Abstract
The biosand filter (BSF) is a promising point of use (POU) technology for water treatment; however there has been little follow-up of initial implementation to assess sustainability. The purpose of this study was to examine continued use, performance, and sustainability of previously implemented concrete BSFs in Bonao, Dominican Republic. Of 328 households visited and interviewed, 90% of BSFs were still in use after approximately 1 year since installation. Water-quality improvement, measured by fecal indicator bacteria reduction, was found to be 84–88%, which is lower than reductions in controlled laboratory studies but similar to other field assessments. In a short prospective cohort study comparing BSF to non-BSF households, odds of reported diarrheal disease in BSF households were 0.39 times the odds of reported diarrheal disease in non-BSF households. These results document high levels of sustained and effective concrete BSF use and associated improvements in water quality and health.
Introduction
Access to clean drinking water is not a reality for nearly 1 billion people in the world.1 This lack of access places significant health and economic burdens on people in the form of diarrheal disease, time away from productive enterprise, costs of medical treatment, and decrements in child development. These burdens disproportionately impact children, with approximately 1.6 million child deaths each year caused by diarrheal diseases linked to unsafe drinking water and many more suffering from disease and developmental deficiencies.2
Household water treatment at the point of use (POU) offers great potential in providing clean, safe drinking water to those lacking it. Building on the growing evidence of the effectiveness of POU water treatment, the parameters of sustainability, cost effectiveness, and scalability become critical to researchers, policymakers, and implementers.3 In a recent review, Schmidt and Cairncross4 argue that the lack of evidence on acceptability and scalability remains a barrier to promotion of POU household drinking water treatment. Although some studies have attempted to measure user compliance and acceptance, there has been little follow-up on the initial positive results seen in randomized controlled trials and other implementation studies.5–7 As a result, there is a lack of robust evidence regarding the sustainability of POU technology, which is measured by continued and effective use, consistent water-quality improvement, and sustained health impact. Existing evidence suggests that continued and effective use and sustained impact based on improved water quality mostly decrease over time, and this decrease is caused by the difficulty of affecting human behavior change, physical breakage of the treatment technology, or lack of physical or economic access to resupply the consumable products or replacement parts.8–10 Because sustainability is a key performance criterion for recommended POU technologies, assessing sustainability is critical evidence to obtain.3,4,10
The biosand filter (BSF), an intermittently operated slow sand filter, is a prevalent and promising POU water treatment technology. Recent estimates suggest that there are more than 140,000 BSFs globally serving more than 500,000 people, with up to 25,000 new filters being installed per year.11 Average cost for construction of the BSF ranges from US $15 to $60.12 Laboratory studies document BSF performance in reducing microbial indicators of fecal contamination, with reductions of approximately 90–99% for bacteria, 90% for viruses, and > 99.9% for protozoan parasites.13–15 In randomized controlled trials, BSFs in the Dominican Republic and Kenya were found to reduce diarrheal disease by 47% and 54%, respectively, in BSF households compared with control households.16,17
Some evidence of BSF continued use has been documented, but few, if any, rigorous field studies have been conducted to assess sustained improvements in drinking water quality and user health. Among 107 households in Haiti in which the BSF had been implemented for more than 2 years, 105 households were found to still use the filter, with average Escherichia coli reduction of 98.5%.18 Among more than 300 households in Cambodia surveyed up to 8 years after installation, 87.5% were found to still be using the BSF.19
The purpose of this study was to assess the overall performance and sustainability of previously implemented BSFs in and around Bonao, Dominican Republic approximately 1 year after initial BSF installation. The study took place from June to August in 2007 and had two phases: (1) a cross-sectional survey and analysis of continued use of the BSF, performance effectiveness, and sustained water-quality improvement and (2) a longitudinal prospective cohort measuring sustained health impact of the BSF on reducing diarrheal disease.
Methods
Ten communities were included in the cross-sectional assessment of continued BSF use. Each community was located near the city of Bonao, the capital of the province of Monseñor Nouel. Two communities, Jayaco and Brisas del Yuna, were the study sites for a BSF randomized controlled trial (RCT) completed in the fall of 2006.16 These two communities were also the focus of the longitudinal assessment and will be referred to as the RCT communities. The remaining eight communities were those where BSFs had been implemented by the Bonao Rotary Club. These eight communities were never part of the original RCT and therefore, will be referred to as the non-RCT communities.
Cross-sectional survey of continued BSF use.
All households selected and recruited into the cross-sectional study had previously received a concrete BSF, with initial education on BSF use and maintenance and sufficient time post-implementation for BSF ripening and adoption.13 The BSFs in the RCT communities were provided as compensation for study participation.16 In RCT communities, 85 BSFs were installed in February 2006, with only 75 of these households completing the RCT in August 2006. Seventy-nine additional BSFs were installed in August of 2006. Randomized at the household level, the February installation group served as the intervention households, receiving almost weekly follow-up for 6 months. The August installation group served as the control households during the original RCT and received BSFs on completion of the study with two follow-up visits post-installation.
The non-RCT community households received fully subsidized concrete BSFs in conjunction with ongoing Bonao Rotary Club implementation programs. All non-RCT BSF installations occurred between September and November 2006 except for one community, which received BSFs in October of 2005. In contrast to RCT households, the non-RCT households received no follow-up visits post-installation.
Of 154 RCT households that completed the study and received BSFs in 2006, 149 were contacted, enrolled, and interviewed in the cross-sectional follow-up study. The remaining five households were not available for the initial visit or the two repeat visits. In addition, three households with BSFs that began but did not complete the RCT were contacted, enrolled, and interviewed in this study. Study details were provided to each contacted household, and informed consent was obtained for interview and BSF sampling. If the BSF was moved to another accessible household, an interview was conducted with the new household when possible.
Of 247 non-RCT households sought for participation, 176 households were contacted, enrolled, and interviewed with assistance of the local Rotary Club. The remaining 71 households were not home at the time of visit, and no return or repeat visits were attempted because of logistical and financial constraints. Before interview, details of the study were provided to all contacted households, and the Rotary Club obtained informed consent from all participating households.
