Abstract
Objective To compare the effects of laparoscopic hysterectomy and abdominal hysterectomy in the abdominal trial, and laparoscopic hysterectomy and vaginal hysterectomy in the vaginal trial.
Design Two parallel, multicentre, randomised trials.
Setting 28 UK centres and two South African centres.
Participants 1380 women were recruited; 1346 had surgery; 937 were followed up at one year.
Primary outcome Rate of major complications.
Results In the abdominal trial laparoscopic hysterectomy was associated with a higher rate of major complications than abdominal hysterectomy (11.1% v 6.2%, P = 0.02; difference 4.9%, 95% confidence interval 0.9% to 9.1%) and the number needed to treat to harm was 20. Laparoscopic hysterectomy also took longer to perform (84 minutes v 50 minutes) but was less painful (visual analogue scale 3.51 v 3.88, P = 0.01) and resulted in a shorter stay in hospital after the operation (3 days v 4 days). Six weeks after the operation, laparoscopic hysterectomy was associated with less pain and better quality of life than abdominal hysterectomy (SF-12, body image scale, and sexual activity questionnaires).
In the vaginal trial we found no evidence of a difference in major complication rates between laparoscopic hysterectomy and vaginal hysterectomy (9.8% v 9.5%, P = 0.92; difference 0.3%, -5.2% to 5.8%), and the number needed to treat to harm was 333. We found no evidence of other differences between laparoscopic hysterectomy and vaginal hysterectomy except that laparoscopic hysterectomy took longer to perform (72 minutes v 39 minutes) and was associated with a higher rate of detecting unexpected pathology (16.4% v 4.8%, P = < 0.01). However, this trial was underpowered.
Conclusions Laparoscopic hysterectomy was associated with a significantly higher rate of major complications than abdominal hysterectomy. It also took longer to perform but was associated with less pain, quicker recovery, and better short term quality of life. The trial comparing vaginal hysterectomy with laparoscopic hysterectomy was underpowered and is inconclusive on the rate of major complications; however, vaginal hysterectomy took less time.
Introduction
In 1996 Stovall and Summitt concluded that well designed clinical trials examining short term outcomes, economics, and quality of life were required to determine the role of laparoscopic hysterectomy.1 Ten previous randomised trials have compared outcomes for abdominal hysterectomy with laparoscopic hysterectomy.2-11 Most of these were from single centres of endoscopic surgical excellence and had small study populations. Each trial showed that laparoscopic hysterectomy was associated with reduced hospital stay and, in most studies, a shorter time to convalescence and notably less pain than abdominal hysterectomy.
Oonly four previously published randomised trials have compared the outcomes of vaginal hysterectomy and laparoscopic hysterectomy.12-15 The only difference shown in these studies was that laparoscopic hysterectomy took longer to perform.
We know of no previous trials that were powered to investigate the safety of the various procedures. We have therefore undertaken a concurrent pair of randomised controlled trials to eVALuate the relative roles of Vaginal, Abdominal, and Laparoscopic hysterectomy in routine gynaecological practice.
Methods
Design
We conducted two parallel, multicentre, randomised trials concurrently. The first compared laparoscopic hysterectomy with abdominal hysterectomy (abdominal trial), and the second compared laparoscopic hysterectomy with vaginal hysterectomy (vaginal trial). Both trials had the same management structure, eligibility criteria, and outcome measures.
We obtained approval for recruitment in South Africa according to local practice. An independent trial steering committee and a data monitoring and ethics committee oversaw the trials.
Participants
Patients who needed a hysterectomy for non-malignant conditions were eligible; excluded were patients who had a second or third degree uterine prolapse, a uterine mass greater than the size of a 12 week pregnancy, a medical illness precluding laparoscopic surgery, or a requirement for bladder or other pelvic support surgery, and patients who refused consent.
Gynaecologists were responsible for recruitment and on clinical grounds entered patients for randomisation into either the abdominal or the vaginal trial. Follow up of patients took place in a clinic at six weeks and then by postal questionnaire, at four months and one year after their operation.
To minimise potential effects due to a learning curve, each surgeon had to have performed at least 25 of each procedure. Cases could be used for teaching, providing the main assistant was the recruiting gynaecologist.
Interventions
Surgical procedures were as currently practised, with four approaches to laparoscopic hysterectomy: laparoscopic hysterectomy, laparoscopic assisted vaginal hysterectomy, laparoscopic supracervical hysterectomy, and total laparoscopic hysterectomy. All conversions were documented. Each surgeon's practice standardised antibiotics, analgesia, anticoagulants, anaesthetic care, and advice concerning resumption of normal activities over the three types of operation.
