Abstract
Routine vaccination against human papillomavirus (HPV), the main cause of cervical cancer, is recommended for 11–12 year old girls, yet vaccine uptake is low. This study evaluates a social marketing campaign initiated by 13 North Carolina counties to raise awareness among parents and reduce barriers to accessing the vaccine in a primarily rural area. The 3-month campaign targeted mothers of girls ages 11–12 and healthcare practices serving pre-teen girls in four counties. Principles of social marketing were: product (recommended vaccine against HPV), price (cost, perception of safety and efficacy, and access), promotion (posters, brochures, website, news releases, doctor’s recommendation), and place (doctors’ offices, retail outlets). We analyzed (1) website traffic, hotline calls, and media placement; (2) cross-sectional surveys of mothers and providers; and (3) HPV immunization rates in intervention versus non-intervention counties. Of respondent mothers (n=225), 82% heard or saw campaign messages or materials. Of respondent providers (n=35), 94% used campaign brochures regularly or occasionally in conversations with parents. HPV vaccination rates within six months of campaign launch were 2% higher for 9–13 year old girls in two of the four intervention counties compared to 96 non-intervention counties. This evaluation supports campaign use in other primarily rural and underserved areas.
Introduction
Routine vaccination against human papillomavirus (HPV), a sexually transmitted infection that is the main cause of cervical cancer, is recommended for 11–12 year old girls, presumably before they are exposed to the virus through sexual activity (Centers for Disease Control and Prevention [CDC], 2007). Two vaccines (Gardasil® and Cervarix®) against HPV are licensed for females aged 9–26 in the United States (U.S. Food and Drug Administration, 2010). HPV vaccines protect against the two HPV strains that cause 70% of cervical cancers (CDC, 2007). Despite HPV vaccine’s availability since 2006 and extensive advertising by the manufacturer of Gardasil®, uptake is still only about one third of females ages 13–17 (Centers for Disease Control and Prevention, 2009).
This study evaluates a pilot social marketing campaign sponsored by a group of 13 North Carolina counties to raise awareness among parents and reduce barriers to accessing the HPV vaccine. The campaign targeted mothers of girls ages 11–12 and healthcare practices serving girls 11–12 years old in a primarily rural four county area in south central North Carolina.
Cervical cancer is a disease of racial, socioeconomic and geographic disparities (National Cancer Institute [NCI], 2009). Women who live in rural areas, particularly in the southern United States, have higher rates of cervical cancer than do women who live in urban areas (Akers, Newman, & Smith, 2007; Newmann & Garner, 2005; Saraiya et al., 2007; Yabroff et al., 2005). African-American women are 50% more likely to be diagnosed with cervical cancer and twice as likely to die from the disease as white women (NCI, 2009). Cervical cancer incidence rates for Hispanic and American Indian women are higher than for non-Hispanic women (American Cancer Society, 2007). Given such disparities, rural, ethnic minority women and their daughters in North Carolina were the targeted audiences for the HPV vaccine campaign evaluated in this study.
While most parents are willing to have their adolescent daughters receive the HPV vaccine, some are unaware of, undecided about or opposed to HPV vaccination, especially for younger daughters (9–12 years old) (Bernat, Harpin, Eisenberg, Bearinger, & Resnick, 2009; Brewer & Fazekas, 2007; Dempsey, Abraham, Dalton, & Ruffin, 2009; Freed, Clark, Butchart, Singer, & Davis, 2010; Kahn et al., 2009; Zimet, Liddon, Rosenthal, Lazcano-Ponce, & Allen, 2006). Awareness of HPV and HPV vaccine differs by socio-demographic group (Cates, Brewer, Fazekas, Mitchell, & Smith, 2009; Cates et al., 2010; Hughes et al., 2009; Tiro, Meissner, Kobrin, & Chollette, 2007). Television advertisements by the vaccine manufacturer have been the most common source of information about HPV vaccine reported by parents in the United States (Gerend, Weibley, & Bland, 2009; Hughes, et al., 2009; Katz et al., 2009). Recommendations from a child’s healthcare provider are consistently influential in parental decisions about HPV vaccination for their daughters (Dempsey, et al., 2009; Gottlieb et al., 2009; Kahn, et al., 2009; Reiter, Brewer, Gottlieb, McRee, & Smith, 2009; Rosenthal et al., 2008).
Social Marketing Intervention
The HPV vaccine campaign in North Carolina was based on classic social marketing process: initial planning, formative research, strategy development, program development and pretesting, implementation, and evaluation (Grier & Bryant, 2005; Kotler & Lee, 2008). The present article reviews the first five steps and focuses on evaluation. A year after the Food and Drug Administration approved the first HPV vaccine in 2006, 13 county health directors in the regional South Central Partnership for Public Health (SCPPH) undertook a social marketing campaign to promote vaccine uptake. The health directors aimed to address the relatively high rates of cervical cancer in their region compared to the state (up to 12.4 per 100,000 women compared to 7.9 for NC) (American Cancer Society, 2008). SCPPH secured state funds of approximately $113,000 for the two-year project and invited communication and public health researchers (including the authors) to help plan, execute and evaluate the campaign.
We based the intervention on the Health Belief Model (Becker, 1974), which addressed mothers’ perceptions of susceptibility to HPV infection, severity of cervical cancer, benefits of vaccination to prevent HPV infection and cancer, and possible barriers, including questions of safety, efficacy, cost, and access. We piloted the campaign for three months, June–August, 2009, in four counties (Cumberland, Robeson, Harnett, and Richmond) in the SCPPH region, with a goal of demonstrating an effective intervention that could be expanded in the future to all 13 counties. Our overall outcome objective was to “boost” HPV immunization rates among pre-teen girls by 5% over comparison counties, since studies show that communication campaigns that include mass media have an average effect size of about 5 percentage points (Snyder, 2007).
