Abstract
Pre-analytic variables, specifically cold ischemic time, have been implicated as key variables in the measurement of proteins by immunohistochemistry. To determine the significance and magnitude of antigenic loss due to pre-analytic variables, we have compared protein antigenicity in core needle biopsies, with essentially no cold ischemic time, to that in routinely processed tumor resection specimens. Two cohorts of matched core needle biopsies and tumor resections were collected with 20 matched pairs and 14 matched pairs, respectively. Both series were analyzed by quantitative immunofluorescence using the AQUA® method. Antibodies to phospho-ERK, total ERK, phospho-AKT, total AKT, phospho-S6K1, total S6K1, Estrogen Receptor, Ki67, cytokeratin and GAPDH were measured. Detection levels for all phospho-epitopes were significantly decreased in tumor resections compared to biopsies while no significant change was seen in the corresponding total proteins. Of the other four proteins examined, Estrogen Receptor and cytokeratin showed significant loss of antigenicity. This data suggests that measurement of phospho-protein antigenicity in formalin-fixed tissue by immunological methods is dramatically affected by pre-analytic variables. This study suggests that core needle biopsies are more accurate for assessment of tissue biomarkers.
Keywords: Antigenicity, biomarkers, core needle biopsy, ischemic time, phosphorylation, pre-analytical variables, resection tissue
Standard specimen preparation in anatomic pathology often involves long cold ischemic time or other pre-analytic variables. Pre-analytic variables are defined as conditions that can alter the diagnostic assessment of the tissue, particularly by immunological methods. The list of pre-analytic variables is long and can be studied on an individual basis or collectively considered as a “black box”.1. Individual studies have examined: 1) time interval starting from blood vessel ligation until fixation;2 2) the temperature of the specimen before formalin fixation;3and, 3) the rate of formalin penetration and biological inactivation.4 However, there are many other variables that are much harder to address, including things such as the brand and lot of formalin (with potential for minor but significant variations in concentration), the humidity in the air during the cold ischemic time, and even individual variations in surgical technique that could produce biological changes prior to the initiation of cold ischemia. In human tissue, the most rapid inactivation of biological processes occurs after the immediate fixation of a core needle biopsy. Core needle biopsies are a fairly standardized procedure. They facilitate quick formalin fixation with rapid biological inactivation, due to small diameter of specimens.4. Thus, in this study, we chose core needle biopsies as the standard, representing the minimal pre-analytic variation achievable in a human tissue system. We compared core needle biopsies to tumor resection specimens in the same patients. There are hundreds or thousands of uncontrolled variables in tumor resection specimens, compared to core needle biopsies. Because it is impractical – maybe impossible – to dissect out each variable, we treated the pre-analytic variables as a “black box” and assessed changes seen in tumor resections as compared to the defined standard, core needle biopsies.
Although the biological processes affected by pre-analytic variation are numerous, one of the most commonly assessed is phosphorylation.5 Phospho-protein markers of cell signaling have been broadly implicated in both translational research and clinical settings to predict the response to chemotherapy or prognosis. Response to EGFR inhibitors in lung cancer or glioblastoma and trastuzumab in breast cancer has been reported to be predicted by measurement of a series of phospho-protein markers including phospho-AKT (pAKT), phospho-ERK (pERK), and phospho-HER2 (pHER2).6-14 However, at least in some cases, reproduction of these findings has been difficult. Furthermore, a negative result (or even a series of negative results) may never be published to refute an observation that may be highly dependent on pre-analytic conditions. As a result, phospho-protein assessment has not become a standard companion diagnostic for any therapy, even though pre-clinical data suggests it would be both accurate and specific.5, 15-16
Recently, a group of oncologists and pathologists convened to set standards for immunohistochemical testing. When they examined the literature, they found relatively little information addressing the pre-analytic variation. Despite this, they produced a set of standards aimed at minimizing pre-analytical variation, first for Her217 and subsequently for ER.18 Their effort increased awareness of the pre-analytic variation issue and prompted us to take a quantitative look at the problem, with special attention to phospho-modified epitopes. First, we performed a pilot study of a series of samples on a tissue microarray (TMA). The results of that pilot prompted the more thorough study that follows, which assesses pairs of core needle biopsies and tumor resections for antigenicity levels of several proteins and phospho-proteins.
Materials and Methods
Cohorts
The formalin-fixed paraffin-embedded primary invasive breast cancer tumors were obtained from patients who underwent core needle biopsies and subsequent surgery at Yale University/New Haven Hospital from 1998 to 2005. All patients were diagnosed with infiltrating ductal carcinoma of the breast. The first cohort consisted of 20 paired core needle biopsies and tumor resections obtained from 1998 to 2000 from the archives of the Pathology Department of Yale University. This cohort was analyzed in a TMA format. The second cohort consisted of 14 paired core needle biopsies and tumor resections obtained from 2001 to 2005 from the archives of the Pathology Department of Yale University. This second cohort was analyzed in the conventional whole tissue section format. During this time period the estimated range of time to fixation was as short as 1 hour to as long as 4-5 hours. Data on age, type of procedure; size of specimen grossly; size of the tumor microscopically; the status of specimen upon receipt; ER, PR and HER2 status; node status; nuclear grade and histology grade are shown in Table 1. No patients received chemotherapy or radiation prior to resection. The median time from core needle biopsy to tumor resection was 27.5 days. The study was approved by the institutional review board for Yale University.
