Abstract
Introduction
Self poisoning with paraquat has a case fatality ratio (CFR) over 65% in Sri Lanka. Plasma paraquat concentration is the best prognostic indicator for patient outcome but is not readily available. Alternative surrogate clinical markers could be useful in management and determining prognosis.
Anecdotal reports by medical and research staff suggested that patients who complained of burning sensation of the body had a poor prognosis and a prospective study was initiated.
Methods
This was a prospective observational study in 3 hospitals in Sri Lanka. We collected demographic data, presence or absence of burning sensation and major outcome and determined plasma paraquat concentration within 24 hours post ingestion.
Results
There were 179 patients with deliberate self ingestion of paraquat over 30 months.
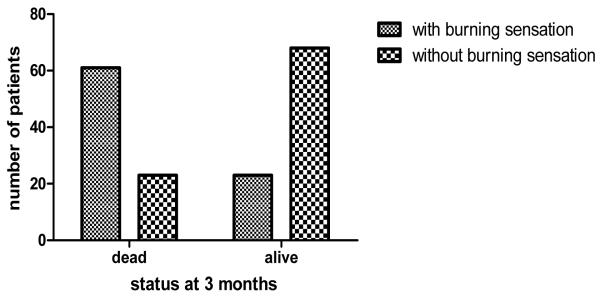
Burning sensation was reported in 84 patients (48%) which initiated at a median of 1 day (range 1-3 days) post ingestion. Of the patients who had burning, 61 died (case fatality rate72.62%; 95% CI 62-81). Of the 91 patients who had no peripheral burning, 23 died (CFR 25.27%, 95% CI 18.15-35.9).figure 1.
Presence of peripheral burning sensation was associated with a significantly higher risk of death (Odds Ratio: 7.8, 95% CI: 3.9-15, p <0.0001). Patients who complained of peripheral burning died at a median of 36 hours (IQR 30.5-88) following ingestion while those who had no peripheral burning died at a median of 50.5 hours (IQR 16.75-80). The difference was not significant (p>0.05). Median admission plasma paraquat concentration in patients with peripheral burning (2.67 μg/mL, 95% CI 0.84-14.2) was significantly higher than in the patients with no peripheral burning (0.022 μg/mL, 95% CI 0.005-0.78; p<0.001).
Peripheral burning has a sensitivity of 0.72 (95% CI: 0.6-8) and specificity of 0.74 (95% CI: 0.64-.08) and a positive predictive value of 0.73 (95% CI: 0.6-.8).
Discussion
It is possible that this symptom may help discriminate between patients who have poor chance of survival and those who may potentially benefit from interventions. The mechanism is not clear but could include either a direct concentration related effect or be a marker of oxidative stress.
Conclusion
Presence of burning sensation is associated with high plasma paraquat concentrations and is strongly predictive of death.
Introduction
Self-poisoning with pesticides is a major public health problem across the Asia Pacific Region1. It is estimated that globally 250,000-370,000 people die from pesticide poisoning each year2. Sri Lanka has a major problem with intentional self-poisoning with high total and youth suicide rates3. Self poisoning is the 4th leading cause of death in some regions of Sri Lanka4. Overall, self poisoning in Asia has a relatively high case fatality ratio (10-20%)5 while paraquat self poisoning has the highest individual case fatality ratio (approximately 65%) for any given poison in Sri Lanka6.
The best prognostic marker that has been shown to predict mortality to date is the plasma paraquat concentration with acceptable sensitivity and specificity7-9. Measurement of plasma paraquat concentration is not available in Sri Lankan hospitals.
While conducting two research studies on paraquat toxicity (prospective observational study and a randomized controlled clinical of immunosuppression) in Sri Lanka, medical and research staff noted that patients who complained of burning sensation of the skin of trunk and limbs (described as if their skin was on fire) seemed more likely to die. This symptom was not previously described and was distinctly different from the epigastric burning sensation commonly experienced by patients who have ingested paraquat. The symptom was termed ‘peripheral burning pain’ to differentiate it from the burning epigastric pain. The objectives of the study were to examine the predictive value of peripheral burning pain for death following self ingestion of paraquat and to examine its correlation with admission plasma paraquat concentration.
Methods
Ethical approval for both studies (observational study and the randomized controlled clinical trial) was obtained from the Ethics Review Committees of Sri Lanka Medical Association; Faculties of Medicine of Peradeniya and Ruhuna and Australian National University. All paraquat self poisoning patients who presented to three study hospitals in Sri Lanka from January 2006 to July 2008 and were able to give a history were asked for the presence or absence of peripheral burning sensation on a twice daily basis by medically qualified (doctors) research assistants. A plasma sample was taken soon after admission. Samples were stored frozen and sent to Syngenta CTL (Alderley Park, Macclesfield, Cheshire, UK) for determination of paraquat ion concentration using High Performance Liquid Chromatography (HPLC), Liquid Chromatography Mass Spectrophotometry (LC–MS–MS )and LC fluorescence10. Patients were followed up until death or discharge. Patients discharged from hospital were visited at their homes after 3 months and outcome recorded. All out of hospital deaths were confirmed by examination of the death certificate issued by the registrar of deaths.