Outcome measures
The primary end point of the trials was the occurrence of at least one major complication (box 1). Major haemorrhage was regarded as a major complication if a blood transfusion was required, minor otherwise; haematoma was a major complication if surgical drainage was required, minor otherwise. An independent clinical reviewer differentiated between major and minor anaesthetic problems. Secondary end points were minor complications (box 2), blood loss, pain measured by a visual analogue scale and analgesia requirements, and questionnaire assessments of sexual activity,16 body image,17 and health status (SF-12).18
Sample size
The sample size for the abdominal trial was based on detecting a relative reduction in complication rates of 50% from 9%19; 487 patients in each arm were 80% power and 5% significance (two sided), not corrected for continuity.19
The complication rate in the vaginal trial was expected to be 4% for vaginal hysterectomy.20 To detect a 50% reduction in this rate, 1141 patients were required per treatment arm. As vaginal hysterectomy was performed relatively infrequently we did not expect to recruit this number but wanted to collect the randomised data as this would represent the largest such trial of vaginal hysterectomy that we are aware of.
Box 1: Major complications
Major haemorrhage (requiring transfusion)
Haematoma requiring transfusion or surgical drainage
Bowel injury
Ureteric injury
Bladder injury
Pulmonary embolus
Major anaesthesia problems
Unintended laparotomy
Wound dehiscence
Box 2: Minor complications
Haemorrhage not requiring transfusion
Infection: chest, urinary, wound, pelvic, other; or fever ≥ 38°C on any single occasion
Haematoma (spontaneous drainage)
Deep vein thrombosis
Cervical stump problems
Minor anaesthesia problems
Others
Randomisation
We chose a 2:1 unbalanced randomisation to provide more exposure to data on the new laparoscopic procedure and to reduce the potential impact of any remaining learning curve, with little loss of power. Patients were allotted to either the abdominal or vaginal trial according to the individual surgeon's usual practice. Randomisation to the selected conventional approach or laparoscopic hysterectomy alternative was made by telephone access to a computer-generated randomisation programme held at the Northern and Yorkshire Clinical Trials Research Unit. We minimised randomisation by proposed trial, surgeon, intended removal of ovaries, and body mass index (≤ 30 or > 30).
Statistical methods
The primary analysis was by intention to treat. We also performed a secondary analysis of the primary end point, according to the procedure that was started (per protocol analysis).
We used χ2 tests to compare the primary outcome. We also did sensitivity analysis, assuming that patients not having an operation would not have had a major complication, and then assuming that they would. We used logistic regression to adjust the major complication rate for the stratification factors of body mass index and intended removal of the ovaries.
The analysis of minor complication rates and of the rate of additional pathology found during the operation was the same as for major complications. Patients recorded pain and use of opiates in a daily diary booklet, scored on day 0 (operation day) and then days 2, 7, and 21 after the operation. We used analysis of covariance to adjust average pain scores over days 0-6 by the number of days opiates were used. We calculated length of procedure as time in minutes from first incision to last suture and length of stay as operation to day of discharge. We planned no formal statistical testing on these times.
We assessed quality of life at randomisation; before the operation; and six weeks, four months, and one year after the operation. We used analysis of covariance to adjust for prerandomisation questionnaires (baseline). For patients having a laparoscopic hysterectomy we used a series of univariate logistic regression models to identify predictors of major complications.
Results
Forty three gynaecologists from 28 UK and two South African centres recruited 876 patients into the abdominal trial and 504 into the vaginal trial between November 1996 and September 2000. The recruitment target in the abdominal trial was therefore not reached. The trial steering committee closed the trials in September 2000 because funding ended and the rate of recruitment decreased.
Demography
Baseline characteristics were well matched in each of the allocated trials (table 1). The baseline characteristics between the two trials differed. More than 90% of the patients allocated to the vaginal trial had had one or more vaginal deliveries compared with less than 85% in the abdominal trial. This distribution was reversed for caesarean deliveries. Only one of 30 patients with palpable endometriosis was allocated to the vaginal trial. Patients with pelvic pain, more than one indication for hysterectomy, a fixed uterus, no uterine descent, or intended removal of the ovaries were more likely to be allocated to the abdominal trial.
Table 1.
Baseline characteristics of participants in the two trials. Values are numbers (percentages) of participants unless otherwise indicated
|
Abdominal trial
|
Vaginal trial
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Abdominal hysterectomy (n=292) | Laparoscopic hysterectomy (n=584) | Vaginal hysterectomy (n=168) | Laparoscopic hysterectomy (n=336) | ||||
| Mean (SD) age | 41.2 | (7.6) | 41.7 | (7.2) | 40.8 | (6.5) | 40.9 | (6.9) |
| Mean (SD) body mass index | 25.9 | (5.4) | 26.6 | (5.1) | 26.5 | (4.7) | 26.4 | (5.1) |
| Mode number of pregnancies (% ever pregnant) | 2 | (90.7) | 2 | (91.4) | 2 | (95.2) | 2 | (96.7) |
| Vaginal deliveries mode (% having at least one vaginal delivery) | 2 | (83.4) | 2 | (80.9) | 2 | (91.0) | 2 | (94.3) |
| Caesarean deliveries mode (% having at least one caesarean section) | 0 | (16.9) | 0 | (19.1) | 0 | (9.6) | 0 | (10.2) |
| Vaginal capacity: | ||||||||
| Narrow | 14 | (4.8) | 32 | (5.5) | 8 | (4.8) | 7 | (2.1) |
| Normal | 275 | (94.2) | 549 | (94.0) | 157 | (93.5) | 322 | (95.8) |
| Large | 2 | (0.7) | 2 | (0.3) | 2 | (1.2) | 4 | (1.2) |
| Palpable endometriosis | 10 | (3.4) | 19 | (3.3) | 1 | (0.6) | 0 | (0.0) |
| Current smoker | 142 | (48.6) | 241 | (41.3) | 72 | (42.9) | 131 | (39.0) |
| Previous pelvic surgery | 185 | (63.3) | 368 | (63.0) | 102 | (60.7) | 197 | (58.6) |
| Mean (minimum to maximum) uterine size (expressed as equivalent to weeks of pregnancy) | 6 | (0 to 12) | 6 | (0 to 12) | 6 | (0 to 12) | 6 | (0 to 12) |
The mean waiting times for the operations were similar, about 70 days. The main indications for hysterectomy were dysfunctional uterine bleeding (874/1380 cases, 63%), fibroids (235 cases, 17%), pelvic pain (151 cases, 11%), endometriosis (126 cases, 9%), and failed ablation (104 cases, 8%).