Table 1. Clinical Characteristics of Resection Tissues.
| Code | Age | Procedure | Tumor size (cm) | Specimen size (cm) | Upon receiving | ER | PR | HER2 | Node | Nuclear Grade | Histology Grade |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1R | 80 | M | 1.1×0.9×0.5 | 6.2×4×1 | fresh | P | P | N | N | 2 | 6 |
| 2R | 45 | M | 1.8×1.2×1.1 | 26×24.5×6 | fresh | P | P | N | N | 2 | 5 |
| 3R | 63 | L | 1.5×1.5×1.4 | 11.6×5.5×2 | fresh | P | P | N | N | 3 | 6 |
| 4R | 53 | L | 0.8×0.6 | 4.7×3×2.5 | fixed | P | P | N | (N1) | 2 | 4 |
| 5R | 52 | M (p) | 1.3×0.5×0.4 | 7.5×7×1 | fresh | P | P | (w)P | N | 2 | 5 |
| 6R | 51 | M (p) | 0.2 | 7×5×2 | fresh | P | P | N | N | N/D | N/D |
| 7R | 51 | L | 1.1 | 9×7×1.8 | fresh | P | P | N | N | 3 | 7 |
| 8R | 45 | L | 1.8 | 3.5×3×1 | fresh | N | N | (w)P | N | 3 | 3 |
| 9R | 75 | M | 5 | 17×13×4 | fresh | P | P | P | N | 3 | 3 |
| 10R | 40 | M (r) | 3.5 | 24×22×5 | fresh | P | P | (w)P | (N1) | 3 | 3 |
| 11R | 44 | M | 0.99 | 17×16×2.5 | fresh | P | P | P | N | 3 | 6 |
| 12R | 88 | L | 4 | 11×6×4.5 | fresh | N | N | (w)P | N | 2 | 7 |
| 13R | 39 | M (r) | 8.5 | 18×14×7 | fresh | N | N | N | (N2) | 3 | 2 |
| 14R | 78 | L | 1.5×1.2 | 5×4.5×2 | fresh | P | P | N | (N1) | 2 | 6 |
Abbreviations: R: Resection; M: Mastectomy; L: Lumpectomy; (p): partial; (r): radical; P: Positive; (w) P: weakly positive; N: Negative; N/D: Not Determined
Antibodies and Immunohistochemistry
The arrays and whole tissue sections were incubated at 60°C for 20 minutes before being deparaffinized with xylene, rehydrated, and antigen-retrieved by pressure cooking for 15 min in citrate buffer (pH = 6). Slides were preincubated with 0.3% bovine serum albumin in 0.1 mol/L TBS (pH = 8) for 30 min at room temperature. The procedure for pAKT staining was as follows: slides were incubated with a cocktail of pSer473-AKT antibody diluted at 1:1000 (Mouse monoclonal, clone 587F11; Cell Signaling Technology, Danvers, MA) and a wide-spectrum rabbit anti-cow cytokeratin antibody (Z0622; Dako Corp, Carpinteria, CA) diluted 1:100 in bovine serum albumin/TBS overnight at 4°C. This was followed by a 1-hr. incubation at room temperature with Alexa 546-conjugated goat anti-rabbit secondary antibody (A11010; Molecular Probes, Eugene, OR) diluted 1:100 in mouse EnVision reagent (K4001, Dako Corp, Carpinteria, CA). Cyanine 5 (Cy5) directly conjugated to tyramide (FP1117; Perkin-Elmer, Boston, MA) at a 1:50 dilution was used as the fluorescent chromogen for pAKT detection. Prolong mounting medium (Prolong Gold, P36931; Molecular Probes, Eugene, OR) containing 4′,6-diamidino-2-phenylindole was used to identify tissue nuclei. Other antibodies performed in a similar manner are listed in Table 2.
Table 2. Antibodies, epitiopes, sources and dilutions.
| Protein | Site | Species | Clone | Dilutions | Supplier |
|---|---|---|---|---|---|
| pAKT | Ser473 | Mouse mAb | 587F11 | 1:1000 | CST |
| AKT | Rabbit MAb | 11E7 | 1:1000 | CST | |
| pERK1/2 | Thr202/Tyr204 | Rabbit mAb | 20G11 | 1:1000 | CST |
| ERK1/2 | Mouse mAb | L34F12 | 1:1000 | CST | |
| pS6K1 | Thr389 | Mouse mAb | 1A5 | 1:350 | CST |
| S6K1 | Rabbit mAb | 49D7 | 1:450 | CST | |
| GAPDH | Rabbit mAb | 14C10 | 1:500 | CST | |
| Ki67 | Mouse mAb | B56 | 1:500 | BD Pharmingen | |
| ER | Mouse mAb | 1D5 | 1:50 | Dako | |
| pTyrosine | Tyr | Mouse mAb | 4G10 | 1:20000 | Upstate |
| p53 | Mouse mAb | DO-7 | 1:50 | Dako |
Automated Quantitative Analysis
Automated Quantitative Analysis (AQUA) allows exact measurement of protein concentration within subcellular compartments, as described in detail elsewhere.19-20 In brief, a series of high-resolution monochromatic images were captured by the PM-2000 microscope (HistoRx). For whole tissue sections, multiple regions of interest (ROIs) containing only invasive tumor were circled by investigators trained in histopathology on the AQUA system screen based on the cytokeratin (cytoplasm) image of the immunohistochemically stained slide taken with the AQUA system. The selected ROIs were automatically overlaid with a grid by the image capturing program and each field of view (FOV) was defined automatically. For each histospot of the TMA and each FOV of the whole tissue section, in- and out-of-focus images were obtained using the signal from the 4′,6-diamidino-2-phenylindole, cytokeratin-Alexa 546 and target protein-Cy5 channel. Target protein antigenicity was measured using a channel with emission maxima above 620 nm, in order to minimize tissue autofluorescence. Tumor was distinguished from stromal and non-stromal elements by creating an epithelial tumor “mask” from the cytokeratin signal. This created a binary mask (each pixel being either “on” or “off”) on the basis of an intensity threshold set by visual inspection of histospots. The AQUA score of the target protein in each subcellular compartment was calculated by dividing the target protein compartment pixel intensities by the area of the compartment within which they were measured. AQUA scores were normalized to the exposure time and bit depth at which the images were captured, allowing scores collected at different exposure times to be directly comparable. Standardization and reproducibility associated with AQUA are described elsewhere.21
Statistical analysis
The average values for target AQUA scores from duplicate histospots or from multiple ROFs were calculated and treated as independent continuous variables. The Wilcoxon Signed Rank test was employed to assess the paired differences, considered significant at a p-value less than 0.05. Error bars in the accompanying graphs represent 95% confidence interval (CIs). Power calculations based on a paired t-test were performed for each epitope (Table 3).