Data were entered into an excel worksheet and analyzed using Stata (version 10.1, Stata Corp. 2001. Statistical Software: Release 7.0. College Station, TX: Stata) and Graph Pad Prism (version 4.03 for Windows, GraphPad Software, San Diego CA USA). Parametric data were analyzed using unpaired t test while non parametric data were compared using Chi square and Mann-Whitney Test.
Results: (table 1)
Table1.
Demography and outcome
| Group with peripheral burning N=84 (males: 66 (78.6%)) |
Group with no peripheral burning N=91 (males: 68 (74.7%) |
Significance | |
|---|---|---|---|
| Age (years) (range) | 28.5 (21-37) | 26(21-38) | Not Significant |
| Admission plasma paraquat concentration, median and IQR (ug/mL) |
2.7 (0.81-13) N=48 |
0.02 (0.005-0.78) N=49 |
Significant (p<0.001) |
| Number of deaths | 61 | 23 | |
| Case fatality rate | 72.6% (95% CI 62- 81) |
25.27% (95% CI 18.15-35.9) |
Significant (p<0.05) |
| Time to death and IQR(hours) |
39.2 (30.5-93.6) | 50 (9-81) | Not Significant |
There were 179 patients with deliberate self ingestion of paraquat from January 2006 to June 2008. 4 patients were excluded as they were too unwell to respond to verbal commands. There were 84 deaths giving an overall case fatality rate of 48%. 5 different commercial preparations containing 200g/L were used for self ingestion (X press®, One shot®, Gramoxone®, Gramoxone Inteon® (containing additionally a purgative and an alginate that forms a gel on contact with stomach acid) and Baur’s paraquat®) by the patients.
Peripheral burning sensation was observed in 84 patients (48%) which initiated at a median of 1 day (range 1-3 days) post ingestion. Of the patients who had burning, 61 died (case fatality rate 72.62%; 95% CI 62-81). Of the 91 patients who had no peripheral burning, 23 died (CFR 25.27%, 95% CI 18.15-35.9). (Figure 1).
Figure1.
Outcome of patients with burning and without burning sensation
Presence of peripheral burning sensation was associated with a significantly higher risk of death (Odds Ratio: 7.8, 95% CI: 3.9-15, p <0.0001). Patients who complained of peripheral burning died at a median of 36 hours (IQR 30.5- 88) following ingestion while those who had no peripheral burning died at a median of 50.5 hours (IQR 16.75-80). The difference was not significant (p>0.05).
Peripheral burning has a sensitivity of 0.72 (95% CI: 0.6-8) and specificity of 0.74 (95% CI: 0.64-0.83) and a positive predictive value of 0.73 (95% CI: 0.6-0.8) in predicting death following self poisoning with paraquat.
Admission plasma paraquat concentration was available in 49 patients who had no peripheral burning sensation and in 48 patients who had peripheral burning sensation. Median admission plasma sampling time was 8.3 (IQR 4.21-13.25) hours. Median admission plasma paraquat concentration in patients with peripheral burning (2.67 μg/mL, 95% CI 0.84-14.2) was significantly higher than in the patients with no peripheral burning (0.022 μg/mL, 95% CI 0.005-0.78; p<0.001).
There was no significant difference (p>0.05) in admission plasma paraquat concentrations and time to death in the deceased patients in the two groups.
Discussion
The mechanism of this symptom is not clear. It is possible that the peripheral burning sensation is due to a primary effect of paraquat on peripheral nociceptive nerve fibres or as a result of paraquat induced oxidative stress which causes lipid peroxidation, mitochondrial toxicity, activation of Nuclear Factor kappa B (NF Kb) and cell death11-14. One of the causes of nociceptive pain is tissue inflammation. Generation of free radicals induce inflammation of tissues, including skin, which may stimulate nociceptors. Further studies to correlate this symptom with quantification of oxidative stress generated should be carried out.
Peripheral burning sensation has a clinically useful sensitivity as a bedside marker of prognosis following paraquat self ingestion in resource poor settings. This may be clinically useful particularly in settings where laboratory based prognostic markers are not readily available and could potentially assist in discriminating between patients who have no chance of survival and those who may potentially benefit from interventions in clinical trials using investigational antidotes such as immunosuppression with dexamethazone, cyclophosphamide and methylprednisolone. A bedside prognostic marker could improve stratification of patients in clinical trials and reduce the potential bias of post-hoc stratification.