Numbers analysed
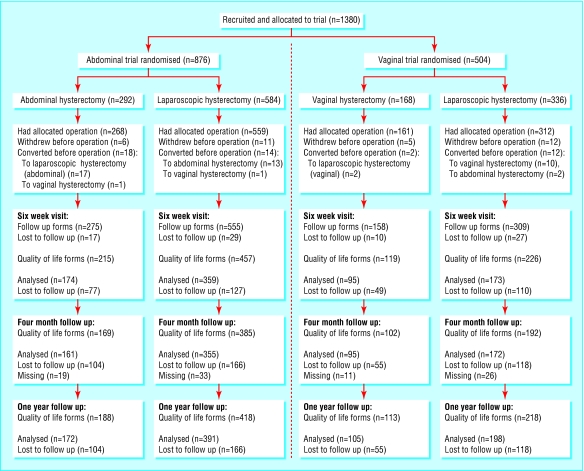
The figure shows the flow of patients through the trials. We performed a per protocol analysis as 46 (3.3%) patients were allocated to one procedure but had an alternative operation because of preoperative conversion (patient's decision (25 cases, 54%) and surgeon's unavailability (10 cases, 22%)). We undertook sensitivity analyses for the 34 patients who did not actually have an operation. Reasons for withdrawing preoperatively were mainly cancelled operations (25 cases, 74%).
Figure 1.
Flow of participants through the trials. Among patients whose procedures were converted, 283 underwent abdominal hysterectomies and 576 laparoscopic hysterectomies in the abdominal trial; 173 underwent vaginal hysterectomies and 314 laparoscopic hysterectomies in the vaginal trial. Follow up forms not received within the appropriate time frames were not included in the analysis. The time frames were 14 days at six weeks and 28 days at four months and one year
Primary outcome
Table 2 details the major complications. Patients had up to four major complications. Of particular importance in the abdominal trial were severe haemorrhage following laparoscopic hysterectomy (4.6%) and abdominal hysterectomy (2.4%), as well as ureteric injuries in both trials. All six of the damaged ureters occurred in the laparoscopic hysterectomy arms. Unintended laparotomy was the second most common complication, affecting 45 patients; of these 13 had another major complication. The reasons given for the other conversions included additional pathology, poor access, removal of ovarian cyst, unable to secure haemostasis, and endometrial cancer.
Table 2.
Primary end point of both trials: major complications. Values are numbers (percentages) of participants
|
Abdominal trial
|
Vaginal trial
|
|||
|---|---|---|---|---|
| Abdominal hysterectomy (n=292) | Laparoscopic hysterectomy (n=584) | Vaginal hysterectomy (n=168) | Laparoscopic hysterectomy (n=336) | |
| Major haemorrhage | 7* (2.4) | 27* (4.6) | 5 (2.9) | 17 (5.1) |
| Bowel injury | 3 (1) | 1 (0.2) | 0 | 0 |
| Ureteric injury | 0 | 5 (0.9) | 0 | 1 (0.3) |
| Bladder injury | 3 (1) | 12* (2.1) | 2 (1.2) | 3 (0.9) |
| Pulmonary embolus | 2 (0.7) | 1 (0.2) | 0 | 2 (0.6) |
| Anaesthesia problems | 0 | 5* (0.9) | 0 | 2 (0.6) |
| Unintended laparotomy: | ||||
| Intraoperative conversion | 1† (0.3) | 23 (3.9) | 7 (4.2) | 9 (2.7) |
| Return to theatre | 1 (0.3) | 3 (0.5) | 0 | 1 (0.3) |
| Wound dehiscence | 1 (0.3) | 1 (0.2) | 0 | 1 (0.3) |
| Haematoma | 2 (0.7) | 4 (0.7) | 2 (1.2) | 7 (2.1) |
| Other complications | 0 | 0 (0) | 1 (0.6) | 0 (0) |
| At least one major complication | 18 (6.2) | 65 (11.1) | 16 (9.5) | 33 (9.8) |
A patient may have had more than one complication.
