Abstract
Aim
Early identification of individuals in the prodrome and first episode of psychosis can lead to preemptive intervention and perhaps prevention of the significant functional decline that often accompanies a first psychotic episode. The development of an extensive community outreach and education campaign is essential for programs that aim to identify and treat individuals in the early stages of psychotic illness.
Methods
Over the last decade, the Cognitive Assessment and Risk Evaluation (CARE) Program at the University of California San Diego has implemented a recruitment strategy to increase public awareness about early psychosis and establish community collaboration in San Diego County. Educational materials were distributed to community partners, local media and via the internet. The number and pattern of referrals were then analyzed to inform ongoing recruitment efforts.
Results
Overall, 799 referrals were telephone screened. Of 313 who completed diagnostic interviews, 223 were enrolled including 122 in an “At Risk” state and 101 in an Early Psychotic episode. The majority who met inclusion criteria were referred by outpatient mental health practitioners (46.6%), while 16.1% came from inpatient facilities and 16.1% from internet sites. Other important referral sources were the public schools, community colleges and the National Alliance for the Mentally Ill.
Conclusions
The successful recruitment efforts of the CARE program reflect not only the extensive educational outreach but the emphasis on enhancing professional relationships with community partners. The internet became an important source of information and referrals and will likely be an essential component of any public education campaign.
Keywords: Prodrome, Psychosis, Public Health, Recruitment, “Ultra High Risk”
Introduction
In the past two decades, researchers and clinicians have demonstrated that early intervention and treatment of psychosis can improve functional outcomes, lowering costs for individuals and society 1,2,3. As schizophrenia typically begins during late adolescence and early adulthood, the illness sets in during a period of critical development and maturation, thwarting normal brain processes that sustain cognition and functioning. Beyond an individual’s loss, functional loss occurs at a community level, impairing the person’s potential contribution to society, making schizophrenia among the leading causes of disability in the United States 4 – an analysis in 2002, showed the overall cost to be $62.7 billion, with total indirect costs due to unemployment in excess of $32.4 billion 5. Although the financial cost of proactive strategies such as early identification may appear exorbitant, it is suggested that early identification paired with appropriate intervention and treatment may be cost saving 6.
The premorbid phase of schizophrenia is characterized by social and cognitive deficits, alongside subtle neurological abnormalities which long precede the first episode of psychosis 7. The “at risk”8 (sometimes called “prodromal” 9, “ultra high risk” 10 or “clinical high risk” 11) period is defined by worsening positive and negative symptoms, and a deteriorating course of psychosocial impairment culminating in the onset of frank psychosis 12. While researchers have previously studied changes in the first episode of psychosis, recent studies have examined those at risk for developing schizophrenia with the hope that intervention prior to the onset of psychosis may prevent further decline and morbidity.
Research efforts have demonstrated the success of community outreach and education regarding those at risk for developing schizophrenia and it is now possible to use empirically defined criteria to identify individuals at an increased risk for a psychotic illness 13. Recent research supports this idea indicating that community education may reduce the duration of untreated psychosis (DUP). A Norwegian TIPS (Early Treatment and Intervention in Psychosis) study examined whether specialized community education and a mobile detection program could affect DUP 14. When comparing health service regions in which an early psychosis detection program was introduced to areas without such a program, DUP was reduced to a matter of weeks. Positive clinical differences were maintained at three month, one-year, and two-year follow-ups in the TIPS program 15,16.
Recruitment of prodromal subjects includes many components such as locating potential participants, informing subjects of the risks and benefits of participation, initial evaluations, determining and informing subjects of their “at risk” status, and arranging for longitudinal psychological monitoring17. Unfortunately, recruiting individuals at risk for psychosis is difficult and requires effort, commitment and time. Unlike clinical samples contained within institutions, the “at risk” population is often less accessible and more difficult to immediately recognize 18. In a recent review that included eight sites that are part of the North American Prodromal Longitudinal Studies (NAPLS) consortium studying “at risk” individuals, 20% of participants had no previous contact with mental health services19. Help-seeking individuals tend to be dispersed in different care networks among the mental health system or within primary care settings. Identification of mental health issues is sometimes complicated by legal status (such as immigration status) and stigma that create additional challenges 20. Additionally, many clinicians struggle with large caseloads and limited resources. Requesting their assistance with recruitment often places burdens on those on the front line.
Working with adolescents also requires special effort to ensure voluntary recruitment, and the most frequently reported difficulty is obtaining parental consent 21. Adolescents’ decisions to participate in research are influenced by their parents 22. Therefore, the ability to establish a good relationship with the parents is essential for recruitment. Several previous studies indicated higher levels of engagement and participation by adjusting the interviewing process to meet the needs of the parents and accommodating such requests as interviewing on weekends or in the evenings, obtaining consent in the participants’ homes, and providing childcare during these interviews 20.
