Abstract
This prospective study of children with recurrent abdominal pain (N = 133; ages 8–15 years) used path analysis to examine relations among dispositional pain beliefs and coping styles, cognitions and behavior related to a specific pain episode, and short- and long-term outcomes. Children believing they could not reduce or accept pain appraised their episode-specific coping ability as low and reported passive coping behavior. Dispositional passive coping had direct effects on both episode-specific passive coping and long-term symptoms and disability. Accommodative coping (acceptance and self-encouragement) was associated with reduced episode-specific distress, which itself predicted reduced depressive symptoms 3 months later. Results suggest that coping-skill interventions for children with chronic pain should target reductions in passive coping and consider the potential benefits of accommodative coping strategies.
Keywords: pain, pain beliefs, appraisal, coping, children
Studies of children’s coping with chronic pain typically have conceptualized coping at the dispositional level and have examined the relation of coping styles to broad outcomes such as symptom severity, disability, and health service utilization (e.g., Gil, Williams, Thompson, & Kinney, 1991; Thomsen et al., 2002; Walker, Smith, Garber, & Van Slyke, 1997). The process by which children’s styles of coping with pain may lead to these outcomes rarely has been examined. However, it is reasonable to assume that children’s coping styles predict their episode-specific coping strategies and these, in turn, determine whether the outcomes of individual pain episodes will be positive or negative, in a process that repeats itself multiple times to yield long-term outcomes. For example, children who report on a retrospective questionnaire that they usually go to bed when they experience pain would be expected to report in a diary assessment that they had gone to bed on the day of a pain episode. Of course, pain episodes may vary considerably across time and circumstances, and this would be reflected in variability in the coping strategies a child might use during a particular pain episode. Thus, the correspondence between dispositional and episode-specific coping would never be perfect.
The goal of this study was to test a conceptual model of the relations among dispositional pain beliefs and coping styles, cognitions and behavior related to a specific pain episode, and short-and long-term outcomes. The relations in this model are important on a conceptual level for understanding the process by which appraisal and coping with pain influence children’s health and on a practical level for evaluating the use of children’s retrospective reports of their usual coping style in predicting their behavior during specific episodes of pain. The relation of dispositional styles of coping to episode-specific coping has been examined in the general stress and coping literature (e.g., Carver & Scheier, 1994; Schwartz, Neale, Marco, Shiffman, & Stone, 1999) and is the focus of continued attention in a debate regarding the consistency of coping behavior and whether it can be regarded as a trait (e.g., Ptacek & Gross, 1997; Schwartz et al., 1999). Little is known, however, about the relation between dispositional styles of coping with pain and coping associated with individual pain episodes (Rudolph, Dennig, & Weisz, 1995).
General Conceptual Framework
The proposed model is based on the appraisal and coping framework advanced by Lazarus and Folkman (1984; Folkman, Lazarus, Dunkel-Schetter, DeLongis, & Gruen, 1986). This framework emphasizes the importance of the individual’s perceptions in evaluating potential stressors (cf. Monroe & Kelley, 1995). Lazarus and Folkman conceptualized subjective evaluation of stressors as appraisal of coping potential, that is, the individual’s evaluation of “which coping options are available, the likelihood that a given coping option will accomplish what it is supposed to, and the likelihood that one can apply a particular strategy or set of strategies effectively” (p. 35). In the context of pain, appraisal of coping potential has been investigated elsewhere as pain self-efficacy (Lefebvre et al., 1999). According to the framework put forward by Lazarus and Folkman, appraisals of coping potential predict the nature of coping strategies individuals use in confronting a particular stressor. These strategies, in turn, predict outcomes.
This conceptual framework can be applied both at the dispositional level in understanding how coping beliefs and styles of coping with chronic stressors influence global outcomes and at the situational level in understanding how cognitions and behaviors associated with a particular stressor episode influence the immediate outcome of that episode. We have combined both levels of analysis in a model in which chronic pain is the stressor. Prior pediatric investigations have examined the relation of pain coping styles to adjustment (e.g., Gil et al., 1991; Thomsen et al., 2002; Walker et al., 1997) and the relation of pain cognitions to distress during a single episode of pain (Claar, Walker, & Smith, 2002), but this is the first to examine both appraisal and coping with pain and to include both dispositional and situational levels of analysis in the same model.
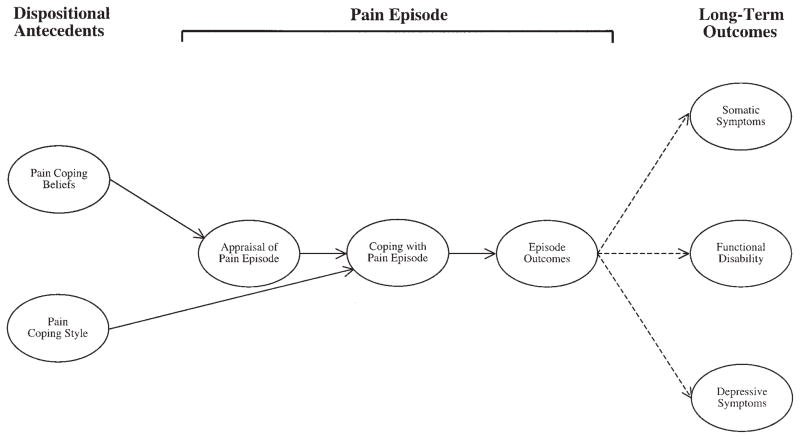
Our general conceptual model is depicted in Figure 1. Pain beliefs and coping styles are hypothesized to influence appraisals and coping strategies associated with a single pain episode. Episode-specific appraisals should further influence the specific coping strategies used during the pain episode, and these coping activities, in turn, are hypothesized to influence acute outcomes of the pain episode. Finally, episode-specific outcomes are hypothesized to contribute to long-term outcomes including somatic symptoms, functional disability, and depressive symptoms. Although the figure depicts a single pain episode, it is intended to represent a process that is repeated multiple times in chronic or recurrent pain.
Figure 1.
Conceptual model. The dashed lines indicate that the observed relations between short- and long-term outcomes were expected to be weak.
Of course, the relations of dispositional pain beliefs and coping styles to episode-specific appraisals and coping behaviors would be attenuated by contextual factors that influence responses unique to the particular episode. Similarly, we reasoned that only in extreme circumstances would the outcomes of a single encounter strongly influence long-term outcomes. Instead, it is the pattern of outcomes over a series of episodes that is hypothesized to shape long-term outcomes. Thus, we expected the observed relations between episode-specific outcomes and long-term outcomes to be weak, as represented in Figure 1 by dashed lines from episode-specific outcomes to long-term outcomes.
A Combined Dispositional–Situational Model
We translated the general theoretical framework into a testable model, with each construct in Figure 1 represented by measurable variables. We tested this model in a sample of children with recurrent abdominal pain (RAP), the most common recurrent pain condition of childhood (Apley, 1975; McGrath, 1994). The study builds on prior investigations demonstrating that dispositional coping styles of children with RAP predict long-term health outcomes (Walker et al., 1997). No prior investigations have examined how children with RAP cope with individual pain episodes.