A total of 328 households from both RCT and non-RCT communities was visited to assess continued BSF use in June and July of 2007. Trained local staff conducted all interviews in Spanish, the local language. The Institutional Review Board of the University of North Carolina and the Provincial Health Sector of Monseñor Nouel, Dominican Republic approved the study.
Data collected for analysis included demographic, geographic, socioeconomic, and health-related factors including: time since installation, community, level of education, health education, soap in the household, access to sanitation, safe storage practices, hand washing, drinking water source, payment for water, time to water source, number of assets, and perception of diarrhea. Descriptions of these factors are listed in Table 1.
Table 1.
List of variables used in logistic regression for the cross-sectional survey of continued BSF use and the longitudinal prospective cohort study of the BSF in Bonao, Dominican Republic, from June to August of 2007
| Variable | Variable type | Description |
|---|---|---|
| Access to sanitation | Binary | Access to latrine or toilet |
| Age | Binary | Participants were grouped as < 5 or ≥ 5 years of age |
| Categorical age | Ordinal | Participants were grouped as < 2, 2–4, and ≥ 5 years of age |
| Community | Binary | Brisas del Yuna or Jayaco |
| Drinking water source | Categorical | Responses were not mutually exclusive and included surface (river or canal), ground (well or spring), rain, piped (inside and outside), and bottled water |
| Sex | Binary | Participant's sex |
| Hand washing | Binary | Reported hand washing always with soap and water after defecating |
| Health education | Binary | Primary respondent received health education about preventing or treating diarrhea from any source |
| Household wealth | Dichotomous | Categorized (lower 40% or upper 60%) wealth score |
| Level of education | Binary | Primary respondent and spouse received primary education |
| Number of assets | Ordinal | Summary of the number of six household assets |
| Number of participants | Ordinal | Total number of household members |
| Payment for water | Binary | Any amount of payment for water by household |
| Perception of diarrhea | Binary | Primary respondent reported belief that diarrhea is an illness from which children can die |
| Safe storage practices | Binary | Use of covered or narrow-mouth water-storage container |
| Soap in the household | Binary | Presence of soap in the household |
| Time since installation | Binary | Installation group based on filter installation date |
| Time to water source | Categorical | Time to drinking water source: < 5, 5–9, 10–19, 20–39, or ≥ 40 minutes |
| Week | Categorical | Eight categories for the 8 study weeks: 1–8 |
Cross-sectional survey data analysis.
Data were entered into specified data forms in EpiInfo (Centers for Disease Control and Prevention [CDC], Atlanta, GA) before being transferred into and analyzed using Intercooled Stata 8.0 software (StataCorp., College Station, TX). Initially, analyses were conducted using ordinary logistic regression to test the variables of time since installation and community for association with continued BSF use. Association with continued BSF use was determined by odds ratio (OR), and time since installation was the only variable included in the final model.
Controlling for time since installation, another stratified analysis was conducted using ordinary logistic regression to assess for correlation between BSF disuse and the collected demographic, geographic, socioeconomic, and health-related factors. Association with continued BSF use was determined by OR. This analysis was conducted only for RCT households, because the in-depth baseline questions asked during the previous RCT of study households were not asked of non-RCT households because of time constraints.
Cross-sectional survey water-quality analysis.
Water samples for laboratory analysis were taken when available from all RCT households. The samples collected included untreated water, treated water direct from concrete BSF outlet pipe, and BSF-treated and stored water. For non-RCT households, only the first household in each set of four households interviewed was selected to provide water samples if available. This sampling approach was taken because of constraints of time and finances.
Water samples of approximately 500 mL were collected in sterile Whirlpak bags and immediately stored in ice-cooled containers. The microbiological analysis was conducted within 24 hours of sample collection, with all RCT samples and most non-RCT samples being processed within 6 hours of collection. The samples were analyzed for E. coli and total coliforms using the IDEXX Colilert Quanti-Tray 2000 system (IDEXX Laboratories, Westbrook, ME).
Water sample data were entered into an Excel spreadsheet, and analysis was conducted in both Microsoft Excel (Microsoft Corp., Redmond, WA) and Intercooled Stata 8.0. Total coliform, E. coli, and turbidity measures were compared using arithmetic mean concentrations, geometric mean concentrations, and percent reductions calculated from the difference between untreated and BSF-treated water.
Longitudinal prospective cohort study in RCT households to examine diarrheal disease.
An 8-week longitudinal prospective cohort study was performed to assess continued health impact and water quality in a subset of RCT households compared with control households identified and recruited from the same two RCT communities (Brisas del Yuna and Jayaco). To be eligible to participate in the prospective cohort study as an RCT household, the RCT household needed to report having a child less than 5 years of age and still using the concrete BSF during the cross-sectional interview. Control households were identified as eligible if they never had and did not currently have a BSF and if they had at least one child less than 5 years of age.
The community-level recruitment and matching began in February 2007 and was completed in June 2007. Given the eligibility requirements, 102 RCT households and 98 control households were identified in Brisas del Yuna and Jayaco. The Jayaco community was further subdivided into five distinct geographic sublocations. With more control households eligible in Brisas del Yuna and more RCT households eligible in the five Jayaco sublocations, random selection was conducted until approximately equal numbers of RCT and control households were obtained in Brisas del Yuna and each Jayaco sublocation. This approach was taken to decrease the potential differences between the cohorts, because each location (Brisas del Yuna and five Jayaco sublocations) had similar drinking water sources, distances between houses, and distance from the main road. As a result, 66 RCT households and 69 control households were selected to participate.
In-depth baseline interviews were conducted with all control households to assess demographic, socioeconomic, diarrheal disease, and sanitation factors for each household, which was previously collected for RCT households in the previous study.16 Descriptions of these factors are listed in Table 1. The prospective cohort study then began on July 2nd, 2007 and ended on August 23rd, 2007. A diagram of overall study design, household selection, and participation is provided in Figure 1.
Figure 1.