Using an iterative process, we solicited input from the target audience in campaign material development. Our first step was to conduct formative research with mothers of pre-teen girls in the intervention counties. We targeted parents of girls at the CDC’s routinely recommended vaccination age of 11–12 to understand (1) behavioral determinants for vaccination decisions, (2) mothers’ trusted sources of information and (3) reactions to pre-developed concepts that would motivate them to initiate HPV vaccination for their daughters.
We conducted four focus groups with racially diverse mothers (n=40) of girls who had not been vaccinated against HPV. Initial message concepts introduced in focus groups reflected two basic emotional “truths:” a mother’s instincts to protect her daughter from harm and to embrace aspirations for her future. Participants commented on design, layout, images and text in two poster versions presented in the first two focus groups and two revised versions presented in the subsequent two focus groups.
We found that mothers were unaware of the age recommendation for pre-teen girls, had many questions about the vaccine’s safety, and were distrustful of the widespread advertising (Rothman & Rothman, 2009) by the vaccine manufacturer. Some participants mentioned the legacy of Tuskegee experimentation, but did not seem paralyzed by lingering distrust. They primarily questioned why the company was trying so hard to reach women and asked, “What’s the rush?” Mothers preferred information from their daughter’s doctor, family, friends and the Internet where they could review multiple sites.
We further tested six poster executions via intercept interviews with 39 mothers of girls 9–13 years old at retail locations in the counties. In this phase of research, we targeted mothers of girls 9–13 to include parents who may be contemplating HPV vaccination or who had just missed CDC’s target ages of 11–12. Of the 79 mothers who participated in focus groups or intercept interviews, 42 were African American, 19 American Indian, 13 white, 3 Latina and 2 of mixed race. Final messages for campaign materials included the slogan: “Help protect your daughter from cervical cancer. Vaccinate today. Protect her tomorrow,” and the phrase “You have hopes and dreams for her future, and they don’t include cervical cancer.” Final images portrayed physical closeness between mothers and daughters of multiple races. Final copy emphasized that doctors recommended the HPV vaccine for pre-teen girls, included information on safety, efficacy, and access, and tagged the campaign as sponsored by SCPPH (Shafer, Cates, Diehl, & Hartmann, in press). See Figure 1 for final poster execution.
Figure 1.
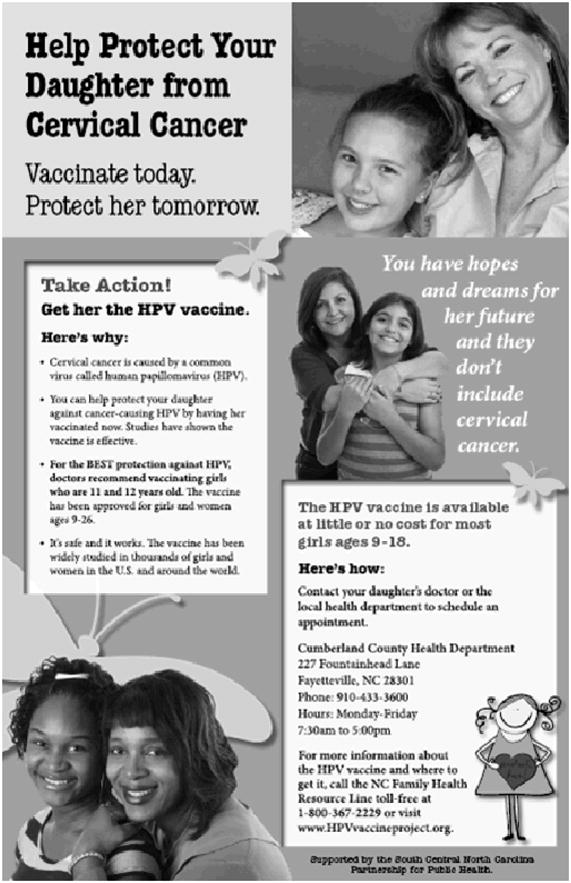
Final Campaign Poster Execution
We also interviewed 14 key informants (e.g., healthcare providers, community organizers) in the four counties to gain insights about past health campaigns in the area, channel reach and feasibility. Overall, both mothers and key informants strongly endorsed a locally sponsored, targeted, print-based campaign that would educate mothers about the vaccine.
Principles of social marketing (Lefebvre & Rochlin, 1997) incorporated in the campaign were: product (recommended vaccine against HPV), price (monetary cost, perception of safety and efficacy, and where to get the vaccine), promotion (posters, brochures, website, news releases, doctors’ recommendation) and place (doctors’ offices, pharmacies, retail outlets). Our strategies targeted not only mothers but also healthcare providers and the media, important influencers in health behavior (Andreasen, 2006). We distributed materials in English and Spanish through two primary channels, healthcare provider offices and community locations likely frequented by mothers. Since healthcare providers (both private practices and the public health department) were trusted sources and the only distributors of HPV vaccine, we created an access map of providers and prioritized them based on number of patients served. We located 127 healthcare practices and successfully contacted 112 (88%) who agreed to receive campaign materials, including posters and brochures, guide to “starting the conversation” with parents, buttons to encourage patient-parent-provider dialogue, and sticky notes for the patient encounter form to remind providers to recommend the vaccine. In all, 64 practices received materials in-person and 48 by mail.
The second primary channel targeted community locations where mothers were likely to be (e.g., pharmacies, beauty salons, grocery stores). With permission by location we placed posters and brochures in English and/or Spanish with a goal of one location for every ten mothers of 11–12 year old girls in each city in the four counties, according to census data. We placed materials at 662 sites and achieved placements of 48% of goal in Cumberland, 78% in Robeson, 93% in Harnett and 137% in Richmond County. Secondary channels included a project website, toll-free hotline, media releases, and a radio public service announcement.
Methods
We evaluated the campaign through (1) assessing website traffic, hotline calls, and media release or public service announcement (PSA) placement, (2) conducting cross-sectional surveys of mothers and healthcare providers, and (3) comparing HPV immunization rates in the four intervention counties to rates in non-intervention counties. The university’s Institutional Review Board approved the study.
