Abstract
Background
The importance of exchanging sucrose for artificial sweeteners on risk factors for developing diabetes and cardiovascular diseases is not yet clear.
Objective
To investigate the effects of a diet high in sucrose versus a diet high in artificial sweeteners on fasting and postprandial metabolic profiles after 10 weeks.
Design
Healthy overweight subjects were randomised to consume drinks and foods sweetened with either sucrose (∼2 g/kg body weight) (n = 12) or artificial sweeteners (n = 11) as supplements to their usual diet. Supplements were similar on the two diets and consisted of beverages (∼80 weight%) and solid foods (yoghurts, marmalade, ice cream, stewed fruits). The rest of the diet was free of choice and ad libitum. Before (week 0) and after the intervention (week 10) fasting blood samples were drawn and in week 10, postprandial blood was sampled during an 8-hour meal test (breakfast and lunch).
Results
After 10 weeks postprandial glucose, insulin, lactate, triglyceride, leptin, glucagon, and GLP-1 were all significantly higher in the sucrose compared with the sweetener group. After adjusting for differences in body weight changes and fasting values (week 10), postprandial glucose, lactate, insulin, GIP, and GLP-1 were significantly higher and after further adjusting for differences in energy and sucrose intake, postprandial lactate, insulin, GIP, and GLP-1 levels were still significantly higher on the sucrose-rich diet.
Conclusion
A sucrose-rich diet consumed for 10 weeks resulted in significant elevations of postprandial glycaemia, insulinemia, and lipidemia compared to a diet rich in artificial sweeteners in slightly overweight healthy subjects.
Keywords: glucose, insulin, leptin, triacylglycerol, NEFA, GLP-1, GIP, meal test, overweight
The effect on health of a high intake of sugars (fructose, sucrose, high-fructose corn syrup) is still subject to scientific and public debate. Currently, a high intake of dietary sucrose and fructose coincides with the worldwide pandemic of obesity, type-2 diabetes, and cardiovascular diseases, and this has increased the concerns about the possible adverse effects of excessive sugar consumption (1, 2).
In general, it is recommended to limit the intake of added sugars to below 10 E% primarily to ensure an adequate intake of micronutrients (3, 4), which can be problematic in population groups with relatively small energy requirements (children and elderly) (5, 6). However, several other problems may arise from a large consumption of sugars. Firstly, a relatively large consumption of sugars, especially in the form of liquid sugar, has been shown to result in increased energy intake and body weight. This has been explained by subjects being unable to compensate properly for the energy and thus consuming excess amounts of energy when sugars are consumed as soft drinks (7–9). Secondly, large cohort studies have linked a high intake of sugar-sweetened beverages to an increased risk of developing type-2 diabetes (10–12) and both human and animal intervention studies have demonstrated decreased insulin sensitivity after consumption of a high-sucrose diet (13–16). Thirdly, recent studies have linked sucrose and fructose intake to the development of lipid dysregulation, visceral adiposity, hypertension, inflammation, and clinical coronary heart disease (16–18). In order to avoid excessive intake of calories and the ensuing health hazards, it would therefore seem prudent to exchange sucrose for a non-calorie containing alternative such as artificial sweeteners. Due to the scarcity of publications in this area, the actual efficiency of this practice in the longer term is, however, still unclear. The aim of the present study was to investigate the effects of sucrose versus artificial sweeteners on the fasting and postprandial metabolic profiles after 10 weeks’ intervention in slightly overweight subjects.
Subjects and methods
Experimental design
The study was designed as a 10 week parallel intervention study with two groups randomised to receive supplemental drinks and foods containing either sucrose or artificial sweeteners. Subjects consumed these as part of their daily food intake and collected the supplements at the Department of Human Nutrition every week. Subjects were not informed about the true purpose of the study, but were all told that they would receive supplements containing artificial sweeteners. The study comprised a main group of 41 subjects and a representative subgroup of 23 subjects. The present paper reports data from the subgroup. Data on the main group have been reported previously (8, 19). In this sub-study additional measurements of fasting and postprandial metabolic profiles were performed on a total of 23 subjects (19 women and 4 men).
Fasting blood was sampled in week 0 and 10 and postprandial blood sampled during an 8-hour meal test in week 10 (day 70). Height, waist-to-hip ratio, sagittal height, and blood pressure were measured in week 0. Measures of body weight and composition were conducted in week 0, 2, 4, 6, 8, and 10. The subjects spend the day and night before the blood sampling days in a respiratory chamber (data not included here). In the morning (9 am) body weight and waist-to-hip ratio were measured after voiding. After 10 min of resting in a supine position blood pressure, body composition, and sagittal height were measured. A venflon catheter was inserted in an antecubital arm vein and after another 10 min fasting blood samples were drawn. On the meal test day (week 10), subjects subsequently received breakfast (10 am) and lunch (2 pm) at the Department. The breakfast and lunch were precise reproductions of what the subjects consumed the previous day, where they could eat ad libitum from menus selected in the respiratory chamber. The supplemental foods were eaten at breakfast and the supplemental beverages both at breakfast and lunch. Subjects were asked to use a maximum of 20 min to eat the meals. After the meals, subjects were allowed to move quietly around, read, and watch television. Postprandial blood samples were drawn at 30, 45, 60, 120, 180, 240 (just before lunch), 270, 285, 300, 360, 420, and 480 min after breakfast. Subjects rested in a supine position 10 min before each blood sampling.
Subjects
The inclusion criteria were: 20–50 years of age, overweight (BMI of 25–30 kg/m2 or >10% overweight according to weight and height tables (20), healthy, not dieting, and for women not pregnant or lactating. The two study groups, the sucrose group (n=12) and the sweetener group (n=11) were well matched at baseline regarding gender, anthropometric measures, blood pressure, and physical activity (Table 1). The study was approved by the Municipal Ethical Committee of Copenhagen and Frederiksberg as being in accordance with the Helsinki II Declaration. All subjects gave written informed consent after the experimental procedures had been explained to them orally and in writing.
Table 1.
