Abstract
Although musculoskeletal disorders are the most common reason for general practitioner visits, training did not keep pace. Implementation of learning from patients with rheumatologic disorders linked together with the teaching of theoretical knowledge in the preclinical medical education might be an important step forward in the improvement of quality of care for these patients. The Leiden Medical School curriculum has implemented two non-obligatory real patient learning (RPL) practicals integrated within the preclinical block musculoskeletal disorders. This study investigates the educational effectiveness of the practicals, the expectations students have of RPL, and students’ satisfaction. Participants’ grades on the end-of-block test served as the test results of the educational effectiveness of the practicals and were compared with those of the non-participants. Qualitative data was collected by means of questionnaires generated by focus groups. The participants in practicals scored significantly higher at the end-of-block test. The expected effects of the contact with real patients concerned positive effects on cognition and skills. ‘Contextualizing of the theory’, ‘better memorizing of clinical pictures’, and ‘understanding of the impact of the disease’ were the most frequently mentioned effects of the practicals. Overall, the participants were (very) enthusiastic about this educational format. The RPL practicals integrated within a preclinical block musculoskeletal disorders are a valuable addition to the Leiden medical curriculum. This relatively limited intervention exhibits a strong effect on students’ performance in tests. Future research should be directed towards the long-term effects of this intervention.
Keywords: Focus groups, Medical, Medical education, Musculoskeletal diseases, Patients, Questionnaires, Students, Undergraduate
Introduction
While musculoskeletal (MSK) complaints are the second most common reason for counselling a doctor [1–3], training did not keep pace [4] and in many medical circumstances, MSK complaints are not taken seriously [5]. The appreciation of this problem [6, 7] was reflected in the world wide designation of 2000–2010 as an International Bone and Joint Decade [6, 8] and led to the development of initiatives tackling this problem at several levels of education be it undergraduate curricula [6, 9, 10] or at the general practitioner level [11].
In the past decades, the prospect of the patients with inflammatory joint diseases has changed dramatically [12] while the need to improve the education in MSK diseases is still current. The development of new disease-modifying anti-rheumatic drugs (DMARDs), the successful application of a combination of DMARDs, and, last but not the least, the availability of biologicals mediated this change in treatment strategy. Early start of treatment, however, remains vital [13, 14]. The primary condition for early treatment is (1) early recognition of the inflammatory condition by the general practitioner followed by (2) timely referral to the rheumatologist. It is, thus, important to realize that a lack in training of skills in history taking and physical examination of patients with MSK complaints might have a serious negative effect on the life perspective of patients and action should be taken to ensure optimal quality of care [15, 16]. In addition, in the feeling of many, the clinical education of medical studies has been moving too much away from the bedside [5, 17].
Systematic implementation of learning from real patients with rheumatologic disorders linked together with the teaching of theoretical knowledge in the preclinical medical education might be a step forward in the improvement of quality education in respect to knowledge, skills, and attitude and have positive impact on the quality of care for these patients. Described positive effects of early contacts with real patients are multiple and concern above all the effects on learning processes, skills, and attitudes. Contacts with real patients reportedly ease learning processes by demonstration of practical relevance of theory [18–21] and by making learning more meaningful and more focused [22]. Learning from real patients has been experienced as giving students insight into the ethical dimension of patient care [23, 24] and as help to attain an empathic attitude towards patients [25, 26]. It was reported supportive in strengthening of students’ self-awareness and of feeling more confident when meeting patients but also, last but not the least, in taking diagnostic histories and performing physical examination [23, 24, 27]. Early contact with patients improved students’ motivation and reduced the stress of the transition to the clinical environment [18, 26, 27] and improved their clinical skills [28].
With the exception of the study by Branch [24], there is, however, less decisive evidence concerning positive effect on students’ performance in knowledge assessments. The 2006 best evidence medical education (BEME) systematic review [29] concludes that, although there is some evidence that students who had early experience perform better on summative tests [30], the effect sizes are small and the claims are either based on sketchy data or week study methods [21, 31] and it also reports studies with neutral results [32, 33].
Our study took place in the preclinical block musculoskeletal disorders (MSD) of Leiden Medical School. It comprises small-scale preclinical patient encounters in the form of non-obligatory real patients learning (RPL) practicals which are the subject of this study. These two practicals, which feature patients with (1) back pain (BP) and (2) rheumatoid arthritis (RA), enable students to meet patients in a safe environment. The main goal of the practicals is to demonstrate in practice the theory discussed in the lectures and tutorials, and to make students aware of the impact of a disease on patients’ lives. In addition, students are, within time limits, trained in history taking and physical examination of the musculoskeletal system.