Table 3. Statistical Comparison Between Core Needle Biopsies and Tumor Resections with Experimental Power.
| Epitope | p value | Experiment Sample Size (pair) | Experiment Power | Sample Size Needed to give Power=0.80 (pair) | Coefficient of Variation for Loss of Epitope |
|---|---|---|---|---|---|
| pAKT | 0.0039 | 10 | 0.93 | 7 | 102% |
| AKT | 0.0645 | 10 | 0.74 | 12 | 138% |
| pERK | 0.0098 | 10 | 0.98 | 5 | 86% |
| ERK | 0.3750 | 10 | 0.21 | 90 | 380% |
| pS6K1 | 0.0020 | 10 | 0.99 | 2 | 52% |
| S6K1 | 0.2324 | 10 | 0.46 | 26 | 205% |
| ER | 0.0273 | 10 | 0.96 | 6 | 93% |
| Ki67 | 0.7910 | 10 | 0.10 | 516 | 914% |
| GAPDH | 0.4973 | 13 | 0.26 | 79 | 357% |
| Pan Cytokeratin | 0.0245 | 14 | 0.88 | 11 | 133% |
For each epitope of interest, a linear mixed-effects model was fit to the AQUA scores of ROFs from full histological sections. Individual model parameterizations were selected on the basis of the Akaike Information Criterion and Bayesian Information Criterion.22 These criteria guide selection of a parsimonious model by rewarding models for close prediction of observed data while penalizing them for use of additional parameters.
The form of the model is yikj = β0 + b0i + roij + (β1 + b1i)si + εijk, where i = 1,…,number of subjects; j = 1,…,number of ROI in subject i; k = 1,…,number of FOV in ROI j; and the factor si = 0 for core needle biopsy specimens and si = 1 for tumor resection specimens. The term εijk is the residual error. In other words, yikj represents the AQUA score of the kth FOV from the jth ROI of the ith patient. The parameters b0, b1 r0, εijk are assumed to be normally distributed with variances , , , respectively. This assumption was verified for all models. All analyses were performed with the R Program for Statistical Computing,23 nlme package.24
Results
Differences in biomarker expression in core needle biopsies vs. surgical tumor resections
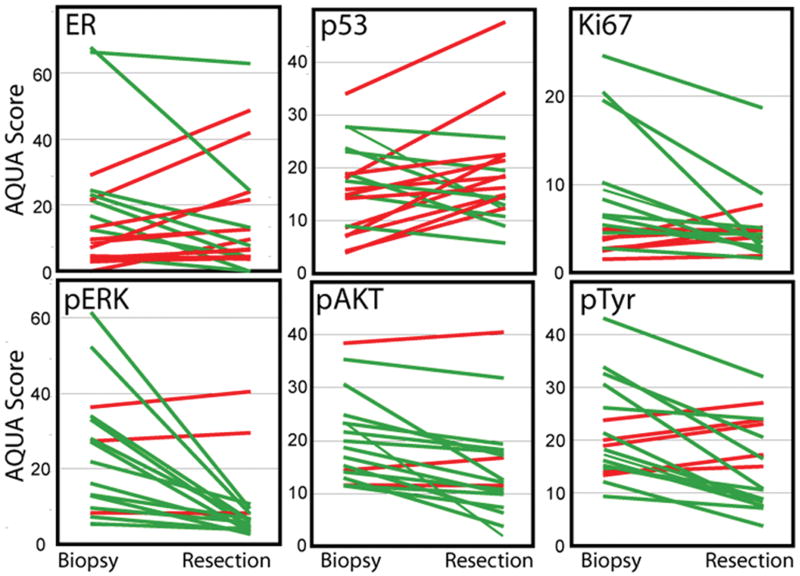
To determine if there is a difference in antigenicity between core needle biopsies and subsequent tumor resections, we performed a pilot study on 20 core needle biopsies and matched tumor resections on a tissue microarray. Antibodies to Estrogen Receptor (ER), Ki67, p53 and phospho-proteins including pERK, pAKT and phospho-tyrosine (pTyr) were immunofluorescently stained and the results were quantified by AQUA. Scores for each core needle biopsy and tumor resection were determined by the average of two TMA spots, then plotted in pairs as shown in Figure 1. Antigenicity of pERK, p-AKT, pTyr and Ki67 was decreased in tumor resections compared to that in core needle biopsies. ER and p53 exhibited no trend for reduction in tumor resections. In these TMA-based experiments no statistically significant differences were observed possibly due to heterogeneity between fields and/or the small amount of tissue assessed in a TMA. However, the trends seen in this pilot ultimately motivated a more complete assessment.
