Abstract
Objective
To examine the influence of social factors (e.g., attention, relief from responsibility) and children’s perceived competence on pediatric symptom maintenance.
Methods
Participants were 151 pediatric patients (ages 8–18) with recurrent abdominal pain. They were interviewed at a clinic visit and again 2 weeks later. The Social Consequences of Pain questionnaire assessed four types of social consequences: positive attention, negative attention, activity restriction, and privileges.
Results
Two types of social consequences (positive attention and activity restriction) predicted greater symptom maintenance, but this effect was moderated by children’s perceived self-worth and academic competence. To the extent that children rated their self-worth and academic competence as low, the impact of social factors on symptom maintenance was stronger.
Conclusions
Children’s success in their normal social roles may affect the extent to which they identify with the sick role and find it a rewarding alternative to other social roles.
Keywords: recurrent abdominal pain, social learning, secondary gain, perceived competence
Diverse theoretical traditions propose that symptom maintenance may be influenced by social consequences of illness. Freud (1959) introduced the psychodynamic concept of secondary gain, defined as interpersonal or social advantage attained by the patient as a consequence of illness. Behavior theory offers an alternative conceptual framework in which symptoms and disability are regarded as responses influenced by their consequences. Applying this operant conditioning model to chronic pain, Fordyce (1989) suggested that consequences such as positive attention from others may serve as rewards that reinforce symptoms. The constructs of secondary gain and reinforcers are similar in that both are social consequences hypothesized to maintain symptoms (Fishbain, 1994). These constructs have been applied in efforts to understand maintenance of symptom complaints and disability in both adults and children (Craig, 1978; McGrath, 1990).
It has been proposed that the impact of social consequences on illness behavior in children may vary as a function of children’s psychosocial development (Walker, 1999). For example, a critical task of middle childhood is the development of a sense of mastery or competence (Erikson, 1964). Relief from responsibility as a consequence of illness may be more rewarding for children who have not developed a sense of competence than for children who perceive themselves as competent. Specifically, children who perceive themselves as inadequate may welcome being excused from the challenge of school and social activities; for them, relief from responsibility may serve as a reward that reinforces illness-related disability. In contrast, children who perceive themselves as competent may regard being excused from activities as a lost opportunity for further success; for them, relief from responsibility may be aversive and is unlikely to reinforce symptoms and disability.
In addition to relief from responsibility, children may receive solicitous attention from others as a consequence of illness. Theoretical and empirical literature suggests that such interpersonal attention may reinforce symptom complaints (e.g., Blount et al., 1989; Fordyce, 1989). For example, solicitous attention from parents predicted slower recovery from oral surgery in adolescent patients (Gidron, McGrath, & Goodday, 1995). The impact of solicitous attention on children’s illness behavior may also vary as a function of children’s competence. For example, children who have not mastered school activities and peer relationships may welcome attention for symptoms as an alternative source of self-validation. In contrast, children who perceive themselves as competent in routine daily activities may place less value on attention for symptoms.
This study tested the hypothesis that the impact of social consequences on symptom maintenance is moderated by children’s perceived success at normative tasks of psychosocial development. We conceptualized this success in terms of perceived global self-worth as well as perceived competence specific to academic and social roles (cf. Harter, 1985). The study sample consisted of children with recurrent abdominal pain (RAP), a common pediatric condition typically not associated with significant organic disease (Apley, 1975). Children with RAP experience frequent debilitating episodes of abdominal pain and complain of a variety of other nonspecific somatic symptoms as well (Walker, Garber, & Greene, 1991). An advantage of studying symptom maintenance in a functional condition such as RAP was that the course of organic disease was not a confound in predicting changes in children’s symptoms. We expected that positive attention and relief from responsibility would predict symptom maintenance 2 weeks following a medical evaluation, but this effect would be moderated by children’s perceived competence. Specifically, the impact of positive attention and relief from responsibility on symptom maintenance was expected to be greater at lower levels of perceived competence.
Social consequences of illness may be negative as well as positive. According to behavioral theory, negative attention from others (e.g., irritation) should punish and therefore decrease symptoms. However, the empirical literature is mixed regarding the impact of negative attention on symptom maintenance. For example, in a study of adult pain patients, negative attention from others was associated with increased pain behavior, perhaps because negative attention created affective distress that contributed to somatic symptoms (Kerns et al., 1991). Therefore, we did not make specific hypotheses regarding the impact of negative social consequences on children’s symptom maintenance.
Instruments designed to assess social consequences of illness in children have focused exclusively on positive responses by parents toward their children (cf. Walker & Zeman, 1992; Whitehead et al., 1982; 1986). Thus, a secondary goal of this study was to develop a new instrument, the Social Consequences of Pain Questionnaire (SCP), which assesses both positive and negative social consequences of children’s illness behavior. Factor analysis was conducted to identify dimensions of social consequences assessed by the new instrument. Preliminary validity data also were obtained.