This study investigates the following:
The performance of the participants in the RPL practicals integrated in a preclinical block in knowledge assessment (end-of-block test).
The expectations students have from the real patient learning.
The experienced effects of the practicals and students’ satisfaction.
Methods
Context
The curriculum of Leiden Medical School, the Netherlands, consists of four preclinical and two clinical years. The preclinical semesters consist of 3- to 6-week blocks divided in themes [34] featuring different educational formats, such as formal lectures, small group tutorials, and self-directed learning. Early clinical experience is very rarely included. In years 3 and 4, clinical problems are the starting point of each theme.
This study was conducted in the block on MSD in the final 3 weeks of year 3. In this block, students learn to apply structured clinical reasoning in dealing with problems of the musculoskeletal system. This block implemented two RPL practicals, which are a novelty to the Leiden Medical School curriculum and subject of this study.
Throughout the year 3, none of the educational formats is obligatory. Students who wish to follow one of the small-scale educational formats such as small group tutorial and/or RPL practical must register and are consequently obliged to be present. The end-of-block test takes place the last day of the block. According to the medical school rules, however, students who undertake the block are not obliged to sit the end-of-block test at that particular moment.
Real patient learning practicals
Each of the two RPL practicals are planned after the formal lectures and small group tutorials concerning the subjects illustrated in the practicals. Each practical lasts 90 min and accommodates 15 students and 4 patients, thus assuring individual scale contact.
Due to the local situation, both RPL practicals are organized differently.
Patients who participate in the practical ‘Back pain’ are out-patients of the departments of rheumatology, orthopedic surgery, and/or patients under treatment of the local physical therapists) because of chronic low back pain and/or participants in the local training groups for patients with spondylarthritis. Students are obliged to take the history, perform the physical examination of the spine, decide on the differential diagnosis, and present their case to their peers. The practical is supervised by an experienced physical therapist. A small incentive is provided for the patients.
Patients who participate in the practical ‘Arthritis’ are members of a professional organization of arthritis educators which employs patients with RA in different phases of their disease [35, 36]. These patients are trained to give presentations and to teach medical students and general practitioners how to recognize and examine inflamed joints and teach about the consequences the disease has on their quality of life. The supervision by a senior staff member is limited to achieve optimal contact between students and patients. Patients receive hourly wages.
Recruitment of student participants
Two months prior to the start of the block, a lecture was given to the cohort of students who were going to participate in the MSD block explaining the purpose of the RPL practicals. In addition, an e-mail was sent to all students with the same content as the lecture. From that moment on until 2 weeks before the start of the MSD block, the practicals were open for enrolment.
Although medical ethics committees in Dutch academic medical centers are currently not required to evaluate this type of study, an ethical procedure was agreed on with the academic hospital’s medical ethics advisor. This meant that students were informed that their data (questionnaires and grades) would be anonymized, but not informed about the content of the questionnaires. They were invited to express any disagreement with the procedure and given the assurance that, if they disagreed, their data would be removed from the database. No disagreement was expressed by any of the students.
Students’ characteristics
The data concerning the gender and enrolment behavior in the (non-obligatory) educational modules in other blocks then in the block musculoskeletal disorders were collected by means of a short questionnaire presented to all students participating in the end-of-block test just after the test.
Primary outcome
Educational effectiveness
Students’ grades on the end-of-block test served as the measure of the educational effect of the practicals.
The test consisted of ten multiple choice questions (range 0–10 points) which examined the basic science knowledge and therapeutic problems (such as side effects of drugs) not directly related to low back pain or arthritis. Twenty extended matching questions (range 0–40 points) examined the knowledge of the musculoskeletal signs and symptoms and differential diagnostic considerations (12 out of 20 related either to low back pain or arthritis). To assess the in-depth acquisition of knowledge, one open question concerning arthritis was included to examine the capacity of the students to exercise the analytical problem-solving method taught during the block (range 0–13 points). In addition, the test included also one open question concerning a pharmacological approach to gout treatment (range 0–4 points). Final test score represents a sum of all subscores (range 0–63 points) with about 60% (37/63) of score representing knowledge concerning either arthritis or low back pain.
The final test grade was determined by method of Cohen–Schotanus [37]. It ranges from 0 (worst) to 10 (best), a score of six points or more means passing the exam.
To be able to correct for the potentially confounding volunteer bias, the test grades received by the students in the third year blocks preceding the MSD block (block abdominal problems, pulmonal and cardiac problems, and oncology) were collected from the medical school database (past test grades). These blocks were chosen because the level of difficulty was similar to that of the MSD block. The past tests’ grades range from 0 (worst) to 10 (best).
