Abstract
Objective To determine whether asthma specialist nurses, using a liaison model of care, reduce unscheduled care in a deprived multiethnic area.
Design Cluster randomised controlled trial.
Setting 44 general practices in two boroughs in east London.
Participants 324 people aged 4-60 years admitted to or attending hospital or the general practitioner out of hours service with acute asthma; 164 (50%) were South Asian patients, 108 (34%) were white patients, and 52 (16%) were from other, largely African and Afro-Caribbean, ethnicities.
Intervention Patient review in a nurse led clinic and liaison with general practitioners and practice nurses comprising educational outreach, promotion of guidelines for high risk asthma, and ongoing clinical support. Control practices received a visit promoting standard asthma guidelines; control patients were checked for inhaler technique.
Main outcome measures Percentage of participants receiving unscheduled care for acute asthma over one year and time to first unscheduled attendance.
Results Primary outcome data were available for 319 of 324 (98%) participants. Intervention delayed time to first attendance with acute asthma (hazard ratio 0.73, 95% confidence interval 0.54 to 1.00; median 194 days for intervention and 126 days for control) and reduced the percentage of participants attending with acute asthma (58% (101/174) v 68% (99/145); odds ratio 0.62, 0.38 to 1.01). In analyses of prespecified subgroups the difference in effect on ethnic groups was not significant, but results were consistent with greater benefit for white patients than for South Asian patients or those from other ethnic groups.
Conclusion Asthma specialist nurses using a liaison model of care reduced unscheduled care for asthma in a deprived multiethnic health district. Ethnic groups may not benefit equally from specialist nurse intervention.
Introduction
The numbers and roles of specialist nurses are increasing, but uncertainty remains about their effects on the costs and use of health care.1 Two types of intervention involving asthma specialist nurses have been evaluated: educating patients after hospital attendance with acute asthma and outreach to educate and support general practitioners and practice nurses. Evaluations show inconsistent benefits on unscheduled care for the first,2-6 and no benefit for the second.7
We tested a liaison model of specialist nursing, which combined the education of patients after discharge with educational outreach and clinical support for primary care clinicians. This model may be particularly appropriate in deprived areas, where general practices vary in their capacity to manage chronic illness.8
Improving asthma outcomes for ethnic minority groups remains a global challenge. Morbidity due to asthma is higher for minority or disadvantaged groups.9,10 In the United Kingdom, hospital admission rates for South Asian patients have been double those of white patients and high for black patients.11,12 South Asian patients may benefit less from asthma education than white patients and have poorer access to care during attacks.13,14 Although evaluations of asthma specialist nurses have been in socioeconomically deprived areas, none has included large populations of ethnic minority groups.2,5 Whether asthma specialist nurses can reduce morbidity in multiethnic inner city populations is unknown.
Two important questions remain for specialist nurses, particularly those dealing with asthma. Can they reduce health service use, and can they improve outcomes equally across ethnic groups? We tested the effectiveness of asthma specialist nurses using a liaison model of care across a single health district comprising one of the most ethnically diverse and deprived areas in the United Kingdom. We focused on patients attending hospital with acute asthma, because they have the highest morbidity and health service use and costs. We compared this intervention group with practices receiving outreach visits promoting standard asthma guidelines, since this itself modestly improves care.15 We used a pragmatic cluster randomised controlled design, as an important element of the intervention addressed clinicians in general practice. We hypothesised that asthma specialist nurses would reduce unscheduled care for asthma.
Methods
We invited to participate in our study all 42 general practices in the London borough of Tower Hamlets and additionally two practices in the neighbouring borough of Newham, which served large Bangladeshi populations using the Royal London Hospital, where the specialist nurses were based. All 44 practices consented to take part. We randomised practices to intervention and control groups using a minimisation programme,16 stratifying by partnership size, training practice status, hospital admission rate for asthma, employment of practice nurse, and whether the practice nurse was trained in asthma care (table 1).
Table 1.