Appraisals of coping potential were assessed as the child’s perceived ability to engage in the two major forms of coping described by Lazarus and Folkman (1984). Thus, appraisal of problem-focused coping potential (PFCP) refers to the ability to alter circumstances to make them more desirable (in this case, to alleviate pain), whereas appraisal of emotion-focused coping potential (EFCP) refers to the ability to accept and adjust to circumstances, even if they cannot be improved (in this case, to accept and adjust to pain). Prior literature has only examined global self-efficacy beliefs regarding pain coping (Jensen, Turner, & Romano, 1991; Lefebvre et al., 1999; Thompson, Gil, Abrams, & Phillips, 1992). However, the distinction between PFCP and EFCP is important because current pain management approaches emphasize that efforts to eradicate pain (problem-focused coping) may not be as adaptive as accepting pain and maximizing one’s activities (i.e., emotion-focused, accommodative coping; e.g., Bursch, Walco, & Zeltzer, 1998; McCracken, 1998).
Appraisals of coping potential were expected to predict three broad categories of coping that we have previously applied to pediatric pain (Walker et al., 1997). Children who believed that they had the ability to reduce or eliminate their pain (i.e., high PFCP) were hypothesized to engage in problem-focused, coping strategies that pain coping literature has referred to as active coping (e.g., Brown & Nicassio, 1987; Walker et al., 1997). Children who believed that they could not reduce their pain (i.e., low PFCP) but could accept and adjust to pain (i.e., high EFCP) were expected to engage in a range of emotion-focused strategies that entailed accommodation to pain and which we have previously referred to as accommodative coping (Walker et al., 1997). Finally, children who believed that they could neither reduce their pain (i.e., low PFCP) nor accept and adjust to their pain (i.e., low EFCP) were expected to respond to pain with coping strategies characterized by passivity, negative cognitions, and lack of active problem solving. This form of coping reflects a second type of emotion-focused coping in the Lazarus and Folkman (1984) framework that has been referred to as passive coping in the pain literature (e.g., Brown & Nicassio, 1987; Walker et al., 1997). To maintain the distinction between accommodative and passive forms of emotion-focused coping, below we refer to the modes of coping by the names used in the pain coping literature: active, accommodative, and passive coping.
In the pain coping literature (e.g., Brown & Nicassio, 1987), passive coping, which involves such strategies as taking to bed, restricting one’s activities, and assuming the worst,1 has been associated with psychological distress and functional impairment (e.g., Brown, Nicassio, & Wallston, 1989; Gil et al., 1991; Smith, Wallston, Dwyer, & Dowdy, 1997; Turner, 1991). Active coping, which involves problem-solving strategies aimed at reducing pain, has been associated with more positive outcomes (e.g., Brown & Nicassio, 1987; Gil et al., 1991; Smith et al., 1997). Finally, accommodative coping, which theoretically enables one to adapt to unchangeable stressors (see Lazarus, 1991; Smith & Lazarus, 1990), has been associated with beneficial outcomes (Turner, 1991; Walker et al., 1997).
All constructs were operationalized at the dispositional and situational levels. Appraisals of coping potential were assessed at the dispositional level as children’s pain coping beliefs and at the situational level as children’s appraisals of their ability to cope with a particular pain episode. Coping styles were assessed at the dispositional level as the degree to which the child usually engaged in each coping category when in pain. At the situational level, coping was assessed in terms of coping strategies the child actually used during a specific pain episode. Short-term outcomes were represented by somatic symptoms and emotional distress that the child reported experiencing during the pain episode. Long-term outcomes were represented by measures of more chronic health outcomes including somatic symptoms, functional disability, and depressive symptoms that often are elevated in children with persistent abdominal pain (Walker, Garber, & Greene, 1993).
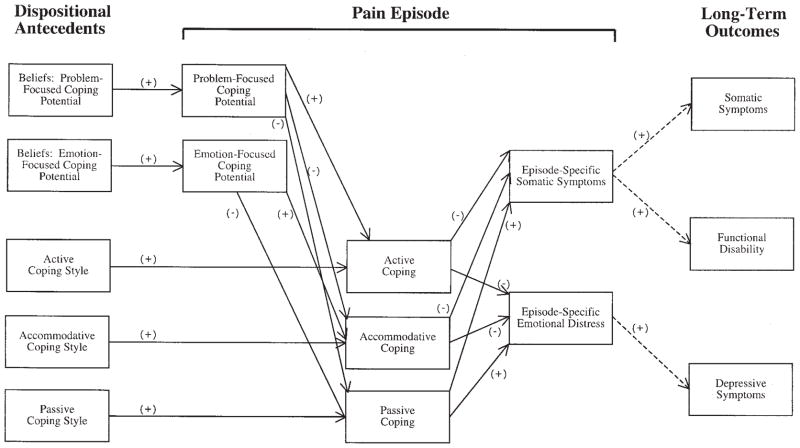
Figure 2 summarizes the hypothesized relations among these variables. We started with the simplifying assumption that each dispositional variable would predict its situational counterpart but only its counterpart.2 Thus, for example, we predicted that a passive coping style would be associated with passive coping during a particular pain episode but not with active or accommodative coping during the pain episode. Within the pain episode, we expected episode-specific appraisals to be associated with episode-specific coping. Specifically, we predicted that episode-specific PFCP would be positively associated with episode-specific active coping because active coping involves problem-solving efforts to alleviate pain (Walker et al., 1997). Episode-specific EFCP was expected to be positively associated with accommodative coping as it involves emotional acceptance of pain. When appraisal of PFCP is low, accommodative coping is more likely (Folkman, 1984; Lazarus & Folkman, 1984), and thus we also predicted that PFCP would be negatively associated with accommodative coping. Finally, we predicted that low levels of both PFCP and EFCP would be associated with passive coping, as passive coping reflects giving up.
Figure 2.
Specific model of hypothesized relations among variables. The dashed lines indicate that the depicted relations between short- and long-term outcomes were expected to be weak.
All three types of episode-specific coping efforts were expected to predict short-term outcomes. Active coping and accommodative coping were expected to have the greatest potential benefit and thus to be negatively associated with somatic and affective symptoms. In line with prior literature, episode-specific passive coping was expected to be associated with increased levels of both somatic and emotional distress. These short-term outcomes were then predicted to be positively associated with long-term outcomes. To simplify, we predicted that each short-term outcome would be related to the long-term outcome(s) it most resembled. For example, episode-specific somatic symptoms were predicted to be positively associated with both long- term somatic symptoms and functional disability but not with depressive symptoms.
Method
Sample
The sample included 133 consecutive new patients who were referred to a pediatric gastroenterology clinic for evaluation of abdominal pain. Patients were eligible if they had experienced chronic or recurrent episodes of abdominal pain severe enough to interrupt activities and occurring over a period of at least 3 months and if they were between 8 and 15 years of age, the period when chronic or recurrent abdominal pain is most common (cf. Apley, 1975). Exclusionary criteria included a chronic health condition or mental retardation. Of the 229 patient families contacted, 57 (26%) did not meet eligibility criteria and 18 (8%) declined, leaving 154 participants. Complete data were obtained for 133 participants3 who constituted the final sample. The sample was primarily Caucasian (95%) and female (57%), with a mean age of 10.80 years (SD = 2.10).