Characteristics of subjects at baseline (week 0)1
| Sucrose group (n=12) | Sweetener group (n=11) | |
|---|---|---|
| Age (years) | 35.3±2.8 | 35.5±3.6 |
| Body weight (kg) | 84.5±2.4 | 80.1±2.9 |
| Height (cm) | 171.8±2.0 | 170.5±2.2 |
| BMI (kg/m2) | 28.7±0.7 | 27.6±0.8 |
| Fat mass (kg) | 31.2±1.1 | 27.5±1.4 |
| Fat mass (%) | 36.9±0.9 | 34.4±1.4 |
| Fat-free mass (kg) | 53.3±1.7 | 52.6±2.4 |
| Fat-free mass (%) | 63.1±0.9 | 65.6±1.4 |
| Waist-to-hip ratio | 0.78±0.02 | 0.79±0.03 |
| Sagittal height (cm) | 20.8±0.7 | 20.4±0.7 |
| Systolic BP (mmHg) | 119.5±4.0 | 116.6±1.9 |
| Diastolic BP (mmHg) | 72.6±3.6 | 72.0±2.7 |
| Physical activity (h/wk) | 8.7±2.5 | 12.1±2.8 |
| Physical activity level2 | 2.9±0.3 | 3.1±0.2 |
Mean±SEM. BP: blood pressure. No significant differences between groups (unpaired t-test).
elf-reported, rated from 1 to 5, with 1=low and 5=high.
Experimental diets
Diets have been described in detail before (8). In brief, subjects in the sucrose group were instructed to consume an amount of sucrose corresponding to about 2 g sucrose/kg body weight and similar amounts of artificially sweetened beverages and foods were given to the sweetener group. For an 80 kg person with an energy intake of 12 MJ/d this meant 23% of energy from sucrose. The beverages accounted for about 80% and solid foods for about 20% by weight of the supplements. The beverages consisted of soft drinks (Coca Cola, Fanta, and Sprite – all from Coca Cola Tapperierne A/S, Fredericia, Denmark) and flavoured fruit juices (orange, raspberry, ‘sport’, and mixed). The caps were changed and all labels were removed to hinder subjects from guessing which drinks were ‘light’. The solid foods consisted of yoghurt (strawberry, Peach Alexander, and cherry for the sucrose group or strawberry-rhubarb, Peach Melba, and forest berries for the sweetener group), jam (orange, raspberry, and black currant), ice cream (strawberry, pistachio, and vanilla), and canned fruits (apricots, prunes, and apples). Except for the yoghurts the types of beverages and foods in the two groups were matched. Because some of the artificially sweetened products were fat-reduced, the sweetener group was given additional butter or corn oil to make the fat intake in the groups as similar as possible. Besides the experimental diet, subjects were allowed to freely consume their habitual diet throughout the intervention period.
Food intake was measured by 7 day dietary records at week 0, 5, and 10. Digital food scales with an accuracy of 1g were used (Soehnle 8020 and 8009; Soehnle-Waagen GmbH & Co, Murrhardt, Germany). The computer database of foods from the National Food Agency of Denmark (Dankost 2.0) was used to calculate the energy and nutrient intakes (21). On the meal test day the breakfast contained different types of bread, butter, cheese, fruit juice, cereals, and milk. The lunch consisted of different types of bread, butter, cheese, vegetables, sandwich spread with meat and fish, eggs, and milk. The supplemental foods were consumed at breakfast and the supplemental beverages both at breakfast and lunch.
Anthropometry and blood pressure
Body weight was measured to the nearest 0.1 kg with a digital scale (Seca model 708; Seca Mess und Wiegetechnik, Vogel & Halke GmbH & Co, Hamburg, Germany). Body composition was estimated with the bioelectrical impedance method using an Animeter (HTS-Engineering Inc, Odense, Denmark). Fat mass (FM) and fat-free mass (FFM) were calculated as described previously (22). Height was measured to the nearest 0.5 cm before intervention using a wall-monitored stadiometer. Waist and hip circumferences were measured with a tape measure. Sagittal height was measured in the supine position to the nearest 0.5 cm. Blood pressure was also measured in the supine position after 10 min of rest with an automatically inflating cuff (UA-743, A&D Company Ldt, Tokyo).
Laboratory analyses
Blood drawn fasting and postprandially was analysed for concentrations of glucose, lactate, insulin, non-esterified fatty acids (NEFA), triacylglycerol (TAG), total cholesterol, high density lipoprotein (HDL), glucagon, glucose-dependent insulinotropic polypeptide (GIP), glucagon-like peptide-1 (GLP-1), and leptin. Blood was sampled without stasis through an indwelling catheter into iced syringes. Within 30 min, samples were centrifuged for 10 min at 3000×g and 4°C, and the supernatant fluid was stored at –80 or –20°C until analysed.
Blood for determination of plasma glucose and lactate was collected in flouride-EDTA prepared tubes (Vacurette; Greiner labortechnik; Kremsmoenster, Austria) and was analysed by standard end-point enzymatic methods (MPR3 Gluco-Quant Glucose/HK and MPR3 Hexokinase/G&P-DH test kits; Boehringer Mannheim GmbH Diagnostica, Copenhagen) (23, 24).
Blood for insulin analysis was sampled in dry tubes. Determination of serum insulin was done with an enzyme-linked immunosorbent assay using a non-competitive sandwich assay (25) with a DAKO RIA insulin kit (DAKO A/S, Glostrup, Denmark). The NEFA concentration in plasma was measured by enzymatic quantitative colorimetric method (Wako NEFA test kit, NEFA C, ACS-ACOP method; Wako Chemicals GmbH, Germany). Concentration of serum TAG was analysed by an enzymatic endpoint method (Test-Combination Triacylglycerol (GPO-PAP) kit; Boehringer Mannheim GmbH Diagnostica, Copenhagen) (26). Cholesterol and HDL serum concentrations were measured using the enzymatic kolorimetric Monotest Cholesterol High Performance CHOD-PAP method (Boehringer Mannheim GmbH Diagnostica, Copenhagen) and the HDL-Cholesterol precipitant method (supplementary pack to the Monotest Cholestrol High Performance CHOD-PAP method, Boehringer Mannheim GmbH Diagnostica, Copenhagen).
The GIP, GLP-1, and glucagon concentrations in plasma were all measured after extraction of plasma with 70% ethanol (vol/vol, final concentration). For the GIP radioimmunoassay (27) we used the C-terminally directed antiserum R 65, which cross-reacts fully with human GIP. Human GIP and 125-I human GIP (70 MBq/nmol) were used for standards and tracer. The plasma concentrations of GLP-1 were measured (28) against standards of synthetic GLP-1 7-36amide using antiserum code no. 89390. The glucagon radio-immunoassay (29) was directed against the C-terminus of the glucagon molecule (antibody code no. 4305). Leptin was analysed using radio-immunoassay and an Automatic Gamma Counter (DRG Human Leptin RIA Kit (RIA-1624) 1272 Clinigamma LKB Wallac Four 1½ Detectors).
Statistical analyses
All results are given as means±SEM. All statistical analyses were performed in SAS version 8 (SAS Institute, Cary, NC). Estimates of insulin resistance and pancreatic β-cell function, introduced as a Homeostasis Model Assessment (HOMA) by Matthews et al. (30) were used as indices of insulin resistance:
HOMA-R (relative insulin resistance)=glucose (mmol/l)×insulin (µU/l)/22.5.