Secondary outcomes
Focus groups
Students’ opinions concerning their expectation of the early small scale patient contacts, experienced effects, and satisfaction with the practicals were collected by means of two questionnaires, Q1 and Q2. The questionnaires consisted of items generated by focus groups (focus group 1 and 2). Focus group approach has been shown to be effective in eliciting a rich variety of opinions from groups [38] and have been used in investigations similar to ours [20]. The members of the focus group were students who subscribed to practicals and agreed to participate. They were recruited by e-mail send out to all students who subscribed. This procedure resulted in a focus group of six female students (50%) and six male students (50%). The participants in focus group agreed that the results of the interviews will be reported anonymously and they received a small financial compensation for their efforts.
The focus group was scheduled twice before (focus group 1) and twice after the practicals (focus group 2) and lasted 2 h each. It was chaired by a moderator–educationalist (SV) who stimulated the discussion by asking additional questions and encouraged students to participate in the discussion. The focus group members discussed the following topics:
Focus group 1: The expectations from the early patient encounter during the practicals.
Focus group 2: The experienced (subjective) effects and satisfaction with the practicals.
The focus group discussions were taped, transcribed literally, and subsequently analyzed by the researchers as described by Diemers [20]. Summaries were written and sent to the focus group students for their approval and comments. The qualitative data collected in the focus group meetings were analyzed in three phases as described by Miles and Huberman [39]. First, two researchers extracted separately the aspects of early patient contacts that were mentioned by the students. Second, they combined their analysis and decided about the list of aspects of early patient contacts as put forward by the students. Third, the transcript was analyzed by a third researcher in order to control whether the list of aspects of early patient contact was comprehensive. When this turned out to be the case, the aspects were converted into survey questions. They were piloted with two students to check whether the questions were understandable.
Students’ expectations
Q1 contained a list of 13 statements and students were instructed to select three which they regarded as most important.
Experienced effects and satisfaction with the practicals
Q2 consisted of the list of 12 statements concerning the subjective effects of both practicals. Students were asked to give a level of their agreement with each statement on a five-point Likert scale (0 = I strongly disagree, till 5 = I strongly agree). The practical ‘Back pain’ and the practical ‘Arthritis’ were assessed separately. In addition, four statements concerning the general satisfaction with the practicals were included. Again, students were asked to indicate to what extent they agreed with each statement on a five-point Likert scale.
The questionnaires were transcribed into NetQuestionnaire and e-mailed to all participants of the practicals. Q1 was sent 1 week before start of the block (and again the day before the start of the first practical), Q2 shortly after the end-of-block test (with a reminder 1 week later).
Statistical analysis
Data were analyzed using Statistical Package for Social Sciences version 16.0 based on intention-to-treat as initially assigned. The differences between the participants and non-participants were analyzed using Student’s unpaired t test or chi-square test where appropriate. The mean past test grades were calculated only when at least two out of three grades were available and were used in the linear regression analysis to account for potential confounders. P values below 0.05 were considered to be statistically significant. Effect size was calculated according to Cohen [40].
Results
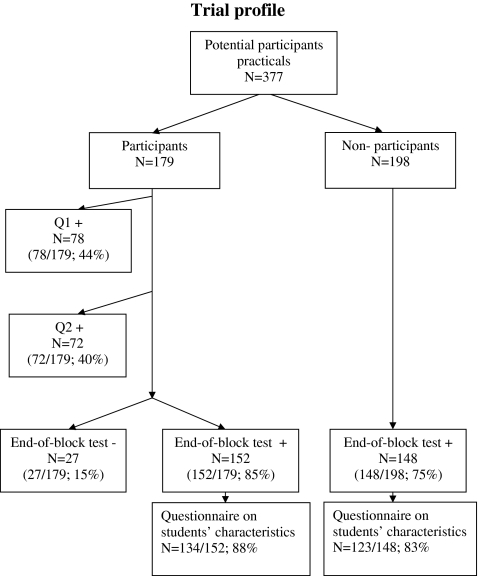
In the academic year 2007–2008, when this study was conducted, 377 students (potential participants) participated in the block musculoskeletal disorders (Fig. 1).
Fig. 1.
Potential participants, cohort of students followed the MSD block. Participants, students who enrolled in real patient learning practicals. Non-participants, students who did not enrol in RPL practicals. Q1, questionnaire introduced to students before the start of RPL practicals. Q2, questionnaire introduced to students after the participation in RPL practicals. End-of-block test+, number of students who sat the end-of-block test. End-of-block test−, number of students who did not sit the end-of-block test
The questionnaire, collecting students’ characteristics and presented to the students who sat the test, was answered by 134 participants (134/152; 88%) and 123 (123/148; 83%) non-participants who sat the test.