Procedure
Parents of children scheduled for evaluation of abdominal pain were identified by clinic staff and contacted several days prior to their clinic visit. Those who expressed interest in the study were screened for eligibility and asked to arrive early if they wished to participate. Informed consent was obtained at the clinic by research staff. Interviews were conducted prior to the medical evaluation. An interviewer read the questionnaire items to children in a private room, and the children selected answers from a response sheet. Approximately 2 weeks later, the family was contacted by telephone in the evening on each of 5 consecutive school days and an interviewer administered the Daily Diary Interview (DDI) to the children (Walker, Smith, Garber, Van Slyke, & Claar, 2001). Three months following the clinic visit, measures of somatic symptoms, depressive symptoms, and functional disability were administered to the children by telephone. The administration protocol was the same for all participants.4 The clinic interview and diary interviews took 30–45 min, and the follow-up interview (at 3 months) took 20 min. Children received $10 for each assessment. The study was approved by the Institutional Review Board.
Measures
Pain Beliefs Questionnaire (PBQ)
Children’s pain beliefs were assessed with the PBQ (Van Slyke, 2001). The PBQ was developed to assess appraisals (cf. Lazarus & Folkman, 1984; Smith & Lazarus, 1990) of pain in children with recurrent pain. These beliefs are assumed to be relatively stable. The PBQ includes conceptually derived subscales, each with six items, to assess PFCP (e.g., “When I have a bad stomach ache, there are ways I can get it to stop”) and EFCP (e.g., “I know I can handle it no matter how bad my stomach hurts”). Children use a 5-point rating scale to indicate how true each statement is about their abdominal pain. In this sample, alpha reliabilities were .82 and .76 for PFCP and EFCP, respectively.
Pain Response Inventory (PRI)
The PRI (Walker et al., 1997) assessed children’s typical styles of coping with abdominal pain. The PRI consists of 60 items rated on a 5-point scale. It yields three broad-band factor scores: Active Coping reflects problem-focused strategies aimed at pain reduction (e.g., “Try to do something to make it go away”), Passive Coping reflects strategies that avoid confronting pain (e.g., “Not even try to do anything about it because it will not help”), and Accommodative Coping reflects efforts to accept and adjust to pain (e.g., “Try to learn to live with it”). Alpha reliabilities were .84 for Active Coping, .90 for Passive Coping, and .88 for Accommodative Coping.
Children’s Somatization Inventory (CSI)
The CSI (Garber, Walker, Zeman, 1991; Walker & Garber, 2003; Walker, Garber & Greene, 1991) assesses the severity of nonspecific somatic symptoms (e.g., “headaches,” “dizziness”) that often are reported by children with RAP and need not have organic disease etiology (Walker et al., 1991). Respondents rate the extent to which they have experienced each of 35 symptoms during the last 2 weeks using a 5-point scale, ranging from 0 (not at all) to 4 (a whole lot). Three-month test–retest Pearson product–moment correlation reliabilities for the CSI are .50 for well patients and .66 for patients with chronic pain (Walker et al., 1991). In this sample, the CSI had an alpha reliability of .90 and a 3-month stability of .54.
Functional Disability Inventory (FDI)
The FDI (Walker & Greene, 1991) assessed children’s self-reported difficulty in physical and psychosocial functioning due to their physical health during the past 2 weeks. The FDI has high levels of internal consistency and 3-month test–retest reliability estimates exceeding .60 for patients with RAP (Walker & Greene, 1991). Scores on the FDI correlate significantly with school absence (Walker & Greene, 1991). In this sample, the FDI had an alpha reliability of .88 and a 3-month stability of .56.
Children’s Depression Inventory (CDI)
Depressive symptoms were assessed with the CDI (Kovacs, 1981; Kovacs & Beck, 1977). The CDI contains 27 self-report items representing depressive symptoms, each rated on a 3-point scale, and summed to obtain a total score. Reliability and validity are adequate (Saylor, Finch, Spirito, & Bennett, 1984). In the present sample, the CDI had an alpha reliability of .85 and a 3-month stability of .74.
The DDI
Episode-specific measures were obtained with the DDI (Walker et al., 2001), administered to children in the evening on each of 5 school days. The DDI discriminates between pain patients and well children and yields reliable measures of episode-specific pain appraisals, pain coping behavior, and pain outcomes (Walker et al., 2001). The DDI asks children to respond to structured questions regarding the worst pain episode of the day. Data from the first pain episode reported by the child during the week were used to represent the episode-specific appraisals, coping activities, and outcomes for that child. Measures related to these pain episodes are described below.
Children’s appraisals of abdominal pain episodes were assessed with respect to PFCP and EFCP. To assess perceived PFCP, we had children first respond yes or no to the question, “When your stomach hurt, did you think you would be able to do something to make it feel better?” Next, children responded to the question, “How sure were you when your stomach hurt that you (could–could not) do something to make it feel better?” using a 5-point scale, ranging from 0 (not at all) to 4 (a whole lot). The total score for PFCP was obtained by combining the responses to the two questions into a single score that ranged from −4 (indicating high degree of certainty that the child would not be able to reduce the pain) to +4 (indicating a high degree of certainty that the child would indeed be able to reduce the pain). A response of 0 on either of the two original scales was coded as a 0 (i.e., at the midpoint) of this combined scale, resulting in a single 9-point scale. Assessment of EFCP used a similar format with the questions reworded to read, “When your stomach hurt, did you think you would be able to deal with your pain or handle your pain, even if it did not go away?” and “How sure were you that you (could–could not) deal with it or handle it, even if your stomach pain did not go away?”
Three types of episode-specific coping were assessed: Active Coping, Passive Coping, and Accommodative Coping. Items were derived from the PRI (Walker et al., 1997). Active Coping was assessed with three items: “Try to figure out what to do about it” “Ask someone for help” and “Talk to someone who you thought would understand how you felt.” Passive Coping was assessed with three items: “Think to yourself that there was nothing you could do, so you did not even try” “Go off by yourself “ and “Think to yourself that the situation was going to get worse.” Accommodative Coping was assessed with four items: “Try to accept it” “Think of things to take your mind off the situation” “Tell yourself that the situation was not that bad” and “Tell yourself to keep going even though this was happening.” Children reported use of each strategy on a 5-point scale, ranging from 0 (not at all) to 4 (a whole lot). Mean alpha reliabilities for the week were .70, .57, and .79 for Active Coping, Passive Coping, and Accommodative Coping, respectively.