Stratified randomisation and characteristics of 44 participating general practices allocated to nurse led intervention for acute asthma or standard guidelines for asthma
| Characteristic | Intervention practices (n=22) | Control practices (n=22) |
|---|---|---|
| Partnership size: | ||
| Singlehanded | 9 | 9 |
| 2 partners | 5 | 5 |
| ≥3 partners | 8 | 8 |
| Practice nurse employed | 17 | 17 |
| Practice nurse trained in asthma care | 6 | 9 |
| Approved for general practitioner training | 4 | 5 |
| Hospital admission rate for asthma*: | ||
| Low | 7 | 6 |
| Medium | 6 | 7 |
| High | 8 | 8 |
| Member of out of hours cooperative | 11 | 10 |
Lower, middle, and upper tertiles of practices' mean hospital admission rates for asthma for previous two years.
Patients were eligible for inclusion if they had asthma diagnosed by a doctor, were aged 4-60 years, and had been admitted to or attended the accident and emergency department at the Royal London Hospital or the general practitioner out of hours service with acute asthma. We identified eligible participants prospectively by monitoring attendance at these services. We also wrote to patients who had been admitted to or had attended the accident and emergency department with asthma in the previous two years. We invited eligible patients to attend a specialist nurse run asthma clinic at the Royal London Hospital, where we sought consent to participate according to the randomisation status of their practice and access to medical records.
Practices and participants
The two specialist nurses were accredited by the National Respiratory Training Centre in Stratford, east London. They intervened at the levels of the general practice and the patient (see bmj.com).
General practices randomised to the intervention group received two one hour visits by the specialist nurses at the start of the study to discuss guidelines for managing patients with acute asthma. We used a behaviour change model, incorporating discussion of relevant research evidence.17 We provided a computer template or stamp to prompt patient review, including identification as a patient with high risk asthma, inhaler technique and peak expiratory flow assessment, and self management advice.
Participants registered with the intervention practices were reviewed for asthma control and drugs by the specialist nurses at the nurse run clinic immediately after recruitment. They discussed a self management plan. Patients with sufficient understanding were provided with a peak flow meter, a supply of rescue oral corticosteroids for future use, and a written plan produced by the National Asthma Campaign with standard thresholds for peak flow and symptoms. Instructions were to double their dose of inhaled corticosteroid if their peak expiratory flow rate was between 70% and 80% of best or they were waking at night with symptoms, to contact their doctor to arrange a course of oral corticosteroids if their peak expiratory flow rate was between 50% and 70% or breathlessness was increasing, and to contact their doctor urgently if their peak expiratory flow rate was below 50% of best or if symptoms continued to worsen. Most South Asian participants were Bangladeshis speaking Sylheti—a dialect with no written form; they received a plan written in English, explained through a bilingual advocate. Participants with insufficient comprehension of guided self management were educated about their drugs and encouraged to contact their general practice should their asthma control worsen. Nurses reinforced advice with a face to face or telephone consultation.
The control group received a single visit from the nurses to discuss standard guidelines for asthma. Participants registered with control practices were checked for inhaler technique in the nurse run clinic immediately after recruitment. Drugs were unaltered. Participants otherwise continued with usual care.
Outcome measures
Prespecified primary outcomes were the percentage of participants attending for unscheduled asthma care and the time to first attendance for unscheduled asthma care in the year after intervention. Unscheduled care was defined as a consultation in primary, secondary, or out of hours care, where a participant presented with symptoms or signs related to acute asthma, including wheeze, cough, or breathlessness. We included acute presentations for cough requiring for example an increase in asthma drugs or antibiotics, and we logged these separately.
Secondary outcomes were rates of attendance for unscheduled care and review, self management behaviour, and quality of life, assessed by generic (EQ-5D) and respiratory specific (AQ20 and north of England) scales.6,18-20 Consultations for non-acute asthma were classified as reviews or other consultations.
Data collection
Medical records
Researchers blinded to the randomisation status of the general practice photocopied written and computerised general practice records. We obtained medical records for the 13 participants who had moved out of the study area. With blinding retained, we checked the hospital administration records for admissions and accident and emergency attendances that may have been missing from the general practice records. To retain blinding during data extraction, GF removed from the records any letters from the specialist nurse. CG extracted data outside the practice setting. Completeness and accuracy of extraction was validated by another blinded researcher (GSF), who checked 10 sets of records, chosen using random numbers. Of 165 consultations assessed, there were five discrepancies (3%) involving misclassification of unscheduled care.