The Internet has become an important source of information and referrals to recruitment programs. The use of computers has grown exponentially in the last decade 23 – today, over 70% of American adults use the Internet regularly, and among American youth, 87% use it regularly (over half log on daily) 24. The Internet is increasingly a place for health care advice and interpersonal contacts. Over half of a nationally representative sample of individuals indicated that the Internet had helped them either personally cope with a major illness or helped another individual in their life cope with a major illness 25.
The Personal Assessment and Crisis Evaluation (PACE) Clinic 26 in Melbourne (Australia) has been recruiting “Ultra High Risk” individuals since 1994. The PACE program outlines four strategies for community outreach: 1) providing regular sessions for clinicians at mental health clinics that educate about “at risk” criteria and appropriate treatment options; 2) offering training sessions for non-mental health professionals (general practitioners, substance use counselors, school psychologists, clergy) on screening for symptoms of early psychosis; 3) distribution of educational brochures and posters, and providing website access with information about the prodrome and treatment options; 4) sending regular newsletters to the above targets and to any who have referred patients to the clinic 27,28. Additionally, most clinics for “at risk” individuals have trained staff available to triage calls and to conduct rapid evaluations of potential referrals 17. Further serial assessments by clinic teams determine whether or not the individual is at risk for developing psychosis and appropriate treatment.
The Cognitive Assessment and Risk Evaluation (CARE) Program, at the University of California San Diego, was established by Dr. Kristin Cadenhead in 2000 to study the early phases of psychosisand to identify those at risk for developing psychotic symptoms. The CARE Program provides longitudinal assessment of “at risk” youth on clinical, neuropsychological, information processing, electrophysiological and neuroimaging measures as a means to both better predict risk for psychosis and understand the mechanism by which the neuropathological processes evolve in the early phase of psychosis.
The development of the CARE Program, funded through the National Institute of Mental Health (NIMH), has required recruitment of “at risk” individuals and those who have already experienced their first episode of psychosis. The current manuscript describes the development of an outreach and education program in the county of San Diego, California. Our hope is to identify those recruitment efforts that have been the most successful and economically feasible, demonstrating applicability for community outreach and education in general.
Methods
The goal of the CARE program is to identify individuals at risk for psychosis in order to assess vulnerability markers, help predict risk and identify treatment interventions. In order to achieve this goal, identification and recruitment of participants who are at risk for developing psychosis is crucial; this could not have been achieved without the assistance of community collaboration.
Community collaboration for recruitment was established through a variety of means. Initially, hospitals, pediatricians and family practitioners, public schools, community colleges, universities, National Alliance on Mental Illness (NAMI) and other mental health agencies and mental health practitioners, were contacted by letter, telephone, email and/or fax. Potential recruitment sites were provided with an explanation of the CARE Program, criteria for inclusion, benefits of participation, and contact information. Additionally, these sites were offered the opportunity to have a more comprehensive presentation regarding the above issues and related topics at their site. Many of the sites within the community who work with young people were eager for this type of education. Typical presentations were approximately an hour in length and included information regarding recognition of symptoms associated with psychosis and related features, factors that may increase the risk of schizophrenia, treatment strategies and implications, and local resources for assistance with mental health related issues.
CARE staff also explained to the potential referrers that they would, with the participant’s written consent, be provided with feedback, thus forming a collaborative relationship with the referring party. Depending on the referring party’s preferences, we would offer either a written summary of the clinical consultation and evaluation or a verbal discussion of our impressions. We were clear with potential referrers that our goal was to work together to provide the best treatment for the patient. Because the CARE program is not a treatment program, we were explicit that we were not taking over the care of patients from providers and that we are primarily a research based program. For those individuals who did not have a treating mental health professional, we were able to refer them to the best resource for them depending on their insurance status, resources, age and location within the city. Another component of our program has been case management and the development of a catalogue of referral sources. The development of these collaborative relationships with community resources was essential to not only providing comprehensive treatment for participants, but also for establishing and building a continual source of referrals.
The distribution of educational brochures to gatekeepers, potential participants and their families that stress the importance of early identification and intervention in delaying or preventing the onset of a serious mental illness has also aided in increasing community awareness. The brochures are written in a way that avoids stigmatizing but informs, educates and encourages individuals to seek help if they or a loved one exhibit the warning signs of possible mental illness. We also have a website www.ucsdcareprogram.com that provides useful information about psychosis, mental illness, and the research program, and is linked with a variety of search engines and mental health sites. The CARE website does not contain any type of self-assessment or diagnostic tools. Instead, it encourages the reader to contact CARE directly by telephone or email with any questions or for an initial telephone screening.