Episode-specific somatic symptoms were assessed with the Index of Somatic Symptoms (Walker et al., 2001), an abbreviated state version of the CSI (Garber et al., 1991; Walker et al., 1991) comprised of five frequently endorsed items from the CSI (i.e., “headache,” “nausea,” “tired,” “sore muscles,” “feeling weak”). Children reported how much they felt each symptom during the pain episode. The mean alpha reliability for the index was .73 across administrations.5
Episode-specific emotional distress was assessed with an abbreviated state version of the Positive and Negative Affect Scale (Watson, Clark, & Tellegen, 1988). Children reported how much they experienced each affect during the pain episode on a 5-point scale, ranging from 0 (not at all) to 4 (a whole lot). Total scores for Positive Affect and Negative Affect were constructed by summing responses to items corresponding to each sub-scale. Episode-Specific Emotional Distress was constructed by subtracting total Positive Affect from total Negative Affect. The mean alpha reliability for the 12-item index was .81 across the week of administrations.
Results
Overview of Model Testing and Preliminary Analyses
The proposed model of pain coping was tested using path analysis based in structural equation modeling. This type of approach was selected because it simultaneously examines multiple hypothesized paths of direct and indirect influence and can provide global indices of the fit between the data and a proposed theoretical model (Holmbeck, 1997; Peyrot, 1996). We examined the interrelations among observed indicators and did not use multiple indicators to model interrelations among latent constructs. This limitation was imposed because the theoretical model we set out to test (see Figure 2) is rather complex and the added complications of modeling the latent constructs would have rendered the planned model testing computationally unfeasible. All analyses were conducted with the EQS program (Version 5.4; Bentler & Wu, 1995) using the maximum-likelihood method of parameter estimation.
In presenting the path analyses, we report several indicators of fit. The most basic indicator is a chi-square reflecting the degree of discrepancy between the observed covariance matrix derived from the data and that predicted by the model. A small, nonsignificant chi-square indicates that one cannot reject the null hypothesis that the tested model fits the data. However, several problems are associated with the chi-square statistic (see, e.g., Hu & Bentler, 1998). First, at a conceptual level, models are taken to be approximations of reality, and testing whether the observed and predicted covariance matrices are identical may be too strict a criterion. Moreover, the chi-square statistic is dependent on sample size and sensitive to model complexity and deviations from multivariate normality in the data (e.g., Hu & Bentler, 1998; La Du & Tanaka, 1989). Accordingly, we report additional fit indices that circumvent these problems. First, the ratio of chi-square:degree of freedom takes model complexity into account. Values less than 3 reflect an acceptable model (e.g., Church & Burke, 1994; Marsh & Hocevar, 1985). Second, the root-mean-square error of approximation (RMSEA) provides an estimate of the average absolute discrepancy between the model covariance estimates and the observed covariances. For this index, values less than .05 indicate a close fit to the data, and values of about .08 represent an acceptable fit (e.g., Browne & Cudek, 1993). Finally, the comparative fit index (CFI; Bentler, 1990) indicates the degree to which the theoretical model better fits the data than a base model constraining all constructs to be uncorrelated with one another. The CFI is considerably more robust than the chi-square statistic from deviations from multivariate normality. A CFI value above .90 reflects a good fit to the data (e.g., Bentler, 1990).
Testing the Fit of the Hypothesized Model
Prior to testing the model, we examined bivariate correlations among variables (see Table 1). The expected relations were generally observed. To examine the overall fit of the hypothesized model, we initially tested the model as depicted in Figure 2. In addition to the paths in the figure, the five exogenous variables representing dispositional antecedents (beliefs and coping styles) were allowed to intercorrelate with one another. The fit of this model to the data was not acceptable, χ2(76, N = 133) = 353.4, p < .01, χ2:df = 4.65, CFI = .62, RMSEA = .17. Accordingly, several modifications were made based on a consideration of theory and the modification indices yielded by the EQS algorithm. Modifications to the a priori model were only made if they were theoretically defendable and did not change the basic thrust of the model.
Table 1.
Intercorrelations Among Variables Entering the Model
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Dispositional problem-focused coping potential | — | ||||||||||||||
| 2. Dispositional emotion-focused coping potential | .62 | — | |||||||||||||
| 3. Dispositional active coping style | .04 | −.05 | — | ||||||||||||
| 4. Dispositional accommodative coping style | .37 | .49 | .29 | — | |||||||||||
| 5. Dispositional passive coping style | −.43 | −.47 | .10 | .00 | — | ||||||||||
| 6. Episode-specific problem-focused coping potential | .29 | .22 | .11 | .12 | −.18 | — | |||||||||
| 7. Episode-specific emotion-focused coping potential | .25 | .40 | .03 | .26 | −.11 | .40 | — | ||||||||
| 8. Episode-specific active coping | .03 | −.02 | .28 | .07 | −.11 | .14 | −.12 | — | |||||||
| 9. Episode-specific accommodative coping | .28 | .35 | .16 | .53 | −.03 | .23 | .44 | .19 | — | ||||||
| 10. Episode-specific passive coping | −.23 | −.28 | −.02 | −.14 | .42 | −.32 | −.33 | .15 | −.02 | — | |||||
| 11. Episode-specific somatic symptoms | −.29 | −.26 | .19 | .11 | .26 | −.29 | −.26 | .23 | .09 | .49 | — | ||||
| 12. Episode-specific distress | −.31 | −.28 | .03 | −.23 | .33 | −.31 | −.28 | −.02 | −.25 | .45 | .43 | — | |||
| 13. Somatic symptoms as outcome | −.24 | −.20 | .01 | .10 | .43 | −.24 | −.20 | .02 | .12 | .28 | .34 | .26 | — | ||
| 14. Functional disability as outcome | −.30 | −.20 | .04 | .05 | .46 | −.30 | −.20 | .03 | .04 | .30 | .28 | .25 | .77 | — | |
| 15. Depressive symptoms as outcome | −.30 | −.35 | .02 | −.11 | .50 | −.30 | −.35 | −.10 | −.14 | .32 | .33 | .37 | .53 | .45 | — |
Note. N = 133. For all entries in the table, rs > .17, ps < .05; rs > .22, ps < .01.
First, the error terms associated with the variables were allowed to correlate within each of the three sets of variables representing episode-specific appraisal, short-term outcomes, and long-term outcomes. These changes allowed the model to account for the fact that, perhaps because of shared method variance, the variables within each of these three sets were more highly intercorrelated than was allowed by the initial model.
Next, the constraints on how short-term outcomes could predict long-term outcomes were loosened slightly. In the initial model, episode-specific somatic symptoms were allowed to predict only somatic symptoms and disability. In the revised model, episode-specific somatic symptoms also were allowed to predict depressive symptoms. Additionally, in the revised model, dispositional passive coping style was allowed to predict the three long-term outcomes. This latter change reflects the relation between dispositional passive coping and long-term outcomes that has been documented in previous pain literature (e.g., Brown et al., 1989; Gil et al., 1991). In allowing these paths, we are indicating that, as anticipated by the dashed lines in the original theoretical model (see Figures 1 and 2), the trait-level relations between coping style and long-term outcomes cannot fully be accounted for by the observation of a single pain episode.