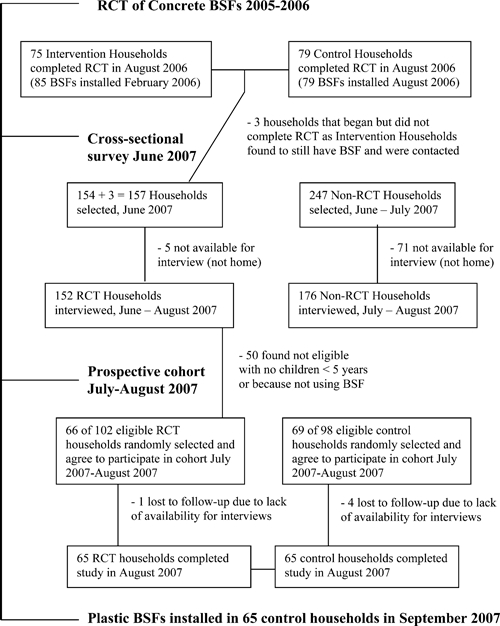
Diagram and timeline of household enrollment and participation in the cross-sectional survey and longitudinal prospective cohort study of concrete BSFs in Bonao, Dominican Republic in 2007.
During the study, households were visited weekly and asked questions about water-management practices in the home and diarrheal disease within the past 7 days (7-day recall period). When a case of diarrheal disease was reported, the primary respondent was asked for additional information regarding the case of diarrhea: the date that the case began, frequency of the evacuations, duration, and consistency of stool, including the presence of blood. Cases identified at the time of interview were tracked through interview with the primary respondent, with the same questions being asked the next week and during ensuing household visits until the case subsided. A case of diarrhea was defined as the passage of three or more loose or watery evacuations in a 24-hour period or one or more evacuation containing blood in a 24-hour period. A new case was assigned only when the participant experienced at least 3 successive days free of previously reported diarrheal disease.
Longitudinal prospective cohort study data analysis.
Data were entered into specified data forms in EpiInfo before being transferred into and analyzed using Intercooled Stata 8.0 software. Initially, comparability analysis was conducted to assess for potential differences between RCT households included in the longitudinal prospective cohort study and those not included in the study. Furthermore, cohort comparability analysis was conducted to assess for potential differences between RCT and control households of the longitudinal prospective cohort study. These analyses used the collected demographic, geographic, socioeconomic, and health-related factors. Significant difference between cohorts was determined by χ2 test or t test based on P < 0.05. Of those collected, selected characteristics included in the analyses were community, number of participants, sex, age, level of education, health education, soap in the household, access to sanitation, safe storage practices, hand washing, drinking water source, payment for water, time to water source, and household wealth (Table 1).
Household wealth was developed and estimated using principal components analysis (PCA) of household assets.20 PCA was used to evaluate and generate a wealth score from household information collected for the following assets: car, motorcycle, refrigerator, television, fan, washing machine, cellular phone, and education levels of the primary respondent and the spouse of the primary respondent. Based on the results of the PCA (using the first principal component), households were classified into quintiles of wealth. Because the quintiles would have divided groups into categories with low numbers of households, a dichotomous wealth variable was generated based on the lowest 40% category and the remaining households that constituted the upper 60% category, which was done in the previous RCT study in these communities.16
Longitudinal prospective cohort study data analysis continued with diarrheal disease as the main outcome variable. In developing the model to assess odds of diarrheal disease, univariate and multivariate analyses were conducted using ordinary logistic regression to test selected factors for confounding of diarrheal disease incidence rates in RCT and control households. Covariates were added individually to the model in a forward stepwise fashion and were only included when the outcome coefficient changed by > 10%. The following covariates were assessed: categorical age, level of education, health education, soap in the household, access to sanitation, safe storage practices, hand washing, drinking water source, payment for water, time to water source, number of assets, and perception of diarrhea (Table 1). Categorical age was the only characteristic included in the final model.
Controlling for categorical age, analysis of odds of diarrheal disease was conducted using ordinary logistic regression stratified by sex, community, and observation week. Furthermore, still controlling for categorical age, an overall OR was calculated using random intercepts logistic regression, which allows for adjustment of correlation of individuals over time as well as clustering of individuals within the same household.16,21,22.
Random intercepts logistic regression can accommodate clustering that occurs when repeatedly sampled individuals belong to subgroups and are nested in clusters.21 Increasingly, these models are being used to account for three level hierarchical structures. Wang and others22 described the use as an appropriate approach to analysis of clustered and repeated binary response data from a youth smoking cessation study. The data from our study lend well to the three-level hierarchical model structure, because individual participants were observed repeatedly; additionally, they each belonged to the BSF or control household. The random intercepts logistic regression model provided the most correct estimate of the standard error, which was used to estimate the 95% confidence intervals.
Results
Cross-sectional survey of continued BSF use.
The information on cross-sectional study participation and results are detailed in Table 2 and Figure 1. Approximately 10% of BSFs were found not to be in use among the 328 households that completed the survey (Table 2). Of those 27 households, the primary reason for disuse in 17 (63%) of the non-use households surveyed was poor perception or dislike of the BSF water, with the following responses included in this category: do not like using BSF, BSF water is of poor quality, BSF water has a bad odor, too much time is needed to use, and it is not necessary to use BSF. Three (11%) households reported that the BSF was broken or not working as the primary reason for disuse. Two (7%) households reported giving away the BSF as the primary reason for disuse. Five (19%) households reported other primary reasons for disuse including away from house because of an operation, use of neighbor's BSF, not living or currently staying in house, and BSF filled with ants. Responses were categorized into mutually exclusive reasons.
Table 2.
Continued use of concrete BSFs in a cross-sectional survey of communities in Bonao, Dominican Republic, from June to July of 2007
| Results from cross-sectional survey | RCT* | Non-RCT | All |
|---|---|---|---|
| No. of households selected | 157† | 247 | 404 |
| No. of households interviewed | 152‡ | 176§ | 328 |
| Using BSF (%)¶ | 143 (91.1%) | 158 (89.8%) | 301 (90.4%) |
RCT refers to households that previously participated in a randomized controlled trial of the BSF. Non-RCT refers to households that received BSFs from Rotary Clubs.
