged Exposure, Sudden Gains, Children, Adolescents, Treatment
During the last decade researchers have examined instances in which sudden reductions in symptoms occurred between consecutive sessions in treatment. These large, sudden reductions were referred to as sudden gains (Tang & DeRubeis, 1999). Sudden gains were defined as between-session improvements that (a) are large in absolute terms, (b) represent at least a 25% reduction from the pre-gain level of symptoms, and (c) are stable, such that the mean symptom level in the three pre-gain sessions is significantly higher than the mean symptom level in the three post-gain sessions. Sudden gains were initially examined in the treatment of depression and were found to be common, occurring in more than 50% of responders to treatment (Tang & DeRubeis, 1999). Individuals who experienced sudden gains had reduced depression scores at post-treatment, and at follow-up measurements, compared to individuals who did not experience sudden gains (Tang & DeRubeis, 1999). This indicates that sudden gains are an important phenomenon occurring in the treatment for depression and have an impact both on outcome and follow-up.
Since the initial study, the phenomenon of sudden gains has been repeatedly examined in various treatments for depression (e.g., Vittengl, Clark, & Jarrett, 2005). Importantly, sudden gains were also detected in treatments for adolescents including cognitive behavioral, family and supportive treatments (Gaynor, Weersing, Kolko, Birmaher, Heo, & Brent, 2003). Sudden gains have been consistently found to predict post-treatment depression (e.g., Gaynor et al., 2003; Vittengl et al., 2005). However, whereas some studies find that sudden gains are predictive of follow-up measurements (e.g., Gaynor et al., 2003), others do not (e.g., Vittengl et al., 2005).
Evidence is accumulating that sudden gains may play an important role in additional disorders beside depression. Stiles et al. (2003) found sudden gains in the treatment of individuals who suffered from a variety of disorders and were treated with a diverse set of clinical approaches in a naturalistic setting. Moreover, sudden gains were found in treatments for panic disorder (Clerkin, Teachman, & Smith-Janik, 2008), generalized anxiety disorder (Present et al., 2008), and posttraumatic stress disorder (PTSD; Doane, Feeny, & Zoellner, 2010; Kelly, Rizvi, Monson, & Resick, 2009). In the present study, we examined sudden gains in prolonged exposure (PE) treatment for pediatric PTSD. To our knowledge, no study has examined sudden gains in PTSD symptoms among children and adolescents.
Prolonged exposure (PE) is a well-validated treatment for PTSD among adult survivors of trauma (Rothbaum, Meadows, Resick, & Foy, 2000). PE has also been found to be effective among children and adolescents in an open trial (Foa, Chrestman, Gilboa-Schechtman, 2008) and in a randomized controlled trial (Gilboa-Schechtman et al., 2010).
The aim of the present study was to examine sudden gains in PE for PTSD among children and adolescents. We hypothesized that sudden gains in posttraumatic symptoms would be detected and that individuals with sudden gains would report lower PTSD and depressive symptoms compared to individuals without sudden gains, both at post-treatment and at follow-up.
Method
Participants
Participants were 63 children and adolescents who sought treatment for PTSD at a large public clinic in Israel. Participants were between 8 and 17 years of age, and 37 were female (58.7%). Following Gaynor et al. (2003) we considered individuals below the age of 13 as children and individuals 13 and over as adolescents. Of the total sample, 38 (60.3%) were children and 25 (39.7%) were adolescents. All participants were diagnosed with primary PTSD according to DSM-IV criteria, and all experienced single-event trauma1. Table 1 presents demographic, clinical and trauma related measures for all participants.
Table 1.