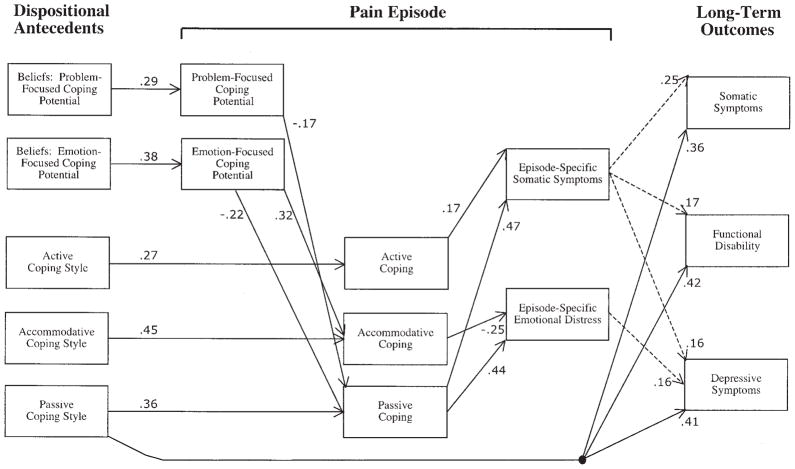
Finally, to simplify model presentation, we eliminated nonsignificant paths among variables and nonsignificant correlations among exogenous variables. The substantive paths of the resulting model are depicted in Figure 3. Significant correlations among the exogenous variables are depicted in Table 2, and those among the relevant endogenous variables’ error terms are depicted in Table 3.
Figure 3.
Final model of observed relations among variables, χ2(75, N = 133) = 142.5, p < .01, comparative fit index = .91, root-mean-square error of approximation = .08. The numerical values represent standardized beta weights. The dashed lines indicate that the depicted paths between short- and long-term outcomes were expected to be weak.
Table 2.
Intercorrelations Among Exogenous Variables
| Variable | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Dispositional problem-focused coping potential | — | ||||
| 2. Dispositional emotion-focused coping potential | .62 | — | |||
| 3. Dispositional active coping style | — | ||||
| 4. Dispositional accommodative coping style | .34 | .50 | .28 | — | |
| 5. Dispositional passive coping style | −.42 | −.56 | — |
Note. All depicted correlations are statistically significant at p < .05. Empty cells represent nonsignificant correlations.
Table 3.
Intercorrelations Among Selected Model Error Terms
| Variable | EEFCE | EDISE | OSYME | OFDE |
|---|---|---|---|---|
| EPFCE | .36 | |||
| ESYME | — | .33 | ||
| OFDE | — | — | .70 | — |
| ODEPE | — | — | .36 | .24 |
Note. All depicted correlations are statistically significant at p < .05. Dashes indicate that correlations were not computed. EPFCE = error term for episode-specific problem-focused coping potential; ESYME = error term for episode-specific somatic symptoms; OFDE = error term for functional disability as an outcome; ODEPE = error term for depressive symptoms as an outcome; EEFCE = error term for episode-specific emotion-focused coping potential; EDISE = error term for episode-specific distress; OSYME = error term for somatic symptoms as an outcome.
The fit of this modified model was adequate, χ2(75, N = 133) = 142.5, p < .01, χ2:df = 1.90, CFI = .91, RMSEA = .08. Overall, this model conforms well to the original model depicted in Figure 2. For instance, each of the episode-specific appraisal and coping variables was reliably predicted by its dispositional counterpart, and in each case, the dispositional counterpart was the only dispositional variable predicting the episode-specific variable.6 In addition, episode-specific data were consistent with the proposed causal flow, such that appraisals of coping potential influenced episode-specific coping activities, which in turn influenced short-term outcomes.
Nonetheless, there were several discrepancies between the proposed and final models, especially concerning episode-specific active coping. Contrary to expectations, active coping with the pain episode was not predicted by appraisals of PFCP, was not related to episode-specific emotional distress, and was positively, rather than negatively, associated with episode-specific somatic symptoms. These results are in line with a history of inconsistent results for active or problem-focused modes of coping (cf. Smith, Wallston, & Dwyer, 2003). Other findings that deviate from the proposed model concern episode-specific accommodative coping, which was predicted by appraisals of EFCP, as hypothesized, but was not associated with lower appraisals of PFCP. In turn, episode-specific accommodative coping was associated with lower levels of short-term emotional distress, as predicted, but did not predict lower levels of somatic symptoms.
Testing a Follow-Up Model
We hypothesized that short-term outcomes of the pain episode would be related to long-term outcomes but these relations would be modest because of the limited impact that a single pain episode should have on long-term adjustment. In fact, statistically reliable, if modest (standardized βs = .16–.25), relations to the long-term outcomes were found: Episode-specific somatic symptoms were associated with all three outcomes, and episode-specific emotional distress was associated with depressive symptoms. However, the meaning of these relations is ambiguous because the long-term outcomes are relatively stable, as indicated by their 3-month stabilities presented above. Thus, without controlling for prior levels of the long-term outcomes, one cannot determine whether the observed relations primarily reflect relations of the short-term outcomes to the stable component of the long-term outcomes, or whether they are associated with changes in the outcomes over 3-months, which would be suggestive of the hypothesized causal contribution of the short-term outcomes to the long-term outcomes.
To investigate this issue, we tested a final model in which baseline values of the three long-term outcomes at the time of the initial clinic visit were added to the model. These three additional exogenous variables were allowed to correlate freely with one another and with the other exogenous dispositional antecedents, and each was allowed to predict to itself (only) at the follow-up assessment. The overall fit of this model (not depicted) was also adequate, χ2(98, N = 133) = 178.7, p < .01, χ2:df = 1.82, CFI = .93, RMSEA = .08. Two aspects of this model are noteworthy. First, other than the relations to the long-term outcomes, none of the associations among variables depicted in Figure 3 were changed appreciably by adding initial values of the long-term outcomes to the model. This suggests that the relations observed in the model are computationally stable. Second, the relations between the short-term and long-term outcomes were weakened and no longer reached statistical significance. However, although the relation between episode-specific emotional distress and long-term depressive symptoms essentially disappeared (β = .05, z < 1), the relations of short-term somatic symptoms maintained trend-level associations to each of the long-term outcomes (βs = .14, .12, and .16; zs = 1.84, 1.65, and 1.68 for somatic symptoms, functional disability, and depressive symptoms, respectively). These latter relations suggest that, in repeated occasions over time, the short-term outcomes may influence long-term outcomes.
Discussion
The theoretical literature on the development of chronic pain in children has highlighted the importance of exaggerated threat appraisal and passive coping in sustaining chronic pain (Walker, 1999; Zeltzer & Feldman, 1999). We have extended that literature by differentiating threat appraisals into appraisals of PFCP and EFCP, by examining accommodative coping in addition to active and passive coping and by testing a model that includes both dispositional and episode-specific pain appraisals and coping as predictors of health outcomes. Our findings provide empirical support and a more fine-grained picture of the process by which children’s pain appraisals and coping may influence a range of outcomes including somatic symptoms, depressive symptoms, and functional disability.