Total of 157 includes 154 households that completed the RCT in August of 2006 and 3 households that began but did not complete the RCT as intervention households found to still have a BSF.
Multiple attempts were made, but five households were unable to be reached for interview. Two BSF filters had been moved to new and accessible households.
No repeat visits were attempted.
The percentage in use was calculated based on the total selected for RCT households and the total interviewed for non-RCT households, because no repeat attempts were made for that group.
Based on data from the cross-sectional interview, several selected factors (Table 1) were identified and analyzed as potential predictors of continued BSF use. Time since installation was found to be associated with continued BSF use in the RCT households. Specifically, BSFs installed in February of 2006 were 9.9 (95% confidence interval [CI] = 1.17–83.85) times as likely to be in use as BSFs installed in August of 2006. No effect of time in use was found for non-RCT households, with all but one of the non-RCT communities having filters for the same amount of time.
Analysis of additional selected factors (Table 1) was conducted using ORs and controlling for time since installation for RCT households only given the lack of data collected on these selected factors for non-RCT households. The factors were selected for analysis because of their potential involvement in the complex process of accepting and using new technologies such as the BSF.23,24 After controlling for time since installation, no significant association was found between any of the factors considered and continued use of the BSF in the RCT households.
Water-quality results from the cross-sectional survey.
When available, water samples were collected for all RCT households still using the BSF and approximately 25% of non-RCT households. Concentrations of E. coli in untreated water and water direct from the concrete BSF outlet pipe were categorized into decimal (order of magnitude) concentrations as shown in Table 3; 33% of untreated water samples for all communities had ≤ 10 E. coli most probable number (MPN)/100 mL, whereas 75% of water samples direct from the BSF had ≤ 10 E. coli MPN/100 mL (Table 3). The World Health Organization (WHO) considers water samples from 0 to 10 E. coli MPN/100 mL to be in the reasonable range of water safety.25
Table 3.
Number (percentages) of samples by decimal E. coli concentrations in household drinking water during the cross-sectional survey of continued concrete BSF use in Bonao, Dominican Republic, from June to July of 2007
| Study households | E. coli concentration* | ||||||
|---|---|---|---|---|---|---|---|
| < 1 N (%) | 1–10 N (%) | 11–100 N (%) | 101–1,000 N (%) | 1,001+ N (%) | Total (N) | Geometric mean† | |
| All untreated | 19 (11%) | 36 (22%) | 63 (38%) | 37 (22%) | 12 (7%) | 167 | 28.3 |
| All BSF‡ | 68 (40%) | 65 (35%) | 28 (16%) | 7 (4%) | 2 (1%) | 170 | 3.3 |
MPN E. coli per 100 mL.
Geometric mean concentrations were significantly different (P < 0.001) by two-sample t test.
Water was direct from concrete BSF outlet pipe.
Average percent reductions in E. coli, total coliforms, and turbidity based on concentrations in untreated compared with either BSF-treated or BSF-treated and stored water are provided in Table 4. Average reductions for both types of bacteria were lower for BSF-treated and stored drinking water compared with untreated water than for BSF-treated water compared with untreated water.
Table 4.
Percent reductions* of E. coli, total coliforms, and turbidity during the cross-sectional survey of households in Bonao, Dominican Republic, in June of 2007
| Sample group comparisons | E. coli | Total coliforms | Turbidity | ||
|---|---|---|---|---|---|
| Untreated to BSF-treated | Untreated to BSF-treated and stored | Untreated to BSF-treated | Untreated to BSF-treated and stored | Untreated to BSF-treated | |
| All communities | 88.4%† | 50.6%† | 88.7%† | 15.4% | 29.5%† |
Percent reduction values are computed as (1 − 10−average log reduction) × 100 for E. coli and total coliform measures and as ((influent − effluent)/influent) × 100 for turbidity. Percent reductions compare untreated water with either water direct from a concrete BSF outlet pipe or concrete BSF-treated and stored water.
Geometric mean concentrations were significantly different (P < 0.001) using two-sample t tests for comparison of water samples.
Longitudinal prospective cohort study and sustained impact on diarrheal disease.
A total of 66 RCT (BSF) and 69 control (non-BSF) households were recruited into the 8-week longitudinal prospective cohort study beginning on July 2nd, 2007 and ending on August 23rd, 2007. One RCT household (1.5% of total) and four control households (5.8% of total) dropped out during the study because of lack of availability for interviews, representing loss to follow-up.
Comparability analysis of RCT households and other households that completed the RCT in August 2006 but were not selected for this study was conducted to determine if those households selected were representative of all households in the previous RCT, with selected characteristics found to be similar in distribution (data not shown). Furthermore, based on data from the previous RCT, there was no significant difference in odds of diarrheal disease (unadjusted OR = 1.10; 95% CI = 0.91–1.35) between the 66 selected households and those not selected.16
Cohort comparability analysis of RCT (BSF) and control households in this longitudinal prospective cohort study was conducted for a variety of factors that might impact household levels of diarrheal disease, and the results are detailed in Table 5. Significant differences were found using χ2 or t tests for number of people in each cohort, average number of members per household, and average age of participants less than 5 years of age. There were non-significant differences in levels of education and class (Table 5).
Table 5.