Interviews
Two researchers blinded to randomisation status interviewed participants in person at baseline and by telephone at two, six, nine, and 12 months after recruitment to gather data on personal characteristics, quality of life, and self management of asthma. Participants self identified their ethnicity. We adapted outcome scales into Sylheti; validation of this audiotaped version was by back translation using lay and expert panels and comparison of randomised sequential interviews of bilingual respondents.21
Statistical power and analyses
Audit in a pilot general practice showed that 90% of high risk patients had unscheduled care over one year. Allowing for clustering, our study was powered (80%) to detect a 15% decrease (90% to 75%) in the percentage of patients requiring unscheduled care, at the 5% significance level; we considered a 10-15% change to be clinically important. Based on previous studies, we used 0.05 as an estimate of intracluster correlation. After taking into account drop outs and unequal numbers of patients in practices, we estimated 145 patients were needed in each group. Sample size for time to first attendance could not be estimated due to inadequate data.
Before breaking the coded allocation of practices, we carried out main and prespecified subgroup analyses. Analyses for primary outcomes were by ethnicity (South Asian (Bangladeshi, Indian, Pakistani), white, other), after exclusion of patients with both asthma and chronic obstructive pulmonary disease noted in the medical records, those recruited retrospectively and prospectively, and children and adults. For secondary outcomes we carried out the main and subgroup analyses by ethnicity.
For unscheduled care, review, and quality of life, we fitted generalised estimating equations to individual level data in STATA, fitting different equations depending on the type of outcome; binary, time to event, or number of events. In each case we specified the model to take account of the clustering by practice. For time to unscheduled care and time to review we fitted proportional hazards models assuming an underlying Weibull distribution for the hazard. We used model diagnostics to choose appropriate models. Analyses were by intention to treat. Participants who changed general practice during the study were analysed in the group to which they were allocated at recruitment.
We allowed for clustering by practice except when the intracluster correlation was negative (implying that individuals within clusters were more divergent for the outcome than the general population); in this case we attributed this to sampling error and present results with and without clustering. Covariates were number of exacerbations or reviews at baseline and time since last exacerbation, as appropriate. Time to first contact for unscheduled care and review are represented by Kaplan-Meier plots.
For self management we analysed data at the level of the episode (exacerbation). Self management behaviour was reported for each exacerbation. We initially fitted models accounting for clustering within individuals, which was much stronger than clustering within practice. Because these models showed wide and inconclusive confidence intervals we did not pursue further analyses adjusting for clustering at both individual and practice level.
Results
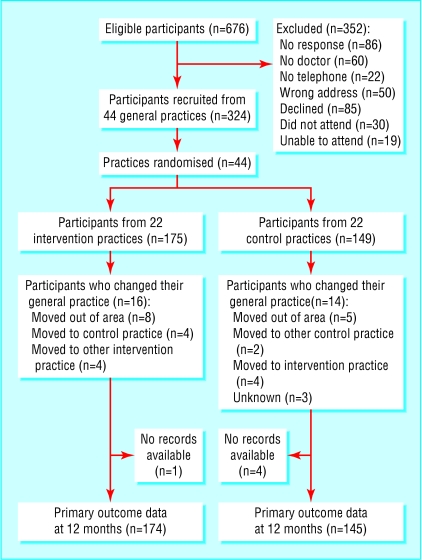
Practices in the intervention and control groups were well matched for stratifying factors (table 1). Figure 1 shows the flow of participants and practices through the trial. Practices contributed a mean of eight (range 2-28) participants. The characteristics of participants were similar between groups (table 2). Overall, 50% (164/324) of the participants were South Asian, 34% (108) were white, and 16% (52) were from 12 other ethnic groups, predominantly black African, Afro-Caribbean, and black British. Fourteen different first languages were spoken; 45% (146) of participants spoke English. Eighty nine per cent (269) lived in rented accommodation and 55% (177) were unemployed. Overall, 63% (204) of participants were recruited prospectively after attendance with acute asthma. The remainder met eligibility criteria over the previous years.