Demographic, trauma related, and pre-treatment clinical measures
| Measure | Total (N=63) |
Children (N=38) |
Adolescents (N=25) |
Statistic | p |
|---|---|---|---|---|---|
| Gender (%) | χ2(1) = 3.01 | 0.08 | |||
| Male | 26 (41.3) | 19 (50.0) | 7 (28.0) | ||
| Female | 37 (58.7) | 19 (50.0) | 18 (72.0) | ||
| Age | 11.9 (3.2) | 9.6 (1.7) | 15.3 (1.5) | F(1,61) = 181.2 | <0.001 |
| Living with both biological parents (%) |
38 (60.3) | 22 (57.9) | 16 (64.0) | χ2(1) = 0.24 | 0.63 |
| Parental education (years) | |||||
| Mother | 13.8 (2.9) | 13.6 (2.9) | 14.1 (3.0) | F(1,45) = 0.28 | 0.60 |
| Father | 14.2 (3.1) | 13.6 (2.2) | 15.2 (4.1) | F(1,23) = 1.61 | 0.22 |
| Type of Trauma (%) | χ2(4) = 6.83 | 0.23 | |||
| Motor Vehicle Accidents | 24 (38.1) | 16 (42.1) | 8 (32.0) | ||
| Terror Attacks | 18 (28.6) | 9 (23.7) | 9 (36.0) | ||
| Non-sexual assault | 2 (3.2) | 1 (2.6) | 1 (4.0) | ||
| Sexual assault | 9 (14.3) | 4 (10.5) | 5 (20.0) | ||
| Other | 10 (15.8) | 8 (21.1) | 2 (8.0) | ||
| Time since trauma (in months) |
17.0 (17.5) | 17.5 (17.6) | 16.3 (17.7) | F(1,52) = 0.07 | 0.80 |
| Number of missing sessions | 1.5 (1.6) | 1.6 (1.6) | 1.2 (1.5) | F(1,61) = 0.94 | 0.34 |
| Additional AXIS-I disorder (%) |
30 (47.6) | 11 (28.9) | 19 (76.0) | χ2(1) = 13.38 | <0.001 |
| MDD (%) | 14 (22.2) | 1 (2.6) | 13 (52.0) | χ2(1) = 21.26 | <0.001 |
| Anxiety disorders (%) | 14 (22.2) | 6 (15.8) | 8 (32.0) | χ2(1) = 2.29 | 0.13 |
| Disruptive behavior disorders (%) |
10 (15.9) | 4 (10.5) | 6 (24.0) | χ2(1) = 2.05 | 0.15 |
| Medication (%) | 5 (7.9) | 1 (2.6) | 4 (16.0) | χ2(1) = 3.69 | 0.06 |
| CPSS | 24.8 (9.4) | 23.6 (9.6) | 26.6 (8.9) | F(1,61) = 1.62 | 0.21 |
| BDI | - | - | 18.5 (8.2) | - | - |
| CDI | - | 11.3 (7.0) | - | - | - |
| Converted BDIa | 15.3 (8.6) | 13.2 (8.4) | 18.5 (8.2) | F(1,61) = 6.14 | <0.05 |
Note. MDD = Major depressive disorder; ADHD = Attention-deficit hyperactivity disorder; CPSS = Child posttraumatic stress disorder symptom scale; BDI = Beck depression inventory; CDI = Children’s depression inventory.
To facilitate comparison we converted CDI scores into BDI scores. First, we divided CDI scores by the total possible score (54) and turned them into percentages. Second, we multiplied these percentages by the total BDI score (63) to assign a converted BDI score.
Participants were included in the present study if they were between 8 and 18 years of age, received a primary diagnosis of PTSD, and were fluent in Hebrew. Participants were excluded if they suffered head injuries resulting in permanent brain damage, changed medication or dosage during treatment, had current substance abuse, or attended an additional psychotherapeutic treatment. In addition, following previous studies (e.g., Clerkin et al., 2008; Tang & DeRubeis, 1999) individuals attending less than 7 treatment sessions were not included in analyses. This is to ensure that individuals included in the analyses received a sufficient dose of treatment. Otherwise, these individuals may be erroneously categorized as not experiencing sudden gains because they did not have the opportunity to do so. Of 85 individuals who began treatment, 63 were considered completers, whereas the remaining 22 (25.9%) dropped out from treatment and did not attend 7 sessions2. Drop-outs completed 3.6 sessions on average (SD = 1.87). No significant differences between drop-outs and completers were found on any demographic or clinical variable (all ps > 0.05).