Method
Participants
Study participants included 151 children referred to a pediatric gastroenterology clinic for evaluation of recurrent episodes of abdominal pain of at least 3 months’ duration (cf. von Baeyer & Walker, 1999). New patients without identified organic disease or mental retardation were eligible. Participants ranged in age from 8 to 18 years (M = 12.01, SD = 2.5). Most were female (57%) and Caucasian (96%). Family socioeconomic status (SES) ranged from the lowest (8) to highest level (66) on the Hollingshead Two-Factor Index of Social Status (Hollingshead, 1975) (M = 41.91, SD = 11.70).
Procedure
Parents of patients referred for evaluation of abdominal pain were contacted by telephone several days prior to the scheduled clinic appointment. The study was described and those who expressed interest were screened for eligibility criteria and asked to arrive early at the clinic. Informed consent procedures, approved by the institutional review board, were conducted prior to administering the study protocol. Parents completed questionnaires in the waiting room while children were interviewed in a private room nearby. A second interview with the children was conducted by telephone two weeks following the initial interview.
Development of a Measure of Social Consequences of Pain
The Illness Behavior Encouragement Scales (IBES; Walker & Zeman, 1992) provided the format and initial content for development of the SCP. The IBES refers exclusively to positive consequences delivered by parents. The SCP includes consequences delivered by parents, teachers, and peers. Moreover, the SCP assesses both positive consequences (e.g., attention, relief from responsibility, and privileges associated with illness) and negative consequences (e.g., being ignored or criticized for symptom complaints). The stem for SCP items is “When you have a bad stomach ache, how often …” Like the IBES, the 5-point response format includes “Never” (coded 0), “Hardly Ever” (coded 1), “Sometimes” (coded 2), “Often” (coded 3), and “Always” (coded 4). The SCP was administered at the initial evaluation.
The SCP was factor analyzed using a principal-components factor analysis with varimax rotation. Inspection of the scree plot of eigenvalues suggested a four-factor solution. Items with the highest factor loadings were used to define each of the four factors. The initial factor accounted for 23.1% of the variance and was characterized by positive attention from others. It was labeled “positive attention.” Factor 2 (10.5% of the variance) included items assessing relief from responsibilities and restriction of activities. It was labeled “activity restriction” (rather than “relief from responsibility”) to avoid the implication that not doing one’s chores was necessarily a “relief.” Factor 3 (6.4% of the variance) included items assessing criticism and failure of others to validate the child’s symptoms. It was labeled “negative attention.” Factor 4 (5.5% of the variance) included items reflecting special privileges and was labeled “privileges.” Table I lists the items, factor loadings, and eigenvalues for each factor. Subscale scores were computed as the average item rating for each factor.
Table I.
Factor Loadings for the Items from the Social Consequences of Pain Scale
| Items | Factors
|
|||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| When you have a bad stomach ache, … | ||||
| Does your mom or dad give you a lot of extra attention? | .72 | .19 | −.14 | .36 |
| Does your mom or dad spend more time than usual with you? | .72 | .04 | .02 | .06 |
| Does your mom or dad stay at home with you more? | .71 | .20 | −.01 | .06 |
| Does your mom or dad check on you a lot to see how you’re feeling? | .68 | .21 | −.15 | .01 |
| Is your mom or dad extra nice to you? | .64 | .05 | −.09 | .34 |
| Does your mom or dad tell others in the family not to bother you? | .60 | .14 | .18 | −.14 |
| Do you do fewer chores (like not putting your things away)? | .59 | .36 | .19 | .17 |
| Are the kids extra nice to you? | .50 | .12 | −.05 | .31 |
| Is the teacher extra nice to you? | .47 | .00 | −.10 | .21 |
| Do you sleep or rest somewhere special, like in your parents’ room or on the couch? | .36 | .28 | .29 | .32 |
| Does your mom or dad tell you that you’ll be OK? | .32 | .00 | .20 | .10 |
| Do you get behind in your schoolwork? | −.05 | .65 | .15 | −.02 |
| Do you spend more time in bed or on the couch? | .33 | .61 | .03 | .00 |
| Do you spend less time with other kids? | .15 | .60 | .10 | −.01 |
| Do you miss a test at school? | −.01 | .60 | .20 | .22 |
| Do you spend more time inside? | .38 | .59 | .08 | −.09 |
| Do you spend less time doing sports or exercise? | .29 | .58 | .01 | −.09 |
| Do you have to stay at home and not go anywhere? | .24 | .56 | .23 | .19 |
| Do you stay home from school? | −.05 | .55 | −.12 | .09 |
| Do you do less homework and other schoolwork? | .09 | .53 | −.02 | .38 |
| Do you sleep later than usual in the morning? | .06 | .53 | .13 | .27 |
| Do you miss gym class (P.E.) at school? | .19 | .39 | .09 | .07 |
| Does your mom or dad get mad or frustrated with you? | −.09 | .19 | .77 | .01 |