The majority of participants and non-participants was female (75% and 67%; P = 0.125, respectively). The participants enrolled more often than the non-participants in the (non-obligatory) educational modules in other blocks (93% and 70.2%, respectively; P = 0.000). One hundred seventy-nine (55%) students enrolled in the practicals.
Primary outcome
Educational effectiveness of the practicals
For the analysis of the educational effectiveness of the practicals, data of all participants (N = 152) and non-participants (N = 148) who set the end-of-block test were used (Fig. 1).
As demonstrated in Table 1, for all test results including the final grade, final test score, and score for open question rheumatology, the participants in practicals scored higher than the non-participants. In addition, the participants scored also higher for the past test grades suggesting that, in general, students who score higher on tests have chosen to enroll the practicals. When, however, the end-of-block test results were corrected for this potential confounder, the pattern did not change.
Table 1.
Educational effectiveness of the practicals
| Outcome | Non-participants mean (SD) | Participants mean (SD) | Regression coefficient (B) unadjusted | P value | Regression coefficient (B) adjusted | P value |
|---|---|---|---|---|---|---|
| End-of-block test takena | 148 | 152 | ||||
| Final test gradeb (0–10) | 6.12 (1.0) | 6.8 (1.0) | 0.655 | 0.000 | 0.286 | 0.019 |
| Final test scorec (0–63) | 45 (9) | 51 (9) | 5.863 | 0.000 | 2.664 | 0.008 |
| Score open question rheumatologyd (0–13) | 3 (2) | 4 (2) | 1.212 | 0.000 | 0.370 | 0.000 |
| Past test gradese (0–10) | 6 (1) | 7 (1) | 0.678 | 0.000 | – | – |
aTest sat by all registered participants in the block musculoskeletal disorders at the last day of the block
bFinal test grade determined by method of Cohen–Schotanus
cSum of all subscores
dScore for the open question rheumatology
eMean of the grades received by the students in the third year blocks preceding the MSD block (block abdominal problems, pulmonal and cardiac problems, oncology)
Effect size amounted, when using final test score and final test grade, to 0.66 and 0.68, respectively. This effect size is considered in the literature to be between medium (0.5) and large (0.8) [40].
Secondary outcomes
Students’ expectations
Q1 was returned by 78 participants (78/179; 44%).
Table 2 demonstrates that the three most important expectations of the practicals were ‘better memorizing of clinical pictures’ (46/78; 58.9%), ‘contextualization of theory’ (42/78; 53.8%), and ‘improvement of physical examination skills’ (42/78; 53.8%). ‘Understanding of the impact of the disease’ was mentioned only by a minority of the students (12/78; 15.4%).
Table 2.
Students’ expectations
| No. of participants who completed Q1a | N = 78 (%) |
|---|---|
| Better memorizing of clinical pictures | 58.9 |
| Contextualizing of theory | 53.8 |
| Improvement of physical examination skills | 53.8 |
| Improvement of application of theoretical knowledge | 28.2 |
| Deepening of the subject material | 19.2 |
| Understanding the impact of disease | 15.4 |
| Improvement of interview skills | 15.4 |
| Development of professional attitude | 14.1 |
| Development of confidence in own medical knowledge | 14.1 |
| Additional motivation to study | 11.5 |
| To obtain a higher end-of-block grade | 10.3 |
| Reflection on own competence | 1.3 |
| No effect | 1.3 |
aQuestionnaire introduced to students before the participation in RPL practicals
Experienced effects
Q2 was completed by 72 participants of the practicals (72/179; 40%).
Tables 3 and 4 show that the most important experienced effects of the practicals, practical ‘Back pain’, and ‘Arthritis’ alike, were: ‘contextualizing of theory’ (93.0% and 97.1%, respectively), ‘better memorizing of clinical pictures’ (91.6% and 95.7%, respectively), ‘understanding of the impact of disease’ (91.6% and 95.7%, respectively), ‘deepening of the subject matter’ (85.9% and 94.2%, respectively) and ‘feedback from the patients’ (77.5% and 73.9%, respectively).
Table 3.