Website Traffic
Website usage was assessed by placing Google Analytics tracking software on the campaign website (www.HPVvaccineproject.org) prior to launch. Tracking data were analyzed on two geographic levels (world and intervention counties) from June 1 to December 31, 2009.
Hotline Phone Calls
Phone calls referencing HPV or the HPV vaccine placed to the state-funded North Carolina Family Health Resource Line were tallied during the duration of the campaign.
Media Response
On launch date and six weeks later, media releases about the campaign were sent to 10 newspapers and PSAs were sent to 15 radio or television stations. We tracked their subsequent publication or broadcast by calling to inquire whether any had occurred during the campaign and checked with health departments to see if any other HPV vaccine campaigns had occurred during the summer months.
Survey of Mothers
Sample
Two weeks after the campaign’s conclusion, we surveyed mothers of daughters ages 9–18 in the intervention counties to assess how the primary target audience responded to campaign materials. We included mothers of girls 9–18 years old to compare HPV vaccine awareness and actions taken by mothers of younger girls 9–13 compared with mothers of older girls 14–18. We hypothesized a greater response to the campaign among mothers with daughters in the younger group, since images and messages were designed for them.
We selected a sample of 1,000 mothers from a targeted frame of 1,680 addresses purchased from a national marketing firm (USAData Inc., New York, NY). Population estimates in the four counties are 53% White, 30% African American and 7% Hispanic (remaining are other races), with 35% of the households having incomes $25,000 or below. To more closely represent county demographics (US Census, 2009), all mothers in households with incomes of $150,000 or higher were excluded, all Hispanics (n=71) or those with incomes less than $25,000 (n=201) were included. The remaining 728 addresses were randomly selected by county, so the sample proportion of mothers from each county matched the proportion in the frame.
Survey description and methods
The self-administered paper-and-pencil survey assessed awareness and recall of and actions taken in response to the HPV vaccine campaign. To encourage participation, we applied best practices in survey design, including personalized letters (Edwards et al., 2009). Mothers received a postcard announcing the survey one week prior to the initial survey mailing and a duplicate survey if they did not respond within four weeks. We offered mothers a chance for one of 32 gift cards for $25 as an incentive, and provided a stamped, addressed envelope to return the survey.
We used a short series of check-box questions and two open-ended questions. The survey introduction asked mothers to respond to an HPV vaccine campaign other than Gardasil® or the manufacturer’s “Tell Someone” or “One Less” commercials. Questions started broadly, first assessing awareness of any HPV vaccine messages (“Have you heard or seen any messages about the HPV vaccine this summer [other than messages about Gardasil®]?”), and became more specific with questions about message, materials, and logo recall (e.g., “Have you seen posters about protecting your daughter from cervical cancer?”). Follow-up questions assessed frequency and location of exposure. Two open-ended questions asked mothers to list what they remembered about posters and brochures. The survey concluded with a question about actions taken in response to information mothers saw or heard about HPV vaccine during the campaign period (e.g., talking with their daughter’s doctor), reasons for not taking action after exposure (if applicable), race and health insurance status. Health department staff from the four intervention counties reviewed the survey for readability and content.
Data analysis
We analyzed relationships between campaign awareness and actions taken by mothers. We dichotomized daughters’ ages into mothers with at least one daughter 9–13 years old and those with all daughters 14–18 years old and recoded open-ended race/ethnicity responses into three categories (white, black, and other). We dichotomized the county variable into rural or urban designations (North Carolina Rural Economic Development Center, 2010). Cumberland County was defined as urban while Harnett, Richmond, Robeson counties were rural.
A dichotomous summary measure of campaign awareness was defined as awareness of any campaign messages, logos, posters, or brochures. We created two variables to recode open-ended responses for what mothers recalled about the posters or brochures. Actions related to HPV vaccination were compared between those who were aware and unaware of the campaign. Fisher’s Exact tests were used for all comparisons, and unadjusted p-values are reported. Statistical analyses were performed using SAS software, version 9.2 (SAS Institute, Cary, NC).
Survey of Healthcare Providers
Sample
Healthcare providers (physicians, health directors, nurses, health educators, office managers, and social workers) were surveyed in the four-county intervention region to assess how they responded to campaign materials. We requested permission to contact staff who regularly interact with mothers in the 64 practices visited. Of 123 staff members, 116 (94%) agreed to be contacted by email or mail for an evaluation survey. One person per practice volunteered to serve as a key contact and complete an extended survey with both practice and individual-level questions. All other participants completed individual-level questions only.
Survey description and methods
We sent self-administered surveys via email or mailed paper copy to providers within the same week of the mothers’ survey mailing. Questions asked about changes in office and individual practices due to the campaign as well as provider use of and satisfaction with campaign materials. Providers who had not yet responded electronically were contacted two additional times with a reminder email and survey link; those who asked to be contacted by mail received one reminder mailing with a duplicate paper survey. Providers had a four-week window to complete the survey.
Measurement included Likert-type scales and check box lists. Practice-level questions assessed whether and how practices used campaign materials including posters, brochures, sticky note reminders, and project buttons (e.g., “Did your practice or organization: display and/or distribute HPV Vaccine Project brochures?”). An image of each item appeared next to the question as a reminder. Follow-up questions asked where practices displayed or used materials, and reasons for not using materials when applicable.
The individual-level portion of the survey assessed (1) behavior change (e.g., “Since the beginning of June, how likely were you to recommend the HPV vaccine to 11–12 year old girls and their parents?”; and “Since the beginning of June did YOU: Refer patients and/or parents to the local health department for the HPV Vaccine?”); (2) use of campaign materials (e.g., “Since the beginning of June did YOU: Use the HPV Vaccine Project brochure in conversations with girls and parents about the HPV vaccine?”); (3) satisfaction with the campaign, resources, and support (e.g., “How helpful were the toolkit materials to you: HPV Vaccine Access materials?”); and (4) perceptions of the campaign’s exposure in the community (e.g., “Did you see posters or other materials about the campaign in the community?”). The questionnaire included two open-ended questions asking for comments on campaign materials and general feedback about the campaign.