| Does your mom or dad tell you that there’s nothing they can do about your stomach ache? | .00 | .15 | .76 | .00 |
| Does your mom or dad tell you not to make such a fuss about your stomach? | .13 | .05 | .73 | .08 |
| Does your mom or dad ignore you when you talk about your stomach hurting? | −.04 | .14 | .66 | .04 |
| Does your mom or dad expect you to do things anyway? | −.37 | −.31 | .50 | −.01 |
| Do kids hassle you? | .11 | .38 | .40 | −.14 |
| Do you get special privileges like staying up late or watching more TV? | .14 | .15 | .05 | .72 |
| Does your mom or dad let you get away with more things? | .27 | .20 | .06 | .72 |
| Do you spend more time doing things you like? | .07 | −.18 | .04 | .66 |
| Do you get special food or drinks? | .20 | .27 | −.05 | .46 |
| Eigenvalues | 7.40 | 3.36 | 2.06 | 1.76 |
| Percentage of variance | 23.1 | 10.5 | 6.4 | 5.5 |
Other Measures
Children’s Somatization Inventory
The Children’s Somatization Inventory (CSI; Garber, Walker, & Zeman, 1991; Walker, Garber, & Greene, 1991) assesses the severity of nonspecific somatic symptoms commonly reported by children with RAP. It was completed by children at the initial visit and again 2 weeks later. The CSI includes symptoms from the revised third edition of the Diagnostic and Statistical Manual of Mental Disorders criteria for somatization disorder (DSM-III-R: American Psychiatric Association, 1987) and from the somatization factor of the Hopkins Symptom Checklist (Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, 1974). Examples of items include “headaches,” “feeling low in energy,” and “faintness or dizziness.” Respondents rate the extent to which they have experienced each of the 35 symptoms during the last 2 weeks using a 5-point scale ranging from “not at all” (0) to “a whole lot” (4). Total scores, obtained by summing all item ratings, can range from 0 to 140. Three-month test-retest Pearson reliability for the CSI is .50 for well patients and .66 for patients with a chronic pain syndrome (Walker et al., 1991). In this study, alpha reliability was .89 at the initial administration and .91 at the follow-up administration.
Perceived Competence
Children’s perceived competence was assessed at the initial evaluation with three subscales of the Self-Perception Profile for Children (SPPC; Harter, 1985). The SPPC assesses children’s global and domain-specific perceptions of self-worth. Subscales included in this study were Global Self-Worth, Academic Competence, and Social Competence. The SPPC has a 4-point response format and six items on each subscale. Harter (1985) reported adequate internal consistency and convergent validity. Total scores on each subscale were computed by summing responses to items on that subscale. Alpha reliability was .83 for Global Self-Worth, .77 for Academic Competence, and .59 for Social Competence.
Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, Powell, Farley, Werkman, & Berkoff, 1990)
The MSPSS is a brief, self-report measure of perceived social support. It was administered to children at the initial evaluation. Subscales assessing Family Support and Peer Support were administered in order to examine their relation to SCP positive attention and negative attention. Each MSPSS subscale has four items rated on a 7-point Likert-type scale ranging from “very strongly disagree” (coded 1) to “very strongly agree” (coded 7). The MSPSS has good internal reliability and strong factorial validity (Zimet et al., 1990). In this study, alpha reliability was .74 for Family Support and .71 for Peer Support.
Results
Psychometric Properties and Descriptive Data on the SCP Scales
Alpha Reliability and Intercorrelation of SCP Scales
Alpha reliability for the SCP subscales was .73 for negative attention, .84 for positive attention, .83 for activity restriction, and .67 for privileges. The intercorrelation among the subscales is presented in Table II. The Pearson correlation coefficients between SCP subscales ranged from .02 (between privileges and negative attention) to .50 (between positive attention and activity restriction), indicating that the sub-scales assess relatively independent constructs.
Table II.
Pearson Correlation Among Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Positive attention | .24** | .45*** | .07 | −.27*** | .00 | −.03 | .23** | .24** | .11 | .16 | −.03 | |
| 2. Activity restriction | .50*** | .24** | .03 | .29*** | .24** | −.12 | .02 | −.15 | −.06 | −.03 | ||
| 3. Privileges | .02 | −.01 | .01 | −.06 | −.01 | .12 | .06 | .15 | .03 | |||
| 4. Negative attention | −.03 | .22** | .34*** | −.35*** | −.15 | −.24** | −.10 | −.22 | ||||
| 5. Age | .29*** | .18* | −.30*** | −.02 | −.15 | −.15 | .08 | |||||
| 6. CSI (clinic) | .72*** | −.22** | −.16* | −.17* | −.11 | −.04 | ||||||
| 7. CSI (follow-up) | −.41*** | −.22** | −.25*** | −.13 | −.13 | |||||||
| 8. Mother support | .30*** | .37*** | .16 | .08 | ||||||||
| 9. Friend support | .21 | .21** | .39*** | |||||||||
| 10. Global self-worth | .50*** | .51*** | ||||||||||
| 11. Academic competence | .36*** | |||||||||||
| 12. Social competence |
CSI = Children’s Somatization Inventory.
p < .05.
p < .01.
p < .001.