These patients converted procedure before the operation: one patient undergoing abdominal hysterectomy converted to laparoscopic hysterectomy before the operation in the abdominal trial and had a major haemorrhage. Two patients in the abdominal trial who were undergoing laparoscopic hysterectomy converted to abdominal hysterectomy before the operation and had a major haemorrhage. One patients undergoing laparoscopic hysterectomy in the abdominal trial converted to abdominal hysterectomy before the operation and had a major anaesthetic problem. One patient undergoing laparoscopic hysterectomy in the abdominal trial converted to abdominal hysterectomy before the operation and had a bladder injury.
This patient in the abdominal trial was randomised to abdominal hysterectomy, converted to laparoscopic hysterectomy before the operation, and then converted back to abdominal hysterectomy during the operation.
In the abdominal trial significantly more patients undergoing laparoscopic hysterectomy than patients undergoing abdominal hysterectomy had at least one major complication (11.1% v 6.2%, mean difference 4.9%, 95% confidence interval 0.9% to 9.1%; odds ratio 1.91, 1.11 to 3.28). The number needed to treat to harm was 20. In this trial the odds of having a major complication was approximately twice as likely for patients undergoing laparoscopic hysterectomy.
We found no difference in the complication rates after the two procedures in the vaginal trial (9.8% for laparoscopic hysterectomy, 9.5% for vaginal hysterectomy (n = 18), mean difference 0.3%, -5.2% to 5.8%, P = 0.92; odds ratio 0.97, 0.52 to 1.81); the number needed to treat to harm was 333. However, this trial was not powered to detect a difference.
Per protocol and sensitivity analyses narrowed the size of difference between the types of operation for both trials, but the difference remained in the same direction. Adjustment for stratification factors made little difference to treatment effects.
Secondary outcomes
Minor complications—In the abdominal trial the percentage of patients who had at least one minor complication was 27.1% in patients undergoing abdominal hysterectomy compared with 25.2% for laparoscopic hysterectomy, and in the vaginal trial 27.9% for patients undergoing vaginal hysterectomy and 23.2% for laparoscopic hysterectomy (table 3). We found no evidence to show that there was any difference in minor complication rates between the procedures (P > 0.05) in any of the comparisons (intention to treat and sensitivity).
Table 3.
Secondary end points of both trials: minor complications. Values are numbers (percentages) of patients
|
Abdominal trial
|
Vaginal trial
|
|||
|---|---|---|---|---|
| Abdominal hysterectomy (n=292) | Laparoscopic hysterectomy (n=584) | Vaginal hysterectomy (n=168) | Laparoscopic hysterectomy (n=336) | |
| Major haemorrhage | 3 (1) | 8 (1.4) | 2 (1.2) | 8 (2.4) |
| Anaesthesia problems | 0 (0) | 2 (0.3) | 1 (0.6) | 3 (0.9) |
| Fever | 9 (3.1) | 29 (4.9) | 12 (7.1) | 18 (5.4) |
| Infection | 47 (16.1) | 86 (14.7) | 24 (14.3) | 36 (10.7) |
| Haematoma | 17 (5.8) | 25 (4.3) | 10 (5.9) | 14 (4.2) |
| Deep vein thrombosis | 0 (0) | 2 (0.3) | 0 | 0 |
| Other complications | 22 (7.5) | 40 (6.8) | 17 (10.1) | 24 (7.1) |
| At least one minor complication | 79 (27.1) | 147 (25.2) | 47 (27.9) | 78 (23.2) |
A patient may have had more than one complication.
Additional pathology found during the operation—In the abdominal trial additional pathology was reported in 12.7% (373/292) of patients undergoing abdominal hysterectomy compared with 22.6% (132/584) undergoing laparoscopic hysterectomy (mean difference -9.9%, -15.4 to -4.4%, P = < 0.01). In the vaginal trial the rates were 4.8% (8/168) for vaginal hysterectomy and 16.4% (53/336) for laparoscopic hysterectomy (mean difference -11.6%, -17.7% to -5.5%, P = < 0.01). The main additional findings were adhesions, endometriosis, and fibroids.
Pain—In the abdominal trial abdominal hysterectomy was more painful than laparoscopic hysterectomy (adjusted mean pain score 3.9 abdominal hysterectomy, 3.5 laparoscopic hysterectomy; mean difference 0.4, 0.09 to 0.7, P = 0.01). A slightly higher proportion of patients undergoing abdominal hysterectomy used opiates than patients undergoing laparoscopic hysterectomy (80% v 76%). We found no evidence of a difference in pain scores in the vaginal trial. In this trial a higher proportion of patients undergoing vaginal hysterectomy (71%, 119/168) used opiates than patients undergoing laparoscopic hysterectomy (62%, 209/336).