Comparison of HPV Immunization Rates
Description of data source
Data on 704,964 girls who were 9–19 years old as of December of 2008 were obtained from the North Carolina Immunization Registry (NCIR) (North Carolina Department of Health and Human Services, 2010). Rates include vaccinations reported by county health departments and the majority of private health care providers statewide. The data are not complete immunization coverage rates because registry compliance is voluntary and level of participation from practices varies bycounty. For example, Cumberland County has a large population for whom data from military providers are incomplete.
Methods and data analysis
We used NCIR data to compare cumulative HPV vaccination rates for girls ages 9–19 in the four intervention counties with rates in non-intervention counties in the region (nine counties) and the state (all other 96 North Carolina counties). The nine counties in the region are similar in socioeconomic characteristics to the four intervention counties, but exposure to campaign materials may have been possible if mothers crossed county lines for healthcare or visited retail outlets. The 96 counties in the rest of the state were less similar to the intervention counties and unlikely to have been exposed to the localized campaign. We aggregated data into two age groups, (9–13 and 14–19) based on their age on December 31, 2008. Monthly cumulative rates were calculated as the percentage of girls vaccinated prior to the first day of the month. Fisher’s Exact tests were used to compare the proportions of unvaccinated girls who received vaccinations during the six months following the start of the campaign in the four intervention counties with the nine non-intervention counties in the region and the 96 non-intervention counties in the state. Since the intervention targeted younger aged girls, we conducted separate analyses for girls 9–13 and 14–19. Additionally, the data were stratified to investigate the intervention’s differing effects by race (white, black, other).
Findings
Website Traffic
During the seven months measured, the website generated 1,312 visits from 53 countries/territories, including 55 from the four intervention counties. The average number of pages viewed was 3 overall and 2.5 for the intervention counties. The most popular pages beyond the homepage were “FAQs: about the HPV vaccine” and “Where to get the vaccine.”
Hotline Phone Calls
The Family Health Resource Line answered two phone calls in response to the campaign. Due to state budget cutbacks, the hotline was not operational for most of the campaign.
Media Response
The media outreach resulted in publication of four newspaper articles and broadcast of the campaign PSA on four radio and television stations from one time to every day during the campaign period. The newspaper articles were published in all four intervention counties and broadcast announcements occurred in all but Robeson County.
Survey of Mothers
Of the 1,000 mailed surveys, 53 were undeliverable, and 274 were returned, for a response rate of 28.9%. Forty-eight mothers indicated that they did not have a daughter between 9 and 18 years old and one refused, therefore results are based on responses from 225 mothers. Overall, 22% of daughters were ages 11–12 and 48% of mothers had at least one daughter age 9–13. The majority of respondents were white (64%), and almost all reported insurance coverage for their daughters (92%). A lower percentage of African Americans responded (20%) than were included in the sample (33%) and sixteen percent of respondents had household incomes less than $25,000 (see Table 1), compared to 21% of the original sample
Table 1.
Respondent Characteristics
| Number | (%) | |
|---|---|---|
| Age of daughter, yearsa | n=294 | |
| 9–10 | 27 | (9) |
| 11–12 | 66 | (22) |
| 13–14 | 80 | (27) |
| 15–16 | 88 | (30) |
| 17–18 | 33 | (11) |
| Number of daughters ages 9–18b | n =213 | |
| 1 | 143 | (67) |
| ≥2 | 70 | (33) |
| Race/Ethnicityc | n=218 | |
| White | 140 | (64) |
| Black | 43 | (20) |
| American Indian | 21 | (10) |
| Other | 14 | (6) |
| Insurance Coverage (Daughters) | n = 222 | |
| Yes | 205 | (92) |
| No | 17 | (8) |
| Household Incomed | n = 224 | |
| <$25,000 | 36 | (16) |
| $25–75,000 | 134 | (60) |
| >$75,000 | 54 | (24) |
| Residenced | n = 225 | |
| Urban (Cumberland) | 123 | (55) |
| Rural (Harnett, Richmond, Robeson) | 102 | (45) |
Notes. Percents may not sum to 100% due to rounding.
Sums to total number of daughters reported by mothers.
Ages of 12 daughters not reported by mothers.
“Other” category includes Hispanic (n = 11), Asian (n = 1), mixed race or ethnicity (n = 2).
Data from USAData, Inc.
Campaign awareness and recall
Most respondents (82%) were aware of HPV messages, logos, or both. Overall awareness did not differ by daughters’ age, mother’s race, income level, or rural/urban residence. More than half of respondents in the target age group (mothers of 9–13 year old daughters) reported recognizing each of the three tag lines from the campaign materials (“Vaccinate Today”; “Hopes and Dreams”; “Protect”) although only 24% recognized the campaign name, “HPV Vaccine Project” (see Table 2). Equal proportions of mothers remembered seeing campaign posters (43%) and brochures (44%). Mothers most frequently reported seeing posters and brochures in the doctor’s office or health department (84% and 91%, respectively), and in drug stores (18% and 11%, respectively). Mothers in the target age group were less likely to see posters “frequently” or “occasionally” than mothers with older daughters (44% vs. 69%, p<.05), however, they were equally likely to have seen brochures. Open-ended responses were primarily non-specific to either the campaign or any for Gardasil.® Only 16% of mothers in the target group reported having seen the campaign’s logo.
Table 2.