Our study excluded a small (n= 4) group of patients who were unable to give a history on admission. We did not attempt to grade the severity of the symptom by examining pain scores or the extent of symptoms. Further studies should examine whether there is possible grading of severity of peripheral burning which may be clinically useful. A severity score should be designed and its correlation with biochemical changes such as liver and renal impairment, severity of oxidative stress and magnitude of hypoxia should be studied. Another limitation is that the researchers were not blinded to the study hypothesis which should be addressed in a future study. However, plasma paraquat concentrations were significantly higher in the group with peripheral burning which implies that this bias may have been minimal.
Conclusion
Presence of burning sensation is associated with high plasma paraquat concentrations and is strongly predictive of death. The cause of this new symptom is unknown and warrants further study.
Acknowledgments
The support given by Physicians, medical officers, research assistants of SACTRC and nurses of the 3 hospitals is acknowledged. The South Asian Clinical Toxicology Research Collaboration is funded by the Wellcome Trust/National Health and Medical Research Council International Collaborative Research Grant 071669MA. IG is funded by the Australian Leadership award-2008. We also wish to thank Syngenta for performing plasma paraquat assays.
References
- 1.Eddleston M, Phillips MR. Self poisoning with pesticides. BMJ. 2004 Jan 3;328(7430):42–4. doi: 10.1136/bmj.328.7430.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal pesticide self-poisoning: systematic review. BMC Public Health. 2007;7:357. doi: 10.1186/1471-2458-7-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organisation . Annex Table 2: death by cause, sex and mortality stratum in WHO Regions, estimated for 2001. World Health Organisation; Geneva, Switzerland: World Health Report 2002. [Google Scholar]
- 4.Department Of Health Services . Annual Health Bulletin 2004/05. State Printing Cooperation; Colombo, Sri Lanka: 2005. [Google Scholar]
- 5.Eddleston M. Patterns and problems of deliberate self-poisoning in the developing world. QJM. 2000 Nov;93(11):715–31. doi: 10.1093/qjmed/93.11.715. [DOI] [PubMed] [Google Scholar]
- 6.Wilks MF, Fernando R, Ariyananda PL, Eddleston M, Berry DJ, Tomenson JA, et al. Improvement in survival after paraquat ingestion following introduction of a new formulation in Sri Lanka. PLoS Med. 2008 Feb;5(2):e49. doi: 10.1371/journal.pmed.0050049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones AL, Elton R, Flanagan R. Multiple logistic regression analysis of plasma paraquat concentrations as a predictor of outcome in 375 cases of paraquat poisoning. QJM. 1999 Oct;92(10):573–8. doi: 10.1093/qjmed/92.10.573. [DOI] [PubMed] [Google Scholar]
- 8.Proudfoot AT, Stewart MS, Levitt T, Widdop B. Paraquat poisoning: significance of plasma-paraquat concentrations. Lancet. 1979 Aug 18;2(8138):330–2. doi: 10.1016/s0140-6736(79)90345-3. [DOI] [PubMed] [Google Scholar]
- 9.Senarathna L, Eddleston M, Wilks MF, Woollen BH, Tomenson JA, Roberts DM, et al. Prediction of outcome after paraquat poisoning by measurement of the plasma paraquat concentration. QJM. 2009 Apr;102(4):251–9. doi: 10.1093/qjmed/hcp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blake DK, Gallegher RT, Woollen BH. Improved methods for the analysis of paraquat in biological fluids. Chromatographia. 2002;55(Suppl):S183–S5. [Google Scholar]
- 11.Bus JS, Gibson JE. Paraquat: Model for oxidant-initiated toxicity. Environ Health Perspect. 1984;55:37–46. doi: 10.1289/ehp.845537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yasaka T, Ohya I, Matsumoto J, Shiramizu T, Sasaguri Y. Acceleration of lipid peroxidation in human paraquat poisoning. Arch Intern Med. 1981;141(9):1169–71. [PubMed] [Google Scholar]
- 13.Yamada K, Fukushima T. Mechanism of cytotoxicity of paraquat. II. Organ specificity of paraquat-stimulated lipid peroxidation in the inner membrane of mitochondria. Exp Toxicol Pathol. 1993;45(5–6):375–80. doi: 10.1016/S0940-2993(11)80433-1. [DOI] [PubMed] [Google Scholar]
- 14.Kratsovnik E, Bromberg Y, Sperling O, Zoref-Shani E. Oxidative stress activates transcription factor NF-κB-mediated protective signaling in primary rat neuronal cultures. J Mol Neurosci. 2005;26(1):27–32. doi: 10.1385/jmn:26:1:027. [DOI] [PubMed] [Google Scholar]