Length of surgery and length of stay—Table 4 summarises the data for length of procedure. In the abdominal trial the median (minimum, maximum) length of stay after abdominal hysterectomy was four (1, 36) days and three (1, 36) days after laparoscopic hysterectomy, and in the vaginal trial three (1, 16) days after vaginal hysterectomy and three (1, 19) days after laparoscopic hysterectomy. In the abdominal trial only 60% 177/292of patients who underwent abdominal hysterectomy were discharged by day 4 compared with 80% (492/584) after laparoscopic hysterectomy; in the vaginal trial 80% of patients in both the vaginal hysterectomy arm (135/168) and the laparoscopic hysterectomy arm (269/336) were discharged by day 4. We undertook no formal statistical testing, but these differences may be clinically important.
Table 4.
Length of surgery in minutes, from first incision to last suture
|
Abdominal trial
|
Vaginal trial
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Length of surgery | Abdominal hysterectomy (n=292) | Laparoscopic hysterectomy (n=584) | Vaginal hysterectomy (n=168) | Laparoscopic hysterectomy (n=336) | ||||
| Median (95% Cl) | 50 | (48 to 53) | 84 | (80 to 85) | 39 | (35 to 42) | 72 | (66 to 77) |
| Minimum (maximum) | 19 | (155) | 10 | (325) | 14 | (168) | 21 | (220) |
| Mean | 55.2 | 85.9 | 46.6 | 76.5 | ||||
| Mean difference between trial arms (95% Cl) | −30.7 | (−34.9 to −26.4) | −29.9 | (−35.9 to −23.9) | ||||
Quality of life—All procedures were associated with improvements in the physical and mental components of SF-12, body image scale, and aspects of sexual activity at four months compared with baseline. These changes were maintained or improved further at 12 months. In the abdominal trial we found a highly significant difference in the physical component summary score of the SF-12 at six weeks between abdominal hysterectomy and laparoscopic hysterectomy (score -5.1, 95% confidence interval -7.1 to -3.2, P < 0.01). We also found highly significant differences in body image scale between abdominal hysterectomy and laparoscopic hysterectomy in the abdominal trial at six weeks (1.5, 0.5 to 2.4, P ≤ 0.01), a borderline significant difference at four months (1.1, 0.06 to 2.1, P = 0.06) but no difference at 12 months (table 5). According to the sexual activity questionnaire “habit” scores in this trial were higher at six weeks after laparoscopic hysterectomy than after abdominal hysterectomy (-0.3, 0.1 to 0.6, P ≤ 0.01). We found no evidence of a difference in quality of life at any time point in the vaginal trial.
Table 5.
Mean (SD) SF-12 scores (abdominal trial). Difference at each time point
| Baseline (n=668) | Six weeks (n=449) | Four months (n=438) | One year (n=478) | |||||
|---|---|---|---|---|---|---|---|---|
| Physical component summary* | ||||||||
| Abdominal hysterectomy | 45.6 | (11.5) n=221 | 41.7 | (9.7) n=148 | 51.6 | (8.6) n=134 | 52.7 | (9.3) n=148 |
| Laparoscopic hysterectomy | 44.9 | (11.7) n=447 | 46.8 | (10.1) n=301 | 52.6 | (8.6) n=304 | 53.6 | (8.4) n=330 |
| Difference (95% Cl) | 0.6 | (−1.2 to 2.5) | −5.1 | (−7.1 to −3.2) | −1.0 | (−2.8 to 0.7) | −0.9 | (−2.5 to 0.8) |
| P value | — | <0.001 | 0.25 | 0.32 | ||||
| Mental component summary | ||||||||
| Abdominal hysterectomy | 45.3 | (11.3) n=221 | 51.9 | (10.8) n=148 | 51.8 | (9.5) n=134 | 51.9 | (10.2) n=148 |
| Laparoscopic hysterectomy | 45.8 | (11.7) n=447 | 50.0 | (11.4) n=301 | 50.9 | (10.5) n=304 | 50.7 | (10.7) n=330 |
| Difference (95% Cl) | −0.5 | (−2.4 to 1.4) | 1.8 | (−0.4 to 4.0) | 0.8 | (−1.3 to 2.9) | 1.1 | (−0.9 to 3.2) |
| P value | — | 0.11 | 0.44 | 0.27 | ||||
|
Body image scale results (abdominal trial): mean (SD) and difference at each time point†
| ||||||||
|
|
Baseline (n=813)
|
6 weeks (n=529)
|
4 months (n=505)
|
1 year (n=555)
|
||||
| Abdominal hysterectomy | 9.0 | (7.9)(n=270) | 5.2 | (5.9)(n=172) | 4.4 | (6.3) n=159 | 4.1 | (5.7)(n=168) |
| Laparoscopic hysterectomy | 8.8 | (8.1)(n=540) | 3.7 | (4.9)(n=357) | 3.3 | (4.9)(n=346) | 3.4 | (5.2)(n=387) |
| Difference (95% Cl) | 0.2 | (−0.9 to 1.4) | 1.5 | (0.5 to 2.4) | 1.1 | (0.06 to 2.1) | 0.7 | (−0.2 to 1.7) |
| P value | — | 0.01 | 0.06 | 0.13 | ||||
A high score represents a better quality of life.
A low score represents a better body image.