HOMA-ß (ß-cell function)=20×insulin (µmU/ml)/glucose (mmol/l) – 3.5.
The Incremental areas under the curves (iAUC) was calculated for all postprandial blood measures separately for each subject as the difference between the integrated area of the response curve and the rectangular area above or below fasting concentrations. Differences between groups in subject characteristics, daily energy intake and macronutrient composition at baseline (week 0) were analysed using Student's unpaired t-tests.
The average daily energy and macronutrient intakes (from food dairies, week 0, 5, and 10) and the body weight and body composition of the sucrose and the sweetener group were analysed using repeated measurements analyses (PROC MIXED in SAS) testing the effect of group (diet), time (week), and group×time interaction. Baseline value was used as a cofactor in analyses of body weight and body composition.
Differences in fasting concentration of blood parameters, HOMA-R, HOMA-β between groups were analysed using Student's unpaired t-test. Changes from week 0 to 10 between groups were analysed using covariance test first with baseline value as a cofactor and subsequently also with changes in body weight as a cofactor (PROC GLM in SAS). Differences between groups in energy and macronutrient intakes at the meal test day (breakfast, lunch, and breakfast+lunch) and sensory evaluation of the meals were analysed using Student's unpaired t-tests.
Repeated measurements analyses (PROC MIXED in SAS) over time during the meal test day were used for analyses of postprandial blood parameters. The effects of group, time (min) and group×time were tested with and without changes in body weight, fasting value (week 10), and energy and sucrose intake on the test day (week 10) as cofactors in the analyses. For all repeated measurement analyses, the model was reduced when the group×time interaction was insignificant and Tukey-Kramers adjusted post hoc tests were applied where appropriate. The iAUC were analysed using Analyses of variance (ANOVA) (PROC GLM in SAS) with group as a factor. The level of significance was P<0.05.
Results
Changes during the 10 week intervention were as follows.
Dietary intake
In week 0 the groups were well matched with regard to energy and macronutrient intake (Table 2). During the intervention, energy and macronutrient intake did not change in the sweetener group. However, in the sucrose group the intake of sucrose increased by 161% and of carbohydrate by 31% from week 0 to 10 and in week 10, energy intake was 32% higher compared with the sweetener group (p<0.01). The amount (gram) of consumed protein, dietary fibre, total fat or alcohol did not differ between groups at any time, but energy density increased significantly on the sucrose compared with the sweetener diet (p<0.01). A similar dietary pattern was evident on the meal test day in week 10 (Table 3).
Table 2.
Average daily energy and macronutrient intakes in the sucrose and sweetener groups at baseline (week 0) and during the intervention (week 5 and week 10)1
| P (ANOVA) | |||||||
|---|---|---|---|---|---|---|---|
| Week 0 | Week 5 | Week 10 | Group×time | Group | Time | ||
| Energy (kJ/d) | Sucrose | 10219±886 | 10984±8553 | 11759±8664 | NS | 0.02 | NS |
| Sweetener | 9378±597 | 8630±708 | 8909±337 | ||||
| Carbohydrate (g/d) | Sucrose | 294±33a | 383±29b,5 | 386±24b,5 | 0.0033 | <0.001 | NS |
| Sweetener | 258±14 | 232±20 | 245±9 | ||||
| Carbohydrate (E%)2 | Sucrose | 48±2a | 60±1b,5 | 56±1b,5 | <0.001 | <0.001 | <0.001 |
| Sweetener | 48±2 | 46±2 | 47±2 | ||||
| Sucrose (g/d) | Sucrose | 69±22a | 189±14b,5 | 180±7b,5 | <0.001 | <0.001 | <0.001 |
| Sweetener | 50±8 | 23±4 | 27±5 | ||||
| Sucrose (E%) | Sucrose | 10±2a | 30±1b,5 | 27±1b,5 | <0.001 | <0.001 | <0.001 |
| Sweetener | 9±1 | 4±1 | 5±1 | ||||
| Dietary fibre (g/d) | Sucrose | 20±2 | 21±2 | 20±2 | NS | NS | NS |
| Sweetener | 19±2 | 21±2 | 22±2 | ||||
| Fat (g/d) | Sucrose | 91±7 | 80±8 | 90±8 | NS | NS | NS |
| Sweetener | 86±10 | 78±9 | 77±6 | ||||
| Fat (E%) | Sucrose | 35±1a | 28±1b | 29±1ab | 0.02 | NS | 0.01 |
| Sweetener | 34±2 | 34±2 | 32±2 | ||||
| Protein (g/d) | Sucrose | 84±6 | 74±7 | 79±6 | NS | NS | NS |
| Sweetener | 78±4 | 74±5 | 78±4 | ||||
| Protein (E%) | Sucrose | 14±1a | 11±0b,5 | 11±0 b,5 | <0.001 | 0.003 | 0.01 |
| Sweetener | 15±1 | 15±1 | 15±1 | ||||
| Alcohol (g/d) | Sucrose | 12±2 | 9±2 | 18±5 | NS | NS | NS |
| Sweetener | 13±2 | 16±5 | 19±4 | ||||
| Alcohol (E%) | Sucrose | 4±1 | 3±13 | 4±1 | NS | NS | NS |
| Sweetener | 4±1 | 6±1 | 6±1 | ||||
| Weight of food (g/d) | Sucrose | 3098±296 | 3750±278 | 3727±318 | NS | NS | 0.009 |
| Sweetener | 3374±287 | 3614±213 | 3840±226 | ||||
| Energy density (kJ/g) | Sucrose | 3.4±0.2 | 3.0±0.1 | 3.2±0.24 | NS | 0.03 | <0.001 |
| Sweetener | 3.0±0.3 | 2.4±0.2 | 2.4±0.1 | ||||
Mean±SEM. At week 0 and 10, n=12 in the sucrose group and n=11 in the sweetener group. At week 5 n=11 in both groups. Values in the same row with different superscript letters are significantly different (repeated measurements over weeks), P<0.05.
E%, percentage of energy.
Significant difference between the sucrose and sweetener groups (ANOVA): 3P<0.05, 4P<0.01, 5P<0.001.
Table 3.