Figure 1.
Differences in biomarker expression in core needle biopsies vs. tumor resections. Twenty core needle biopsies and matched tumor resections were arrayed in TMA with 2-fold redundancy. 1.5-mm core from each tumor block was arrayed in a recipient block. The TMA was immunohistochemically stained with ER, p53, Ki67, pERK, pAKT and pTyr and the results were quantified using AQUA. Scores represent the average of two cores. Specimens that showed decreased staining in the resection relative to biopsy are shown in green; those with higher resection levels are shown in red.
Assessment of phosphor-protein epitope loss in paired whole tissue sections
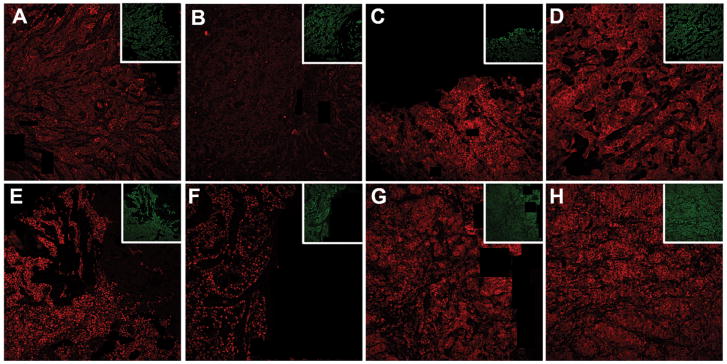
Toward a more comprehensive investigation, we assessed whole sections from matched pairs of core needle biopsies and tumor resection specimens. Representative pictures of pAKT, AKT, ER and GAPDH in biopsy tissues and paired tumor resection are shown in Figure 2. Both pAKT and ER show lower signal in a representative FOV from the tumor resection compared to the core needle biopsy (Fig. 2 A, B, E, and F), while total AKT and GAPDH appear to show no change (Fig. 2 C, D, G, and H) between the core needle biopsy and tumor resection.
Figure 2.
Comparison of biomarker staining images between biopsies vs. tumor resections on whole tissue section slides. Representative immunofluorescence staining of p-AKT (Red) in CNB (A) and tumor resection (B), AKT (red) in CNB (C) and tumor resection (D), ER (red) in CNB (E) and tumor resection (F), GAPDH (red) in biopsy (G) and tumor resection (H) were illustrated. Each corresponding Cytokeratin staining is shown as inset (Green). Photographs are shown at magnification of 20×.
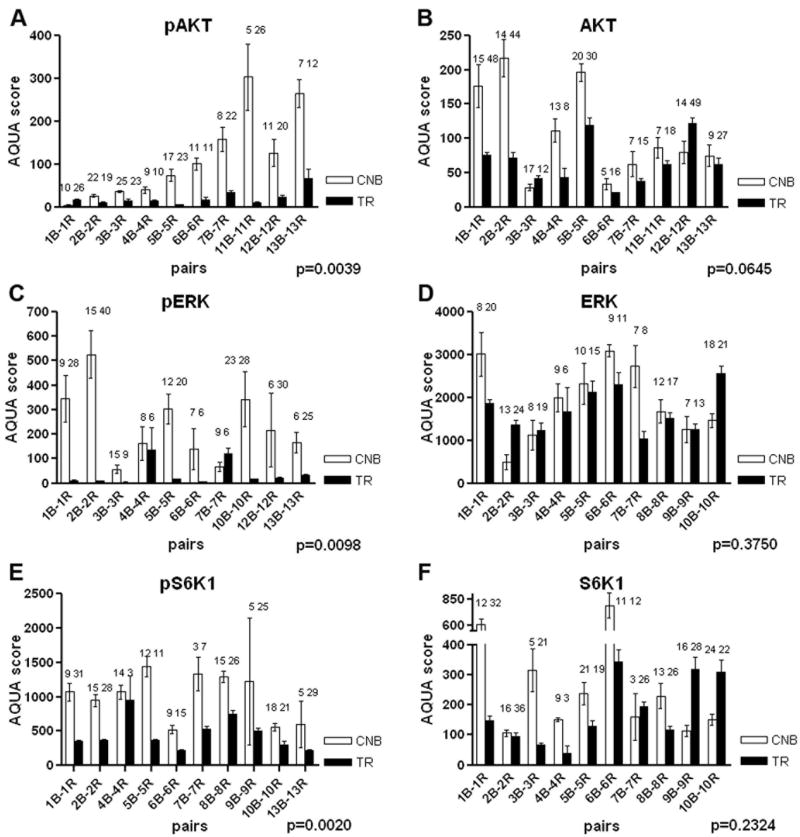
First, differences in phospho-protein antigenicity between core needle biopsies and tumor resections were assessed paired with a second antibody that recognized the protein, independent of phosphorylation status. Tissue sections were stained with antibodies of pAKT, AKT, pERK, ERK, pS6K1 and S6K1. Then each case pair was compared by taking the average of the AQUA scores over all FOVs in a specimen. The average number of FOV was 11 and 19 on each section of core needle biopsies and tumor resections, respectively. There were consistently and significantly lower levels of pAKT, pERK and pS6K1 (p<0.05) in the tumor resections than in the core needle biopsies, as evaluated by Wilcoxon Signed-Ranks tests (Fig. 3 A, C, and E). In contrast, the antigenicity of total AKT, ERK and S6K1 did not exhibit significant differences (p>0.05) (Fig.3 B, D, and F). However, our power calculations indicate that we did not have a large enough sample size to detect differences for the total protein epitopes. Due to the large variation between subjects in the amount of change between core needle biopsy and tumor resection for these epitopes, a larger sample size would be required to sufficiently power the study. The ratio of the standard deviation of decrease between subjects relative to the mean decrease can be summarized numerically as the coefficient of variation. A summary of the data with p-values, experimental power, calculated required sample size requirements, and coefficient of variation is shown in Table 3.