Comparison of selected characteristics regarding community, age, gender, sanitation, hygiene, education, and wealth for BSF and control households that completed the longitudinal prospective cohort study in Bonao, Dominican Republic, from July to August of 2007
| BSF group (N = 65 households; %) | Control group (N = 65 households; %) | P value* | |
|---|---|---|---|
| Community | |||
| Brisas del Yuna | 22 (34) | 26 (40) | 0.467 |
| Jayaco | 43 (66) | 39 (60) | |
| Total number of participants | 369 | 279 | 0.001* |
| Mean participants per household | 5.7 | 4.3 | 0.001* |
| Gender and age | |||
| Female ≥ 5 years | 151 (41) | 101 (36) | 0.222 |
| Female < 5 years | 44 (12) | 40 (14) | 0.365 |
| Male ≥ 5 years | 129 (35) | 99 (36) | 0.890 |
| Male < 5 years | 43 (12) | 39 (14) | 0.378 |
| Age (years) | |||
| Mean age of participants ≥ 5 | 24.7 | 26.4 | 0.154 |
| Mean age of participants < 5 | 2.6 | 1.8 | 0.001* |
| Education level of household† | |||
| Primary respondent: none | 6 (9) | 12 (18) | 0.156 |
| Primary respondent: some formal education‡ | 56 (86) | 53 (81) | |
| Missing | 3 (5) | – | |
| Spouse: none | 20 (30) | 23 (35) | 0.710 |
| Spouse: some formal education‡ | 42 (65) | 42 (65) | |
| Missing | 3 (5) | – | |
| Access to sanitation§ | |||
| Shared | 15 (23) | 23 (35) | 0.169 |
| Private | 47 (72) | 42 (65) | |
| Missing¶ | 3 (5) | – | |
| Interviewee reported receiving health education‖ | |||
| Yes | 30 (46) | 32 (49) | 0.924 |
| No | 32 (49) | 33 (51) | |
| Missing¶ | 3 (5) | – | |
| Household wealth** | |||
| Lower 40% | 31 (48) | 23 (35) | 0.096 |
| Upper 60% | 31 (48) | 42 (65) | |
| Missing¶ | 3 (4) | – | |
P values were used to determine significant difference between groups based on P < 0.05. P values were generated by χ2 test except for mean participants per household and mean age of participants, where t tests were used.
Describes whether the primary respondent and the primary respondent's spouse received any primary education.
Some formal education considered at least primary education.
All participating households reported having either a shared latrine or toilet or private latrine or toilet.
Missing cross-sectional data for three intervention households that did not provide this information in the cross-sectional interview.
Describes whether the primary respondent received health education about preventing or treating diarrhea from any source (friend, clinic, media, etc.).
Categorized (lower 40% or upper 60%) wealth score generated using principal component analysis of six household assets (motorcycle/moped, refrigerator, television, washing machine, fan, or cell phone) and level of education of primary respondent and primary respondent's spouse.
In developing the model to assess odds of diarrheal disease, selected factors (Table 1) were tested as potential confounders through univariate and multivariate analyses using ordinary logistic regression. Categorical age was the only characteristic included in the final model based on changing the outcome coefficient by > 10%.
Controlling for categorical age, the RCT (BSF) households experienced 61% lower odds of diarrheal disease (OR = 0.39; 95% CI = 0.23–0.68) compared with control households for all participants of the prospective cohort study. Controlling for categorical age, the OR was also stratified by age, week, sex, and community, with the results given in Table 6 and Figure 2. Despite finding lower unadjusted odds of diarrheal disease among RCT (BSF) households compared with control (non-BSF) households in all 8 weeks of the study, adjusted diarrheal incidence analysis by week found the effect of the BSF intervention to vary from week to week (Figure 2). Specifically, only in weeks 1 and 4 were significantly decreased odds of diarrheal disease among RCT households compared with control households.
Table 6.
Overall and stratum-specific ORs for diarrheal disease in BSF and control households during longitudinal prospective cohort study in Bonao, Dominican Republic, from July to August of 2007
| OR (95% CI; SS)* | |
|---|---|
| Overall† | 0.39 (0.20–0.76; 5,221) |
| Gender‡ | |
| Female | 0.30 (0.13–0.72; 2,714) |
| Male | 0.46 (0.23–0.92; 2,507) |
| Community‡ | |
| Brisas del Yuna | 0.43 (0.20–0.90; 1,840) |
| Jayaco | 0.38 (0.17–0.83; 3,381) |
OR (95% CI; sample size).
OR was calculated using random intercepts logistic regression comparing BSF with control households after adjustment for categorical age and clustering.
ORs were calculated using ordinary logistic regression comparing BSF with control households after adjustment for categorical age.
Figure 2.
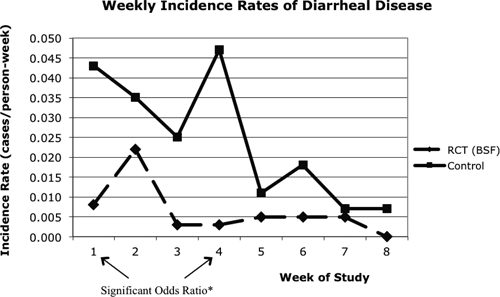
Weekly incidence rates of diarrheal disease in concrete BSF and control households for the longitudinal prospective cohort study in Bonao, Dominican Republic, from July to August 2007. *ORs for diarrheal disease are calculated using ordinary logistic regression comparing BSF with control households after adjustment for categorical age. Week 1 (OR = 0.25; CI = 0.07–0.91; sample size = 669) and week 4 (OR = 0.08; CI = 0.01–0.64; sample size = 645) were statistically significant with confidence intervals not crossing the null value of 1.00.
Using the random intercepts logistic regression model, which controlled for categorical age and clustering, the OR of diarrheal disease for the RCT (BSF) households compared with control (non-BSF) households was 0.39 (95% CI = 0.20–0.76), suggesting 61% lower odds of diarrheal disease for RCT households compared with control households for all participants of the prospective cohort study.
Discussion
Cross-sectional survey of continued BSF use after implementation.
Despite positive findings from previous intervention studies and other trials on BSFs and other POU technologies, the lack of follow-up of POU performance subsequent to these interventions highlights important data gaps.16,17,26 Among three follow-up assessments cited in a meta-analysis of 38 water, sanitation, and hygiene studies by Fewtrell and others,27 only two were in response to health impact studies, of which only one involved a POU technology. Another more recent meta-analysis found that one of the major predictors of impact from POU household water treatment was user compliance with the intervention.9
This is one of the few studies to return to RCT communities and assess continued concrete BSF use and effectiveness. Continued use rate was 90% among all households. This rate is relatively high compared with the rate seen for other POU technologies, which ranges from as low as 5% to as high as 80% for technologies such as ceramic filtration, solar disinfection, chlorination, and coagulant flocculant disinfectant.5–9,26,28–30 Furthermore, the proportion of BSFs in use in this study supports findings of other BSF interventions and use studies, which report 98.1% and 87.5% continued use in Haiti and Cambodia, respectively.18,19 Together, the high and relatively consistent continued BSF use rates seen across different studies compared with the rates seen for other POU technologies provide strong evidence of the sustainability of the concrete BSF.