Subjective effects of the practical ‘Back pain’
| No. of students who completed Q2a | Participants (N = 72) (%) | ||
|---|---|---|---|
| Disagree | Neutral | Agree | |
| Contextualizing of theory | 1.4 | 5.6 | 93.0 |
| Better memorizing of clinical pictures | 4.2 | 4.2 | 91.6 |
| Understanding of the impact of disease | 1.4 | 7.0 | 91.6 |
| Deepening of the subject matter | 2.8 | 11.3 | 85.9 |
| Feedback from the patients | 8.5 | 14.1 | 77.5 |
| Improvement of application of theoretical knowledge | 7.0 | 16.9 | 76.1 |
| Additional motivation to study | 7.0 | 29.6 | 63.4 |
| Improvement of physical examination skills | 21.1 | 16.9 | 62.0 |
| Development of confidence in own medical knowledge | 16.9 | 35.2 | 47.9 |
| Development of professional attitude | 5.6 | 45.1 | 49.3 |
| Improvement of interview skills | 23.9 | 26.8 | 49.3 |
| Reflection on own competence | 28.2 | 35.2 | 36.7 |
aQuestionnaire introduced to students after the participation in RPL practicals
Table 4.
Subjective effects of the practical ‘Arthritis’
| No. of students who completed Q2a | Participants (N = 72) (%) | ||
|---|---|---|---|
| Disagree | Neutral | Agree | |
| Contextualizing of theory | 0 | 2.9 | 97.1 |
| Better memorizing of clinical pictures | 0 | 4.3 | 95.7 |
| Understanding of the impact of disease | 0 | 4.3 | 95.7 |
| Deepening of the subject matter | 1.4 | 4.3 | 94.2 |
| Feedback from the patients | 5.8 | 20.3 | 73.9 |
| Improvement in application of theoretical knowledge | 7.2 | 23.2 | 69.6 |
| Additional motivation to study | 7.2 | 21.7 | 71.0 |
| Improvement of physical examination skills | 8.7 | 15.9 | 75.4 |
| Development of confidence in own medical knowledge | 13.0 | 31.9 | 55.1 |
| Development of professional attitude | 8.7 | 56.5 | 34.7 |
| Improvement of interview skills | 39.1 | 39.1 | 21.7 |
| Reflection on own competence | 34.8 | 30.4 | 34.8 |
aQuestionnaire introduced to students after the participation in RPL practicals
The least important experienced effects of the practicals ‘Back pain’ and ‘Arthritis’ were: ‘reflexion on own competence’ (36.7% and 34.8%, respectively), ‘improvement of interview skills’ (49.3% and 21.7%, respectively), and ‘development of professional attitude’ (49.3% and 34.7%, respectively).
Students’ satisfaction
As demonstrated in Table 5, 80.6% of the students were satisfied with the practicals, 79.1% of the students would recommend the practicals to other students, 73.6% preferred more practicals during the curriculum, and 100% of the students would subscribe again for the practicals.
Table 5.
Students’ satisfaction with the practicals
| Number of students who completed Q2a | Participants in practicals (N = 72) | ||
|---|---|---|---|
| Disagree (%) | Neutral (%) | Agree (%) | |
| Questionnaire items | |||
| I would like to have more ‘real patient learning’ in preclinical blocks | 19.4 | 6.9 | 73.6 |
| I recommend the practicals to other students | 16.7 | 4.2 | 79.1 |
| I was satisfied with the practicals | 16.7 | 2.8 | 80.6 |
| Next time, I would again subscribe for the practicals | 0 | 0 | 100 |
aQuestionnaire introduced to students after the participation in RPL practicals
Discussion
This study gives an example of a successful implementation of real patient learning integrated in a preclinical block thus time wise linked with the teaching of theoretical knowledge and reports extensively on its effects. The qualitative data were collected by means of questionnaires based on focus group interviews.
The implementation of real patient learning practicals in teaching of musculoskeletal disorders to undergraduate students resulted in a significantly better performance in the end-of-block test and great satisfaction of the participating students. The students found this small-scale early patient contacts a valuable learning experience.
Our study is one of the few which demonstrate a positive effect of the early contact with real patients on students’ performance in knowledge assessments. The BEME systematic review [29] reports studies using performance in examinations as an outcome measure but concludes that the reviewed data are insufficient to support firmly a positive conclusion. Our results concerning the educational effectiveness are, however, in agreement with data presented by Branch et al. [24] not mentioned in the review. This randomized controlled study was performed as a part of the ‘Introduction to Clinical Medicine’ course and the participants were second year medical students. The students, who were not blinded, were randomized to receive either a video presenting demonstrating techniques and maneuvers used to examine musculoskeletal system or combination of video and instruction provided by trained arthritis educators. Before and after the intervention, the students sat a test and their ability of performing a joint examination was tested. Students who were randomized to participate in the combination video and personal instruction improved significantly more on written examination in which 5 out of 12 questions addressed retention of information concerning arthritis. They also demonstrated a significant greater improvement in confidence to perform musculoskeletal examination and in musculoskeletal examination skills. This well-designed study illustrates that real patient learning can be employed to reach different educational goals depending on the design of the module and its place in the curriculum. In our study, the RPL was placed within a theoretical block thus, supporting the development of clinical reasoning skills which was one of the main goals of that particular block. In the study of Branch, the RPL took place during ‘Introduction to Clinical Medicine’ course teaching basic clinical skills and demonstrates its value in development of musculoskeletal examination skills and increase in confidence in performing musculoskeletal examination.