Regarding passive coping, we found that children who believed that they had little ability either to reduce or to accept pain were likely to appraise their ability to cope with a specific pain episode as low and to exhibit passive coping behavior in confronting that pain episode. Passive coping with a pain episode, defined as social withdrawal and catastrophizing cognitions, was associated with higher levels of episode-specific symptoms and emotional distress. These outcomes, in turn, had small but statistically reliable effects on somatic symptoms, functional disability, and depressive symptoms assessed 3 months later. The latter effects, which were predicted to be weak, were still evident as statistical trends, even after controlling for initial values of the long-term outcomes. This suggests that over repeated pain episodes, the influence of episode-specific outcomes on long-term outcomes could become profound. Finally, consistent with the notion that passive coping fuels an escalating cycle of pain amplification (Philips, 1987), we found that dispositional passive coping had significant direct effects both on episode-specific passive coping and on long-term symptoms and disability.
Accommodative coping with pain, defined as acceptance of pain and self-encouragement, has been less extensively studied than either passive or active coping with pain. In this study, appraisals of higher EFCP predicted episode-specific accommodative coping, which was associated with lower levels of emotional distress related to the pain episode. Lower episode-specific distress, in turn, predicted lower levels of depressive symptoms 3 months later. Thus, accommodative coping, which can be conceptualized as a potentially adaptive type of emotion-focused (Lazarus & Folkman, 1984; Smith & Lazarus, 1990) or secondary control engagement coping (Thomsen et al., 2002), appears to be relevant for the regulation of both short- and long-term negative affect. To the extent that accommodative coping facilitates children’s exposure to situations associated with pain, it may help break the escalating cycle of pain fear and avoidance that characterizes chronic pain (Bursch et al., 1998).
The unexpected findings for episode-specific active coping may be explained by several factors. First, the fact that the relation of dispositional active coping to episode-specific active coping was lower than the relation of passive or accommodative coping to their episode-specific counterparts suggests that active coping may be more dependent on environmental resources and thus more context specific than other types of coping. Moreover, the meaning of active coping may depend on the nature of concurrent coping strategies. For example, the impact of seeking social support (an active coping strategy) is likely to differ when combined with self-encouragement than with catastrophizing cognitions. In the latter case, seeking social support might actually represent a passive strategy for attempting to get someone else to take responsibility for a problem. Finally, it is possible that active coping represents targeted problem-solving efforts by some children but in other cases reflects indiscriminant efforts to try anything. For example, children experiencing high levels of distress may engage in a variety of active coping efforts that constitute a cry for help. Thus, the small but significant positive relation between episode-specific active coping and episode-specific somatic symptoms may reflect a direction of causality opposite that hypothesized in our model.
This study is limited by reliance on self-report measures and by the fact that the episode-specific data were embedded in a longitudinal design but were themselves cross-sectional. Although the data proved to be largely consistent with the model we hypothesized and tested, it is possible to generate alternative models that fit the data just as well. As is generally the case with cross-sectional data, changing the direction of influence for supported relations typically will not change a model’s fit. Thus, it is possible that episode-specific outcomes could influence episode-specific coping or that the relations could be bidirectional. For instance, increases in symptoms could lead to increased use of passive coping strategies instead of, or in addition to, the reverse. To sort out such issues, future researchers should use observations of children’s coping with pain in laboratory and natural environments. Replication of this study in other populations of pediatric pain patients, including those with organic disease, would allow a test of the generalizability of the model. In studies of adult pain patients, Turk and Rudy (1988) found that profiles of pain coping were similar across pain populations. This also may be the case for pediatric pain and would have implications for the development of pain management interventions with broad applicability.
Another limitation of this study is that the model was tested on a fairly small sample and has not been cross-validated. A primary concern with small samples is that the observed correlation coefficients have relatively large standard errors. The imprecision in these estimated correlations can cause conditions (such as the correlation matrix failing to be positive definite) that prevent the modeling algorithms from converging on a solution or that lead the algorithms to converge on unstable, nonsensical solutions. The likelihood of these outcomes increases as model complexity increases. A secondary concern is that the parameter estimates and fit indices are derived on the basis of asymptotic models, and thus they are less accurate with smaller samples (see Bollen, 1989).
We took steps to avoid these problems: We limited the complexity of our initial model by making several simplifying assumptions, we modeled observed indicators rather than latent constructs, and we relied primarily on fit indices, such as the CFI and RMSEA, that are less sensitive to sample size and model complexity than is the chi-square. Moreover, the model we evaluated appeared to be both computationally stable (in that individual parameters did not change greatly when various paths and variables were added or removed from the model) and theoretically meaningful. Thus, we are confident that the final model is sound, despite the relatively small sample on which it was based. Nonetheless, as would be the case even with a larger sample, it is important to cross-validate this model in subsequent work.
It also should be noted that in administering the PBQ and the PRI only at the initial clinic visit, we assumed that our dispositional constructs were relatively stable over time. The predictive relations that the dispositional appraisal and coping variables demonstrated to their episode-specific counterparts assessed 2 weeks after the clinic visit offer some validation to this assumption. Nonetheless, the stability of these measures needs to be explicitly examined.
Finally, the model tested in this study does not consider contextual factors that may impact children’s pain behavior (cf. McGrath, 1994). The modest, albeit significant, relations we observed between dispositional appraisals and coping and their episode-specific counterparts suggest that contextual factors may combine with children’s dispositional response tendencies to determine coping in response to specific episodes of pain. Research on how contextual factors, such as parent responses (cf. Frank, Blount, Smith, Manimala, & Martin, 1995; Walker, Claar, & Garber, 2002), and dispositional factors interact to produce coping will provide useful information for the design of interventions to enhance children’s pain coping skills. Our findings further suggest that accommodative strategies, such as acceptance and positive reappraisal, may be useful in regulating children’s negative affect associated with chronic pain. Thus, in future research on children’s coping with chronic pain, it will be important to differentiate coping strategies beyond the dichotomy of active and passive strategies and to consider the potentially beneficial role of accommodative coping strategies.
Acknowledgments
This research was supported by National Institute on Child Health and Human Development Grants R01 HD23264 and P30 HD15052.
Footnotes
A reviewer noted that following Lazarus and Folkman (1984), to be considered coping a strategy should be effortful, and the reviewer wondered whether some of the passive strategies such as assuming the worst were sufficiently effortful to be considered coping. The point is arguable, but we believe that the passive strategies we assessed do qualify as coping as intended by Lazarus and Folkman. Effort was included as a criterion for coping to distinguish coping from both automatized adjustive behaviors and unconscious defense mechanisms (cf. Lazarus & Folkman, 1984). In our view, cognitions such as assuming the worst are not unconscious and need not be automatized. Furthermore, these cognitions are consistent with existing conceptualizations of passive coping with pain (e.g., Brown & Nicassio, 1987). Thus, we opted to risk being overly inclusive, rather than overly exclusive, in our conceptualization of coping.