Figure 3.
Expression of phospho-proteins including pAKT, pERK and pS6K1 were decreased in tumor resections compared to those in biopsies. AQUA scores of each coded biopsy (core needle biopsies, open bars) and tumor resection (tumor resection, filled bars) in staining of pAKT (A), AKT (B), pERK (C), ERK (D), pS6K1 (E) and S6K1 (F) were assessed. The number on the top of each bar indicates number of field of view (FOV) included in the observation. Each AQUA data represents the mean ± 95% CI. N represents the number of FOVs. Comparisons between core needle biopsies and tumor resections were performed via the Wilcoxon Signed Rank test.
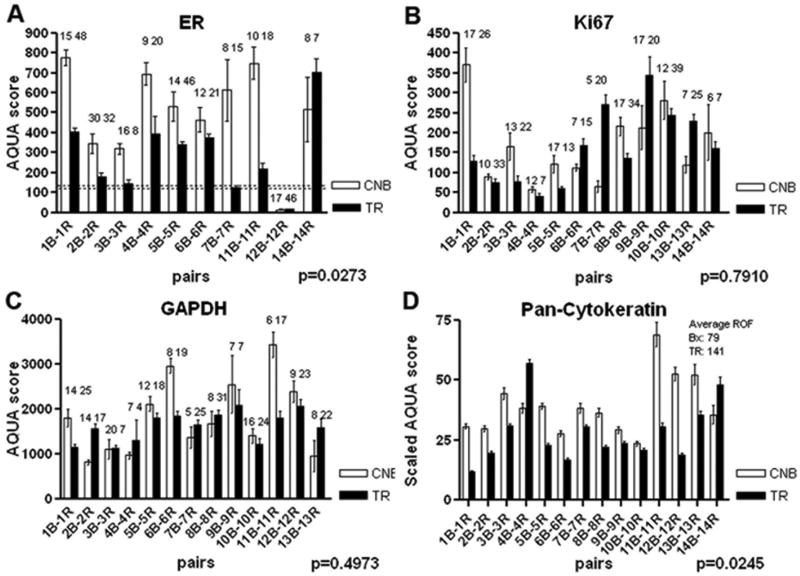
Assessment of non-phosphor-protein epitope loss in paired whole tissue sections
To determine if antigenic lability can be observed in proteins other than phospho-epitopes, we selected some other commonly used antibodies to determine the effects of cold ischemic time on routine reagents. We tested ER, Ki67, GAPDH and Cytokeratin antigenicity on paired tissue sections as above (Fig. 4). To binarize ER into a positive and negative score, a cut-point was determined using a series of 37 breast cancer cases with conventional ER scores defined by the standard clinical ER test. When ranked in order, the highest AQUA score in a clinically negative test was 108 and the lowest AQUA score for a clinically positive test was 118 (unpublished data). Thus, ER was defined as positive for all cases with AQUA score greater than 118 on the paired whole tissue sections. Both ER and Cytokeratin (AE1/AE3) showed statistically significant decreases in the tumor resection compared to the core needle biopsy. Neither Ki67 nor GAPDH showed significant reductions in the tumor resection specimens, but this may have been due to insufficient power. Ki67 especially showed a high coefficient of variation for epitope loss, likely due inherent biologic variability, and thus over 500 subjects are required to adequately power the study (Table 3). Because cytokeratin antigenicity is measured in each AQUA protocol procedure, it was included in all the experiments. As a result, the number of FOVs assessed for this marker is much higher; however much of the data is from serial sections, which are not truly independent FOVs. Additionally, in order to standardize the scores between AQUA procedures, we scaled all CK scores to a 100-point scale. The pooled data for each pair from the nine experiments, with the average number of FOVs equal to 79 and 141 from each core needle biopsy and tumor resection, respectively, showed a statistically significant reduction in the tumor resections compared to the core needle biopsies.
Figure 4.
Epitope-specific protein degradation in tumor resections. AQUA scores of each coded biopsy (core needle biopsy, open bars) and tumor resection (tumor resection, filled bars) in staining of ER (A), Ki67 (B), GAPDH (C), Pan-cytokeratin (D) were assessed. Raw Pan-cytokeratin scores were scaled to a 100-point scale. The number on the top of each bar indicates number of field of view (FOV)) included in the observation. Each AQUA data represents the mean ± 95% CI. n represents the number of FOVs. Comparisons between core needle biopsiess and tumor resections were performed via the Wilcoxon Signed Rank test.