Fig 1.
Flow of practices and participants through study
Table 2.
Characteristics of participants allocated to nurse led intervention for acute asthma or standard guidelines for asthma. Values are numbers (percentages) unless stated otherwise
| Characteristic | Intervention group (n=175) | Control group (n=149) |
|---|---|---|
| Male | 85 (49) | 76 (51) |
| Mean (SD) age (years) | 22.9 (17.4) | 22.2 (18.1) |
| Age <16 years | 91 (52) | 81 (54) |
| Ethnicity: | ||
| South Asian | 95 (54) | 69 (46) |
| White | 56 (32) | 52 (35) |
| Other | 24 (14) | 28 (19) |
| Fluent in English | 141 (81) | 133 (89) |
| English as first language | 73 (42) | 73 (49) |
| Housing* : | ||
| Rented | 152 (88) | 117 (89) |
| Owned | 20 (12) | 16 (11) |
| Employment status of participants (or parent): | ||
| Unemployed | 97 (55) | 80 (54) |
| Employed | 67 (38) | 56 (38) |
| Unknown | 11 (7) | 13 (8) |
| Current smokers (adults aged >16 only) | 26 (31) | 24 (35) |
| Chronic obstructive pulmonary disease in medical record | 13 (7) | 9 (6) |
| Receiving inhaled corticosteroids | 127 (73) | 107 (72) |
Data for 172 intervention and 142 control participants.
Primary outcome: unscheduled asthma care
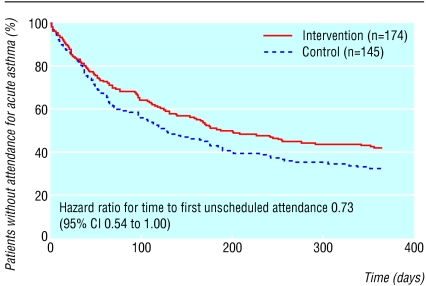
Primary outcome data were gathered for 98% (319/324) of participants. The specialist nurse intervention delayed first attendance for unscheduled asthma care in the year after intervention (fig 2, adjusted hazard ratio for reattendance 0.73, 95% confidence interval 0.54 to 1.00) and reduced the percentage of participants attending for unscheduled care over the following year (58% (101/174) for intervention v 68% (99/145) for control, adjusted odds ratio with clustering 0.61, 0.38 to 0.99, without clustering 0.62, 0.38 to 1.01; table 3). Mean rates of hospital admission, attendance at accident and emergency, and attendance at general practice for exacerbations were all non-significantly lower in the intervention group than in the control group (data not shown). The overall rates of yearly attendance for unscheduled care for each participant were 1.98 for the intervention group and 2.36 for the control group (adjusted incidence rate ratio 0.91, 0.66 to 1.26).
Fig 2.
Time to first unscheduled attendance with acute asthma after intervention for all participants (number of participants without reattendance at 365 days was 73 for intervention and 47 for control)
Table 3.
Percentages (numbers) of participants attending for unscheduled asthma care and for review of asthma in year after intervention
| Outcome | Intervention group (n=174) | Control group (n=145) | Intracluster correlation | Adjusted odds ratio (95% CI) |
|---|---|---|---|---|
| Unscheduled care | 58 (101) | 68 (99) | −0.0056 | 0.62 (0.38 to 1.01)* ; 0.61 (0.38 to 0.99)† |
| Reviewed | 65 (113) | 54 (78) | 0.0905 | 1.66 (0.96 to 1.98) |
| Reviewed in primary care | 47 (82) | 36 (52) | 0.2077 | 1.40 (0.72 to 2.73) |
Without clustering.
With clustering.
Secondary outcomes
Review of asthma care
Overall, 54% (78/145) of participants in the control group were reviewed in secondary or primary care in the year after intervention compared with 65% (113/174) in the intervention group (adjusted odds ratio 1.66, 0.96 to 1.98; table 3); 36% (52/145) of participants in the control group were reviewed in primary care compared with 47% (82/174) in the intervention group (1.40, 0.72 to 2.73). Participants in the intervention group received 1.84 reviews yearly compared with 1.56 of participants in the control group (incidence rate ratio 1.15, 0.85 to 1.57).