Relation of Pain Consequences to Other Constructs
Construct validity of the SCP was assessed by examining the Pearson correlations of the SCP subscales with other variables and constructs including age and social support (Table II). Age had a significant negative correlation with positive attention, probably reflecting decreased parental oversight as children enter adolescence. Positive attention had significant positive correlations with MSPSS family and peer support, whereas negative attention had significant negative correlations with measures of support, providing evidence for the construct validity of these SCP subscales.
Frequency of Social Consequences by Child Gender and Type of Consequence
Analysis of variance with child gender as a factor and type of consequence as a repeated measure indicated a significant difference in the frequency of the different types of consequences (Wilks Lambda [3, 145] = 88.11, p < .0001). Positive Attention was endorsed significantly more frequently than activity restriction (t[151] = 3.26, p < .0001), which in turn was endorsed significantly more frequently than privileges (t[150] = 8.73, p < .0001). Finally, privileges was endorsed significantly more frequently than negative attention (t[150] = 2.38, p < .02). The mean item rating and standard deviation for each subscale was as follows: positive attention, M = 1.97, SD = .81; activity restriction, M = 1.76, SD = .76; privileges, M = 1.11, SD = .84; and negative attention, M = .89, SD = .74. Child gender did not have a significant effect on the frequency of any type of pain consequence.
Pain Consequences as Predictors of Symptom Maintenance
Hierarchical multiple regression analyses were conducted to assess (1) whether pain consequences predicted symptom maintenance 2 weeks following the initial evaluation and (2) whether children’s perceived self-worth, academic competence, and social competence moderated the effect of pain consequences on symptom maintenance. All analyses controlled for initial CSI symptom scores and predicted CSI symptom scores at the 2-week follow-up.
Activity Restriction
The first series of analyses examined the influence of SCP activity restriction on symptom maintenance. Results yielded a significant interaction between activity restriction and global self-worth, shown in Table III. A graph of the interaction between activity restriction and global self-worth indicated that, for children with lower global self-worth, higher levels of activity restriction were associated with higher levels of symptoms at follow-up, controlling for initial symptom levels (Figure 1). Children with higher global self-worth, in contrast, tended to exhibit low symptom levels at follow-up regardless of level of activity restriction. In another analysis, the interaction between activity restriction and academic competence approached significance (p < .06) and was similar to the interaction between activity restriction and global self-worth; activity restriction predicted symptom maintenance in children with low academic competence but not in those with high academic competence. Social competence did not moderate the effect of activity restriction on symptom maintenance.
Table III.
Summary of Hierarchical Regression Analysis Examining the Utility of Activity Restriction and Global Self-Worth in Predicting CSI Symptom Scores at Follow-Up
| Predictor variable | β | T | R2 change |
|---|---|---|---|
| Step 1 | |||
| CSI at initial visit | .69 | 102.88*** | .47*** |
| Step 2 | |||
| SCP activity restriction | .12 | 2.81 | |
| Global self-worth | −.17 | 6.37** | .04** |
| Step 3 | |||
| SCP activity restriction × global self-worth | −.88 | 5.09* | .02* |
p < .05.
p < .01.
p < .001.
Figure 1.
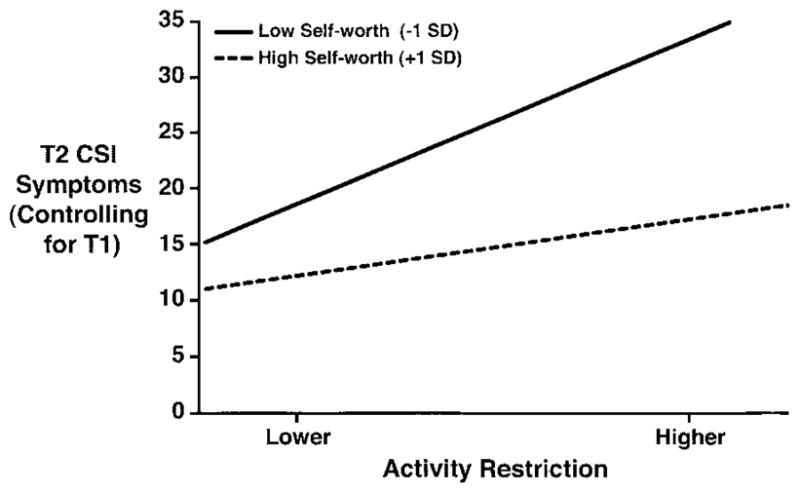
Regression lines controlling for initial (T1) CSI symptom scores and predicting T2 CSI symptom scores for patients with low (−1 SD) and high (+1 SD) scores on Global Self-Worth and varying levels of scores on SCP Activity Restriction.