Over the past year we have been increasing our outreach activities within the Latino community, a population traditionally underserved by mental health services. We have provided presentations for community clinics within the Latino community and have met with staff from mental health organizations in San Diego that specifically assist the Latino population. CARE is able to offer information, presentations and all components of the evaluation process in Spanish so that we may be fully receptive and respectful to the needs of this community.
Obtaining a referral to CARE is the first step to inclusion in the program. Referred individuals are invited to contact CARE via telephone to learn more about the program and to participate in a brief telephone screening that helps to determine whether they are appropriate for the program. The brief screening reviews referral source, presenting complaints, history of psychiatric treatment, family history, medication history, and history of drug abuse. We also query medical and developmental history. We briefly inquire as to any new changes in their perceptions and thoughts, suspiciousness, problems sleeping, difficulty in functioning, or confused thinking they might have experienced. This screening tool has been effective in identifying individuals who are likely to meet the criteria for inclusion. Individuals who appear to meet eligibility criteria are invited to participate and are scheduled for a diagnostic interview with one of our psychiatrists or psychologists. Individuals who are determined to be ineligible for CARE are referred to the most appropriate resources in the community based on their insurance funding and presenting complaints.
Upon arriving for the interview, potential participants sign informed consent (approved by UCSD IRB 090383) prior to providing demographic information and receiving an interview that reviews prodromal symptoms (Structured Interview for Prodromal Symptoms), Axis I disorders (Structured Clinical Interview for DSM-IV Axis I Disorders), symptoms (Scale for the Assessment of Positive Symptoms/ Scale for the Assessment of Negative Symptoms /Brief Psychiatric Rating Scale) and functioning (Global Assessment of Functioning, Social Adjustment Scale). Those potential participants who are under the age of 18 are asked to sign informed consent along with their parent/guardian prior to further participation. Individuals who meet criteria for one of three prodromal syndromes per the Scale Of Prodromal Symptoms or who have developed a first psychotic episode within the last two years are invited to participate in a battery of neurocognitive, electrophysiological, information processing and neuroimaging measures.
In order to assess the pattern of referrals to inform ongoing recruitment efforts, we compiled the number and sources of referrals for this ten year period as well as various demographic information. Chi Square analyses were used to assess categorical data while t-tests and ANOVA’s were used to assess parametric data.
Results
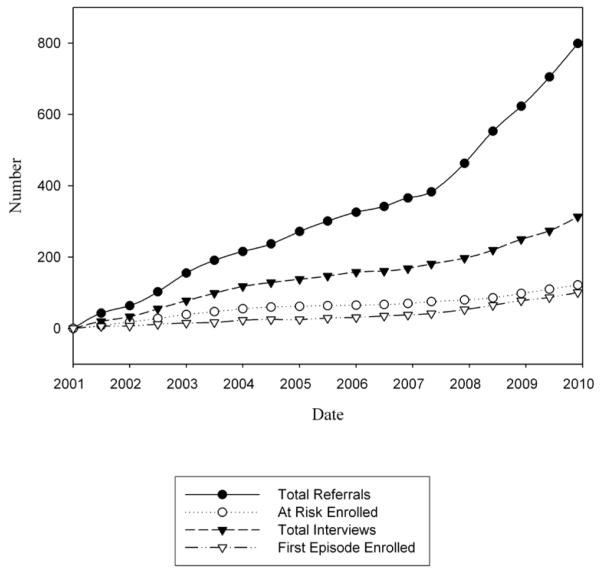
The response to the community outreach and education over the last ten years has been enthusiastic. The CARE Program has received over 799 referrals of potential “at-risk” individuals since 2000 (see Figure 1). In 2009, the average number of new referrals was nearly fifteen per month with many meeting criteria for enrollment.
Figure 1.