Mothers’ awareness of HPV vaccine campaign components
| Daughter’s Age (n=213) | ||||
|---|---|---|---|---|
| 9–13 (n=103)a | 14–18 (n=110)b | |||
| Number reported/total | % | Number reported/total | % | |
| Total combined awareness | 85/103 | 83 | 89/110 | 81 |
| HPV Vaccine Project | 21/87 | 24 | 33/99 | 33 |
| Vaccinate Today. Protect her tomorrow. | 48/89 | 54 | 59/99 | 60 |
| You have hopes and dreams for her future and they don’t include cervical cancer. | 47/92 | 51 | 47/98 | 48 |
| Help protect your daughter from cervical cancer. | 61/95 | 64 | 72/105 | 69 |
| Seen the logo | 16/101 | 16 | 11/105 | 10 |
| Seen logo or messages | 79/103 | 77 | 84/110 | 76 |
| --Frequently/Occasionally | 31/45 | 69 | 33/42 | 79 |
| --Rarely | 14/45 | 31 | 9/42 | 21 |
| Seen HPV vaccine posters | 44/103 | 43 | 48/109 | 44 |
| --Frequently/Occasionally | 19/43* | 44 | 31/45* | 69 |
| --Rarely | 24/43* | 56 | 14/45* | 31 |
| Seen HPV vaccine brochures | 45/102 | 44 | 55/109 | 50 |
| --Frequently/Occasionally | 23/42 | 55 | 32/51 | 63 |
| --Rarely | 19/42 | 45 | 19/51 | 37 |
mothers who have at least one daughter ages 9–13.
mothers who only have daughters ages 14–18.
p<.05
Reported actions
Mothers of girls ages 9–13 who indicated at least some campaign awareness (n=85) were more likely to take action than mothers who were unaware (n =18) (71% vs. 22%, p<.001). Most frequently reported actions were: talked with doctor (38%), talked with daughter (36%), talked with family-friends (33%), and got daughter vaccinated (27%). Reported actions taken did not differ by age of the daughters (see Table 3).
Table 3.
Actions taken by mothers aware of HPV vaccine campaign
| Daughter’s Age (n=174) | ||||
|---|---|---|---|---|
| 9–13 (n=85) | 14–18 (n= 89) | |||
| n | % | n | % | |
| Got daughter HPV vaccine | 23 | 27 | 24 | 27 |
| Made appointment | 11 | 13 | 7 | 8 |
| Talked with doctor | 32 | 38 | 32 | 36 |
| Called/visited health dept. | 2 | 2 | 4 | 4 |
| Talked with daughter | 31 | 36 | 34 | 38 |
| Visited website | 2 | 2 | 7 | 8 |
| Called hotline | 1 | 1 | 0 | 0 |
| Talked with family/friends | 28 | 33 | 27 | 30 |
| No action | 25 | 29 | 24 | 27 |
Of campaign aware mothers with younger daughters who reported taking no action as a result of the campaign (n=25), the most frequently cited concerns were: side effects (48%), need for more information (48%), newness of the vaccine (32%), and lack of confidence in vaccine effectiveness (20%).
Survey of Healthcare Providers
We received responses from 46 of the 116 healthcare providers who agreed to be contacted, for a response rate of 40%. Of the returned surveys, 11 were invalid: six people declined to participate and five consented but did not respond to any questions. Of the 35 respondents who completed the survey, 12 were key contacts and answered questions about organizational response. Most respondents were from health departments (48%) or pediatric groups (45%) in 23 different practices.
Organizational responses
Practices reported using English brochures (92%), Spanish brochures (80%), English posters (82%), and Spanish posters (70%). Brochures were widely used in waiting and exam rooms and placed on bulletin boards, nursing and/or immunization stations. Most practices (73%) had at least one provider who wore the campaign button. Overall, 45% of practices reported using reminder sticky notes.
Individual responses
Of the 35 individual providers who responded, almost all (94%) reported using the brochure in conversations with girls and parents. Many reported wearing a project button (62%). Materials rated as most helpful to providers were the brochures and posters; least helpful materials were the buttons and sticky note reminders. About 80% of providers reported they were “much more” or “somewhat more” likely to discuss the HPV vaccine with parents as a result of the campaign, and to recommend the vaccine since the start of the campaign. Two-thirds (65%) of the providers said they “occasionally” or “regularly” referred patients to the health department for the vaccine since the start of the campaign. When asked “Do you think the campaign influenced parents’ decisions to vaccinate their daughters?’ fifteen percent of providers thought it had a “great influence” while more than half (52%) thought it had a “moderate influence.” One-third (33%) thought the campaign had “no or a slight influence.”
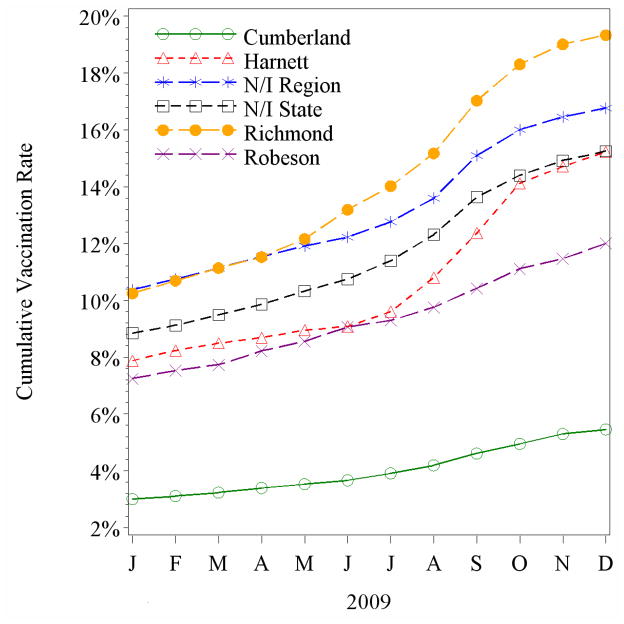
Comparison of HPV Immunization Rates
We compared percentages of girls ages 9–13 vaccinated in the four intervention counties with percentages vaccinated in non-intervention counties (Figure 2). After six months of the campaign (June-November, 2009), the changes in HPV vaccination rates among 9–13 year old girls in the intervention counties were both above (2 counties) and below (2 counties) changes in rates in non-intervention region or all counties in the rest of the state (Table 4). Richmond (7.1%) and Harnett counties (6.8%) had proportional increases significantly above the region (5.2%) and the state (5.0%) while rates in Robeson (3.2%) and Cumberland (1.9%) counties had proportional rate changes significantly below the region and state. Among 14–19 year olds, changes in HPV vaccination rates were significantly lower in Harnett (2.8%), Robeson (2.6%) and Cumberland (1.6%) counties than in the rest of the state (3.5%) and above the region (2.9%) only in Richmond county (3.7%).