Statistical Comparison Between Core Needle Biopsies and Tumor Resections with Experimental Power
After we established the statistical significance of the epitope loss between core needle biopsies and tumor resections, we used linear mixed-effects models to quantify those differences. Variation between individual subjects' magnitude of epitope loss was also significant, as demonstrated in the coefficient of variation for epitope loss (Table 3). Furthermore, loss of different epitopes was not uniform across individual subjects. For example, loss of signal from one epitope and gain of signal from another were seen in the same individual (Supplemental Fig. 1). This shows both variations as a function of tumor heterogeneity as well as variation in time to fixation.
Discussion
As protein biomarkers are now being used to determine therapy, the importance of accurate measurement has increased. This has led to the observation that many events that occur prior to fixation of the tissue (pre-analytic variables) can be critically important. Even the best tests can only measure epitopes that are present on the slide, so the stability of these epitopes during the time between loss of circulation and fixation may be a key factor in their accurate measurement. Variables that can affect the stability of these epitopes include local pH changes, anoxic or ischemic biological reactions, loss of specificity of proteases or phosphatases. All these may result in alterations of post-translational modification and possible transcription of apoptotic factors beginning at the time the blood supply is clamped off.5, 25-28 Although this list of pre-analytic variables is incomplete, in this work we focus specifically on signaling protein phosphorylation. There is evidence that intrinsic enzymatic activity from slowly fixed endogenous phosphotase in large specimens results in the dephosphorylation of biomarkers.29-30 The papers and findings reported here suggest that measurement of phospho-modification is essentially impossible in routinely collected surgical resection specimens.
In this work, we define core needle biopsies as a standard with the assumption that the procedure allows rapid fixation and prevents pre-analytic artifacts. While we believe this is the closest we can come to assessment of live tissue, we have no evidence that artifacts do not occur in the short time between obtaining the core and cross-linking by formalin. However, the fact that measurement of phospho-proteins spans a range of expression in our small case series suggests that at least some of the activity of signaling proteins can be assessed using this technique. This suggests that if phospho-specific markers are critical to companion diagnostic testing, surgical protocols should be altered to include a core needle biopsy of the lesion immediately prior to surgery for diagnostic testing purposes.
If core needle biopsies' assessment is considered to reveal the “truth”, it would be interesting to determine if some protein expression marker could be used to normalize or adjust for degradation due to pre-analytic variables. As cytokeratin staining was done on each specimen as part of the AQUA process, we tested whether normalization of the phospho-protein AQUA scores by the degradation seen in cytokeratin in the tumor resections would more accurately reflect the levels of phospho-protein seen in the core needle biopsies. Our data indicated that AQUA scores of pAKT, pERK, pS6K1 and ER were still lower after pan-CK normalization (data not shown). While it may be possible in the future to find a method of normalization or qualification of tissue for companion diagnostic assay assessment, we believe it will not be possible to normalize for post-translational modifications. We are currently working on intrinsic controls for assessment of tissue quality.
Of the targets studied in this work, only ER is in clinical usage today. The current standard of practice for ER has recently been reviewed and an ASCO/CAP committee has issued standards that include issues related to cold ischemic time. 18. Our work supports the need for those standards as, shown here, the levels of ER in tumor resection specimens was significantly lower than in core needle biopsy specimens. It is common practice to assess ER and PR on core needle biopsy specimens; nonetheless, it is not required. Although none of the cases in this study changed from a designation of ER-positive to a designation of ER-negative between the core needle biopsy and the tumor resection, three cases were very close to negative in the tumor resection while clearly positive in the core needle biopsy (Fig. 4A). In a broader collection of cases, it is highly likely we would see changes in patient ER status resulting in changes in endocrine therapy as a function of which specimen was assayed.
While this work shows quantitative loss of detection for a range of biomarkers, there are several limitations. Specifically, in each setting, we sampled specimens from only 10 to 14 patients. While statistical significance is observed, it would be valuable to validate these results in other labs. Importantly, our power calculations demonstrate that, for every epitope without a significant difference between core needle biopsy and tumor resection, the sample size was insufficient. Thus, further investigation is needed to establish the affect of pre-analytical variables on measurement of non-phospho markers, such as Ki67. This data has led to funding that will assess larger cohorts in the future, including measured time to fixation, which is not available for these specimens. An additional weakness of this work, and essentially all work associated with assessment of core needle biopsies, is representation. In each case we were able to quantify only a limited number of FOVs from each core needle biopsy. Furthermore, we have no way of determining whether a core needle biopsy was representative of an entire tumor. Our previous work suggests that there is substantial heterogeneity in ER expression when multiple tissue blocks are assessed in larger cases.31-32 Heterogeneity may explain the observation that rare cases show higher average expression in the resection than in the core biopsy. For example, case 14 in figure 4A shows higher average levels in the resection, even though all other cases trend in the opposite direction. Finally, another weakness of this work is the fact that that the core needle biopsy was not taken at the same time as the tumor resection. As this was a retrospective collection of tissue, we collected core needle biopsies that were taken as part of routine patient management and which were followed by resections. It is possible that assessment of tumors where the core needle biopsy and tumor resection are taken simultaneously would show different results. A further limitation is that while AQUA is now used in one clinical laboratory, it is not the common standard for assessment of antibody/antigen interactions. However, the immunofluorescence method is identical to DAB based chromogenic studies in detection of antigen. That is, the primary antibody step is the same. The difference is in visualization, where the use of fluorescent visualization methods is easier to accurately quantify. Thus it is important to emphasize that the conclusions we draw from this work are a function of the tissue assessed, not a function of the method of assessment. This is confirmed by work published while this manuscript was under review that showed qualitative assessment of loss of pAKT and pERK using chromogenic stains 33 Nonetheless, work is underway toward the goal of developing quantitative methods that work for chromogenic visualization methods that can be used to assess this and other expression patterns in tissue.