Self management behaviour, quality of life, and symptoms
Self management behaviour and scores for quality of life and asthma symptoms showed no differences at two or 12 months follow up (table 4). Oral rescue corticosteroids were used by similar numbers of participants in each group (4% (7/174) intervention, 7% (10/145) control, odds ratio 0.7, 0.28 to 1.68).
Table 4.
Self management behaviour during exacerbations of asthma, quality of life (AQ20 questionnaire), and symptom scores (north of England scale) at two and 12 months' follow up for participants allocated to nurse led intervention for acute asthma or standard guidelines for asthma. Values are numbers (percentages) of participants unless stated otherwise
| Follow up | Intervention group | Control group | Estimated effect (95% CI) |
|---|---|---|---|
| Two months | |||
| Increased use of bronchodilator* | 111/116 (96) | 71/79 (90) | 2.33 (0.68 to 7.98) |
| Increased use of inhaled corticosteroid* | 49/116 (42) | 38/79 (48) | 0.84 (0.41 to 1.70) |
| Used peak flow meter* | 41/116 (35) | 34/79 (43) | 1.07 (0.52 to 2.19) |
| Scores: | |||
| Quality of life | 10.87 (n=70) | 10.73 (n=52) | 0.16 (−1.75 to 2.07)† |
| Asthma symptoms | 10.75 (n=157) | 11.28 (n=128) | −0.43 (−1.74 to 0.88)† |
| 12 months | |||
| Increased use of bronchodilator* | 518/540 (96) | 484/509 (95) | 1.16 (0.61 to 2.20) |
| Increased use of inhaled corticosteroid* | 238/540 (44) | 238/507 (47) | 0.84 (0.55 to 1.29) |
| Used peak flow meter* | 162/540 (30) | 137/507 (27) | 1.20 (0.76 to 1.91) |
| Scores: | |||
| Quality of life | 11.23 (n=52) | 12.13 (n=48) | −0.84 (−3.18 to 1.50)† |
| Asthma symptoms | 10.35 (n=133) | 11.51 (n=118) | −1.06 (−2.43 to 0.30)† |
Unit of analysis was exacerbation; adjusted for within patient correlation in behaviour but not for within practice correlation. Only analyses without clustering by practice are presented (initial results did not warrant more sophisticated analyses).
Difference.
Subgroup analyses
Exploratory hypothesis generating analysis comparing the effect of specialist nurse intervention on time to attendance between white patients, South Asian patients, and other ethnic groups was not statistically significant (white to South Asian hazard ratio 0.76, 0.44 to 1.29; white to other ethnicities 0.64, 0.39 to1.06). It was, however, compatible with a larger effect for white participants (intervention group compared with control group hazard ratio 0.57, 0.38 to 0.85; South Asians 0.72, 0.48 to 1.09; other ethnicities 1.29, 0.51 to 3.22). The effect of the intervention was not significantly different for other subgroup analyses.
Discussion
Asthma specialist nurses using a liaison model reduced unscheduled care for acute asthma in a deprived multiethnic area. The intervention delayed attendance with acute asthma and reduced the percentage of participants attending with acute asthma over the following year. Rates of hospital admission, attendance at an emergency department, and visits to primary care for acute asthma were all non-significantly lower for participants receiving specialist nurse care, suggesting an impact on healthcare utilisation across both primary and secondary care. These improvements occurred despite comparison with a control group of practices receiving educational outreach for asthma, which itself improves care.15 We found no significant changes in self management behaviour, use of oral rescue corticosteroids, or quality of life, perhaps because our instruments were insufficiently sensitive. Small, non-significant changes were found in the ratio of prescribed inhaled corticosteroid to bronchodilators between groups (data not shown). We did not assess compliance.22
Strengths of our study include completeness of follow up for primary outcome data and a pragmatic design with inclusion of all general practices in one health district, with a representative sample of the local multiethnic population. Use of a control group receiving outreach visits promoting standard asthma guidelines as a comparator for specialist nurse intervention had three benefits: it allowed a comparison against best usual practice, it reduced the impact of any Hawthorne effect (all practices received some education), and it promoted recruitment of a broader range of practices, increasing external validity. Although a secondary aim was to detect differences in effect between ethnic groups, this prespecified subgroup analysis had limited power.