Procedure
All participants and their parents signed informed consent forms. Participants were diagnosed using the Schedule of Affective Disorders and Schizophrenia for School-Age Children- Revised (K-SADS - Kaufman et al., 1997), which was administered both to the parents and to the youngster. Participants began treatment 2 months on average following the intake (SD = 1.7 months). Prior to active treatment, 1-3 sessions devoted to case management and a motivational interview were conducted (Foa et al., 2008). During active treatment, participants filled out self-report measures before every session and the assessment before the first session constituted the pre-treatment measurement. Following treatment completion participants were contacted twice for follow-up assessments in which self-report questionnaires were administered. The first follow-up assessment (FU1) took place 3.4 months (SD = 1.3) following treatment and the second follow-up assessment (FU2) took place 12.1 months (SD = 4.4) following treatment. Of the total sample, 39 participants (61.9%) took part in FU1 and 31 (49.2%) took part in FU2.
Treatment, Therapists, and Treatment Integrity
Treatment in the present study was based on the protocol of PE for children and adolescents (Foa et al., 2008). Treatment consisted of 12-15 sessions and included 3 modules. The first module, psychoeducation and treatment planning, consisted of 2-3 sessions and included education regarding PTSD and the treatment rationale. The second module, exposure, consisted of 8-9 sessions. During these sessions imaginal exposure and in vivo exposure were performed. The third module, relapse prevention and treatment termination, consisted of 2-3 sessions and included a discussion of triggers for possible relapse and appropriate coping strategies. Therapists were clinical psychologists who underwent training in pediatric PE prior to the treatment by Dr. Edna B. Foa. During treatment, all therapists had weekly supervision sessions with Dr. Eva Gilboa-Schechtman to ensure treatment integrity.
Since the number of sessions varied between participants (12-15) we treated the 12th session as the final session. We did this to equate the number of sessions among all participants and thus their opportunities to experience sudden gains3.
Measures
Participants were interviewed using the Schedule of Affective Disorders and Schizophrenia for School-Age Children – Revised for DSM—IV (K-SADS - Kaufman et al., 1997), in order to establish diagnoses. The K-SADS is a highly reliable and valid semi-structured interview, covering both current and lifetime disorders (Kaufman et al., 1997). Before each treatment session participants were administered the Child PTSD Symptom Scale (CPSS – Foa, Johnson, Feeny, & Treadwell, 2001), which is a well-validated self-report inventory with 17 items that assess PTSD symptoms according to the DSM-IV. In addition, before each session participants were administered the Beck Depression Inventory (BDI - Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) if they were 13 years old and over, or the Children’s Depression Inventory (CDI - Kovacs, 1982) if they were under 13 years old.
Definition of Sudden Gains
Criterion A.
Consistent with previous research (Hofmann, Schulz, Meuret, Moscovitch, & Suvak, 2006), we used the reliable change index (RCI; Jacobson & Truax, 1991) to arrive at a gain that is large in absolute terms. This led to a cutoff score of 3.3 for the CPSS. We chose 4 as the final cutoff (7.8% of the total CPSS range) to approximate Tang and DeRubeis (1999) who reported that their cutoff for the BDI constituted 11% of the total BDI range. Thus, changes of 4 or greater were considered as fulfilling criterion A4.
Criterion B.
The gain’s magnitude should exceed 25% of the pre-gain score.
Criterion C.
Consistent with Tang and DeRubeis (1999) we conducted independent t-tests between the three sessions before a sudden gain and the three sessions after a sudden gain. A significant difference indicated that this criterion was fulfilled.
Data Analysis
Following Hofmann et al. (2006) we conducted all analyses using both ANOVA and Hierarchical Linear Modeling (HLM). As HLM results were identical to ANOVA results, we report only the latter to remain consistent with previous studies. We used the Last-Observation-Carried-Forward (LOCF) method to handle missing data in all ANOVA analyses. Thus, all analyses reported include the total sample (n = 63).
Because children filled out the CDI and adolescents filled out the BDI we created a single depression variable in order to facilitate comparison. First, we converted CDI scores into percentages of the total CDI range. We then used the percentage to assign a BDI score by multiplying it by the total BDI range. This facilitated comparison between children and adolescents as well as between the present study and previous studies which used the BDI.