We hypothesize that the vehicle for the positive effect of the RPL integrated in the theoretical course focusing on the same clinical problems on students’ knowledge might be the result of earlier reported effects of contact with real patients. Others showed that the demonstration of practical relevance of theory eases learning processes [20, 21], strengthens the acquisition and retention of knowledge [18, 19], and stimulates learning.
The most frequently mentioned expectations of the practicals were: ‘better memorizing clinical pictures’, ‘contextualization of theory’, and ‘improvement of physical examination skills’. Students’ expectations of preclinical small scale contact with patients are not often mentioned in the literature. Dornan et al. explored the expectations of undergraduate students and other stakeholders in Manchester medical curriculum (then containing only little early medical experience) of the preclinical encounters [26]. Students expected early contact with real patients to help them in memorizing the clinical pictures by linking it to visual images, by contextualizing the theory, and by putting it into perspective. They expected that the contact with real patients will help them understand the theory rather than memorize it. In addition, students expected to learn skills necessary for clinical practice and to improve their professional attitude. The results of this study are very much consistent with our findings.
The most frequently mentioned experienced effects of the practicals were: ‘contextualizing of theory’, ‘better memorizing of clinical pictures’, ‘understanding of the impact of disease’, and ‘deepening of the subject matter’. Last but not the least; students highly valued the feedback by the patients. Surprisingly, while students’ expectations towards the ‘understanding of the impact of the disease’ were not high (15.4%), a majority of the students mentioned it as an important effect afterwards (91.6% and 95.7%). This outcome illustrates, in our opinion, not so much the disinterest of the students in the impact of the disease on the patient but the lack of experience with RPL in our curriculum. Our findings are in agreement with findings of other investigators [18, 20, 23] and underline the strong effects of contact with real patients even when it is relatively limited in scope as in this study.
There are several limitations to this study.
Firstly, due to the local situation, the study is set up as a non-randomized observational study and is thus subjected to bias such as volunteer bias. This presumption is supported by the finding that past test grades of the participants were higher than those of the non-participants. The fact that participants more often than non-participants stated enrolment in the (non-obligatory) educational modules in earlier blocks point in the same direction. We tried to correct for this potential confounder by presenting the data on primary outcome before and after correction for past test results.
Another source of bias might be the lack of blinding of the study participants. The study participants were, indeed, aware that they were participating in a study and they were not blinded to the intervention. They were, however, unaware of the nature of the questions constituting the questionnaires.
Secondly, due to study design, the participants in practicals enjoyed three more teaching hours than the non-participants. Thus, theoretically, better performance of the participants might be due to the higher number of teaching hours.
Finally, the response rate on the digital (NetQuestionnaire) questionnaires is relatively low. Q1 was completed by 44%, while Q2 by 40% of the participants. Reported response rate of electronic surveys with students varies between 22% and 89% depending on multiple factors such as the recruitment of the survey participants, follow-up contacts, number of reminders, survey length, issue salience, and number of previous surveys received [22, 41, 42]. Increasing number of electronic surveys in our institution might be the cause of low response rate in this study and thus limit the value of results on the secondary outcomes. Clearly, response was much higher when a paper–pencil questionnaire was presented directly after our students finished the end-of-block test (overall response 79%).
In conclusion, this is one of the few studies demonstrating that real patient learning of musculoskeletal disorders does have a positive effect on students’ performance in assessments of knowledge and clinical reasoning. Early introduction of ‘real’ musculoskeletal pathology linked together with the teaching of theoretical knowledge in the preclinical medical education might be an important step towards early recognition of inflammatory diseases, early treatment, and better prognosis of the patients. Future research should be directed towards its effects on competences such as clinical skills, professional attitudes, and long-term effects of this intervention.