The principle reason provided for discontinued use of the BSF was negative perception or dislike of the BSF, with 17 of 27 households not using the BSF stating this reason. Studies examining continued use of household chlorination found varying uptake results as well as difficulty in documenting consistent use.4,7 For other POU water treatment devices such as the ceramic water filter, the predominant reported reason for disuse was filter breakage. The breakage rate post-implementation was approximately 2% per month in Cambodia, and 25% of households reported that breakage prevented regular use of their ceramic filter in Bolivia.8,26 Breakage or lack of proper function was reported by only ∼1% of total BSF households and 10% of households not using their BSF, much lower than corresponding rates for ceramic filters. Because these disuse percentages are based on small sample sizes, continued use rates may provide better estimates of sustainability.
The comparison of RCT households, subject to the close oversight and follow-up of a research study, with non-RCT households, representative of a non-governmental organization (NGO) implementation program with minimal follow-up and no research objectives, did not reveal any significant differences in continued use rates, which further supports the sustainability of the BSF.
For RCT households, time since installation was positively correlated with continued BSF use, which is counterintuitive. Although the wide confidence interval suggests variability and uncertainty, the higher continued use rates of BSFs in use longer are likely related to the nature of the original RCT conducted in these communities. Specifically, after intervention households received BSFs in February 2006, they also received weekly visits over 6 months post-installation, during which time keeping the filter was contingent on continued use. In comparison, control households receiving BSFs and equivalent initial education in August of 2006 received no more than two post-installation visits.
The lack of significant correlation between additional factors selected for analysis and continued use of the concrete BSF in RCT households is not unexpected considering the small number of BSFs that were not in use. In future research, additional factors selected for analysis at household and community levels, especially health education and indicators of financial status, which were suggestive of continued BSF use, should be assessed in more detail for possible significant association with continued BSF use.
Sustained BSF impact on water quality in the cross-sectional survey.
Analysis of microbiological water quality in relation to use of the BSF revealed both modest water-quality improvement and relatively low initial levels of fecal contamination of influent untreated waters. When comparing untreated water samples with BSF-treated water samples, the average reduction was 88.4% for E. coli (Table 4). Among these samples, 47% showed greater than 1 log10 reduction (> 90%), with a maximum 3.38 log10 reduction (99.96%).
Compared with the average E. coli reductions of ∼83% for BSF-treated water compared with untreated water seen in the previous RCT in 2006, the reductions in this present study are higher, which supports the BSF as an effective and sustainable POU technology.16 Possible explanations for this improvement in E. coli reductions over time include filter ripening or maturation and variability in reductions dependent on volume filtered, level of E. coli in untreated water, or season.13–16 In households using a combination of BSF-treated water and BSF-treated and stored water, there were only modest average E. coli reductions in the water consumed. This finding is likely because of the already quite low initial E. coli levels in untreated water, which can be explained by variation in source water quality.14,16 Consistent with previous studies, E. coli reductions based on untreated water samples were lower for BSF-treated and stored water samples than for treated water samples directly from the filter outlet, suggesting possible E. coli recontamination or regrowth after treatment.16
The initial levels of E. coli in untreated water samples were low, as was the 88.4% average E. coli reduction by BSF treatment.13–15 In BSF laboratory challenge studies, fecal indicator bacteria reductions were 90–99%, and in other field studies, reductions were 98.5% for 107 BSFs assessed after an average of 2.5 years in use in Haiti and 95% for 104 BSFs in use for up to 8 years in Cambodia.18,19
Because the initial E. coli levels in the untreated water of this study were relatively low, with a geometric mean of 28.3 MPN/100 mL, many samples of BSF-treated and stored water and BSF-treated water had E. coli concentrations that were below the lower detection limit of the laboratory quantification method. With low initial E. coli concentrations in untreated water, non-detects in filtered water, and wide lower and upper method detection limits (< 1 MPN/100 mL to > 2,419.6 MPN/100 mL), the calculated log10 reductions are probably underestimates of those actually achievable by the BSF.
The geometric mean E. coli concentration of BSF-treated water samples was 3.3 MPN/100 mL, which is within the reasonable range of water safety (0–10 MPN/100 mL) according to WHO definitions.25 Average turbidity reductions between untreated water and BSF-treated water were low at 29.5%. Like the E. coli reductions discussed above, the low turbidity levels (1.1 nephelometric turbidity unit [NTU] average) in untreated water samples result in the low turbidity reductions by the BSF filter. Nevertheless, the average 0.6 NTU turbidity level of BSF-treated water is below the US Environmental Protection Agency (EPA) standard of 1 NTU, and the average turbidity level of the untreated water (1.1 NTU) is lower than the WHO guideline value of < 5 NTU.25
Sustained health impact of BSF use in the longitudinal prospective cohort study.
The results from the longitudinal prospective cohort suggest that RCT (BSF) households had 0.39 times the odds of diarrheal disease as the control households from the same community when controlling for age and clustering. This 61% percent reduction in diarrheal disease is consistent with or even greater than the previous 47% reduction of the initial RCT in the same study communities and is similar in magnitude to the diarrheal disease reduction associated with continued BSF use in similar prospective cohort studies in Cambodia and Kenya.16,17,19 These results further support the BSF as a POU technology that is both effective and sustainable in reducing diarrheal disease risk.
For all POU water-treatment technologies, estimates of diarrheal disease reductions, as determined through meta-analyses of RCTs, range from 35% to 51% for users.27,31,32 For ceramic water filters, a POU technology comparable with the BSF because it is water treatment using a filter as a durable good rather than a consumable chemical disinfection treatment such as chlorine, diarrheal disease reductions between 29% and 72% have been reported. In an analogous post-implementation assessment of the pot-style ceramic water purifier in Cambodia using a prospective cohort study design, there was 46% lower diarrheal disease prevalence for filter household members compared with non-filter household members.8
In this study, the stratum-specific analysis of ORs by week found significant reductions in diarrheal disease among BSF households in only 2 of 8 weeks of observation. This variation in diarrheal disease levels in BSF and non-BSF households suggests that the impact of the BSF can change over time, but such interpretation is limited by the 8-week length of the longitudinal study, the small sample size, the low rates of diarrheal disease in the control group, and the potential temporal variations in diarrheal disease illness rates. When evaluated in logistic regression, the week of study did not significantly change the OR from the random intercepts logistic regression model.