In summary, this work quantitatively assesses the effect of delayed formalin fixation on surgical resections by using biopsies as standardized controls. Although it is a limited set of experiments, all three phospho-antibodies tested showed significant degradation in the resection specimens. These results indicate that conventional resection tissues with uncontrolled cold ischemic time should not be used for companion diagnostic testing, at least for the five antibodies shown to be affected here. This work also suggests that any antibody planned for use on resection specimens should be validated for resistance to cold ischemic time.
Supplementary Material
Supplemental Figure 1. Variation in Epitope Loss by Subject. Average decrease in AQUA Score between core needle biopsyand tumor resection as estimated by a mixed-effects model grouped by subject and by epitope.
Acknowledgments
We thank Dr. Valsamo K. Anagnostou and Dr. Maria Baquero for technical assistance and helpful discussions.
Grant Support: Grant Number R01CA45708; Grant Numbers TL 1 RR024137 and KL2 RR024138 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research; Grant Number 2007080 from the Doris Duke Charitable Foundation; and the CTSA Grant Number UL1 RR024139.
Footnotes
Disclosure/conflicts of Interest: Drs. Rimm and Camp are founders, stockholders, and consultants to HistoRx Inc
References
- 1.Werner M, Chott A, Fabiano A, Battifora H. Effect of formalin tissue fixation and processing on immunohistochemistry. Am J Surg Pathol. 2000;24:1016–9. doi: 10.1097/00000478-200007000-00014. [DOI] [PubMed] [Google Scholar]
- 2.De Cecco L, Musella V, Veneroni S, et al. Impact of biospecimens handling on biomarker research in breast cancer. BMC Cancer. 2009;9:409. doi: 10.1186/1471-2407-9-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Micke P, Ohshima M, Tahmasebpoor S, et al. Biobanking of fresh frozen tissue: RNA is stable in nonfixed surgical specimens. Lab Invest. 2006;86:202–11. doi: 10.1038/labinvest.3700372. [DOI] [PubMed] [Google Scholar]
- 4.Start RD, Cross SS, Smith JH. Assessment of specimen fixation in a surgical pathology service. J Clin Pathol. 1992;45:546–7. doi: 10.1136/jcp.45.6.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baker AF, Dragovich T, Ihle NT, Williams R, Fenoglio-Preiser C, Powis G. Stability of phosphoprotein as a biological marker of tumor signaling. Clin Cancer Res. 2005;11:4338–40. doi: 10.1158/1078-0432.CCR-05-0422. [DOI] [PubMed] [Google Scholar]
- 6.Kirkegaard T, Witton CJ, McGlynn LM, et al. AKT activation predicts outcome in breast cancer patients treated with tamoxifen. J Pathol. 2005;207:139–46. doi: 10.1002/path.1829. [DOI] [PubMed] [Google Scholar]
- 7.Modi S, DiGiovanna MP, Lu Z, et al. Phosphorylated/activated HER2 as a marker of clinical resistance to single agent taxane chemotherapy for metastatic breast cancer. Cancer Invest. 2005;23:483–7. doi: 10.1080/07357900500201301. [DOI] [PubMed] [Google Scholar]
- 8.Cappuzzo F, Magrini E, Ceresoli GL, et al. Akt phosphorylation and gefitinib efficacy in patients with advanced non-small-cell lung cancer. J Natl Cancer Inst. 2004;96:1133–41. doi: 10.1093/jnci/djh217. [DOI] [PubMed] [Google Scholar]
- 9.Haas-Kogan DA, Prados MD, Lamborn KR, Tihan T, Berger MS, Stokoe D. Biomarkers to predict response to epidermal growth factor receptor inhibitors. Cell Cycle. 2005;4:1369–72. doi: 10.4161/cc.4.10.2105. [DOI] [PubMed] [Google Scholar]
- 10.Haas-Kogan DA, Prados MD, Tihan T, et al. Epidermal growth factor receptor, protein kinase B/Akt, and glioma response to erlotinib. J Natl Cancer Inst. 2005;97:880–7. doi: 10.1093/jnci/dji161. [DOI] [PubMed] [Google Scholar]
- 11.Baselga J, Tripathy D, Mendelsohn J, et al. Phase II study of weekly intravenous recombinant humanized anti-p185HER2 monoclonal antibody in patients with HER2/neu-overexpressing metastatic breast cancer. J Clin Oncol. 1996;14:737–44. doi: 10.1200/JCO.1996.14.3.737. [DOI] [PubMed] [Google Scholar]
- 12.Svensson S, Jirstrom K, Ryden L, et al. ERK phosphorylation is linked to VEGFR2 expression and Ets-2 phosphorylation in breast cancer and is associated with tamoxifen treatment resistance and small tumours with good prognosis. Oncogene. 2005;24:4370–9. doi: 10.1038/sj.onc.1208626. [DOI] [PubMed] [Google Scholar]
- 13.Cappuzzo F, Finocchiaro G, Metro G, et al. Clinical experience with gefitinib: an update. Crit Rev Oncol Hematol. 2006;58:31–45. doi: 10.1016/j.critrevonc.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Yamashita H, Nishio M, Kobayashi S, et al. Phosphorylation of estrogen receptor alpha serine 167 is predictive of response to endocrine therapy and increases postrelapse survival in metastatic breast cancer. Breast Cancer Res. 2005;7:R753–64. doi: 10.1186/bcr1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mann GB, Fahey VD, Feleppa F, Buchanan MR. Reliance on hormone receptor assays of surgical specimens may compromise outcome in patients with breast cancer. J Clin Oncol. 2005;23:5148–54. doi: 10.1200/JCO.2005.02.076. [DOI] [PubMed] [Google Scholar]