Figure 2.
Cumulative HPV vaccination rates of girls, ages 9–13, by intervention county and non-intervention (N/I) region and state, 2009.
Table 4.
Proportion of girls ages 9–13 unvaccinated as of June 1, 2009 and who were vaccinated June 1 – November 30, 2009
| 96 non-intervention state | 9 non-intervention region | Richmond | Harnett | Robeson | Cumberland | |
|---|---|---|---|---|---|---|
| All | 5.04% (11,006/218,259) | 5.18% (710/13,716) | 7.08%1,2 (96/1,356) | 6.76%1,2 (189/2,794) | 3.23%1,2 (132/4,092) | 1.86%1,2 (218/11,721) |
| White | 4.79% (5,509/114,915) | 5.17% (417/8,069) | 5.95% (45/756) | 6.99%1,2 (121/1,732) | 4.56% (43/942) | 1.77%1,2 (92/5,209) |
| Black | 5.54% (3,084/55,676) | 5.45% (176/3,228) | 9.26%1,2 (46/497) | 6.90% (53/768) | 3.14%1,2 (33/1,050) | 1.81%1,2 (91/5,041) |
| Other races | 7.14% (563/7,882) | 9.14% (49/536) | 5.88% (3/51) | 14.29% (7/49) | 2.40%1,2 (42/1,751) | 2.08%1,2 (7/336) |
Source: North Carolina Immunization Registry (NCIR), 2009.
Notes. Sum of white, black, other does not add up to all because those with unknown races could not be used.
p<.01 comparing intervention county to the estimate for the 9 non-intervention counties in the region.
p<.01 comparing intervention county to the estimate for the 96 non-intervention counties in the state.
HPV vaccination rates by race also varied by county. A larger proportion of white girls ages 9–13 were vaccinated in Harnett (7.0%) and a smaller proportion were vaccinated in Cumberland (1.8%) county compared to the non-intervention counties in the region (5.2%) or state (4.8%). A larger proportion of black girls ages 9–13 were vaccinated in Richmond (9.3%) and smaller proportions in Robeson (3.1%) and Cumberland (1.8%), than in the region (5.5%) or state (5.5%). Lower proportions of girls of other races were vaccinated in Robeson (2.4%) and Cumberland (2.1%) than in the region (9.1%) or state (7.1%).
Discussion
The social marketing campaign initiated by county health departments in a primarily rural and racially diverse part of North Carolina increased HPV vaccine uptake among pre-teen girls for whom the vaccine is routinely recommended. Most mothers who responded to the survey had heard about or seen HPV vaccine campaign messages and materials during the three months of the intervention. Most of the mothers who reported campaign awareness also reported taking action, including talking with their daughter’s healthcare provider about HPV vaccine. Nearly all the healthcare providers who responded to the survey said they used the campaign brochures with parents and thought the campaign made a difference in parents’ decisions to vaccinate their daughters. Most importantly, we found an intervention effect in HPV immunization rates in two rural counties.
The findings in this study are consistent with those reported for other health communication campaigns, where effect sizes have been assessed as associations between awareness of a campaign and behavioral outcomes (Huhman et al., 2007; Potter, Judkins, Piesse, Nolin, & Huhman, 2008). The 2% higher vaccination rates in two intervention counties than in the non-intervention counties are a modest but significant difference. Evaluation of mothers’ awareness of HPV campaign messages and materials was another important way to detect an association between awareness and reported actions as a result of the campaign.
One strength of this HPV vaccine campaign is that it followed a process that included recommended elements of effective social marketing campaigns (Andreasen, 2006; Grier & Bryant, 2005). The campaign was designed to target mothers who were unaware, undecided, or opposed to HPV vaccination for their 11–12 year old daughters. Formative research, program development, and pretesting with racially diverse mothers in the intervention counties indicated that many were unaware that the vaccine was routinely recommended for pre-teens, that the vaccine was safe and effective and that doctors recommended it. Most had seen the vaccine manufacturer’s advertising yet they either thought the vaccine was for older girls or did not trust the source of the commercials. The source of the SCPPH campaign was the local health department, which was noted on all campaign materials and seen as a credible source in formative research. The channels (other than the virtually unused campaign website and unfunded hotline) were local retail establishments and healthcare providers – sources suggested as credible by the mothers and community leaders. Campaign materials were developed with the formative focus group research in mind and pre-tested with mothers through intercept interviews. Providers and the media were targeted as important influencers. These steps helped to shape the relevance of the campaign to racially diverse mothers of pre-teen girls who had not yet been vaccinated against HPV.
Evaluation of the campaign had several limitations, nevertheless. The mail survey of mothers from a marketing database may not be representative of mothers in the intervention counties or other areas with socioeconomic disparities, as responders tended to have higher incomes. Surveys were not conducted in non-intervention counties to assess possible exposure to the campaign. Placement of campaign materials was not completed in all four intervention counties. The providers’ survey may not be representative of providers in the four counties or other areas, as providers who completed surveys may have found the campaign more useful than those who did not respond. Finally, the immunization rates reported to NCIR may not reflect true population level vaccination rates in the counties because reports by providers are voluntary and incomplete.
Implications for Social Marketing and Lessons Learned
The importance of this locally sponsored campaign is that it reached mothers of daughters in the age group targeted for HPV vaccination. Targeting both healthcare providers and mothers was key, as placement of age-appropriate HPV vaccine materials in medical settings gave providers a tool they could use in talking with mothers about vaccination. The campaign successfully used traditional and small media to reach racially diverse mothers in this rural, underserved area. Greater saturation of materials in the two less populated counties may have been a factor in campaign success, and, by contrast a reason for lack of impact in the more populated counties with lower saturation.