Average energy and macronutrient intakes in the sucrose and sweetener groups at breakfast and lunch on the meal test day in week 10 of the intervention1
| Breakfast | Lunch | Breakfast+lunch | ||
|---|---|---|---|---|
| Energy (kJ) | Sucrose | 4264±415 | 4531±575 | 8796±920 |
| Sweetener | 3021±438 | 3651±413 | 6672±759 | |
| Carbohydrate (g) | Sucrose | 184±202 | 126±21 | 311±362 |
| Sweetener | 113±22 | 84±7 | 197±27 | |
| Carbohydrate (E%) | Sucrose | 73±32 | 47±3 | 60±22 |
| Sweetener | 61±4 | 40±2 | 51±3 | |
| Sucrose (g) | Sucrose | 91±134 | 49±143 | 140±224 |
| Sweetener | 10±7 | 0±0 | 10±7 | |
| Sucrose (E%) | Sucrose | 35±34 | 18±34 | 26±34 |
| Sweetener | 3±2 | 0±0 | 2±1 | |
| Dietary fibre (g) | Sucrose | 7±1 | 13±1 | 20±2 |
| Sweetener | 8±1 | 15±1 | 22±2 | |
| Fat (g) | Sucrose | 21±4 | 44±6 | 65±9 |
| Sweetener | 17±3 | 39±7 | 56±10 | |
| Fat (E%) | Sucrose | 18±2 | 37±3 | 28±2 |
| Sweetener | 22±3 | 39±3 | 30±3 | |
| Protein (g) | Sucrose | 31±3 | 38±6 | 69±8 |
| Sweetener | 30±3 | 36±4 | 66±7 | |
| Protein (E%) | Sucrose | 13±13 | 14±1 | 13±13 |
| Sweetener | 19±2 | 17±1 | 18±1 | |
| Energy density (kJ/g) | Sucrose | 3.5±0.23 | 3.6±0.3 | 3.5±0.2 |
| Sweetener | 2.7±0.2 | 3.6±0.4 | 3.1±0.2 |
Mean±SEM. E%, percentage of energy. n=12 in the sucrose group and n=11 in the sweetener group.
Significant difference between the sucrose and sweetener groups (Student's unpaired t-test): 2P<0.05, 3P<0.01, 4P<0.001.
Body weight and body composition
Analysis on body weight during the intervention showed a significant group×week effect (P=0.03) with a body weight increase in the sucrose group (by 1.4±0.6 kg in week 10) compared with the sweetener group (−1.5±0.6 kg in week 10). When analysing FM and lean body mass (in kg and percentage), no significant differences were found between groups (data not shown).
Fasting blood concentrations
Fasting concentrations of blood parameters and HOMA-R and HOMA-β are shown in Table 4 (p-values for changes are corrected for fasting values in week 0). In week 0 fasting concentrations between groups were not significantly different, except for a higher GLP-1 in the sucrose group (P<0.001). Changes from week 0 to 10 showed an increase in fasting concentrations of insulin (P<0.05), GIP (p<0.05), and leptin (P<0.001) in the sucrose group compared with the sweetener group. There was also a tendency towards a difference in HOMA-R (p=0.051) and HOMA-ß, p=0.06). When change in body weight was also used as cofactor in the analyses, all differences between groups became non-significant. In week 10 total fasting TAG was significantly higher in the sucrose group (P<0.05), but the changes from week 0 to 10 were not different between groups.
Table 4.
Fasting plasma or serum concentrations of blood parameters, HOMA-R and HOMA-β in week 0 and week 10, and changes between week 0 and week 10 of the intervention1
| Week 0 | Week 10 | Change2 | ||
|---|---|---|---|---|
| Glucose (mmol/l) | Sucrose | 4.68±0.11 | 4.92±0.12 | 0.24±0.09 |
| Sweetener | 4.78±0.08 | 4.87±0.13 | 0.09±0.15 | |
| Insulin (pmol/l) | Sucrose | 41.8±5.3 | 53.6±7.9 | 11.8±4.93 |
| Sweetener | 37.0±5.3 | 35.8±4.8 | –1.2±3.2 | |
| Lactate (mmol/l) | Sucrose | 1.09±0.14 | 1.11±0.13 | 0.02±0.08 |
| Sweetener | 0.83±0.05 | 0.89±0.12 | 0.06±0.10 | |
| NEFA (µmol/l) | Sucrose | 595±44 | 532±35 | –63±33 |
| Sweetener | 535±53 | 524±69 | –10±80 | |
| TAG (mmol/l) | Sucrose | 1.48±0.18 | 1.75±0.243 | 0.27±0.12 |
| Sweetener | 1.07±0.12 | 1.01±0.14 | –0.05±0.17 | |
| Total cholesterol (mmol/l) | Sucrose | 5.20±0.30 | 5.07±0.29 | –0.13±0.19 |
| Sweetener | 5.28±0.32 | 5.26±0.36 | –0.02±0.17 | |
| HDL-cholesterol (mmol/l) | Sucrose | 1.31±0.06 | 1.34±0.07 | 0.03±0.06 |
| Sweetener | 1.47±0.12 | 1.47±0.13 | 0.00±0.05 | |
| Glucagon (pmol/l) | Sucrose | 3.2±0.4 | 4.0±0.5 | 0.8±0.4 |
| Sweetener | 2.9±0.4 | 3.2±0.4 | 0.4±0.6 | |
| GIP (pmol/l) | Sucrose | 8.8±2.2 | 9.8±1.73 | 1.0±2.03 |
| Sweetener | 7.6±1.9 | 5.1±1.3 | –2.5±2.2 | |
| GLP-1 (pmol/l) | Sucrose | 13.3±0.95 | 13.8±0.75 | 0.4±0.5 |
| Sweetener | 8.0±0.6 | 9.4±0.7 | 1.4±0.8 | |
| Leptin (ng/ml) | Sucrose | 19.8±2.2 | 26.9±2.24 | 7.1±1.74 |
| Sweetener | 16.1±3.4 | 15.1±2.5 | –1.0±2.1 | |
| HOMA-R | Sucrose | 1.46±0.20 | 1.96±0.29 | 0.50±0.18 |
| Sweetener | 1.32±0.21 | 1.32±0.2 | 0.00±0.15 | |
| HOMA-β | Sucrose | 26.0±3.6 | 32.9±5.5 | 6.9±3.5 |
| Sweetener | 22.1±3.4 | 20.7±3.0 | –1.4±1.8 |
Mean±SEM. N=12 in the sucrose group and n=11 in sweetener group. Sucrose: sucrose group, Sweetener: sweetener group, NEFA: non-esterified fatty acids, TAG: triacylglycerol, GIP: glucose-dependent insulinotropic polypeptide, GLP-1: glucagon-like peptide-1.
Change is calculated as week 10 minus week 0. An ANOVA was performed with week 0 value as covariate.
Significant difference between sucrose and sweetener groups (ANOVA). 3P<0.05, 4P<0.01, 5P<0.001.
Postprandial blood concentrations
For all postprandial parameters, there was a significant effect of time (P<0.0001).