Predictors of major complication—Uterine descent and method of haemostasis of the uterine the ovarian pedicles were identified as significant predictors of major complications in patients undergoing laparoscopic hysterectomy (table 6). The vascular pedicles were sutured in only 7% (68/920) of cases, but this was associated with 25% (24/98) of all major complications; insufficient data were available to investigate this further.
Table 6.
Odds ratios and 95% confidence intervals for predictive variables for laparoscopic hysterectomies
| Variable (comparison) | Odds ratio (95% CI) | P value |
|---|---|---|
| Previous pelvic surgery (yes v no) | 0.87 (0.56 to 1.33) | 0.51 |
| Uterine mobility (fixed v freely mobile) | 1.22 (0.54 to 2.78) | 0.64 |
| Vaginal capacity (narrow v normal, large) | 1.91 (0.82 to 4.46) | 0.16 |
| Palpable endometriosis (yes v no) | 2.31 (0.75 to 7.11) | 0.18 |
| Uterine descent (no descent v first degree) | 1.84 (1.05 to 3.21) | 0.02 |
| Type of incision: | ||
| Laparoscopic hysterectomy v other
|
1.08 (0.23 to 5.03)
|
0.32 |
| Laparoscopic assisted vaginal hysterectomy v other
|
1.73 (0.40 to 7.4)
|
|
| Total laparoscopic hysterectomy v other | 0.90 (0.14 to 5.67) | |
| No of incisions (1-3 v 4-6) | 1.08 (0.66 to 1.75) | 0.77 |
| Uterine size (per additional week) | 1.05 (0.98 to 1.11) | 0.15 |
| Maximum intra-abdominal distension pressure: | ||
| ≤10 v ≥20 mm Hg
|
0.91 (0.19 to 4.14)
|
0.74 |
| 11-≤20 v ≥20 mm Hg | 1.21 (0.69 to 2.11) | |
| Haemostasis of uterine pedicle: | ||
| Bipolar v other
|
1.65 (0.36 to 7.2)
|
0.04 |
| Linear stapler v other
|
1.48 (0.31 to 7.1)
|
|
| Suture v other | 2.89 (0.68 to 12.3) | |
| Haemostasis of ovarian pedicle: | ||
| Bipolar v other
|
1.23 (0.43 to 3.56)
|
<0.001 |
| Linear stapler v other
|
1.59 (0.53 to 4.79)
|
|
| Suture v other | 7.09 (2.29 to 21.99) |
Discussion
The results of the two trials confirm the advantages to the patient of avoiding a laparotomy incision. In the abdominal trial laparoscopic hysterectomy was associated with a clinically relevant higher incidence of major complications and took longer to perform. These disadvantages were offset by patient friendly benefits of less pain, shorter hospital stay, quicker recovery, and improved quality of life indicators in the short term. The comparison between laparoscopic and vaginal methods was underpowered but did not show any significant differences between the two methods, except that vaginal hysterectomy was performed in a shorter time.
Laparoscopic hysterectomy is a relatively new approach to hysterectomy and is infrequently performed in the United Kingdom. In 1995 only 3% of 37 000 hysterectomies in the VALUE study were performed by this method.21 Both potential advantages and disadvantages are associated with this approach compared with the standard approaches of abdominal hysterectomy and vaginal hysterectomy, and these parallel trials attempted to investigate these differences.
Limitations of the study
Abdominal and vaginal hysterectomy are both commonly performed; 564 865 were performed in the United States22 and more than 65 000 in the United Kingdom in 1995.21 Despite this large number of potential patients we anticipated that recruiting sufficient numbers of surgeons and patients to this trial would be difficult. Most gynaecologists have well defined indications for each approach, and few would feel comfortable in randomising all patients to any approach. To allow each surgeon to maintain equipoise and maximise recruitment we designed this study as two separate but parallel trials. For similar reasons we excluded some conditions, such as large fibroids, for which most surgeons would prefer to undertake an abdominal hysterectomy, and major degrees of uterovaginal prolapse, for which almost all would undertake a vaginal hysterectomy. This pragmatic approach excluded many patients and several of the most important indications for hysterectomy. These decisions will reduce the generalisability of the study. We believe, however, that the design maximised recruitment of surgeons and patients and concentrated the study where the indications as to preferred method were least clear.
Including unintended laparotomy as a major complication caused debate in the trial's steering committee. It represented the second most common major complication, and a large proportion of these patients did not have any other complication. It could be considered that such conversions represented prudent surgery rather than a major complication. Excluding them would have substantially reduced the overall complication rates associated with both laparoscopic hysterectomy and vaginal hysterectomy. We think that on balance they represented a failure of planned procedure and should be considered as major complications.
Abdominal versus laparoscopic hysterectomy
The eVALuate study confirmed the results of previous smaller studies2-11 and showed in the abdominal trial that laparoscopic hysterectomy caused less pain and was associated with shorter hospital stay than abdominal hysterectomy. Severity of pain is difficult to quantify in the postoperative phase. Variable amounts of several different types of analgesics were taken. We therefore adjusted pain scores according to the number of days on which opiates were used, and when we used this measure laparoscopic hysterectomy in the abdominal trial was still associated with less pain. Patients undergoing laparoscopic hysterectomy in the abdominal trial also felt better in the early weeks of convalescence, as judged by improvements in the physical component of the SF-12 and body image scale at six weeks. In the abdominal trial after laparoscopic hysterectomy sexual activity habit scores were higher at six weeks than after abdominal hysterectomy. Overall the compliance with quality of life questionnaires was excellent, but only 60% (828/1380) of patients returned questionnaires at all three time points. These results should therefore be confirmed by others.