Acknowledgments
Disclosures
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Reference
- 1.Rasker JJ. Rheumatology in general practice. Br J Rheumatol. 1995;34:494–497. doi: 10.1093/rheumatology/34.6.494. [DOI] [PubMed] [Google Scholar]
- 2.Badley EM, Rasooly I, Webster GK. Relative importance of musculoskeletal disorders as a cause of chronic health problems, disability, and health care utilization: findings from the 1990 Ontario Health Survey. J Rheumatol. 1994;21:505–514. [PubMed] [Google Scholar]
- 3.Dequeker J, Rasker H. High prevalence and impact of rheumatic diseases is not reflected in the medical curriculum: the ILAR Undergraduate Medical Education in Rheumatology (UMER) 2000 project. Together everybody achieves more. International League of Associations for Rheumatology. J Rheumatol. 1998;25:1037–1040. [PubMed] [Google Scholar]
- 4.Woolfe AD. Undergraduate medical education in rheumatology–aims. J Rheumatol Suppl. 1999;55:29–30. [PubMed] [Google Scholar]
- 5.Dequeker J. Undergraduate education in rheumatology: challenges for the millennium. J Rheumatol Suppl. 1999;55:3–5. [PubMed] [Google Scholar]
- 6.Woolf AD. Undergraduate medical education in rheumatology in Europe. J Rheumatol Suppl. 1999;55:6–8. [PubMed] [Google Scholar]
- 7.Jacobs JC, Rasker JJ, van den Hoogen FH, et al. Education of rheumatic disorders at Dutch medical schools. J Rheumatol Suppl. 1999;55:14–16. [PubMed] [Google Scholar]
- 8.Hazes JM, Woolf AD. The bone and joint decade 2000-2010. J Rheumatol. 2000;27:1–3. [PubMed] [Google Scholar]
- 9.Wadey V, Tang E, Abelseth G. Canadian multidisciplinary core curriculum for musculoskeletal health. J Rheumatol. 2007;34:567–580. [PubMed] [Google Scholar]
- 10.Williams SC, Gulihar A, Dias JJ, et al. A new musculoskeletal curriculum: has it made a difference? J Bone Joint Surg Br. 2010;92:7–11. doi: 10.1302/0301-620X.92B1.23136. [DOI] [PubMed] [Google Scholar]
- 11.Petrella RJ, Davis P. Improving management of musculoskeletal disorders in primary care: the Joint Adventures Program. Clin Rheumatol. 2007;26:1061–1066. doi: 10.1007/s10067-006-0446-4. [DOI] [PubMed] [Google Scholar]
- 12.Pincus T, Sokka T, Kautiainen H. Patients seen for standard rheumatoid arthritis care have significantly better articular, radiographic, laboratory, and functional status in 2000 than in 1985. Arthritis Rheum. 2005;52:1009–1019. doi: 10.1002/art.20941. [DOI] [PubMed] [Google Scholar]
- 13.Lard LR, Visser H, Speyer I, et al. Early versus delayed treatment in patients with recent-onset rheumatoid arthritis: comparison of two cohorts who received different treatment strategies. Am J Med. 2001;111:446–451. doi: 10.1016/S0002-9343(01)00872-5. [DOI] [PubMed] [Google Scholar]
- 14.Van der Heijde D, Maksymowych W. Spondyloarthritis: state of the art and future perspectives. Ann Rheum Dis. 2010;69:949–954. doi: 10.1136/ard.2009.119529. [DOI] [PubMed] [Google Scholar]
- 15.Rasker JJ. Report and review on the achievements and future plans of the ILAR Standing Committee for Health Professionals. Clin Rheumatol. 2005;24:96–98. doi: 10.1007/s10067-004-1019-z. [DOI] [PubMed] [Google Scholar]
- 16.Woolf AD, Akesson K. Education in musculoskeletal health—how can it be improved to meet growing needs? J Rheumatol. 2007;34:455–457. [PubMed] [Google Scholar]
- 17.Rasker JJ. Attitude education in rheumatology. J Rheumatol Suppl. 1999;55:41–42. [PubMed] [Google Scholar]
- 18.Prince KJ. A qualitative analysis of the transition from theory to practice in undergraduate training in a PBL-Medical School. Adv Health Sci Educ. 2000;5:105–116. doi: 10.1023/A:1009873003677. [DOI] [PubMed] [Google Scholar]
- 19.Seabrook M. Clinical students' initial reports of the educational climate in a single medical school. Med Educ. 2004;38:659–669. doi: 10.1111/j.1365-2929.2004.01823.x. [DOI] [PubMed] [Google Scholar]
- 20.Diemers AD. Students' opinions about the effects of preclinical patient contacts on their learning. Adv Health Sci Educ. 2008;13:633–647. doi: 10.1007/s10459-007-9070-6. [DOI] [PubMed] [Google Scholar]
- 21.Rooks L. A primary care preceptorship for first-year medical students coordinated by an Area Health Education Center program: a six-year review. Acad Med. 2001;76:489–492. doi: 10.1097/00001888-200105000-00024. [DOI] [PubMed] [Google Scholar]