Our liaison model was more effective than the community based approach evaluated in the Greenwich asthma study, with its similar setting in inner London.7 In that study, specialist nurses educated practice nurses but not patients, and outcomes were assessed in the wider population of patients with milder asthma rather than a high risk group. Our liaison model of specialist nursing is probably as effective as the secondary care model, but provides additional support for patients in the community through patient education and clinical recommendations for general practitioners and direct clinical support for patients.2-6 This may be important in inner city areas, where general practices vary in their capacity to manage chronic illness.8 A liaison model of specialist nursing has only previously been evaluated (using a randomised design) for patients discharged after a coronary event.23 This study showed no benefits from the intervention, perhaps because liaison lacked direct clinical involvement in care and was limited to supporting practice nurses.
Ethnicity
Our study was not powered to detect differences in effect of the intervention between ethnic groups, but our exploratory findings are compatible with potentially important differences in outcome between ethnic groups. This is consistent with other work suggesting that minority ethnic groups derive less benefit than majority groups from asthma education.14 No randomised studies of interventions specifically addressing ethnic minority groups have reduced unscheduled asthma care.14,24 These observations are important because interventions that have a differential benefit between majority and minority ethnic groups potentially widen inequalities in health.
What is already known on this topic
Clinical specialist nurse outreach to primary care has not been shown to improve patient outcomes
Education of hospital attenders with acute asthma by asthma specialist nurses has inconsistent effects on unscheduled care
People with asthma from ethnic minority groups experience high levels of morbidity
What this study adds
When asthma specialist nurses educated patients and liaised with primary care clinicians, unscheduled care in a deprived multiethnic area was reduced
Ethnic groups may not benefit equally from specialist nurse intervention
Supplementary Material
 Protocol for study groups is on bmj.com
Protocol for study groups is on bmj.com
We thank the National Asthma Campaign for funding; the participants; Mark Levy for advice on study design; and Yvonne Carter, Allen Hutchinson, Keith Meadows, Jeanette Naish, Peter Stables, Ayesha Khanem, Enid Hennessey, Pat Sturdy, Sarah Cotter, Monica Fletcher, and members of the department of general practice for comments and help.
Contributors: CG conceived the study. CG, NB, GSF, SE, and AL designed the study. GF and SB recruited and followed up the participants. MW and CD carried out the intervention. TC and RH developed recruitment. SE and HT carried out statistical analyses. CG wrote the first draft on which all commented. CG will act as guarantor for the paper.
Funding: National Asthma Campaign.
Competing interests: None declared.
Ethical approval: The study was approved by the local research ethics committee.