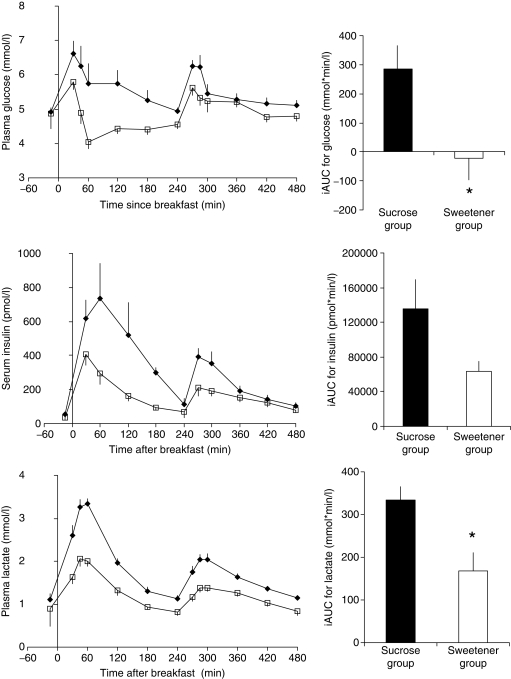
Glucose, insulin, and lactate
The responses over time on the meal test day and the iAUC for glucose, insulin, and lactate are shown in Fig. 1. Postprandial glucose response was significantly higher, especially after breakfast, in the sucrose group compared with the sweetener group (group, p<0.01). Also the iAUCs were significantly different with a slightly negative area in the sweetener group compared with a positive area in the sucrose group (p<0.05).
Fig. 1.
Mean (± SEM) plasma glucose, serum insulin, and plasma lactate concentrations and incremental areas under the curves (iAUC) for a meal test day (week 10) in two groups who received supplementation containing either sucrose (♦), n=12 or artificial sweeteners (□), n=11 for 10 weeks in addition to their habitual diet. Postprandial responses were tested by repeated measurement analysis. For all curves, the time effect was significant (P<0.0001). For glucose there was a significant group difference (p<0.01), and a difference in iAUC (p<0.05). For postprandial insulin there was a group×time effect (p<0.05), whereas the iAUC did not differ (group, p=0.06). For lactate there was a significant group×time effect (P<0.0001) and a difference in iAUC (P<0.01).
The insulin response was significantly higher in the sucrose group compared with the sweetener group, again most markedly after breakfast (group×time effect, p<0.05), but the difference in iAUC's did not reach significance (p=0.06). Also for lactate a significant group×time effect was seen (P<0.0001), due to a larger lactate concentration in the sucrose group compared with the sweetener group. The iAUC was significantly higher in the sucrose group (P<0.01).
Including fasting value and change in body weight as cofactors in the above repeated measurements analyses did not change the findings. The HOMA indices for iAUC of glucose and insulin were not significantly different, although a tendency was observed for the HOMA-R index (480×103 in the sucrose versus –50×103 in the sweetener group, p=0.065).
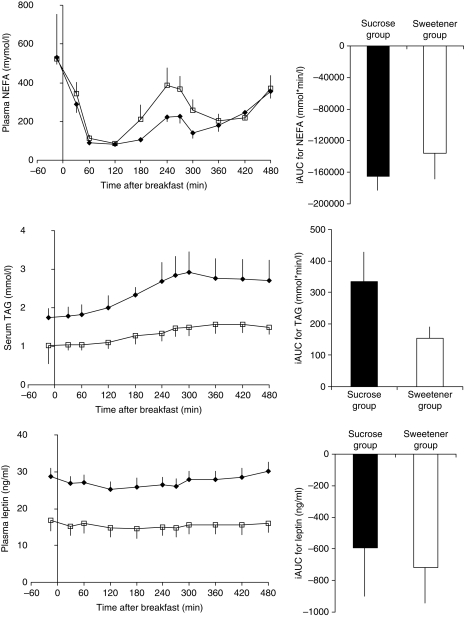
NEFA, TAG, and leptin
The postprandial responses for NEFA, TAG, and leptin are shown in Fig. 2. There were no significant differences between groups in the postprandial NEFA response. For TAG there was a significantly higher postprandial concentration in the sucrose compared with the sweetener group (group, p<0.05). The group difference became insignificant after entering the change in body weight and fasting concentrations as cofactors. Accordingly, there was no significant difference between groups in iAUC.
Fig. 2.
Mean (± SEM) plasma non-esterified fatty acids (NEFA), serum triacylglycerol (TAG), and plasma leptin concentrations and incremental areas under the curves (iAUC) for a meal test day (week 10) in two groups who received supplementation containing either sucrose (♦), n=12 or artificial sweeteners (□), n=11 for 10 weeks in addition to their habitual diet. Postprandial responses were tested by repeated measurement analysis. For all curves, the time effect was significant (P<0.001). For NEFA no significant differences were seen. For postprandial TAG and leptin, there were significant group differences (p<0.05 and p<0.001, respectively), but the iAUCs were not different.
Postprandial leptin response was significantly greater in the sucrose compared with the sweetener group, both without and with fasting concentration as a cofactor (group, P<0.001 and p<0.05, respectively). Further inclusion of changes in body weight as a cofactor made the differences non-significant (p=0.09). The iAUCs were not different between groups.
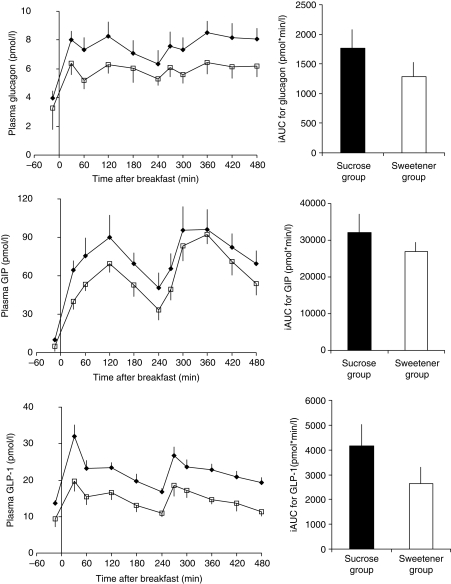
Glucagon, GIP, and GLP-1
The postprandial responses for glucagon, GIP, and GLP-1 are shown in Fig. 3. Postprandial glucagon concentrations were significantly higher in the sucrose group than in the sweetener group (group effect, p<0.05), but the iAUCs were not different. No significant differences between groups in any aspect of the GIP response were found. However, when including fasting value and changes in body weight as cofactors, there was a significant group effect (p<0.01).
Fig. 3.