Results
Frequency of sudden gains
Using the criteria above, we detected 44 sudden gains in posttraumatic symptoms among 31 participants: 18 participants experienced a single gain, and 13 experienced 2 sudden gains. Thus, a total of 49.2% of participants experienced sudden gains. The average sudden gain was 8.51 points on the CPSS and constituted 48.6% of the reduction in CPSS scores during treatment. The largest number of sudden gains occurred between sessions 4 and 5 (22.7%; Table 2). No differences between children and adolescents were found regarding the occurrence of sudden gains, or the number of sudden gains (all ps > 0.05).
Table 2.
Timing of sudden gains
| Session | Frequency | Percent | Cumulative Frequency |
Cumulative Percent |
|---|---|---|---|---|
| 3 | 9 | 20.5% | 9 | 20.5% |
| 4 | 10 | 22.7% | 19 | 43.2% |
| 5 | 7 | 15.9% | 26 | 59.1% |
| 6 | 6 | 13.6% | 32 | 72.7% |
| 7 | 5 | 11.4% | 37 | 84.1% |
| 8 | 2 | 4.5% | 39 | 88.6% |
| 9 | 3 | 6.8% | 42 | 95.5% |
| 10 | 2 | 4.5% | 44 | 100.0% |
We examined possible sudden gains in BDI scores during treatment using the original criteria by Tang and DeRubeis (1999). We found only 2 participants who experienced sudden gains in BDI scores. Thus, no statistical analyses were preformed on these sudden gains.
Sudden gains and outcome
We conducted a repeated-measures MANOVA with Time (2 level within-subject variable: pre vs. post) and Sudden Gains (2 level between-subject variable: present vs. absent) as independent variables. The dependent variables were CPSS and BDI scores. Results indicated a significant Time X Sudden Gains interaction for both CPSS, F(1, 61) = 12.3, p < 0.01, partial η2 = 0.17, and BDI, F(1, 61) = 7.7, p < 0.01, partial η2 = 0.11. In addition, a significant main effect for Time was found on both CPSS, F(1, 61) = 234.6, p < 0.001, partial η2 = 0.79, and BDI, F(1, 61) = 62.9, p < 0.001, partial η2 = 0.51.
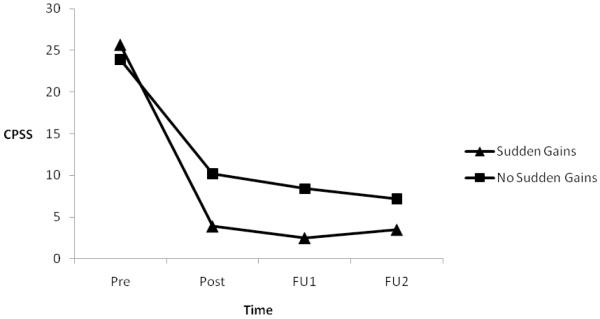
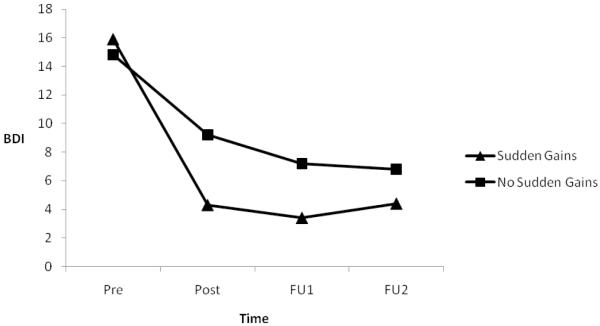
The interaction effect was such that participants who experienced sudden gains in posttraumatic symptoms, reported greater reductions in both CPSS and BDI during treatment (MCPSS change = 21.8; MBDI change = 11.6), compared to participants who did not experience sudden gains (MCPSS change = 13.7; MBDI change = 5.6) (see Figure 1 and 2). Importantly, individuals with and without sudden gains did not differ on pre-treatment CPSS, F(1, 61) = 0.6, p = 0.45, partial η2 = 0.01, or BDI, F(1, 61) = 0.3, p = 0.61, partial η2 = 0.00, but differed significantly on post treatment CPSS, F(1, 61) = 14.4, p < 0.001, partial η2 = 0.19, and BDI, F(1, 61) = 7.9, p < 0.01, partial η2 = 0.12. This suggests that sudden gains are related to better treatment outcome (See Table 3 for descriptive statistics).