This assumption and the other simplifying assumptions we describe were made to keep the initial model we tested as simple and as straightforward as possible, while still doing justice to the more general model depicted in Figure 1. In addition to considerations of parsimony, this was done in light of the relatively small number of observations we had available to test our model (see Method section). Our reasoning was that, all else being equal, a simpler model would have a greater likelihood of converging into a stable solution than a more complicated model. As discussed in the analysis overview, sample-size considerations also led us to model observed indicators instead of attempting to model latent constructs.
Of the 21 participants with incomplete data, 11 did not report an episode of pain during the week of diary interviews, and 10 were lost to follow-up because of either inability to contact the family (e.g., due to disconnected telephones) or because the family declined to participate because of inadequate time available.
Administration of measures at the clinic and by telephone was designed to maximize the equivalence of the procedures. In both instances, the interviewer read the questions to the child and the child selected responses from a printed sheet that listed response options for each measure (these response sheets were mailed to children prior to the telephone interview).
The original version of the Index of Somatic Symptoms (cf. Walker at al., 2001) included a seventh item, “stomach ache.” This item was omitted in the present study because our explicit focus was on an episode involving a stomach ache, and thus ratings on this item could be presumed to be high. Moreover, in this study, we were primarily interested in the degree to which the abdominal pain episode was accompanied by additional somatic symptoms.
The fact that this model fit was achieved without adding paths from additional dispositional variables to the episode-specific appraisal and coping variables suggests reasonable predictive and discriminant validity among the appraisal and coping constructs. However, as a more direct test of the discriminant validity within the appraisal and coping constructs, respectively, two follow-up analyses were performed. In both analyses, the final model was retested, but in the first analysis, episode-specific EFCP was predicted by dispositional PFCP and episode-specific PFCP was predicted by dispositional EFCP, and in the second analysis, each of the three episode-specific coping strategies was predicted by the two dispositional coping strategies other than its counterpart (e.g., episode-specific accommodative coping was predicted by dispositional active and passive coping but not by dispositional accommodative coping). In both analyses, the modified models showed evidence of fitting less well than the final theoretically based model: for the model with the switched predictors of appraised coping potential, χ2(75, N = 133) = 167.1, p < .01, χ2:df = 2.23, CFI = .87, RMSEA = .10, and for the one with the altered predictors of episode-specific coping, χ2(72, N = 133) = 202.2, p < .01, χ2:df = 2.81, CFI = .82, RMSEA = .12. These results provide further support for the discriminant validity of the appraisal and coping constructs.
Contributor Information
Lynn S. Walker, Division of Adolescent Medicine and Behavioral Science, Department of Pediatrics, Vanderbilt University School of Medicine
Craig A. Smith, Department of Psychology and Human Development, Vanderbilt University
Judy Garber, Department of Psychology and Human Development, Vanderbilt University.
Robyn Lewis Claar, Department of Psychology and Human Development, Vanderbilt University.
References
- Apley J. The child with abdominal pains. London: Blackwell; 1975. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Wu EJC. EQS for Macintosh: User’s guide [Computer software manual] Encino, CA: Multivariate Software; 1995. [Google Scholar]
- Bollen KA. Structural equations with latent variables. Oxford, England: Wiley; 1989. [Google Scholar]
- Brown GK, Nicassio PM. Development of a questionnaire for the assessment of active and passive coping strategies in chronic pain patients. Pain. 1987;31:53–63. doi: 10.1016/0304-3959(87)90006-6. [DOI] [PubMed] [Google Scholar]
- Brown GK, Nicassio PM, Wallston KA. Pain coping strategies and depression in rheumatoid arthritis. Journal of Consulting and Clinical Psychology. 1989;57:652–657. doi: 10.1037//0022-006x.57.5.652. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudek R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Bursch B, Walco GA, Zeltzer L. Clinical assessment and management of chronic pain and pain-associated disability syndrome. Developmental and Behavioral Pediatrics. 1998;19:45–53. doi: 10.1097/00004703-199802000-00008. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF. Situational coping and coping dispositions in a stressful transaction. Journal of Personality and Social Psychology. 1994;66:184–195. doi: 10.1037//0022-3514.66.1.184. [DOI] [PubMed] [Google Scholar]
- Church AT, Burke PJ. Exploratory and confirmatory tests of the Big Five and Tellegen’s three- and four-dimensional models. Journal of Personality and Social Psychology. 1994;66:93–114. doi: 10.1037//0022-3514.66.1.93. [DOI] [PubMed] [Google Scholar]
- Claar RL, Walker LS, Smith CA. The influence of appraisals in understanding children’s experiences with medical procedures. Journal of Pediatric Psychology. 2002;27:553–563. doi: 10.1093/jpepsy/27.7.553. [DOI] [PubMed] [Google Scholar]
- Folkman S. Personal control and stress and coping processes: A theoretical analysis. Journal of Personality and Social Psychology. 1984;46:839–852. doi: 10.1037//0022-3514.46.4.839. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology. 1986;50:992–1003. doi: 10.1037//0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- Frank NC, Blount RL, Smith AJ, Manimala MR, Martin JK. Parent and staff behavior, previous child medical experience, and maternal anxiety as they relate to child procedural distress and coping. Journal of Pediatric Psychology. 1995;20:277–289. doi: 10.1093/jpepsy/20.3.277. [DOI] [PubMed] [Google Scholar]
- Garber J, Walker LS, Zeman JL. Somatization symptoms in a community sample of children and adolescents: Further validation of the Children’s Somatization Inventory. Psychological Assessment. 1991;3:588–595. [Google Scholar]
- Gil KM, Williams DA, Thompson RJ, Kinney TR. Sickle cell disease in children and adolescents: The relation of child and parent pain coping strategies to adjustment. Journal of Pediatric Psychology. 1991;16:643–663. doi: 10.1093/jpepsy/16.5.643. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child–clinical and pediatric psychology literatures. Journal of Consulting and Clinical Psychology. 1997;65:599–610. doi: 10.1037//0022-006x.65.4.599. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;4:424–453. [Google Scholar]
- Jensen MP, Turner JA, Romano JM. Self-efficacy and outcome expectancies: Relationship to chronic pain coping strategies and adjustment. Pain. 1991;44:263–269. doi: 10.1016/0304-3959(91)90095-F. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica. 1981;46(Suppl 5–6):305–315. [PubMed] [Google Scholar]