Cumulative Recruiment
Number of Referrals
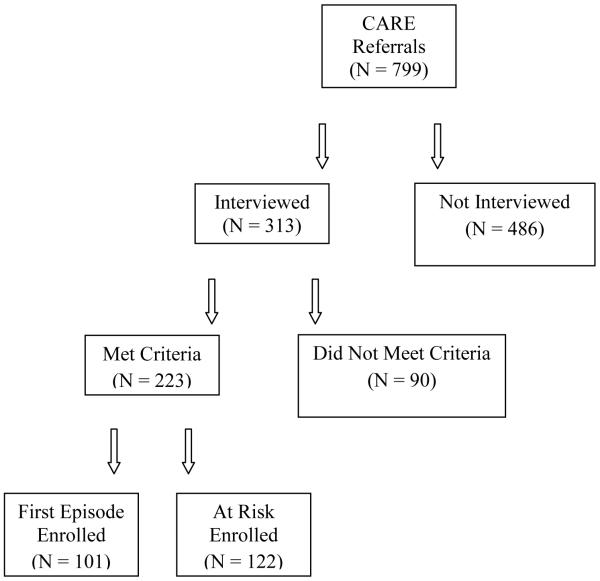
Between the inception of the CARE Program in 2000 and January 1, 2010, 799 referrals have been received from a variety of sources. Following telephone screening by CARE Program staff, 313 individuals were eligible and agreed to further clinical assessment. Of the 313 who participated in a full clinical assessment, 223 were enrolled, with 101 (45%) meeting criteria for the First Psychotic Episode (FE) group and 122 (55%) meeting criteria for the At Risk (AR) group (see Figure 2). Due to the limited scope of this paper, we are presenting findings related only to the referrals that resulted in enrollments in the CARE program. Preliminary investigations demonstrated no differences between the sources or nature of those referrals who were enrolled and those who did not participate in the CARE program.
Figure 2.
Number of Referrals
Sources of Referrals
Outpatient clinicians, a group consisting of outpatient psychiatrists, psychologists, and mental health care practitioners, accounted for the majority of referrals (46.6%) who met criteria for inclusion in the program. Inpatient facilities and the Internet each provided 16.1% of referrals that met CARE Program inclusion criteria. The least successful source of referrals was found through direct advertising (direct mailings, advertisements in newspapers, flyers), bringing in only three participants (see Table 1).
Table 1.
Frequency of Included Participants from Various Referral Sources
| Referral Source | Frequency | Percent |
|---|---|---|
| Outpatient Clinician | 104 | 46.6 |
| Inpatient Facility | 36 | 16.1 |
| Internet | 36 | 16.1 |
| School Counselor/Psychologist | 14 | 6.3 |
| NAMI† | 11 | 4.9 |
| Other Studies | 10 | 4.5 |
| Local College | 9 | 4.0 |
| Advertisements | 3 | 1.3 |
| Total | 223 | 100.0 |
National Alliance on Mental Ilness
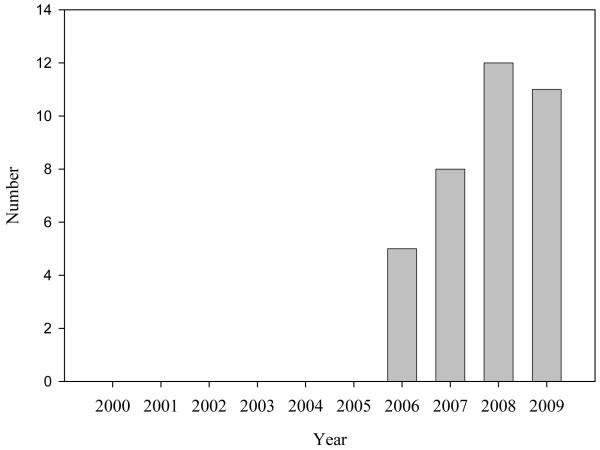
Prior to 2006 there were no referrals through the Internet. Since that time, Internet referralshave increased, with 36 participants entering the program between 2006 and 2009 (see Figure 3). Not surprisingly, we detected a significant difference in terms of enrollment by year for those using the internet as their means of referral (t (1, 35) = 45.16, p <.000. There were no significant differences when this was separated by type of group (AR vs. FE) inclusion (χ 2(3, N = 36) = 2.05, p = .561).
Figure 3.
Enrolled Participants Referred Via Internet By Year
There were no significant differences between those referred from the Internet and those referred from other sources in terms of age (F (1, 221) = 1.97, p=162 ns), gender (χ 2(1, N = 223) = 6.59, p = .417 ns) , ethnicity (χ 2(7, N = 223) = 9.61, p = .212 ns), or type of group inclusion (χ 2(1, N = 223) = 1.83, p = .177 ns). This may be at least partially due to the small sample size within each of these analyses limiting the statistical power.
For those participants included in the program, no significant differences were found between the source of referrals and gender (χ 2(7, N = 223) = 7.95, p = .337 ns). Similarly, no significant differences were found between source of referrals and ethnicity (χ 2(49, N = 223) = 45.43, p = .6.19 ns).
However, a significant difference was found between source of referrals and age of initial evaluation for those included in the research F (7, 215) = 2.25, p=0.032, with school counselors and inpatient settings generating the youngest of the referrals while advertising and NAMI produced the older participants (see Table 2). Of all the included participants, 70% were adults (18 years and older) and 30% were minors.