The primary end point of the trial was the risk of major complications. In the abdominal trial this study provides strong evidence of a substantial and clinically relevant increase in the risk of a major complication associated with laparoscopic hysterectomy compared with abdominal hysterectomy. If the benefits of the laparoscopic approach are to be realised on a large scale, it is essential that these risks are widely recognised and additional techniques and technology to reduce these risks are developed and evaluated.
Vaginal versus laparoscopic hysterectomy
The vaginal trial was underpowered, and its results are inconclusive. It is, however, still a large trial comparing laparoscopic hysterectomy with vaginal hysterectomy. The confidence intervals around the major complication rates show a possible difference of 5% in major complication rates in either direction. Laparoscopic hysterectomy in the vaginal trial took almost twice as long as vaginal hysterectomy. Our study, however, contained cases of low technical challenge. Technically more difficult cases were mostly selected to the abdominal hysterectomy arm, and this limits generalisability. Unexpected pathology in the vaginal trial was detected more often during laparoscopic hysterectomy than vaginal hysterectomy. Even when the indication for the hysterectomy was dysfunctional uterine bleeding, additional pathology was found in 5% of patients undergoing vaginal hysterectomy and 15% of patients undergoing laparoscopic hysterectomy. We have no data about whether these findings led to additional treatment or affected subsequent outcomes. Surgeons must make a value judgment about whether improved diagnostic accuracy justifies the additional operating time for laparoscopic hysterectomy.
Prediction of major complications (laparoscopic hysterectomy)
The study was sufficiently large to indicate an association between the techniques used for laparoscopic hysterectomy, particularly those used to secure the ovarian blood vessels, and the risk of subsequent major complications. These results should be confirmed by others.
What is already known on this topic
Hysterectomy is one of the most often performed of all major surgical operations
It has traditionally been performed by either the vaginal or the abdominal method
Either method has advantages and disadvantages, but the indications for each remain controversial and have never been compared in a randomised controlled trial
More recently a third method of hysterectomy has been developed, laparoscopic hysterectomy
What this study adds
Two parallel trials compared the new technique of laparoscopic hysterectomy to the traditional vaginal and the abdominal method
The results confirm the advantages to the patient of avoiding a laparotomy incision
In the abdominal trial laparoscopic hysterectomy was associated with a clinically relevant higher incidence of major complications and took longer to perform than the abdominal method
With laparoscopic hysterectomy, patients have less pain, shorter hospital stay, quicker recovery, and improved quality of life indicators in the short term
Vaginal hysterectomy is quicker than laparoscopic hysterectomy
Supplementary Material
 A complete list of members of the study group is on bmj.com
A complete list of members of the study group is on bmj.com
We thank all members of the trial steering committee, data monitoring committee, and ethics committee for their hard work in the conduct of this trial, and Derek Tuffnell for his assistance with the independent clinical review of the research data. We thank the Simon Foundation and the University of Teesside for their support of the principal investigator as Simon professor of gynaecology during this study. In addition, the trial would not have been possible without the valued contributions of the women who were willing to give their time and share their experiences to extend our knowledge in this area. The eVALuate Trial including the full data analysis is reported in a submission to the HTA Monograph Series.
Contributors: RG was principal investigator, conceived the study, designed the trial, recruited patients, contributed to data analysis and wrote the manuscript. SM and JF contributed to the preparation of the manuscript and along with VN and JB all working from NYCTU helped design the trial, store and analyse the data. JH, JA, RC, GP, and MW were research fellows who collected much of the data, performed many of the interventions and coordinated with patients involved in the study. RL was concerned with the primary design of the trial and the analysis of the data. SB was involved with the implementation of the trial and data analysis.
Funding: This study was supported by a grant from the National Health Service Research and Development Health Technology Assessment Programme. The views and opinions expressed in the paper do not necessarily reflect those of the NHS Executive.
Competing interests: None declared.
Ethical approval: The trials received approval from the multicentre research ethics committee and the local research ethics committee.