- 16.Hodi Z, Chakrabarti J, Lee AH, et al. The reliability of assessment of oestrogen receptor expression on needle core biopsy specimens of invasive carcinomas of the breast. J Clin Pathol. 2007;60:299–302. doi: 10.1136/jcp.2006.036665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wolff AC, Hammond ME, Schwartz JN, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–45. doi: 10.1200/JCO.2006.09.2775. [DOI] [PubMed] [Google Scholar]
- 18.Hammond ME, Hayes DF, Dowsett M, et al. American Society of Clinical Oncology/College of American Pathologists Guideline Recommendations for Immunohistochemical Testing of Estrogen and Progesterone Receptors in Breast Cancer. J Clin Oncol. 2010;28:2784–95. doi: 10.1200/JCO.2009.25.6529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Camp RL, Chung GG, Rimm DL. Automated subcellular localization and quantification of protein expression in tissue microarrays. Nat Med. 2002;8:1323–7. doi: 10.1038/nm791. [DOI] [PubMed] [Google Scholar]
- 20.Moeder CB, Giltnane JM, Harigopal M, et al. Quantitative justification of the change from 10% to 30% for human epidermal growth factor receptor 2 scoring in the American Society of Clinical Oncology/College of American Pathologists guidelines: tumor heterogeneity in breast cancer and its implications for tissue microarray based assessment of outcome. J Clin Oncol. 2007;25:5418–25. doi: 10.1200/JCO.2007.12.8033. [DOI] [PubMed] [Google Scholar]
- 21.Gustavson MD, Molinaro AM, Tedeschi G, Camp RL, Rimm DL. AQUA analysis of thymidylate synthase reveals localization to be a key prognostic biomarker in 2 large cohorts of colorectal carcinoma. Arch Pathol Lab Med. 2008;132:1746–52. doi: 10.5858/132.11.1746. [DOI] [PubMed] [Google Scholar]
- 22.Pinheiro JCP, Bates DM. Mixed-Effects Models in S and S-PLUS. Berlin: Springer; 2000. [Google Scholar]
- 23.R_Core_Development_Team R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2009. [Google Scholar]
- 24.Pinheiro JC, Douglas Bates, Saikat DebRoy, Deepayan Sarkar, the R Core Team Nlme . R package version 3.1-96 edn. 2009. Linear and Nonlinear Mixed Effects Models. [Google Scholar]
- 25.Kingsbury AE, Foster OJ, Nisbet AP, et al. Tissue pH as an indicator of mRNA preservation in human post-mortem brain. Brain Res Mol Brain Res. 1995;28:311–8. doi: 10.1016/0169-328x(94)00219-5. [DOI] [PubMed] [Google Scholar]
- 26.Cross SS, Start RD, Smith JH. Does delay in fixation affect the number of mitotic figures in processed tissue? J Clin Pathol. 1990;43:597–9. doi: 10.1136/jcp.43.7.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Srinivasan M, Sedmak D, Jewell S. Effect of fixatives and tissue processing on the content and integrity of nucleic acids. Am J Pathol. 2002;161:1961–71. doi: 10.1016/S0002-9440(10)64472-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Allen J, Winterford C, Axelsen RA, Gobe GC. Effects of hypoxia on morphological and biochemical characteristics of renal epithelial cell and tubule cultures. Ren Fail. 1992;14:453–60. doi: 10.3109/08860229209047652. [DOI] [PubMed] [Google Scholar]
- 29.Espina V, Edmiston KH, Heiby M, et al. A portrait of tissue phosphoprotein stability in the clinical tissue procurement process. Mol Cell Proteomics. 2008;7:1998–2018. doi: 10.1074/mcp.M700596-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin TA, Lin TN, He YY, Hsu CY, Sun GY. Effects of focal cerebral ischemia on inositol 1,4,5-trisphosphate 3-kinase and 5-phosphatase activities in rat cortex. Biochem Biophys Res Commun. 1992;184:871–7. doi: 10.1016/0006-291x(92)90671-7. [DOI] [PubMed] [Google Scholar]
- 31.Chung GG, Zerkowski MP, Ghosh S, Camp RL, Rimm DL. Quantitative analysis of estrogen receptor heterogeneity in breast cancer. Lab Invest. 2007;87:662–9. doi: 10.1038/labinvest.3700543. [DOI] [PubMed] [Google Scholar]
- 32.Chen C, Peng J, Xia H, et al. Quantum-dot-based immunofluorescent imaging of HER2 and ER provides new insights into breast cancer heterogeneity. Nanotechnology. 21:95101. doi: 10.1088/0957-4484/21/9/095101. [DOI] [PubMed] [Google Scholar]
- 33.Pinhel IF, Macneill FA, Hills MJ, Salter J, Detre S, A'Hern R, Nerurkar A, Osin P, Smith IE, Dowsett M. Extreme loss of immunoreactive p-Akt and p-Erk1/2 during routine fixation of primary breast cancer. Breast Cancer Res. 2010;12:R76. doi: 10.1186/bcr2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Variation in Epitope Loss by Subject. Average decrease in AQUA Score between core needle biopsyand tumor resection as estimated by a mixed-effects model grouped by subject and by epitope.