Table 2.
Referral Source and Age at Initial Evaluation
| Referral Source | N | Mean | Std. Deviation |
|---|---|---|---|
| Outpatient Clinician | 104 | 19.87 | 4.55 |
| Inpatient facility | 36 | 19.00 | 4.41 |
| Internet | 36 | 20.75 | 3.98 |
| School Counselor/Psychologist | 14 | 16.50 | 2.77 |
| NAMI † | 11 | 21.55 | 4.03 |
| Other Studies | 10 | 19.90 | 4.46 |
| Community College | 9 | 20.67 | 1.23 |
| Advertisements | 3 | 23.33 | 6.66 |
| Total | 223 | 19.82 | 4.35 |
National Alliance on Mental Illness
Ethnicity
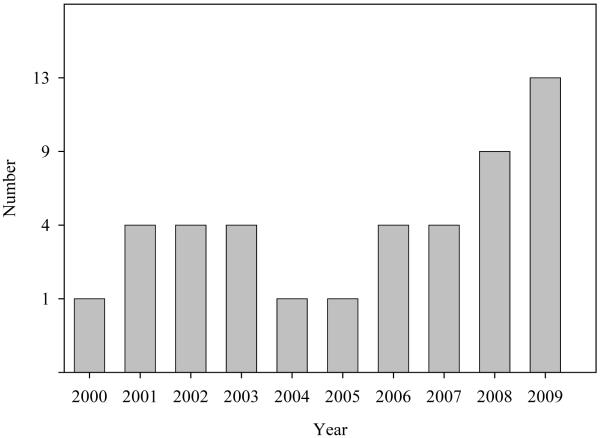
Most of those enrolled in the study were Caucasian (116) with Latino being the second most represented group with 45 participants (see Table 3). The enrollment of Latino participants has increased since the beginning of the CARE program as indicated in Figure 4. Nearly fifty percent of this group was enrolled within the past two years, lending to a significant difference in enrollment of Latinos by year (t (1, 44) = 13.58, p <.000). Similarly to the other variables examined, there was no significant difference in frequency of group inclusion (FE vs. AR) among Latinos (χ 2(1, N = 45) = .56, p = .456ns).
Table 3.
Ethnicity of CARE Program Participants
| Number | CARE Program Percent |
San Diego County Percent |
|
|---|---|---|---|
| Caucasian | 115 | 51.6 | 50.9 |
| Hispanic/ Latino | 45 | 20.2 | 30.9 |
| Asian | 14 | 6.3 | 10.3 |
| African American | 29 | 13.0 | 5.5 |
| Other | 13 | 5.8 | 3.1 |
| American Indian/ Alaska Native | 5 | 2.2 | 1.0 |
| Native Hawaiian/ Pacific | |||
| Islander | 1 | .4 | .5 |
| Unknown | 1 | .4 | n/a |
| Total | 223 | 100.0 | n/a |
Figure 4.
Enrollment of Hispanic Participants
Gender
Nearly twice as many males participated in the CARE Program as females (148 vs. 75) with an even larger ratio of male to female participants in the FE group as in the At Risk group χ 2(1, N = 223) = 6.52, p < .011 (see Table 4).
Table 4.
Gender and Group Inclusion Count
| Group Inclusion | Total | |||
|---|---|---|---|---|
| FE† | At Risk | |||
| Gender | Male | 77 | 71 | 148 |
| Female | 24 | 51 | 75 | |
| Total | 101 | 122 | 223 | |
First Episode of Psychosis
Discussion
Developing a successful recruitment strategy for individuals at risk for major mental illness is challenging, costly and time consuming but essential for early recognition of psychosis. Our efforts in community outreach aim to have an impact on public health, as they address primary prevention goals in terms of providing educational campaigns that may help to identify individuals experiencing early symptoms of psychosis. We also strive to provide secondary and tertiary prevention to those participating in the CARE Program by referring young people to appropriate treatment providers and community organizations.
The recognition of these early changes and prompt intervention is particularly important as in the past decade this “at risk” group has become a reliably identifiable clinical entity with power to predict the onset of schizophrenia within the near future (from weeks to two years) 29. This is significant as the duration of untreated psychosis (DUP) is known to correspond to further functional decline 30.
The majority of referrals to CARE came from gatekeepers in outpatient clinical settings. This may in part be related to the fact that UCSD provides training to many local psychiatrists, psychologists, social workers and marriage and family counselors in the San Diego community. The CARE research program is located at the University of California, San Diego, Medical Center and serves as a training site for psychiatric residents and interns in psychology. Over the last ten years, many of these trainees continue to communicate with us for consultation. Because of the number of referrals we get from local mental health practitioners, we regularly correspond with this group of individuals and invite them to educational programs that we provide on an annual basis. It’s these established relationships between practitioners that allows CARE to be utilized as an asset within the community and to receive frequent referrals from outpatient clinicians.