References
- 1.Stoval TG, Summitt RL. Laparoscopic hysterectomy—is there a benefit? N Engl J Med 1996;335: 512-3. [DOI] [PubMed] [Google Scholar]
- 2.Summitt RL, Stovall TG, Steege JF, Lipscomb GH. A multicentre randomized comparison of laparoscopically assisted vaginal hysterectomy and abdominal hysterectomy in abdominal hysterectomy candidates. Obstet Gynaecol 1998;92: 321-6. [PubMed] [Google Scholar]
- 3.Lumsden MA, Twaddle S, Hawthorn R, Traynor I, Gilmore D, Davis J, et al. A randomised comparison and economic evaluation of laparoscopic-assisted hysterectomy and abdominal hysterectomy. Br J Obstet Gynaecol 2000;107: 1386-91. [DOI] [PubMed] [Google Scholar]
- 4.Perino A, Cucinella G, Venezia R, Castelli A, Cittadini E. Total laparoscopic hysterectomy versus total abdominal hysterectomy: an assessment of the learning curve in a prospective randomized study. Hum Reprod 1999;14: 2996-9. [DOI] [PubMed] [Google Scholar]
- 5.Falcone TMD, Paraiso MFR, Mascha EMS. Prospective randomized trial of laparoscopically assisted vaginal hysterectomy versus total abdominal hysterectomy. Am J Obstet Gynecol 1999;180: 955-62. [DOI] [PubMed] [Google Scholar]
- 6.Marana R, Busacca M, Zupi E, Garcea N, Paparella P, Catalano GF. Laparoscopically assisted vaginal hysterectomy versus total abdominal hysterectomy: a prospective, randomized, multicenter study. Am J Obstet Gynaecol 1999;180: 270-5. [DOI] [PubMed] [Google Scholar]
- 7.Ollson J, Ellström M, Hahlin M. A randomised prospective trial comparing laparoscopic and abdominal hysterectomy. Br J Obstet Gynaecol 1996;103: 345-50. [DOI] [PubMed] [Google Scholar]
- 8.Nezhat F, Nezhat C, Gordon S, Wilkin F. Laparoscopic versus abdominal hysterectomy. J Reprod Med 1992;37: 247-50. [PubMed] [Google Scholar]
- 9.Phipps JH, Nayak JS. Comparison of laparoscopic assisted vaginal hysterectomy and bilateral salpingo-oophorectomy with conventional abdominal hysterectomy and bilateral salpingo-oophorectomy. Br J Obstet Gynaecol 1993;100: 698-700. [DOI] [PubMed] [Google Scholar]
- 10.Raju KS, Auld BH. A randomized prospective study of laparoscopic vaginal hysterectomy versus abdominal hysterectomy each with bilateral salpingo-ophorectomy. Br J Obstet Gynaecol 1994;101: 1068. [DOI] [PubMed] [Google Scholar]
- 11.Langebrekke A, Eraker R, Nesheim B, Urnes A, Busund B, Sponland G. Abdominal hysterectomy should not be considered as a primary method for uterine removal. Acta Obstet Gynaecol Scand 1996;75: 404-7. [DOI] [PubMed] [Google Scholar]
- 12.Soriano S, Goldstein A, Lecuru F, Darai E. Recovery from vaginal hysterectomy compared with laparoscopy-assisted vaginal hysterectomy. Acta Obstet Gynaecol 2001;80: 337-41. [PubMed] [Google Scholar]
- 13.Summitt RL, Stovall TG, Lipscombe GH, Ling RW. Randomized comparison of laparoscopy-assisted vaginal hysterectomy with standard vaginal hysterectomy in an outpatient setting. Obstet Gynaecol 1992;80: 895-9. [PubMed] [Google Scholar]
- 14.Richardson RE, Bournas N, Magios AL. Is laparoscopic hysterectomy a waste of time? Lancet 1995;345: 36-41. [DOI] [PubMed] [Google Scholar]
- 15.Ottosen C, Lingman G, Ottosen L. Three methods for hysterectomy: a randomised, prospective study of short-term outcome. Br J Obstet Gynaecol 2000;107: 1380-5. [DOI] [PubMed] [Google Scholar]
- 16.Thirlaway K, Fallowfield L, Cuzick J. The sexual activity questionnaire: a measure of women's sexual functioning. Qual Life Res 1996;5: 81-90. [DOI] [PubMed] [Google Scholar]
- 17.Hopwood P, Fletcher I, Lee A, Al Ghazal S. A body image scale for use with cancer patients. Eur J Cancer 2001;37: 189-97. [DOI] [PubMed] [Google Scholar]
- 18.Ware JE, Kosinski M, Keller SD. SF-12 physical and mental health summary scales. Boston, MA: Health Institute, New England Medical Center, 1995.
- 19.Elashoff JD. nQuery Advisor Version 4.0 User's Guide. Los Angeles, CA, 2000.
- 20.Casey MJ, Garcia-Padial J, Johnson C, Osborne NG, Sotolongo J, Watson P. A critical analysis of laparoscopic assisted vaginal hysterectomies compared with vaginal hysterectomies unassisted by laparoscopy and transabdominal hysterectomies. J Gynaecol Surg 1994;10: 7-14. [DOI] [PubMed] [Google Scholar]
- 21.Maresh MJ, Metcalfe MA, McPherson K, Overton C, Hall V, Hargreaves J, et al. The VALUE national hysterectomy study: description of the patients and their surgery. Br J Obstet Gynaecol 2002;109: 302-12. [DOI] [PubMed] [Google Scholar]
- 22.Farquhar CM, Steiner CA. Hysterectomy rates in the United States 1990-1997. Obstet Gynecol 2002;99: 229-34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.