Although our formative research indicated that mothers search the Internet for health information, few visitors to the project website were from the target area. We could not conclude whether a better strategy to drive mothers to the site would have worked or whether they searched sites other than the project website for information. Failure of the hotline during the campaign was problematic and unfixable, which demonstrates the importance of having a multi-component campaign. For maximum impact, we recommend use of campaign materials in late summer to coincide with back-to-school reminders for doctors’ visits and other pre-teen vaccinations (e.g., TdAP and meningococcal). Future research could evaluate replication of campaign components in other racially diverse, rural, and underserved areas to increase HPV vaccination among 11–12 year old girls.
Conclusion
The county-sponsored HPV vaccine social marketing campaign successfully targeted mothers of 11–12 year olds and the healthcare providers who serve them to increase vaccine uptake. This evaluation supports expansion of the pilot campaign in other rural and racially diverse areas to increase HPV vaccination among the age group for whom the vaccine is routinely recommended.
Acknowledgments
James L. Knight professorship funds from Dr. Jane Brown; support from the University Cancer Research Fund; South Central Partnership for Public Health for their initiative; Beth Quinn for NCIR collaboration; People Designs for marketing input; Emily Brostek, Ali K. Groves, Miriam Hartmann, Carrie Meier, Carmina G. Valle for message designs; Noel Brewer, Heather Gates, Cathy Melvin, Lisa Harrison, Amanda Dayton, Sabrina Boyce, Ashley Leighton, Terence Ng and Lacy Dean for project execution; Jane Brown and Heidi Hennick-Kaminski for manuscript review. This project was supported in part by Award Number UL1RR025747 from the National Center for Research Resources. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Contributor Information
Joan R. Cates, School of Journalism and Mass Communication at the University of North Carolina at Chapel Hill.
Autumn Shafer, School of Journalism and Mass Communication at the University of North Carolina at Chapel Hill.
Sandra J. Diehl, Lineberger Comprehensive Cancer Center at the University of North Carolina at Chapel Hill.
Allison M. Deal, Lineberger Comprehensive Cancer Center at the University of North Carolina at Chapel Hill.
References
- Akers A, Newman S, Smith JS. Factors underlying disparities in cancer incidence, Screening and treatment in the United States. Curr Prob Cancer. 2007;31(3):157–181. doi: 10.1016/j.currproblcancer.2007.01.001. [DOI] [PubMed] [Google Scholar]
- American Cancer Society. Annual Report to the Nation on the Status of Cancer, 1975–2004. Featuring Cancer in American Indians and Alaska Natives. 2007 doi: 10.1002/cncr.23044. Retrieved from http://www.cancer.org/docroot/MED/content/MED_2_1x_Annual_Report_to_the_Nation_Finds_Cancer_Death_Rate_Decline_Doubling.asp. [DOI] [PubMed]
- American Cancer Society. North Carolina Cervical Cancer Incidence, 2001–2005. By Race and County. 2008 Retrieved from http://www.schs.state.nc.us/SCHS/CCR/docs/NC_2008_CountyLevelData.pdf.
- Andreasen AR. Social marketing in the 21st century. Thousand Oaks, CA: Sage; 2006. [Google Scholar]
- Becker MH. The Health Belief Model and personal health behavior. Health Education Monographs, Monog. 1974:2. [Google Scholar]
- Bernat DH, Harpin SB, Eisenberg ME, Bearinger LH, Resnick MD. Parental support for the human papillomavirus vaccine. Journal of Adolescent Health. 2009;45(5):525–527. doi: 10.1016/j.jadohealth.2009.04.014. [DOI] [PubMed] [Google Scholar]
- Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: A theory-informed systematic review. Prev Med. 2007;45(2–3):107–114. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Cates JR, Brewer NT, Fazekas KI, Mitchell CE, Smith JS. Racial differences in HPV knowledge, HPV vaccine acceptability, and related beliefs among rural, Southern women. Journal of Rural Health. 2009;25(1):93–97. doi: 10.1111/j.1748-0361.2009.00204.x. [DOI] [PubMed] [Google Scholar]
- Cates JR, Shafer A, Carpentier FD, Reiter PL, Brewer NT, McRee AL, et al. How parents hear about human papillomavirus vaccine: Implications for uptake. Journal of Adolescent Health. 2010;47(3):305–308. doi: 10.1016/j.jadohealth.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National, state, and local area vaccination coverage among adolescents aged 13–17 Years --United States, 2008. Morbidity and Mortality Weekly Report. 2009;58(36):997–1001. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] Quadrivalent human papillomavirus vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP) Morbidity and Mortality Weekly Report. 2007;56(RR02):1–24. [PubMed] [Google Scholar]
- Dempsey AF, Abraham LM, Dalton V, Ruffin M. Understanding the reasons why mothers do or do not have their adolescent daughters vaccinated against human papillomavirus. Annals of Epidemiology. 2009;19(8):531–538. doi: 10.1016/j.annepidem.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards P, Roberts I, Clarke M, DiGuiseppi C, Wentz R, Kwan I, et al. The Cochrane collaboration. John Wiley & Sons; 2009. Methods to increase response to postal and electronic questionnaires. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Parental vaccine safety concerns in 2009. Pediatrics. 2010;125(4):654–659. doi: 10.1542/peds.2009-1962. [DOI] [PubMed] [Google Scholar]