- Kovacs M, Beck AT. An empirical–clinical approach toward a definition of childhood depression. In: Schulterbrandt J, Raskin A, editors. Depression in childhood: Diagnosis, treatment, and conceptual models. New York: Raven Press; 1977. pp. 1–25. [Google Scholar]
- La Du TJ, Tanaka JS. Influence of samples size, estimation methods, and model specification on goodness-of-fit assessments in structural equation modeling. Journal of Applied Psychology. 1989;74:625–635. [Google Scholar]
- Lazarus RS. Emotion and adaptation. New York: Oxford University Press; 1991. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Lefebvre JC, Keefe FJ, Affleck G, Raezer LB, Starr K, Caldwell DS, Tennen H. The relationship of arthritis self-efficacy to daily pain, daily mood, and daily pain coping in rheumatoid arthritis patients. Pain. 1999;80:425–435. doi: 10.1016/s0304-3959(98)00242-5. [DOI] [PubMed] [Google Scholar]
- Marsh HW, Hocevar D. Application of confirmatory factor analysis to the study of self-concept: First- and higher order factor models and their invariance across groups. Psychological Bulletin. 1985;97:562–582. [Google Scholar]
- McCracken LM. Learning to live with the pain: Acceptance of pain predicts adjustment in persons with chronic pain. Pain. 1998;74:21–27. doi: 10.1016/S0304-3959(97)00146-2. [DOI] [PubMed] [Google Scholar]
- McGrath PA. Pain in children: Nature, assessment, and treatment. New York: Guilford Press; 1994. [Google Scholar]
- Monroe SM, Kelley JM. Measurement of stress appraisal. In: Cohen S, Kessler R, Gordon L, editors. Measuring stress: A guide for health and social scientists. New York: Oxford University Press; 1995. pp. 122–147. [Google Scholar]
- Peyrot M. Causal analysis: Theory and application. Journal of Pediatric Psychology. 1996;21:3–24. doi: 10.1093/jpepsy/21.1.3. [DOI] [PubMed] [Google Scholar]
- Philips HC. Avoidance behaviour and its role in sustaining chronic pain. Behaviour Research and Therapy. 1987;25:273–279. doi: 10.1016/0005-7967(87)90005-2. [DOI] [PubMed] [Google Scholar]
- Ptacek JT, Gross S. Coping as an individual difference variable. In: Pierce GR, et al., editors. Sourcebook of social support and personality. New York: Plenum/Kluwer Academic; 1997. pp. 69–92. [Google Scholar]
- Rudolph KD, Dennig MD, Weisz JR. Determinants and consequences of children’s coping in the medical setting: Conceptualization, review, and critique. Psychological Bulletin. 1995;118:328–357. doi: 10.1037/0033-2909.118.3.328. [DOI] [PubMed] [Google Scholar]
- Saylor CF, Finch AJ, Jr, Spirito A, Bennett B. The Children’s Depression Inventory: A systematic evaluation of psychometric properties. Journal of Consulting and Clinical Psychology. 1984;52:955–967. doi: 10.1037//0022-006x.52.6.955. [DOI] [PubMed] [Google Scholar]
- Schwartz JE, Neale J, Marco C, Shiffman SS, Stone A. Does trait coping exist? A momentary assessment approach to the evaluation of traits. Journal of Personality and Social Psychology. 1999;77:360–369. doi: 10.1037//0022-3514.77.2.360. [DOI] [PubMed] [Google Scholar]
- Smith CA, Lazarus RS. Emotion and adaptation. In: Pervin LA, editor. Handbook of personality: Theory and research. New York: Guilford Press; 1990. pp. 609–637. [Google Scholar]
- Smith CA, Wallston KA, Dwyer KA. Coping and adjustment to rheumatoid arthritis. In: Suls J, Wallston KA, editors. Social psychological foundations of health and illness. Malden, MA: Blackwell; 2003. pp. 458–494. [Google Scholar]
- Smith CA, Wallston KA, Dwyer KA, Dowdy SW. Beyond good and bad coping: A multidimensional examination of coping with pain in persons with rheumatoid arthritis. Annals of Behavioral Medicine. 1997;19:11–21. doi: 10.1007/BF02883422. [DOI] [PubMed] [Google Scholar]
- Thompson RJ, Gil KM, Abrams MR, Phillips G. Stress, coping, and psychological adjustment of adults with sickle cell disease. Journal of Consulting and Clinical Psychology. 1992;60:433–440. doi: 10.1037//0022-006x.60.3.433. [DOI] [PubMed] [Google Scholar]
- Thomsen AH, Compas BE, Colletti RB, Stanger C, Boyer MC, Konik BS. Coping and stress responses in children with recurrent abdominal pain. Journal of Pediatric Psychology. 2002;27:215–226. doi: 10.1093/jpepsy/27.3.215. [DOI] [PubMed] [Google Scholar]
- Turk DC, Rudy TE. Toward an empirically derived taxonomy of chronic pain patients: Integration of psychological assessment data. Journal of Consulting and Clinical Psychology. 1988;56:233–238. doi: 10.1037//0022-006x.56.2.233. [DOI] [PubMed] [Google Scholar]
- Turner JA. Coping and chronic pain. In: Bond MR, Charlton JE, Woolf CJ, editors. Pain research and clinical management: Vol. 4. Proceedings of the 6th World Congress on Pain. New York: Elsevier; 1991. pp. 219–227. [Google Scholar]
- Van Slyke DA. Unpublished doctoral dissertation. Vanderbilt University; 2001. Parent influences on children’s pain behavior. [Google Scholar]
- Walker LS. The evolution of research on recurrent abdominal pain: History, assumptions and new directions. In: McGrath PJ, Finley GA, editors. Chronic and recurrent pain in children and adolescents. Seattle, WA: International Association for the Study of Pain; 1999. pp. 141–172. [Google Scholar]
- Walker LS, Claar RL, Garber J. Social consequences of children’s pain: When do they encourage symptom maintenance? Journal of Pediatric Psychology. 2002;27:689–698. doi: 10.1093/jpepsy/27.8.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker LS, Garber J. Manual for the Children’s Somatization Inventory. Nashville, TN: Vanderbilt University Medical Center, Department of Pediatrics; 2003. [Google Scholar]
- Walker LS, Garber J, Greene JW. Somatization symptoms in pediatric abdominal pain patients: Relation to chronicity of abdominal pain and parent somatization. Journal of Abnormal Child Psychology. 1991;19:379–394. doi: 10.1007/BF00919084. [DOI] [PubMed] [Google Scholar]
- Walker LS, Garber J, Greene JW. Psychosocial correlates of recurrent childhood pain: A comparison of pediatric patients with recurrent abdominal pain, organic illness, and psychiatric disorders. Journal of Abnormal Psychology. 1993;102:248–258. doi: 10.1037//0021-843x.102.2.248. [DOI] [PubMed] [Google Scholar]
- Walker LS, Greene JW. The Functional Disability Inventory: Measuring a neglected dimension of child health status. Journal of Pediatric Psychology. 1991;16:39–58. doi: 10.1093/jpepsy/16.1.39. [DOI] [PubMed] [Google Scholar]
- Walker LS, Smith CA, Garber J, Van Slyke DA. Development and validation of the Pain Response Inventory for children. Psychological Assessment. 1997;9:392–405. [Google Scholar]
- Walker LS, Smith CA, Garber J, Van Slyke DA, Claar R. The relation of daily stressors to somatic and emotional symptoms in children with recurrent abdominal pain. Journal of Consulting and Clinical Psychology. 2001;69:85–91. [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Zeltzer L, Feldman S. Soothing and chronic pain. In: Lewis M, Ramsay D, editors. Soothing and stress. Mahwah, NJ: Erlbaum; 1999. pp. 195–227. [Google Scholar]