Figure 1.
CPSS scores for individuals with and without sudden gains
Figure 2.
BDI scores for individuals with and without sudden gains
Table 3.
Clinical measures for individuals with and without sudden gains (n = 63)
| Pre-treatment | Post-treatment | Follow-up 1 (M=3.4 months) |
Follow-up 2 (M=12.1 months) |
|
|---|---|---|---|---|
| Total sample (N=63) | ||||
| CPSS | 24.8 (9.4) | 7.1 (7.3) | 5.5 (6.8) | 5.4 (6.4) |
| Converted BDIa | 15.3 (8.6) | 6.8 (7.3) | 5.3 (6.5) | 5.6 (7.1) |
| Individuals with sudden gains (N=31) |
||||
| CPSS | 25.7 (9.0) | 3.9 (4.0) | 2.5 (3.0) | 3.5 (4.3) |
| Converted BDIa | 15.9 (8.3) | 4.3 (5.2) | 3.4 (4.9) | 4.4 (6.0) |
| Individuals without sudden gains (N=32) |
||||
| CPSS | 23.9 (9.7) | 10.2 (8.4) | 8.4 (8.0) | 7.2 (7.6) |
| Converted BDIa | 14.8 (9.0) | 9.2 (8.2) | 7.2 (7.4) | 6.8 (7.9) |
Note. The last-observation-carried-forward (LOCF) technique was used to impute missing values in follow-up measurements; CPSS = Child posttraumatic stress disorder symptom scale; BDI = Beck depression inventory.
To facilitate comparison we converted CDI scores into BDI scores. First, we divided CDI scores by the total possible score (54) and turned them into percentages. Second, we multiplied these percentages by the total BDI score (63) to assign a converted BDI score.
In addition, we found that among individuals who did not experience sudden gains, post-treatment scores were significantly lower compared to pre-treatment scores on both the CPSS, F(1, 31) = 67.1, p < 0.001, partial η2 = 0.68, and BDI, F(1, 31) = 14.8, p < 0.001, partial η2 = 0.32. Thus, even individuals who did not experience sudden gains significantly improved during PE.
Sudden gains and follow-up
We examined long-term effects of treatment using a MANOVA with Time (3 level within-subject variable: post vs. FU1 vs. FU2) and Sudden Gains (2 level between-subject variable: present vs. absent) as independent variables. Dependent variables were CPSS and BDI. A significant main effect of Sudden Gains emerged for both CPSS, F(1, 61) = 17.4, p < 0.001, partial η2 = 0.22, and BDI, F(1, 61) = 6.4, p < 0.05, partial η2 = 0.10. No other significant effects were found. The effect of Sudden Gains was such that overall, individuals who experienced sudden gains had lower CPSS and BDI scores following treatment compared to individuals who did not experience sudden gains (see Table 3 and Figures 1 and 2). This effect was significant at post-treatment for both CPSS, F(1, 61) = 14.4, p < 0.001, partial η2 = 0.19, and BDI, F(1, 61) = 7.9, p < 0.01, partial η2 = 0.12, at FU1 for both CPSS, F(1, 61) = 15.0, p < 0.001, partial η2 = 0.20, and BDI, F(1, 61) = 6.0, p < 0.05, partial η2 = 0.09, and at FU2 for CPSS, F(1, 61) = 5.8, p < 0.05, partial η2 = 0.09, but not for BDI, F(1, 61) = 1.9, p = 0.18, partial η2 = 0.03. Thus, sudden gains were associated with reduced posttraumatic and depressive symptoms during follow-up periods.
Predictors of sudden gains
We examined whether demographic or pre-treatment clinical measures predict the occurrence of sudden gains. We conducted a series of logistic regressions in which the predictors were demographic and pre-treatment clinical measures and the outcome was the occurrence of sudden gains (yes vs. no). No demographic or pre-treatment clinical measure significantly predicted the occurrence of sudden gains.