Positive Attention
The second series of analyses yielded significant effects for the interaction between positive attention and global self-worth and for the interaction between positive attention and academic competence. Results of these analyses are shown in Tables IV and V. Graphs of the interaction effects indicated that, for children with lower global self-worth or academic competence, higher levels of positive attention were associated with higher levels of symptoms at follow-up, controlling for initial symptom levels. Children with higher global self-worth or academic competence, in contrast, tended to exhibit low symptom levels at follow-up regardless of the amount of positive attention that they received for symptoms. The interaction between positive attention and global self-worth is depicted in Figure 2. Social competence did not moderate the effect of positive attention on symptom maintenance.
Table IV.
Summary of Hierarchical Regression Analysis Examining the Utility of Positive Attention and Global Self-Worth in Predicting CSI Symptom Scores at Follow-Up
| Predictor variable | β | T | R2 change |
|---|---|---|---|
| Step 1 | |||
| CSI at initial visit | .69 | 103.76*** | .47*** |
| Step 2 | |||
| SCP positive attention | .01 | 0.05 | |
| Global self-worth | −.18 | 6.91** | .03** |
| Step 3 | |||
| SCP positive attention × global self-worth | −.91 | 5.44* | .02* |
p < .05.
p < .01.
p < .001.
Table V.
Summary of Hierarchical Regression Analyses Examining the Utility of Positive Attention and Academic Competence in Predicting CSI Symptom Scores at Follow-Up
| Predictor variable | β | T | R2 change |
|---|---|---|---|
| Step 1 | |||
| CSI at initial visit | .69 | 103.76** | .47** |
| Step 2 | |||
| SCP positive attention | .01 | 0.03 | |
| Academic competence | −.07 | 0.99 | .01 |
| Step 3 | |||
| SCP positive attention × academic competence | −.86 | 4.60* | .02* |
p < .05.
p < .001.
Figure 2.
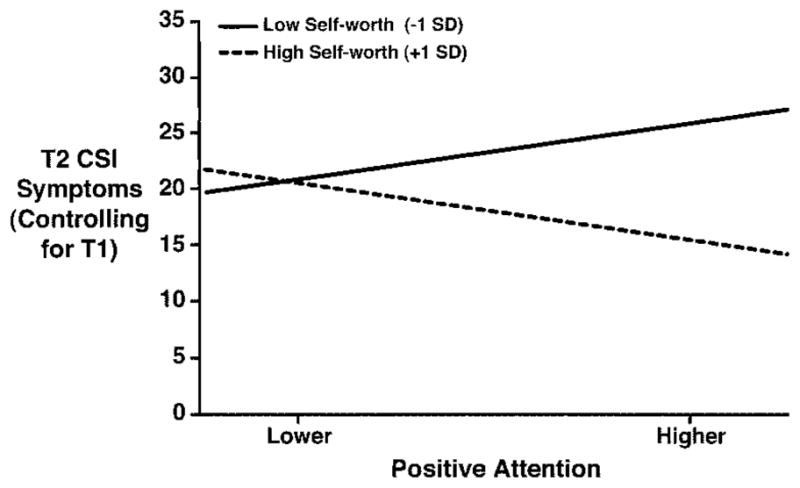
Regression lines controlling for initial (T1) CSI symptom scores and predicting T2 CSI symptom scores for patients with low (−1 SD) and high (+1 SD) scores on Global Self-Worth and varying levels of scores on SCP Positive Attention.
Negative Attention
A third series of analyses indicated a significant interaction effect between negative attention and global self-worth in predicting symptom maintenance. Results of the analysis are presented in Table VI and the interaction effect is illustrated in Figure 3. Higher levels of negative attention were associated with higher symptom levels at follow-up, but only for children with lower global self-worth. Neither perceived academic competence nor social competence moderated the impact of negative attention on symptom maintenance.
Table VI.
Summary of Hierarchical Regression Analysis Examining the Utility of Negative Attention and Global Self-Worth in Predicting CSI Symptom Scores at Follow-Up
| Predictor variable | β | T | R2 change |
|---|---|---|---|
| Step 1 | |||
| CSI at clinic visit | .69 | 103.76** | .47** |
| Step 2 | |||
| SCP negative attention | .23 | 12.09** | |
| Global self-worth | −.13 | 3.73 | .08** |
| Step 3 | |||
| SCP negative attention × global self-worth | −.58 | 3.93* | .02* |
p < .05.
p < .001.
Figure 3.