Over the last few years, the Internet has become another important source for referral to the CARE program. Increasingly, the public goes to the Internet to investigate health concerns and find advice as well as referral information. Based on the data from this study, we plan to continue to increase our presence on the Internet by linking to related websites and posting information that can be helpful to the public. It is clear to the authors that the Internet should be an essential component of any recruitment or public education campaign for detecting early signs of mental illness. However it is also true that the high prevalence of psychotic-like symptoms in the general population31, 32 (median prevalence rate of 5% according to Van os et al. meta-analysis33) may increase the likelihood of getting “false-positive” referrals through this source. As with the CARE Program website, the information posted on the Internet should focus on educational material and avoid self-report questionnaires (which tend to overestimate psychotic symptoms34). While the Internet appears to be a useful tool for obtaining referrals, careful screening interviews by trained clinicians are essential in order to avoid erroneous pathologizing or labeling of healthy individuals.
Based on our results, recruitment efforts will continue to focus on outpatient clinicians and the Internet, but also inpatient facilities, student health facilities, school counselors and local advocacy groups such as the National Alliance for Mental Illness.
The least successful source of referrals was found through direct advertising. This is not surprising given previous literature suggesting that recruitment strategies utilizing direct interaction (telephone contact, interpersonal communication) can be up to 66.5 times more effective than more passive types of recruitment (mass mailings) 35. Unlike the Internet, which requires an active approach to seeking information, direct (passive) advertising, does not. The contrast between these two methods was quite visible in the effectiveness on recruitment. Given the expense of local advertising, this recruitment method may be the least cost effective of our methods.
Detailed phone screenings performed by experienced clinicians are a crucial filter for determining appropriate referrals. The fact that fewer than 30% of the total referrals but 71% of those interviewed actually met criteria for the CARE Program may be reflective of the high frequency of mild transient emotional and behavioral problems in adolescents and young adults, the non-specificity of many psychiatric symptoms and the importance of a telephone screening. This reminds us once more the importance of not labeling, and utilizing a systematic, symptom based approach for assessment.
Enhancing the recruitment efforts in the Latino Community appears to have paid off. Although Latinos are the second most represented ethnic group in CARE Program, the proportion represented in the CARE program is still less than that within the community of San Diego. To achieve an increase in Latino recruitment, it has been crucial to offer information, presentations and all components of the evaluation process in Spanish. Because Latinos are a population traditionally underserved by mental health services, the importance of recruitment in this area cannot be undervalued. Similar efforts in recruitment of other minority ethnic groups (together with the availability of translators for different languages) are future goals of the CARE Program.
The number of referrals received (and their increase over time) likely reflects educational outreach efforts and CARE’s drive to enhance professional relationships with community partners. The CARE Program is somewhat unique in that it offers to collaborate and consult with the treating providers (with participant’s consent). This comprehensive, community-based approach to psychiatric interventions serves to fortify the level of care for participants. In the authors’ opinions, this may be the perfect mix between a research program and a program that cares about the community and works together with their resources in order to achieve better outcomes for the patients.
The ability to identify individuals at risk for psychosis at a very early stage holds considerable promise for understanding the genesis of psychosis and for developing preemptive treatment strategies. Combining “at-risk” criteria with objective biological markers may further improve predictive potential, and thereby open a wider window of opportunity for primary prevention 36, 37, 38. In fact, reliable identification of individuals at greatest risk for psychosis has major public health significance, as it allows early intervention and a first step toward prevention.
While we recognize the limitations of this paper in terms of generalizability (our sample is relatively small and based entirely in Southern California), we hope our experience can be helpful to other investigators conducting similar studies, and also to public health services. We do know that assessment strategies such as the two-stage screening and interview method have been successfully implemented in similar types of research elsewhere. 26 We anticipate that some of our other findings will also have some practical value for those engaging in similar research.
Acknowledgements
Financial Support: This work was supported by the National Institute of Mental Health R01 MH60720 and K24 MH76191 to KSC.