Discussion
We found that sudden gains in posttraumatic symptoms were detected among half of the pediatric completers of an adapted PE protocol. Importantly, sudden gains were also found to predict better outcome at treatment termination and at 3 and 12 months follow-up.
The frequency of sudden gains in the present study (49.2%) is similar to the frequency reported in the previous studies (e.g., Kelly et al., 2009; although see Hofmann et al., 2006). Similar to the present study, previous studies have also found that individuals who experienced sudden gains had less severe symptoms at post-treatment and follow-up compared to individuals who did not experience sudden gains (e.g., Clerkin et al., 2008). Our results suggest that sudden gains are a common phenomenon in PE for PTSD among children and adolescents, and that they are associated with better treatment outcome and follow-up.
Researchers have attempted to identify predictors of sudden gains. Some have proposed that treatment-specific factors such as cognitive changes during treatment result in sudden gains (e.g., Tang & DeRubeis, 1999). Others have suggested non-specific factors such as treatment alliance (e.g., Ilardi & Craighead, 1994) or readiness for treatment, and still others have proposed that individuals with sudden gains begin treatment with higher levels of impairment and are subject to the statistical phenomenon of regression to mean (Hofmann et al., 2006). The findings in the sudden gains literature to date are inconsistent with the treatment-specific factors explanation, mostly because sudden gains have been observed in diverse treatments including pharmacotherapy and even pill placebo (e.g., Vittengl et al., 2005). Elevated pre-treatment symptoms also seem unlikely to be the cause of sudden gains. In the present study, as well as in several other studies, pretreatment clinical measures did not predict the occurrence of sudden gains (e.g., Tang & DeRubeis, 1999). Thus, the most promising predictors of sudden gains remain non-specific factors.
The role of sudden gains in recovery from PTSD bears important clinical implications. It is possible that individuals who do not experience sudden gains by mid-treatment could benefit more from longer, more intensive treatment. Conversely, if sudden gains occur during treatment, the treatment course may be shortened. Moreover, our findings emphasize the importance of conducting assessments regularly throughout treatment and examining the intra-individual course of symptom change. Such an examination can assist in tailoring the treatment to the individual’s specific needs. Future studies can examine strategies for improving outcome among individuals who do not experience sudden gains.
This study has several limitations. First, there are some limitations to children’s self-report. Use of parent’s reports to identify sudden gains can be an intriguing avenue for future research. Second, sample sizes during follow-up measurements were small and replication of our results with larger samples is needed. Third, the present study did not include a control group examining sudden gains among wait-list participants. Finally, we did not measure specific treatment factors (e.g., cognitive change) or general treatment factors (e.g., therapeutic alliance) during treatment. The inclusion of such measures in the future may contribute to the understanding of the sudden gains phenomenon. Despite these limitations, the present study contributes to the sudden gains literature, extending the examination of this important phenomenon to PTSD among children and adolescents. When taken together with previous findings, our findings indicate that sudden gains are found across multiple disorders, multiple types of treatments and across the lifespan. This emphasizes the importance of examining the intra-individual trajectory of change for intervention planning and prognosis.
Acknowledgements:
The authors wish to thank all the therapists, the independent evaluators, and consultants for their help. In addition, we would like to thank Dr. Edna Foa and Dr. Kelly Chrestman from the University of Pennsylvania, and Dr. Orit Krispin, Dr. Olga Goraly, and Dr. Alan Apter from Schneider’s Children Medical Center.
Footnotes
Whereas all individuals in the present study sought treatment due to a specific, single traumatic event, most reported experiencing additional traumatic events in the past that did not develop into PTSD.
We could not examine sudden gains among drop-outs due to missing data. These individuals either attended an insufficient number of sessions, or their pattern of missing data precluded the calculation of sudden gains (i.e., attending alternate sessions, or attending two consecutive sessions and then missing two). Thus we could not determine whether these individuals did or did not experience sudden gains.