- Gerend MA, Weibley E, Bland H. Parental response to human papillomavirus vaccine availability: Uptake and intentions. Journal of Adolescent Health. 2009;45(5):528–531. doi: 10.1016/j.jadohealth.2009.02.006. [DOI] [PubMed] [Google Scholar]
- Gottlieb SL, Brewer NT, Sternberg MR, Smith JS, Ziarnowski K, Liddon N, et al. Human papillomavirus vaccine initiation in an area with elevated rates of cervical cancer. Journal of Adolescent Health. 2009;45(5):430–437. doi: 10.1016/j.jadohealth.2009.03.029. [DOI] [PubMed] [Google Scholar]
- Grier S, Bryant CA. Social marketing in public health. Annual Review of Public Health. 2005;26(1):319–339. doi: 10.1146/annurev.publhealth.26.021304.144610. [DOI] [PubMed] [Google Scholar]
- Hughes J, Cates J, Liddon N, Smith J, Gottlieb S, Brewer N. Disparities in how parents are learning about the HPV vaccine. Cancer Epidemiology, Biomarkers & Prevention. 2009;18(2):363–372. doi: 10.1158/1055-9965.EPI-08-0418. [DOI] [PubMed] [Google Scholar]
- Huhman ME, Potter LD, Duke JC, Judkins DR, Heitzler CD, Wong FL. Evaluation of a national physical activity intervention for children: VERB(TM) Campaign, 2002–2004. American Journal of Preventive Medicine. 2007;32(1):38–43. doi: 10.1016/j.amepre.2006.08.030. [DOI] [PubMed] [Google Scholar]
- Kahn JA, Ding L, Huang B, Zimet GD, Rosenthal SL, Frazier AL. Mothers’ intention for their daughters and themselves to receive the human papillomavirus vaccine: A national study of nurses. Pediatrics. 2009;123(6):1439–1445. doi: 10.1542/peds.2008-1536. [DOI] [PubMed] [Google Scholar]
- Katz ML, Reiter PL, Heaner S, Ruffin MT, Post DM, Paskett ED. Acceptance of the HPV vaccine among women, parents, community leaders, and healthcare providers in Ohio Appalachia. Vaccine. 2009;27(30):3945–3952. doi: 10.1016/j.vaccine.2009.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotler P, Lee NR. Social marketing: Influencing behaviors for good. Thousand Oaks, CA: Sage; 2008. [Google Scholar]
- Lefebvre RC, Rochlin L. Social marketing. In: Glanz FMLK, Rimer BK, editors. Health behavior and health education: Theory, research, and practice. 2. San Francisco, CA: Jossey-Bass; 1997. [Google Scholar]
- National Cancer Institute [NCI] A snapshot of cervical cancer. 2009 Retrieved from http://www.cancer.gov/aboutnci/servingpeople/snapshots/cervical.pdf.
- Newmann SJ, Garner EO. Social inequities along the cervical cancer continuum: A structured review. Cancer Causes Control. 2005;16(1):63–70. doi: 10.1007/s10552-004-1290-y. [DOI] [PubMed] [Google Scholar]
- North Carolina Department of Health and Human Services. Immunize North Carolina: North Carolina Immunization Registry. 2010 Retrieved from http://www.immunizenc.com?NewImmRegistry.htm.
- North Carolina Rural Economic Development Center. Rural Data Bank. 2010 Retrieved from http://www.ncruralcenter.org/databank/index.html.
- Potter LD, Judkins DR, Piesse A, Nolin MJ, Huhman M. Methodology of the outcome evaluation of the VERB(TM) Campaign. American Journal of Preventive Medicine. 2008;34(6, Supplement 1):S230–S240. doi: 10.1016/j.amepre.2008.03.007. [DOI] [PubMed] [Google Scholar]
- Reiter PL, Brewer NT, Gottlieb SL, McRee A-L, Smith JS. Parents’ health beliefs and HPV vaccination of their adolescent daughters. Social Science & Medicine. 2009;69(3):475–480. doi: 10.1016/j.socscimed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- Rosenthal SL, Rupp R, Zimet GD, Meza HM, Loza ML, Short MB, et al. Uptake of HPV vaccine: Demographics, sexual history and values, parenting style, and vaccine attitudes. Journal of Adolescent Health. 2008;43(3):239–245. doi: 10.1016/j.jadohealth.2008.06.009. [DOI] [PubMed] [Google Scholar]
- Rothman SM, Rothman DJ. Marketing HPV vaccine: Implications for adolescent health and medical professionalism. JAMA. 2009;302(7):781–786. doi: 10.1001/jama.2009.1179. [DOI] [PubMed] [Google Scholar]
- Saraiya M, Ahmed F, Krichnan S, Richards TB, Unger ER, Lawson HW. Cervical cancer incidence in a prevaccine era. Obst Gynecol. 2007;109(2 pt1):360–370. doi: 10.1097/01.AOG.0000254165.92653.e8. [DOI] [PubMed] [Google Scholar]
- Shafer A, Cates JR, Diehl S, Hartmann M. Asking Mom:Formative research for an HPV vaccine campaign targeting mothers of adolescent girls. Journal of Health Communication. doi: 10.1080/10810730.2011.571343. (in press) [DOI] [PubMed] [Google Scholar]
- Snyder LB. Health communication campaigns and their impact on behavior. Journal of Nutrition Education and Behavior. 2007;39(2, Supplement 1):S32–S40. doi: 10.1016/j.jneb.2006.09.004. [DOI] [PubMed] [Google Scholar]
- Tiro JA, Meissner HI, Kobrin S, Chollette V. What do women in the U.S. know about human papillomavirus and cervical cancer? Cancer Epidemiol Biomarkers Prev. 2007;16(2):288–294. doi: 10.1158/1055-9965.EPI-06-0756. [DOI] [PubMed] [Google Scholar]
- U.S. Food and Drug Administration. Human papillomavirus vaccine. 2010 Retrieved from http://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm172678.htm.
- Yabroff KR, Lawrence WF, King JC, Mangan P, Washington KS, Yi B, et al. Geographic disparities in cervical cancer mortality: What are the roles of risk factor prevalence, screening, and use of recommended treatment? Journal of Rural Health. 2005;21(2):149–157. doi: 10.1111/j.1748-0361.2005.tb00075.x. [DOI] [PubMed] [Google Scholar]
- Zimet GD, Liddon N, Rosenthal SL, Lazcano-Ponce E, Allen B. Chapter 24: Psychosocial aspects of vaccine acceptability. Vaccine. 2006;24(Supplement 3):S201–S209. doi: 10.1016/j.vaccine.2006.06.017. [DOI] [PubMed] [Google Scholar]