- 22.Bell K, Boshuizen HP, Scherpbier A, et al. When only the real thing will do: junior medical students' learning from real patients. Med Educ. 2009;43:1036–1043. doi: 10.1111/j.1365-2923.2009.03508.x. [DOI] [PubMed] [Google Scholar]
- 23.Littlewood S, Ypinazar V, Margolis SA, et al. Early practical experience and the social responsiveness of clinical education: systematic review. BMJ British medical journal (Clinical research ed ) 2005;331:387–391. doi: 10.1136/bmj.331.7513.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Branch VK, Lipsky PE. Positive impact of an intervention by arthritis educators on retention of information, confidence, and examination skills of medical students. Arthritis Care Res. 1998;11:32–38. doi: 10.1002/art.1790110106. [DOI] [PubMed] [Google Scholar]
- 25.Wykurz G, Kelly D. Developing the role of patients as teachers: literature review. BMJ. 2002;325:818–821. doi: 10.1136/bmj.325.7368.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dornan T. What can experience add to early medical education? Consensus survey. BMJ Br medical journal. 2004;329:834. doi: 10.1136/bmj.329.7470.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ottenheijm RPG. Early student-patient contacts in general practice: an approach based on educational principles. Med Teach. 2008;30:802–808. doi: 10.1080/01421590802047265. [DOI] [PubMed] [Google Scholar]
- 28.Haq I. The use of patient partners with back pain to teach undergraduate medical students. Rheumatology. 2006;45:430–434. doi: 10.1093/rheumatology/kei167. [DOI] [PubMed] [Google Scholar]
- 29.Dornan T, Littlewood S, Margolis SA, et al. How can experience in clinical and community settings contribute to early medical education? A BEME systematic review. Med Teach. 2006;28:3–18. doi: 10.1080/01421590500410971. [DOI] [PubMed] [Google Scholar]
- 30.Elnicki DM. Educational and career outcomes of an internal medicine preceptorship for first-year medical students. J Gen Intern Med. 1999;14:341–346. doi: 10.1046/j.1525-1497.1999.00352.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barley G. What did we learn about the impact on students' clinical education? Acad Med. 2001;76:S68–S71. doi: 10.1097/00001888-200104001-00013. [DOI] [PubMed] [Google Scholar]
- 32.Rogers JC, Swee DE, Ullian JA. Teaching medical decision making and students' clinical problem solving skills. Med Teach. 1991;13:157–164. doi: 10.3109/01421599109029025. [DOI] [PubMed] [Google Scholar]
- 33.Satran L, Harris IB, Allen S, et al. Hospital-based versus community-based clinical education: comparing performances and course evaluations by students in their second-year pediatrics rotation. Acad Med. 1993;68:380–382. doi: 10.1097/00001888-199305000-00024. [DOI] [PubMed] [Google Scholar]
- 34.Mandin H, Harasym P, Eagle C, et al. Developing a "clinical presentation" curriculum at the University of Calgary. Acad Med. 1995;70:186–193. doi: 10.1097/00001888-199503000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Smith MD, Henry-Edwards S, Shanahan EM, et al. Evaluation of patient partners in the teaching of the musculoskeletal examination. J Rheumatol. 2000;27:1533–1537. [PubMed] [Google Scholar]
- 36.Oswald AE, Bell MJ, Snell L, et al. The current state of musculoskeletal clinical skills teaching for preclerkship medical students. J Rheumatol. 2008;35:2419–2426. doi: 10.3899/jrheum.080308. [DOI] [PubMed] [Google Scholar]
- 37.JANKE Cohen-Schotanus Student assessment and examination rules. Med Teach. 1999;21:318–321. doi: 10.1080/01421599979626. [DOI] [Google Scholar]
- 38.Barbour RS. Making sense of focus groups. Med Educ. 2005;39:742–750. doi: 10.1111/j.1365-2929.2005.02200.x. [DOI] [PubMed] [Google Scholar]
- 39.Miles MB, Huberman AM. Qualitative data analysis. Thousand Oaks: SAGE; 1994. [Google Scholar]
- 40.Cohen J. A power primer. Psychol Bull. 1994;112:155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 41.Koch J, Andrew S, Salamonson Y, et al. Nursing students' perception of a web-based intervention to support learning. Nurse Educ Today. 2010;30(6):584–90. doi: 10.1016/j.nedt.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 42.Von Below B, Hellquist G, Rodjer S, et al. Medical students' and facilitators' experiences of an Early Professional Contact course: active and motivated students, strained facilitators. BMC Med Educ. 2008;8:56. doi: 10.1186/1472-6920-8-56. [DOI] [PMC free article] [PubMed] [Google Scholar]