We also allowed the number of sessions to vary (12-15) and found that no additional gains were identified and all results were identical. Thus, we report only analyses based on an equal treatment length of 12 sessions. Number of sessions did not significantly predict posttraumatic or depressive symptoms at post-treatment or at follow-ups (all ps > 0.05).
We also examined a cutoff point that is exactly 11% of the total CPSS score to approximate the original Tang & DeRubeis (1999) study. This translated into a cutoff score of 6 (instead of 4) on the CPSS. Use of this cutoff point resulted in 3 participants who were no longer categorized as experiencing sudden gains. However, results of all analyses were identical. We therefore report only analyses made using the 4 point cutoff score.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
References
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Clerkin EM, Teachman BA, Smith-Janik SB. Sudden gains in group cognitive-behavioral therapy for panic disorder. Behaviour Research and Therapy. 2008;46:1244–1250. doi: 10.1016/j.brat.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doane LS, Feeny NC, Zoellner LA. A preliminary investigation of sudden gains in exposure therapy for PTSD. Behaviour Research and Therapy. 2010;48:555–560. doi: 10.1016/j.brat.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Chrestman K, Gilboa-Schechtman E. Prolonged exposure therapy for adolescents with PTSD. Oxford University Press; New York, NY: 2008. [Google Scholar]
- Foa EB, Johnson KM, Feeny NC, Treadwell KRH. The child PTSD symptom scale: A preliminary examination of its psychometric properties. Journal of Clinical Child Psychology. 2001;30:376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- Gaynor ST, Weersing VR, Kolko DJ, Birmaher B, Heo J, Brent DA. The prevalence and impact of large sudden improvements during adolescent therapy for depression: A comparison across cognitive–behavioral, family, and supportive therapy. Journal of Consulting and Clinical Psychology. 2003;71:386–393. doi: 10.1037/0022-006x.71.2.386. [DOI] [PubMed] [Google Scholar]
- Gilboa-Schechtman E, Foa EB, Shafran N, Aderka IM, Powers M, Rachamim L, et al. Prolonged Exposure Versus Dynamic Therapy for Adolescent PTSD: A Pilot Randomized Controlled Trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1034–1042. doi: 10.1016/j.jaac.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Schulz SM, Meuret AE, Moscovitch DA, Suvak M. Sudden gains during therapy of social phobia. Journal of Consulting and Clinical Psychology. 2006;74:687–697. doi: 10.1037/0022-006X.74.4.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilardi SS, Craighead WE. The role of nonspecific factors in cognitive– behavior therapy for depression. Clinical Psychology: Science and Practice. 1994;1:138–156. [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kelly KA, Rizvi SL, Monson CM, Resick PA. The impact of sudden gains in cognitive behavioral therapy for posttraumatic stress disorder. Journal of Traumatic Stress. 2009;22:287–293. doi: 10.1002/jts.20427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. The Children’s Depression Inventory: A self-rating depression scale for school-aged youngsters. 1982 Unpublished manuscript. [Google Scholar]
- Present J, Crits-Christoph P, Connolly-Gibbons MB, Hearson B, Ring-Kurtz S, Worlay M, et al. Sudden gains in the treatment of generalized anxiety disorder. Journal of Clinical Psychology. 2008;64:119–126. doi: 10.1002/jclp.20435. [DOI] [PubMed] [Google Scholar]
- Rothbaum BO, Meadows EA, Resick P, Foy DW. Cognitive-behavioral therapy. In: Foa EB, Keane TM, Friedman MJ, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. Guilford Press; New York, NY: 2000. pp. 60–83. [Google Scholar]
- Stiles WB, Leach C, Barkham M, Lucock M, Iveson S, Shapiro DA, et al. Early sudden gains in psychotherapy under routine clinic conditions: Practice-based evidence. Journal of Consulting and Clinical Psychology. 2003;71:14–21. [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ. Sudden gains and critical sessions in cognitive behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67:894–904. doi: 10.1037//0022-006x.67.6.894. [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Jarrett RB. Validity of sudden gains in acute phase treatment of depression. Journal of Consulting and Clinical Psychology. 2005;73:173–182. doi: 10.1037/0022-006X.73.1.173. [DOI] [PubMed] [Google Scholar]