References
- 1.Hobbs R, Murray ET. Specialist liaison nurses. BMJ 1999;318: 683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Madge P, McColl J, Paton J. Impact of a nurse-led home management training programme in children admitted to hospital with acute asthma: a randomised controlled study. Thorax 1997;52: 223-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Osman LM, Calder C, Godden DJ, Friend JA, McKenzie L, Legge JS, et al. A randomised trial of self-management planning for adult patients admitted to hospital with acute asthma. Thorax 2002;57: 869-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stevens CA, Wesseldine LJ, Couriel JM, Dyer AJ, Osman LM, Silverman M. Parental education and guided self-management of asthma and wheezing in the pre-school child: a randomised controlled trial. Thorax 2002;57: 39-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wesseldine LJ, McCarthy P, Silverman M. Structured discharge procedure for children admitted to hospital with acute asthma: a randomised controlled trial of nursing practice. Arch Dis Child 1999;80: 110-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levy ML, Robb M, Allen J, Doherty C, Bland JM, Winter RJ. A randomized controlled evaluation of specialist nurse education following accident and emergency department attendance for acute asthma. Respir Med 2000;94: 900-8. [DOI] [PubMed] [Google Scholar]
- 7.Premaratne UN, Sterne JAC, Marks GB, Webb JR, Azima H, Burney PGJ. Clustered randomised trial of an intervention to improve the management of asthma: Greenwich asthma study. BMJ 1999;318: 1251-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Griffiths C, Sturdy P, Naish J, Omar R, Dolan S, Feder G. Hospital admissions for asthma in east London: associations with characteristics of local general practices, prescribing, and population. BMJ 1997;314: 482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ehrlich RI, Bourne DE. Asthma deaths among coloured and white South Africans: 1962 to 1988. Respir Med 1994;88: 195-202. [DOI] [PubMed] [Google Scholar]
- 10.Ng TP, Tan WC. Temporal trends and ethnic variations in asthma mortality in Singapore, 1976-1995. Thorax 1999;54: 990-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ormerod LP. Adult Asian acute asthma admissions reassessed: Blackburn 1991-1992. Respir Med 1995;89: 415-7. [DOI] [PubMed] [Google Scholar]
- 12.Gilthorpe MS, Lay-Yee R, Wilson RC, Walters S, Griffiths RK, Bedi R. Variations in hospitalization rates for asthma among black and minority ethnic communities. Respir Med 1998;92: 642-8. [DOI] [PubMed] [Google Scholar]
- 13.Griffiths C, Kaur G, Gantley M, Feder G, Hillier S, Goddard J, et al. Influences on hospital admission for asthma in south Asian and white adults: qualitative interview study. BMJ 2001;323: 962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moudgil H, Marshall T, Honeybourne D. Asthma education and quality of life in the community: a randomised controlled study to evaluate the impact on white European and Indian subcontinent ethnic groups from socioeconomically deprived areas in Birmingham, UK. Thorax 2000;55: 177-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feder G, Griffiths C, Highton C, Eldridge S, Spence M, Southgate L. Do clinical guidelines introduced with practice based education improve care of asthmatic and diabetic patients? A randomised controlled trial in general practices in east London. BMJ 1995;311: 1473-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Altman DG. Practical statistics for medical research. London: Chapman and Hall, 1991.
- 17.Thomson O'Brien MA, Oxman AD, Davis DA, Haynes RB, Freemantle N, Harvey EL. Educational outreach visits: effects on professional practice and health care outcomes (Cochrane Review). In: Cochrane Library, Issue 4. Chichester: John Wiley, 2003. [DOI] [PubMed]
- 18.EuroQol Group. EuroQol: a new facility for measurement of health related quality of life. Health Policy 1990;16: 199-208. [DOI] [PubMed] [Google Scholar]
- 19.Barley EA, Quirk FH, Jones PW. Asthma health status measurement in clinical practice: validity of a new short and simple instrument. Respir Med 1998;92: 1207-14. [DOI] [PubMed] [Google Scholar]
- 20.Steen N, Hutchinson A, McColl E, Eccles MP, Hewison J, Meadows KA, et al. Development of a symptom based outcome measure for asthma. BMJ 1994;309: 1065-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Griffiths C, Ahmed S, Ahmed S, Nandy S, Abrams C, Meadows KA, et al. Using health-related quality of life measures in minority ethnic groups: an approach to translating measures into Bengali (Sylheti). Eur J Gen Pract 2000;6: 130-4. [Google Scholar]
- 22.Gallefoss F, Bakke P. How does patient education and self-management among asthmatics and patients with chronic obstructive pulmonary disease affect medication? Am J Respir Crit Care Med 1999;160: 2000-5. [DOI] [PubMed] [Google Scholar]
- 23.Jolly K, Bradley F, Sharp S, Smith H, Thompson S, Kinmonth AL, et al. Randomised controlled trial of follow up care in general practice of patients with myocardial infarction and angina: final results of the Southampton heart integrated care project (SHIP). BMJ 1999;318: 706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bonner S, Zimmerman BJ, Evans D, Irigoyen M, Resnick D, Mellins RB. An individualized intervention to improve asthma management among urban Latino and African-American families. J Asthma 2002;39: 167-79. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.