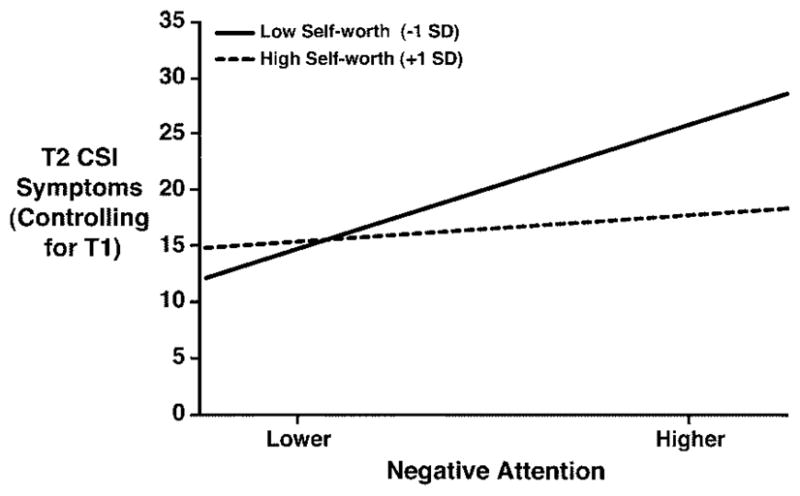
Regression lines controlling for initial (T1) CSI symptom scores and predicting T2 CSI symptom scores for patients with low (−1 SD) and high (+1 SD) scores on Global Self-Worth and varying levels of scores on SCP Negative Attention.
Privileges
The Privileges scale of the SCP had no significant direct or interaction effect on symptom maintenance.
Discussion
Study results suggest that social factors influence symptom maintenance in pediatric pain patients, but the impact of these factors varies as a function of children’s perceived self-worth and academic competence. Among children who rated their self-worth or academic competence as low, restriction of routine daily activities and responsibilities predicted greater symptom maintenance 2 weeks following a medical evaluation. It is possible that activity restriction reinforced symptoms in these children by allowing them to avoid activities at which they expected to perform poorly (cf. Letham, Slade, Troup, & Bentley, 1983). In that sense, activity restriction was indeed a “relief” from responsibility. It also is possible that lower perceived self-worth reflected factors such as depressed mood that contributed to symptom maintenance in these children. Among children with higher perceived self-worth and academic competence, activity restriction did not influence symptoms following the medical evaluation. These children tended to have low symptomatology at follow-up, regardless of the amount of activity restriction at the time of initial evaluation.
Positive attention also influenced symptom maintenance. Similar to the findings for activity restriction, the impact of positive attention varied as a function of children’s perceived self-worth and academic competence. Among children with lower self-worth or lower perceived academic competence, positive attention for symptoms predicted greater symptom maintenance following the clinic visit. This association may reflect social reinforcement of symptoms. Children who perceive themselves as lacking competence in normal daily roles may be especially vulnerable to the reinforcing impact of attention for their somatic symptoms. We expected that such attention would have little impact on symptom maintenance in children with greater perceived competence. Unexpectedly, however, attention for symptoms actually predicted a decrease in symptoms for children with higher self-worth or higher perceived academic competence. It may be that even during times of illness, these very capable children also receive attention for competent behavior not associated with the sick role. To the extent that alternative behaviors are reinforced and are incompatible with sick role behavior, the impact of positive attention on symptoms would be reduced.
Negative attention did not predict symptom decreases and therefore could not be regarded as “punishing” symptoms. Indeed, to the extent that children perceived others as ignoring or criticizing their symptoms, they exhibited greater symptom maintenance. This impact of negative attention was significantly greater for children with lower levels of perceived self-worth. Others have suggested that negative attention may predict symptoms indirectly—that is, by creating emotional distress, which, in turn, contributes to somatic symptoms (cf. Kerns et al., 1991). Children with lower self-worth may be particularly vulnerable to the impact of negative attention if they have difficulty generating alternative behavior that is rewarded with positive attention. Children with higher levels of self-worth, in contrast, may engage in alternative behavior when their symptom complaints are ignored or criticized by others.
As discussed, the data indicated that perceived academic competence played a role similar to that of global self-worth. In contrast, perceived social competence did not moderate the impact of social consequences on symptom maintenance, perhaps because Harter’s (1985) Social Competence scale focuses on peer relationships, whereas the SCP emphasized family more than peer attention to symptom complaints. Prior work has shown that children’s symptom complaints influence peer responses to them (Guite, Walker, Smith, & Garber, 2000). Future work might focus on the effects of positive and negative peer attention on children’s symptom maintenance.
A particular strength of the study was the use of a longitudinal design with statistical control for initial symptom levels in predicting symptoms at follow-up. Most previous research on the relation of social consequences to illness behavior has used cross-sectional data. Because RAP is an episodic condition, future research should include multiple data points over time in order to assess the duration of symptom maintenance.