Mean (± SEM) plasma glucagon, glucose-dependent insulinotropic polypeptide (GIP), and glucagon-like peptide-1 (GLP-1) concentrations and incremental areas under the curves (iAUC) for a meal test day (week 10) in two groups who received supplementation containing either sucrose (♦), n=12 or artificial sweeteners (□), n=11 for 10 weeks in addition to their habitual diet. Postprandial responses were tested by repeated measurement analysis. For all curves, the time effect was significant (P<0.0001). No differences were seen for GIP. For postprandial glucagon and GLP-1, there were significant group differences (p<0.05 and P<.0001, respectively), but no differences in iAUC.
The GLP-1 concentrations were significantly greater in the sucrose group than in the sweetener group, both without and with fasting concentration and changes in body weight as a cofactor (group effect, P<0.0001 and P<0.001, respectively). The iAUCs were not significantly different between diets.
When using fasting value, changes in body weight, energy, and sucrose intake on the test day as cofactors in the repeated measurements analyses, the differences in lactate (group×time, p<0.0001), insulin (group×time, p< 0.05), GIP (p<0.01), and GLP-1 (group, p<0.001) were significant.
Discussion
The major findings in the present study were that 10 weeks intake of a diet rich in sucrose resulted in higher postprandial concentrations of most measured blood parameters – glucose, insulin, lactate, TAG, leptin, glucagon, and GLP-1 – in healthy, overweight subjects compared to a diet rich in non-caloric artificial sweeteners. After adjusting for differences in fasting values, changes in body weight, energy, and sucrose intake in week 10, the differences were significant for lactate, insulin, GIP, and GLP-1.
A relatively large amount of sucrose, (∼28 E% or 185 g/d) was consumed in the sucrose group, mainly in the form of liquid sugar (∼80 weight%). The ensuing increase in total energy intake and body weight on that diet compared with the sweetener diet has been discussed before (8). Since changes in body weight can influence the measured blood parameters, adjustments in the statistical analyses were done in the present study to correct for this. In this way the influence of the diets per se on the blood parameters could be estimated. Still, in the real world the values not adjusted for changes in body weight will be the interesting ones, since these reflect the actual health status of the person in question. The statistical corrections are, therefore, mainly done in order to distinguish between the effects of changes in body weight and the effect of the dietary composition per se on blood concentrations.
Sucrose consists of 50:50 glucose and fructose that undergo different metabolic pathways after absorption from the small intestine. The higher postprandial glucose response on the sucrose-rich diet can be explained by the large amount of available glucose from both sucrose and starch on this diet. The rise in glucose can on the other hand partly explain the large increase in postprandial insulin levels on this diet. Part of the insulin increase may, however, have been induced by the higher postprandial GLP-1 responses in the sucrose group compared to the sweetener group. It can be speculated that the constantly high energy intake in the sucrose group throughout the intervention has facilitated the secretion of GLP-1 by increasing the responsiveness to macronutrients in the small intestine (31). However, after adjusting for differences in energy and sucrose intake on the meal test day, both insulin and GLP-1 concentrations remained significantly higher in the sucrose group. Thus, other factors may have played a role. The fact that GIP became significantly higher on the sucrose diet after adjusting for differences in fasting values, changes in body weight, sucrose, and energy intake also indicates that other factors played a role in the release of GIP on that diet compared with the sweetener diet.
From the fasting results in our study, there was a tendency that the sucrose-rich diet lead to reduced insulin sensitivity after 10 week. This tendency disappeared, however, after adjusting for changes in body weight. In some previous studies, no differences in insulin sensitivity were found when subjects were exposed to sucrose or starch for up to 24 days (15, 32–34). In contrast, a recent study of 10 weeks duration showed a decrease in insulin sensitivity after consumption of fructose-sweetened compared with glucose-sweetened beverages corresponding to 25 E% (16). In our study, large significant postprandial differences in glucose and insulin concentrations were observed, and fasting and iAUC HOMA-R index tended to be different too. These data together with the data in the study by Stanhope et al. (16) suggest that consumption of a sucrose- or fructose-rich diet for an extended period of time (e.g. 10 weeks) produces a less beneficial glycaemic and insulinemic response and a risk of developing insulin resistance compared with a diet sweetened with non-caloric sweeteners or glucose. However, it is likely that changes in body weight can explain part of these findings.
We observed a large increase in lactate concentrations on the sucrose diet compared with the sweetener diet. This can probably be explained by the metabolic fate of the fructose moiety from the sucrose molecule. Thus, fructose present in the portal blood is efficiently extracted by the liver and metabolised to fructose-1-phosphate under the action of the enzyme fructokinase, which is highly specific for fructose (35). Fructose-1-phosphate is further metabolised to triose-phosphate that subsequently can be converted into lactate and released into the systemic circulation (35). In accordance with this, postprandial lactate was shown to be elevated both after short- and longer-term consumption of a sucrose-rich compared with a starch-rich diet (32, 33).
A number of studies have been published in the past decade on the effects of fructose or high-fructose corn syrup on measures of lipidemia. In vitro data indicate that lactate is a main lipogenic precursor after fructose administration and that the activation of pyruvate dehydrogenase is a major regulatory step in this process. At the same time, fructose inhibits hepatic lipid oxidation, thus favouring fatty acid re-esterification and VLDL-triglycerid synthesis (35). Due to the fructose moiety, sucrose may therefore affect concentrations of TAG by increasing hepatic TAG synthesis and Very Low Density Lipoprotein (VLDL) production (36, 37).
Although total fasting TAG was higher in our study after 10 weeks on the sucrose diet, the changes from week 0 to 10 were not significantly different between groups (p=.07). Furthermore, changes in fasting cholesterol concentrations did also not differ between diets. Similarly, fasting TAG and cholesterol concentrations did not differ after 6 months on a low-fat, high-sucrose diet compared with a low-fat, high-starch ad libitum diets in the CARMEN study, in which 398 obese men and women participated (38). It is important to note, however, that in contrast to the present study, subjects in the CARMEN study consumed less energy and lost body weight on the sucrose-rich diet compared with a more fat-rich control diet – probably due to the sucrose-rich diet consisting mostly of solid foods and not of drinks as in the present study.
In the present study, postprandial TAG responses were significantly higher on the sucrose diet compared with the sweetener diet. These results are in accordance with previous studies, where diurnal TAG levels were found to be higher after sucrose, measured after 1–24 days intake, compared with either starch or glucose (32–34). Furthermore, a recent study showed that consuming fructose-sweetened beverages for 10 weeks increased 23-hour postprandial triglyceride AUC and hepatic de novo lipogenesis as well as visceral adiposity compared with glucose-sweetened beverages (16). Since sustained elevation of plasma TAG has been proposed to be an independent risk factor for cardiovascular diseases (39, 40) and since the diurnal TAG response was consistently higher on the sucrose diet in the present study, it can be speculated that this diet would lead to an increased risk of these diseases in the long-term compared with a diet sweetened with non-caloric sweeteners.