It is important to note that the self-reporting of diarrheal disease is a study limitation. The lack of a placebo BSF in this study precludes any ability to determine the influence of underreporting of diarrheal disease by BSF households, which may cause overestimation of reported diarrheal disease reductions.4 Both self-reporting and the technical and ethical issues associated with the placebo approach to controlling for a placebo effect are not unique to this study. The majority of analogous water, sanitation, and hygiene studies encountered and experienced these same limitations.
The contrast between modest cross-sectional study microbiological water-quality improvement and significant decrease in diarrheal disease in the longitudinal study is potentially explained by the underestimation of log10 reductions actually achieved by the BSF and the lack of measurement of parasite removal, which has been shown to be greater than bacterial removal for the BSF.13,15 Regardless, both the microbiological water-quality results and the diarrheal disease reduction results of this study are similar to those seen in preceding RCTs.16,17
The comparability of RCT and control households is also a possible study limitation, with significant differences in the number of people in each cohort, the average number of members per household, and the average age of participants less than 5 years of age. With previous research documenting higher rates of diarrheal disease seen at younger ages, the lower average age of children in control households (1.8 years) compared with children in RCT households (2.6 years) may overestimate the difference expressed in the OR of diarrheal disease.33 By assessing the potential impact of these variables and several others through a univariate and multivariate logistic regression model and then controlling for those variables resulting in greater than 10% change in the outcome coefficient, this potential limitation is minimized.
Additional assessments of BSF sustainability are needed in different settings to determine if the results seen in Bonao, Dominican Republic are generalizable to a larger geographically and demographically more representative scale. Future research is also recommended on cost effectiveness and scalability of BSFs and other POU household water treatments. Addressing these broader issues will require interdisciplinary efforts among business analysts, behavioral scientists, policy makers, and public health researchers, and such collaborative studies are critical for the goal of achieving greater access to safe water by scaled-up implementation schemes for the BSF and other POU water-treatment technologies.
ACKNOWLEDGMENTS
The authors thank the study participants, the interviewers, Dr. Mirna Peña de Guerra's laboratory team, and the family of Dr. Gloria Ortiz, all of Bonao, Dominican Republic, for their assistance, time, and patience. Without them, the study would not have been possible. The authors also thank Douglas Wait and the University of North Carolina Environmental Microbiology and Health Group.
Disclaimer: The authors' views expressed in this publication do not necessarily reflect the views of the US Agency for International Development or the US Government.
Footnotes
Financial support: This publication was made possible by the support of the American people through the US Agency for International Development (USAID). It was prepared under the Environmental Health Indefinite Quantity Contract (EHIQC) GHA-I-00-04-00006/Task Order #2, Line Item #3 and managed by CDM International Inc. Laboratory supplies for water-quality testing were donated by IDEXX Laboratories and Hach Company. We are grateful to the Bonao Rotary Club and the Canadian Embassy of the Dominican Republic for their generous financial support of this study.
Authors' addresses: Benjamin A. Aiken and Mark D. Sobsey, Department of Environmental Sciences and Engineering, University of North Carolina—Chapel Hill Gillings School of Global Public Health, Chapel Hill, NC, E-mails: benjamin_aiken@med.unc.edu and mark_sobsey@unc.edu. Christine E. Stauber, Institute of Public Health, Georgia State University, Atlanta, GA, E-mail: cstauber@gsu.edu. Gloria M. Ortiz, Department of Internal Medicine, Bronx Lebanon Hospital Center, Bronx, NY, E-mail: gortiz1@bronxleb.org.
References
- 1.World Health Organization and United Nations Children's Fund. Progress on Sanitation and Drinking Water 2010 Update. 2010. http://www.who.int/water_sanitation_health/publications/9789241563956/en/index.html Available at. Accessed June 25, 2010.
- 2.World Health Organization Household Water Treatment and Safe Storage. 2008. http://www.who.int/household_water/en/index.html Available at. Accessed June 9, 2008.
- 3.Sobsey MD. Managing Water in the Home: Accelerated Health Gains from Improved Water Supply. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 4.Schmidt WP, Cairncross S. Household water treatment in poor populations: is there enough evidence for scaling up now. Environ Sci Technol. 2009;43:986–992. doi: 10.1021/es802232w. [DOI] [PubMed] [Google Scholar]
- 5.Rose A, Roy S, Abraham V, Holmgren G, George K, Balraj V, Abraham S, Muliyil J, Joseph A, Kang G. Solar disinfection of water for diarrhoeal prevention in southern India. Arch Dis Child. 2006;91:139–141. doi: 10.1136/adc.2005.077867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rainey RC, Harding AK. Acceptability of solar disinfection of drinking water treatment in Kathmandu Valley, Nepal. Int J Environ Res Public Health. 2005;15:361–372. doi: 10.1080/09603120500289168. [DOI] [PubMed] [Google Scholar]
- 7.Arnold BF, Colford JM. Treating water with chlorine at point-of-use to improve water quality and reduce child diarrhea in developing countries: a systematic review and meta-analysis. Am J Trop Med Hyg. 2007;76:354–364. [PubMed] [Google Scholar]
- 8.Brown J, Sobsey M, Proum S. Use of Ceramic Water Filters in Cambodia. 2007. http://www.wsp.org/UserFiles/file/926200724252_eap_cambodia_filter.pdf Available at. Accessed February 23, 2009. [Google Scholar]
- 9.Hunter PR. Household water treatment in developing countries: comparing different intervention types using meta-regression. Environ Sci Technol. 2009;43:8991–8997. doi: 10.1021/es9028217. [DOI] [PubMed] [Google Scholar]
- 10.Sobsey MD, Stauber CE, Casanova LM, Brown JM, Elliot MA. Point of use household drinking water filtration: a practical, effective solution for providing sustained access to safe drinking water in the developing world. Environ Sci Technol. 2008;42:4261–4267. doi: 10.1021/es702746n. [DOI] [PubMed] [Google Scholar]
- 11.Clasen TF. Scaling Up Household Water Treatment among Low-Income Populations. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- 12.Household Water Treatment Options in Developing Countries: Slow Sand Filtration. 2010. (United States Agency for International Development and Centers for Disease Control and Prevention).http://sanitationupdates.wordpress.com/2010/11/09/usaidcdc-slow-sand-filtration-fact-sheet/ Available at. Accessed November 28, 2010.