References
- 1.Addington D, McKenzie E, Addington J, Patten S, Smith A, Adair C. Performance Measures for Early Psychosis Treatment Services. Psychiatr Serv Dec. 2005;56:1570–1582. doi: 10.1176/appi.ps.56.12.1570. [DOI] [PubMed] [Google Scholar]
- 2.Hafner H, an der Heiden W. The course of schizophrenia in the light of modern follow-up studies: the ABC and WHO studies. Can J Psychiatry. 1999;42:139–151. doi: 10.1007/pl00014180. [DOI] [PubMed] [Google Scholar]
- 3.Hegarty JD, Baldessarini RJ, Tohen M, Waternaux C, Oepen G. One hundred years of schizophrenia: a meta-analysis of the outcome literature. Am J Psychiatry. 1994 Oct;151:1409–1416. doi: 10.1176/ajp.151.10.1409. [DOI] [PubMed] [Google Scholar]
- 4.Murray CJL, Lopez AD. Evidence-Based Health Policy - Lessons from the Global Burden of Disease Study. Science. 1996;274(5288):740. doi: 10.1126/science.274.5288.740. [DOI] [PubMed] [Google Scholar]
- 5.Wu EQ, Birnbaum HG, Shi L, et al. The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 2005;66(9):1122–1129. doi: 10.4088/jcp.v66n0906. [DOI] [PubMed] [Google Scholar]
- 6.Valmaggia LR, McCrone P, Knapp M, et al. Economic impact of early intervention in people at high risk of psychosis. Psychological Medicine. 2009;39:1617–1626. doi: 10.1017/S0033291709005613. [DOI] [PubMed] [Google Scholar]
- 7.Davidson M, Abraham R, Jonathan R, Weiser M, Kaplan Z, Mark M. Behavioral and intellectual markers for schizophrenia in apparently healthy male adolescents. American Journal of Psychiatry. 1999;156:1328–1335. doi: 10.1176/ajp.156.9.1328. [DOI] [PubMed] [Google Scholar]
- 8.Broome MR, Woolley JB, Johns LC, et al. Outreach and support in south London (OASIS): implementation of a clinical service for prodromal psychosis and the at risk mental state. Eur Psychiatry. 2005 Aug;20(5-6):372–8. doi: 10.1016/j.eurpsy.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Miller TJ, McGlashan TH, Woods SW, et al. Symptom assessment in schizophrenic prodromal states. Psychiatr Q. 1999 winter;70(4):273–87. doi: 10.1023/a:1022034115078. [DOI] [PubMed] [Google Scholar]
- 10.Yung AR, Nelson B, Stanford C. Validation of “prodromal” criteria to detect individuals at ultra high risk of psychosis: 2 year follow-up. Schizophr Res. 2008 Oct;105(1-3):10–7. doi: 10.1016/j.schres.2008.07.012. at al. [DOI] [PubMed] [Google Scholar]
- 11.Lencz T, Smith CW, Auther A, Correll CU, Cornblatt B. Nonspecific and attenuated negative symptoms in patients at clinical high-risk for schizophrenia. Schizophr Res. 2004 May 1;68(1):37–48. doi: 10.1016/S0920-9964(03)00214-7. [DOI] [PubMed] [Google Scholar]
- 12.Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. 1996;22:353–370. doi: 10.1093/schbul/22.2.353. [DOI] [PubMed] [Google Scholar]
- 13.Addington J, Cadenhead KS, Cannon TD, et al. North American Prodrome Longitudinal Study (NAPLS): a collaborative multi-site approach to prodromal. Schizophrenia. Schizophrenia Bulletin. 2007;33:665–672. doi: 10.1093/schbul/sbl075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johannessen Jo, Larsen TK, Joa I, et al. Pathways to care for first-episode psychosis in an early detection healthcare sector: Part of the Scandinavian TIPS study. The British Journal of Psychiatry. 2005 Aug;187:s24–s28. doi: 10.1192/bjp.187.48.s24. [DOI] [PubMed] [Google Scholar]
- 15.Larsen TK, Melle I, Auestad B, et al. Early detection of first-episode psychosis: the effect on 1-year outcome. Schizophr Bull. 2006 Oct;32(4):758–64. doi: 10.1093/schbul/sbl005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McGorry PD, Killackey E, Yung AR. Early intervention in psychotic disorders: detection and treatment of the first episode and the critical early stages. Med J Australia. 2007;187(Suppl. 7):s8–10. doi: 10.5694/j.1326-5377.2007.tb01327.x. [DOI] [PubMed] [Google Scholar]
- 17.McGlashan TH, Addington J, Cannon T, et al. Recruitment and treatment practices for help-seeking “prodromal” patients. Schizophr Bull. 2007 May;33(3):715–26. doi: 10.1093/schbul/sbm025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rodriguez MD, Rodriguez J, Davis M. Recruitment of first-generation Latinos in a rural community: The essential nature of personal contact. Family Process. 2006;45:87–100. doi: 10.1111/j.1545-5300.2006.00082.x. [DOI] [PubMed] [Google Scholar]