Not many studies have compared sucrose with artificial sweeteners after longer-term consumption. One earlier cross-over study looked at the effect of an intake of 45 g sucrose (9 E%) compared with an equivalent sweetening amount of aspartame for 6 weeks in 9 subjects with NIDDM (41). Here no effect of the added sucrose was observed with regard to fasting triglycerides, total or HDL-cholesterol, glucose and HbA1c, 2-hour postprandial glycaemia, and insulinemia or insulin sensitivity as measured by the euglycemic clamp. The lack of differences in that study could, however, be due to the fairly small sucrose challenge compared with both our study (27 E%) and the recent study by Stanhope et al. (16), where fructose amounted to 25 E%.
We found both increased fasting and postprandial leptin concentrations in the sucrose compared with the sweetener group after 10 weeks’ intervention. The differences in fasting values disappeared, however, after adjusting for changes in body weight. This would correspond to the fact that a higher leptin concentration is an indicator of higher fat deposits. Overall, however, diurnal leptin concentrations were about twice as high on the sucrose-rich diet compared with the sweetener diet. This could be due to the prolonged increase in insulin concentration, since hyperinsulinemia has been found to stimulate leptin release (42). We have previously observed increased postprandial leptin levels after only 14 days’ ad libitum sucrose-rich versus starch-rich diet in normal weight subjects. This finding was also explained by greater postprandial insulin peaks on the sucrose-rich diet (43).
In conclusion, a sucrose-rich diet consumed for 10 weeks resulted in significant elevations of postprandial glycaemia, insulinemia, and lipidemia compared to a diet rich in artificial sweeteners in slightly overweight healthy subjects. However, more studies and of longer duration are needed to substantiate these findings.
Acknowledgements
AR was responsible for the study protocol. THV, ACM, and AR were responsible for conducting the trial and for data collection. JJH was responsible for analyses of blood parameters. BKM was responsible for the data analysis and drafted the first script with supervision from AFL, AA, and AR. All authors contributed to the interpretation of the results and the final version of the manuscript.
Conflict of interest and funding
None of the authors have any conflict of interest. Financial support for this study was provided by The Danish Research Councils, FØTEK (Development Programme for Food Technology), and Danisco Sugar.
References
- 1.Bray GA, Nielsen SJ, Popkin BM. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am J Clin Nutr. 2004;79:537–43. doi: 10.1093/ajcn/79.4.537. [DOI] [PubMed] [Google Scholar]
- 2.Basciano H, Federico L, Adeli K. Fructose, insulin resistance, and metabolic dyslipidemia. Nutr Metab (Lond) 2005;2:5. doi: 10.1186/1743-7075-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diet, nutrition and the prevention of chronic diseases: report of a joint FAO/WHO Expert Consultation, . FAO/WHO; WHO Technical Report Series, Paper No. 916; 28 January–1 February 2002.; Geneva. Geneva: World Health Organisation; 2003. [Google Scholar]
- 4.Nordic Council of Ministers. Nordic nutrition recommendations. Nordisk Ministerråd.; 2004. integrating nutrition & physical activity. 4th ed. [Google Scholar]
- 5.Lyhne N, Ovesen L. Added sugars and nutrient density in the diet of Danish children. Scan J Nutr. 1999;43:4–7. [Google Scholar]
- 6.Beck AM, Ovesen L. Added sugars and nutrient density in the diet of elderly Danish nursing home residents. Scan J Nutr. 2002;46:68–72. [Google Scholar]
- 7.DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes. 2000;24:794–800. doi: 10.1038/sj.ijo.0801229. [DOI] [PubMed] [Google Scholar]
- 8.Raben A, Vasilaras TH, Møller AC, Astrup A. Sucrose compared with artificial sweeteners: different effects on ad libitum food intake and body weight after 10 wk of supplementation in overweight subjects. Am J Clin Nutr. 2002;76:721–9. doi: 10.1093/ajcn/76.4.721. [DOI] [PubMed] [Google Scholar]
- 9.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357:505–8. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- 10.Hu FB, Malik VS. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav. 2010;100:47–54. doi: 10.1016/j.physbeh.2010.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, Willett WC, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA. 2004;292:927–34. doi: 10.1001/jama.292.8.927. [DOI] [PubMed] [Google Scholar]
- 12.Palmer JR, Boggs DA, Krishnan S, Hu FB, Singer M, Rosenberg L. Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women. Arch Intern Med. 2008;168:1487–92. doi: 10.1001/archinte.168.14.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pagliassotti MJ, Shahrokhi KA, Moscarello M. Involvement of liver and skeletal muscle in sucrose-induced insulin resistance: dose-response studies. Am J Physiol. 1994;266:R1637–44. doi: 10.1152/ajpregu.1994.266.5.R1637. [DOI] [PubMed] [Google Scholar]
- 14.Hulman S, Falkner B. The effect of excess dietary sucrose on growth, blood pressure, and metabolism in developing Sprague-Dawley rats. Pediatr Res. 1994;36:95–101. doi: 10.1203/00006450-199407001-00017. [DOI] [PubMed] [Google Scholar]
- 15.Daly M. Sugars, insulin sensitivity, and the postprandial state. Am J Clin Nutr. 2003;78:865S–72S. doi: 10.1093/ajcn/78.4.865S. [DOI] [PubMed] [Google Scholar]
- 16.Stanhope KL, Schwarz JM, Keim NL, Griffen SC, Bremer AA, Graham JL, et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest. 2009;119:1322–34. doi: 10.1172/JCI37385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dhingra R, Sullivan L, Jacques PF, Wang TJ, Fox CS, Meigs JB, et al. Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation. 2007;116:480–8. doi: 10.1161/CIRCULATIONAHA.107.689935. [DOI] [PubMed] [Google Scholar]