- 13.Elliott MA, Stauber CE, Koksal F, DiGiano FA, Sobsey MD. Reductions of E. coli, echovirus type 12 and bacteriophages in an intermittently operated household-scale slow sand filter. Water Res. 2008;42:2662–2670. doi: 10.1016/j.watres.2008.01.016. [DOI] [PubMed] [Google Scholar]
- 14.Stauber CE, Elliot MA, Koksal F, Ortiz GM, DiGiano FA, Sobsey MD. Characterization of the biosand filter for E. coli reductions from household drinking water under controlled laboratory and field use conditions. Water Sci Technol. 2006;54:1–7. doi: 10.2166/wst.2006.440. [DOI] [PubMed] [Google Scholar]
- 15.Palmateer G, Manz D, Jurkovic A, McInnis R, Unger S, Kwan KK, Dutka BJ. Toxicant and parasite challenge of Manz intermittent slow sand filter. Environ Toxicol. 1999;14:217–225. [Google Scholar]
- 16.Stauber CE, Ortiz GM, Loomis DP, Sobsey MD. A randomized controlled trial of the concrete biosand filter and its impact on diarrheal disease in Bonao, Dominican Republic. Am J Trop Med Hyg. 2009;80:286–293. [PubMed] [Google Scholar]
- 17.Tiwari SK, Schmidt WP, Darby J, Kariuki ZG, Jenkins M. Intermittent slow sand filter for preventing diarrhoea among children in Kenyan households using unimproved water sources: a randomized controlled trial. Trop Med Int Health. 2009;14:1374–1382. doi: 10.1111/j.1365-3156.2009.02381.x. [DOI] [PubMed] [Google Scholar]
- 18.Duke WF, Nordin RN, Baker D, Mazumder A. The use and performance of BioSand filters in the Artibonite Valley of Haiti: a field study of 107 households. Rural Remote Health. 2006;6:570. [PubMed] [Google Scholar]
- 19.Liang KR, Stauber CE, Sobsey MD. Independent Evaluation of the Biosand Water Filter in Rural Cambodia: Sustainability, Health Impact and Water Quality Improvement. Washington, DC: World Bank; 2009. [Google Scholar]
- 20.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21:459–468. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 21.Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. College Station, TX: Stata Press; 2005. pp. 101–142. [Google Scholar]
- 22.Wang K, Lee AH, Hamilton G, Yau KKW. Multilevel logistic regression modeling with correlated random effects: application to the smoking Cessation for Youth study. Stat Med. 2006;25:3864–3876. doi: 10.1002/sim.2472. [DOI] [PubMed] [Google Scholar]
- 23.Wellin E. In: Health, Culture, and Community. Paul BD, editor. New York, NY: Russell Sage Foundation; 1955. pp. 71–103. (Water boiling in a Peruvian town). [Google Scholar]
- 24.Rogers E. Diffusion of Innovations. 5th ed. New York, NY; Simon and Schuster: 2003. [Google Scholar]
- 25.World Health Organization . Drinking Water Quality Guidelines. 3rd ed. Vol. 1. Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 26.Clasen T, Brown J, Collin S. Preventing diarrhoea with household ceramic water filters: assessment of a pilot project in Bolivia. Int J Environ Health Res. 2006;16:221–239. doi: 10.1080/09603120600641474. [DOI] [PubMed] [Google Scholar]
- 27.Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM. Water, sanitation, and hygiene interventions to reduce diarrhea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis. 2005;5:42–52. doi: 10.1016/S1473-3099(04)01253-8. [DOI] [PubMed] [Google Scholar]
- 28.Colindres R, Mermin J, Ezati E, Kambabazi S, Buyungo P, Sekabembe L, Baryarama F, Kitabire F, Mukasa S, Kizito F, Fitzgerald C, Quick R. Utilization of a basic care and prevention package by HIV-infected persons in Uganda. AIDS Care. 2007;20:139–145. doi: 10.1080/09540120701506804. [DOI] [PubMed] [Google Scholar]
- 29.Crump JA, Otieno PO, Slutsker L, Keswick BH, Rosen DH, Hoekstra RM, Vulule JM, Luby SP. Household based treatment of drinking water with flocculant-disinfectant for preventing diarrhoea in areas with turbid source water in rural western Kenya: cluster randomized controlled trial. BMJ. 2005;331:478–483. doi: 10.1136/bmj.38512.618681.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luby SP, Mendoza C, Keswick BH, Chiller TM, Hoekstra RM. Difficulties in bringing point-of-use water treatment to scale in rural Guatemala. Am J Trop Med Hyg. 2008;78:382–387. [PubMed] [Google Scholar]
- 31.Gundry S, Wright J, Conroy R. A systematic review of health outcomes related to household water quality in developing countries. J Water Health. 2004;2:1–13. [PubMed] [Google Scholar]
- 32.Clasen T, Schmidt WP, Rabie T, Roberts I, Cairncross S. Interventions to improve water quality for preventing diarrhoea: a systematic review and meta-analysis. BMJ. 2007;334:782. doi: 10.1136/bmj.39118.489931.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kosek M, Bern C, Guerrant RL. The global burden of diarrhoeal disease, as estimated from studies published between 1992 and 2000. Bull World Health Organ. 2003;81:197–204. [PMC free article] [PubMed] [Google Scholar]