- 19.Cadenhead KC, Addington J, Cannon T, et al. Treatment History in the Psychosis Prodrome: Characteristics of the North American Prodrome Longitudinal Study Cohort. Early Interv Psychiatry. 2010 Aug;4(3):220–6. doi: 10.1111/j.1751-7893.2010.00183.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zayas LH, Hausmann-Stabile C, Pilat AM. Recruiting Urban Latina Adolescents and Their Families: Challenges and Lessons Learned in Suicide Attempts Research. Youth Soc. 2009 January;40(4):591–602. doi: 10.1177/0044118X08328590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diviak K, Currt S, Emery S, Mermelstein R. Human participants challenges in youth tobacco cessation research: researcher’s perspectives. Ethics Behavior. 2004;14:321–324. doi: 10.1207/s15327019eb1404_4. [DOI] [PubMed] [Google Scholar]
- 22.Broome M, Richards D. The influence of relationships on children’s and adolescent participation in research. Nursing Research. 2003;52(3):191–197. doi: 10.1097/00006199-200305000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Becker HJ. Who’s wired and who’s not: Children’s access to and use of computer technology. Future of Children. 2000;10:44–75. [PubMed] [Google Scholar]
- 24.Lenhart A, Madden M, Hitlin P. [Retrieved February 1, 2007];Teens and technology: Youth are leading the transition to a fully wired and mobile nation. 2005 July 27; from http://www.pewInternet.org/pdfs/PIP_Teens_Tech_July2005web.pdf.
- 25.Horrigan J, Rainie L. [Retrieved February 22, 2007];The Internet’s growing role in life’s major moments. PEW Internet and American Life Project. 2006 from http://www.pewinternet.org/pdfs/PIP_Major%20Moments_2006.pdf.
- 26.Phillips LJ, Leicester SB, O’Dwyer The PACE Clinic: identification and management of young people at “ultra” high risk of psychosis. J Psychiatr Pract. 2002 Sep;8(5):255–69. doi: 10.1097/00131746-200209000-00002. at al. [DOI] [PubMed] [Google Scholar]
- 27.Yung A, Phillips L, McGorry PD. Treating Schizophrenia in the Prodromal Phase. Taylor & Francis; London, England: 2004. [Google Scholar]
- 28.McGorry PD, Yung AR, Phillips LJ. The “close-in” or ultra high-risk model: a safe and effective strategy for research and clinical intervention in prepsychotic mental disorder. Schizophr Bull. 2003;29:771–790. doi: 10.1093/oxfordjournals.schbul.a007046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McGlashan TH, Addington J, Cannon T, et al. Recruitment and treatment practices for help-seeking “prodromal” patients. Schizophr Bull. 2007 May;33(3):715–26. doi: 10.1093/schbul/sbm025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Melle I, Larsen T, Haahr U, et al. Reducing the duration of untreated first-episode psychosis. Arch Gen Psychiatry. 2004;61:143–150. doi: 10.1001/archpsyc.61.2.143. [DOI] [PubMed] [Google Scholar]
- 31.Kendler KS, Gallagher TJ, Abelson JM, Kessler RC. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:1022–31. doi: 10.1001/archpsyc.1996.01830110060007. [Abstract/Free Full Text]4. [DOI] [PubMed] [Google Scholar]
- 32.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 33.Van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis preneness-persistence-impairment model of psychotic disorder. Psychol med. 2009 Feb;39(2):179–95. doi: 10.1017/S0033291708003814. [DOI] [PubMed] [Google Scholar]
- 34.Compton MT, Kaslow NJ. Self reported psychotic symptoms predict impulsivity among African-American patients in an urban non-psychiatric medical setting. Psychiatry Research. 2005 May;vol 135(1):35–40. doi: 10.1016/j.psychres.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 35.McDonald PW. Population-based recruitment for quit smoking programs: an analytic review of communication variables. Preventive Medicine. 1999;28:545–557. doi: 10.1006/pmed.1998.0479. [DOI] [PubMed] [Google Scholar]
- 36.Cannon TD, Cadenhead KS, Cornblatt B, et al. Prediction of Psychosis in Youth at High Clinical Risk: A Multisite Longitudinal Study in North America. Arch Gen Psychiatry. 2008 Jan;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Haroun N, Dunn L, Haroun A, Cadenhead KS. Risk and Protection in Prodromal Schizophrenia: Ethical Implications for Clinical Practice and Future Research. Schizophr Bull. 2006;32:166–178. doi: 10.1093/schbul/sbj007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McGorry PD, Hickie IB, Yung AR, et al. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Australia and New Zealand Journal of Psychiatry. 2006;40:616–622. doi: 10.1080/j.1440-1614.2006.01860.x. [DOI] [PubMed] [Google Scholar]