- 18.Parks EJ, Hellerstein MK. Carbohydrate-induced hypertriacylglycerolemia: historical perspective and review of biological mechanisms. Am J Clin Nutr. 2000;71:412–33. doi: 10.1093/ajcn/71.2.412. [DOI] [PubMed] [Google Scholar]
- 19.Sørensen LB, Raben A, Stender S, Astrup A. Sucrose from soft drinks increases inflammatory markers in overweight subjects. Am J Clin Nutr. 2005;82:421–7. doi: 10.1093/ajcn.82.2.421. [DOI] [PubMed] [Google Scholar]
- 20.Metropolitan Life Insurance Company. Metropolitan height and weight tables for men and women, according to frame, ages 25–29. Stat Bull Metrop Life Found. 1983;64:2–9. [Google Scholar]
- 21.Møller A. Levnedsmiddeltabeller, Storkøkkencenteret, levnedsmiddelstyrelsen. (Danish food tables, The Danish Food Agency.) Copenhagen: Gyldendahl, 1989 (in Danish). [Google Scholar]
- 22.Heitmann BL. Prediction of body water and fat in adult Danes from measurement of electrical impedance. A validation study. Int J Obes. 1990;14:789–802. [PubMed] [Google Scholar]
- 23.Deeg R, Kraemer W, Ziegenhorn J. Kinetic determination of serum glucose by use of the hexokinase/glucose-6-phosphate dehydrogenase method. J Clin Chem Clin Biochem. 1980;18:49–52. doi: 10.1515/cclm.1980.18.1.49. [DOI] [PubMed] [Google Scholar]
- 24.Noll F. L-(+)-lactate. Determination with LDH, GPT and NAD. In: Bergmayer H, editor. Methods of enzymatic analysis. 2nd ed. New York: Academic Press; 1974. pp. 1475–1479. [Google Scholar]
- 25.Albano JDM, Ekins RP, Maritz G, Turner RC. A sensitive precise radio-immunoassay of serum insulin relying on charcoal separation of bound and free hormone moieties. Acta Endocrinol. 1972;70:487–509. doi: 10.1530/acta.0.0700487. [DOI] [PubMed] [Google Scholar]
- 26.Wahlefeld AW. Triglycerides. Determination after enzymatic hydrolysis. In: Bergmayer H, editor. Methods of enzymatic analysis. 2nd ed. New York: Academic Press; 1974. p. 1878. [Google Scholar]
- 27.Krarup T, Madsbad S, Moody AJ, Regeur L, Faber OK, Holst JJ, et al. Diminished gastric inhibitory polypeptide (GIP) response to a meal in newly diagnosed type I (insulin dependent) diabetics. J Clin Endocrinol Metab. 1983;56:1306–12. doi: 10.1210/jcem-56-6-1306. [DOI] [PubMed] [Google Scholar]
- 28.Ørskov C, Wettergren A, Holst JJ. Secretion of the incretin hormones glucagon-like peptide-1 and gastric inhibitory polypeptide correlates with insulin secretion in normal man throughout the day. Scand J Gastroenterol. 1996;31:665–70. doi: 10.3109/00365529609009147. [DOI] [PubMed] [Google Scholar]
- 29.Holst JJ. Evidence that enteroglucagon (II) is identical with the C-terminal sequence (residues 33-39) of glicentin. Biochem J. 1982;207:381–8. doi: 10.1042/bj2070381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 31.Vilsbøll T, Krarup T, Sonne J, Madsbad S, Vølund A, Juul AG, et al. Incretin secretion in relation to meal size and body weight in healthy subjects and people with type 1 and type 2 diabetes mellitus. J Clin Endocrinol Metab. 2003;88:2706–13. doi: 10.1210/jc.2002-021873. [DOI] [PubMed] [Google Scholar]
- 32.Raben A, Holst JJ, Madsen J, Astrup A. Diurnal metabolic profiles after 14 d of an ad libitum high-starch, high-sucrose, or high-fat diet in normal-weight never-obese and postobese women. Am J Clin Nutr. 2001;73:177–89. doi: 10.1093/ajcn/73.2.177. [DOI] [PubMed] [Google Scholar]
- 33.Daly ME, Vale C, Walker M, Littlefield A, Alberti KGMM, Mathers JC. Acute effects on insulin sensitivity and diurnal metabolic profiles of a high-sucrose compared to a high-starch diet. Am J Clin Nutr. 1998;67:1186–96. doi: 10.1093/ajcn/67.6.1186. [DOI] [PubMed] [Google Scholar]
- 34.Brynes AE, Edwards CM, Ghatei MA, Dornhorst A, Morgan LM, Bloom SR, et al. A randomized four-intervention crossover study investigating the effect of carbohydrates on daytime profiles of insulin, glucose, non-esterified fatty acids and triacylglycerols in middle-aged men. Br J Nutr. 2003;89:207–18. doi: 10.1079/BJN2002769. [DOI] [PubMed] [Google Scholar]
- 35.Tappy L, Lê K-A. Metabolic effects of fructose and the worldwide increase in obesity. Physiol Rev. 2010;90:23–46. doi: 10.1152/physrev.00019.2009. [DOI] [PubMed] [Google Scholar]
- 36.Hellerstein MK. Carbohydrate-induced hypertriglycridemia: modifying factors and implications for cardiovascular risk. Curr Opin Lipidol. 2002;13:33–40. doi: 10.1097/00041433-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Hudgins L. Effect of high-carbohydrate feeding on triglyceride and saturated fatty acid synthesis. Proc Soc Exp Biol Med. 2000;225:178–83. doi: 10.1046/j.1525-1373.2000.22521.x. [DOI] [PubMed] [Google Scholar]
- 38.Saris WHM, Astrup A, Prentice AM, Zunft HJF, Formiguera X, Verboeket-van de Venne WPHG, et al. Randomized controlled trial of changes in dietary carbohydrate/fat ratio and simple vs complex carbohydrates on body weight and blood lipids: the CARMEN study. Int J Obes. 2000;24:1310–8. doi: 10.1038/sj.ijo.0801451. [DOI] [PubMed] [Google Scholar]
- 39.Bansal S, Buring JE, Rifai N, Mora S, Sacks FM, Ridker PM. Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA. 2007;298:309–16. doi: 10.1001/jama.298.3.309. [DOI] [PubMed] [Google Scholar]
- 40.Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA. 2007;298:299–308. doi: 10.1001/jama.298.3.299. [DOI] [PubMed] [Google Scholar]
- 41.Colagiuri S, Miller JJ, Edwards RA. Metabolic effects of adding sucrose and aspartame to the diet of subjects with noninsulin-dependent diabetes mellitus. Am J Clin Nutr. 1989;50:474–8. doi: 10.1093/ajcn/50.3.474. [DOI] [PubMed] [Google Scholar]
- 42.Boden G, Chen X, Kolazcynski JW, Polansky M. Effects of prolonged hyperinsulinemia on serum leptin in normal human subjects. J Clin Invest. 1997;100:1107–13. doi: 10.1172/JCI119621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Raben A, Astrup A. Leptin is influenced both by predisposition to obesity and diet composition. Int J Obesity. 2000;24:450–9. doi: 10.1038/sj.ijo.0801178. [DOI] [PubMed] [Google Scholar]