This study focused on Caucasian children referred to a tertiary care setting for evaluation of recurrent abdominal pain. Additional work is needed to determine whether the findings generalize to children in primary care settings and to children of other ethnic groups. It is possible that gender differences, not observed in this sample, would be evident in those populations. The study is further limited by use of self-report measures. Although subjective perceptions of the consequences of illness are relevant in predicting future pain behavior, inclusion of objective measures of the social consequences of pain would help tease out the relative contribution of each to the development of chronic pain syndromes. Indeed, others have shown that the predictive effect of solicitous behavior on patients’ treadmill performance is greater when solicitous behavior is reported by the caregiver than by the patient (Lousberg, Schmidt, & Groenman, 1992). Finally, inclusion of objective measures of children’s competencies would help to determine whether perceived versus actual competence moderates the effect of social consequences on symptom maintenance.
A second aim of this study was to describe the development and initial validation of the SCP, a measure that assesses children’s perceptions of the frequency of various social consequences associated with their pain episodes. Factor analysis identified four distinct types of consequence that we labeled positive attention, activity restriction, negative attention, and privileges. The only other child-report measure of social consequences of pain, the IBES (Walker & Zeman, 1982) did not assess negative consequences and treated positive consequences as a single dimension. However, a recent study using a Dutch translation of the IBES (Bijttebier & Vertommen, 1999) found that positive responses assessed by the IBES reflected two distinct types of response—“Attention Consequences” (e.g., extra time with parents) and “Escape Consequences” (e.g., being relieved from activities and granted special privileges). Thus, three of the factors on the SCP—positive attention, activity restriction, and privileges—appear to reflect constructs imbedded in the IBES. Additional research is needed to replicate the factor structure of the SCP, examine its test-retest reliability, and further explore its construct validity, particularly the relation of the SCP to observer ratings of social consequences associated with children’s pain episodes.
Results of this study have implications for the evaluation and treatment of children with RAP and other chronic or recurrent pain conditions. In evaluating the role of social consequences in reinforcing children’s symptoms, one must consider the context of children’s progress in normative developmental tasks. Children’s satisfaction with their performance on these tasks may influence the attractiveness or reinforcement value of the sick role. Thus, social consequences associated with sick role behavior, such as staying home from school, may reinforce symptoms in some children but may in fact be aversive for others. In related work, Radley and Greene (1987) postulated that secondary gain occurs when individuals both define themselves in terms of illness and withdraw from participation in normal roles. Children who view themselves as inadequate in normal childhood roles may be most likely to define themselves in terms of their illness. The sick role offers them a legitimate alternative to roles at which they perceive themselves as failing. When attention and relief from responsibility accompany their sick role behavior, symptoms and disability are likely to be reinforced and maintained long after any organic disease processes have resolved. In these cases, it is important that treatment include efforts to develop children’s competencies and to reward their participation in more appropriate roles.
In treating children with chronic or recurrent pain conditions, the clinician must broaden the family’s focus beyond concern for the child’s physical health to consideration of the whole child, including positive health associated with various competencies (cf. Seeman, 1989). Even very protective parents who are reluctant to limit attention to their children’s symptoms may agree to reward their children’s success in activities not associated with the sick role. Thus, the family may be enlisted in promoting children’s competencies so that the relative attractiveness of the sick role is gradually reduced.
Acknowledgments
This study was supported by a grant to the investigators from the National Institute for Child Health and Development (HD23264) and by a core grant (HD15052) to the John F. Kennedy Center, Vanderbilt University.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3. Washington, DC: Author; 1987. rev. [Google Scholar]
- Apley J. The child with abdominal pains. London: Blackwell; 1975. [Google Scholar]
- Bijttbier P, Vertommen H. Antecedents, concomitants and consequences of pediatric headache: Confirmatory construct validation of two parent-report scales. Journal of Behavioral Medicine. 1999;22:437–456. doi: 10.1023/a:1018605423614. [DOI] [PubMed] [Google Scholar]
- Blount RL, Corbin SM, Sturges JW, Wolfe VV, Prater JM, James LD. The relationship between adults’ behavior and child coping and distress during BMA/LP procedures: A sequential analysis. Behavior Therapy. 1989;20:585–601. [Google Scholar]
- Craig KD. Modeling and social learning factors in chronic pain. In: Bonica J, editor. Advances in pain research. Vol. 5. New York: Raven Press; 1978. pp. 813–827. [Google Scholar]
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist. Behavioral Science. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- Erikson E. Childhood and society. 2. New York: Norton; 1964. [Google Scholar]
- Fishbain DA. Secondary gain concept: Definition problems and its abuse in medical practice. American Pain Society Journal. 1994;3:264–273. [Google Scholar]
- Fishbain DA, Rosomoff HL, Cutler RB, Rosomoff RS. Secondary gain concept: A review of the scientific evidence. Clinical Journal of Pain. 1995;11:6–21. [PubMed] [Google Scholar]
- Fordyce WE. The cognitive/behavioral perspective on clinical pain. In: Loeser JD, Egan KJ, editors. Managing the chronic pain patient. New York: Raven Press; 1989. pp. 51–64. [Google Scholar]
- Freud S. Introductory lectures on psychoanalysis (1917) Vol. 16. London: Hogarth Press; 1959. [Google Scholar]
- Garber J, Walker LS, Zeman J. Somatization symptoms in a community sample of children and adolescents: Further validation of the Children’s Somatization Inventory. Psychological Assessment. 1991;3:588–595. [Google Scholar]
- Gidron Y, McGrath PJ, Goodday R. The physical and psychosocial predictors of adolescents’ recovery from oral surgery. Journal of Behavioral Medicine. 1995;18:385–399. doi: 10.1007/BF01857662. [DOI] [PubMed] [Google Scholar]
- Guite JW, Walker LS, Smith CA, Garber J. Children’s perceptions of peers with somatic symptoms: The impact of gender, stress, and illness. Journal of Pediatric Psychology. 2000;25:125–135. doi: 10.1093/jpepsy/25.3.125. [DOI] [PubMed] [Google Scholar]
- Harter S. Manual for the Self-Perception Profile for Children. Denver, CO: University of Denver; 1985. [Google Scholar]
- Hollingshead AB. Working paper. Department of Sociology, Yale University; 1975. Four-factor index of social status. [Google Scholar]
- Kerns RD, Southwick S, Giller EL, Haythornthwaite JA, Jacob MC, Rosenberg R. The relationship between reports of pain-related social interactions and expressions of pain and affective distress. Behavior Therapy. 1991;22:101–111. [Google Scholar]
- Lethem J, Slade PD, Troup JDG, Bentley G. Outline of a fear-avoidance model of exaggerated pain perception—I. Behaviour Research and Therapy. 1983;21:401–418. doi: 10.1016/0005-7967(83)90009-8. [DOI] [PubMed] [Google Scholar]
- Lousberg R, Schmidt AJ, Groenman NH. The relationship between spouse solicitousness and pain behavior: Searching for more experimental evidence. Pain. 1992;51:75–79. doi: 10.1016/0304-3959(92)90011-Y. [DOI] [PubMed] [Google Scholar]
- McGrath PA. Pain in children: Nature, assessment, and treatment. New York: Guilford Press; 1990. [Google Scholar]
- Radley A, Greene R. Illness as adjustment: A methodology and conceptual framework. Sociology of Health and Illness. 1987;9:179–207. [Google Scholar]
- Seeman J. Toward a model of positive health. American Psychologist. 1989;44:1099–1109. doi: 10.1037//0003-066x.44.8.1099. [DOI] [PubMed] [Google Scholar]
- von Baeyer CL, Walker LS. Children with recurrent abdominal pain: Issues in the selection and description of research participants. Journal of Developmental and Behavioral Pediatrics. 1999;20:307–313. doi: 10.1097/00004703-199910000-00001. [DOI] [PubMed] [Google Scholar]
- Walker LS. The evolution of research on recurrent abdominal pain: History, assumptions, and new directions. In: McGrath PJ, Finley GA, editors. Chronic and recurrent pain in children and adolescents. Seattle, WA: International Association for the Study of Pain; 1999. pp. 141–172. [Google Scholar]
- Walker LS, Garber J, Greene JW. Somatization symptoms in pediatric abdominal pain patients: Relation to chronicity of abdominal pain and parent somatization. Journal of Abnormal Child Psychology. 1991;19:379–394. doi: 10.1007/BF00919084. [DOI] [PubMed] [Google Scholar]
- Walker LS, Garber J, Greene JW. Psychosocial characteristics of recurrent childhood pain: A comparison of children with recurrent abdominal pain, organic illness, and psychiatric disorders. Journal of Abnormal Psychology. 1993;102:248–258. doi: 10.1037//0021-843x.102.2.248. [DOI] [PubMed] [Google Scholar]
- Walker LS, Garber J, Van Slyke DA. Do parents excuse the misbehavior of children with physical or emotional symptoms? An investigation of the pediatric sick role. Journal of Pediatric Psychology. 1995;20:329–345. doi: 10.1093/jpepsy/20.3.329. [DOI] [PubMed] [Google Scholar]
- Walker LS, Zeman JL. Parental response to child illness behavior. Journal of Pediatric Psychology. 1993;17:49–71. doi: 10.1093/jpepsy/17.1.49. [DOI] [PubMed] [Google Scholar]
- Whitehead WE, Busch CM, Heller BR, Costa PT. Social learning influences on menstrual symptoms and illness behavior. Health Psychology. 1986;5:13–23. doi: 10.1037//0278-6133.5.1.13. [DOI] [PubMed] [Google Scholar]
- Whitehead WE, Winget C, Fedoravicius AS, Wooley S, Blackwell B. Learned illness behavior in patients with irritable bowel syndrome and peptic ulcer. Digestive Diseases and Sciences. 1982;27:202–208. doi: 10.1007/BF01296915. [DOI] [PubMed] [Google Scholar]
- Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment. 1990;55:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]


