Abstract
Background
Geographic location represents an ecological measure of HIV status and is a strong predictor of HIV prevalence. Given the complex nature of location effects, there is limited understanding of their impact on policies to reduce HIV prevalence.
Methods
Participants were 3,949 and 10,874 respondents from two consecutive Zambia Demographic and Health Surveys from 2001/7 (mean age for men and women: 30.3 and 27.7 years, HIV prevalence 14.3% in 2001/2002; 30.3 and 28.0 years, HIV prevalence of 14.7% in 2007). A Bayesian geo-additive mixed model based on Markov Chain Monte Carlo techniques was used to map the change in the spatial distribution of HIV/AIDS prevalence at the provincial level during the six-year period, accounting for important risk factors.
Findings
Overall HIV/AIDS prevalence changed little over the 6-year period, but the mapping of residual spatial effects at the provincial level suggested different regional patterns. A pronounced change in odds ratios in Lusaka and Copperbelt provinces in 2001/2 and in Lusaka and Central provinces in 2007 were observed following adjustment for spatial autocorrelation. Western province went from a lower prevalence area in 2001 (13.4%) to a higher prevalence area in 2007 (17.3%). Southern province went from the highest prevalence area in 2001 (17.3%) to a lower prevalence area in 2007 (15.9%).
Interpretation
Findings from two consecutive surveys corroborate the Zambian government’s effort to achieve MDG 6. The novel finding of increased prevalence in Western province warrants further investigation. Spatially-adjusted provincial-level HIV/AIDS prevalence maps are a useful tool for informing policies to achieve MDG 6 in Zambia.
Keywords: MDG 6, HIV prevalence, geographic location, spatial autocorrelation
INTRODUCTION
The importance of monitoring HIV prevalence to assess the impact of HIV interventions in a population is widely recognized. In 2000, the United Nations’ Millennium Summit identified the reduction of HIV prevalence as one of the eight fundamental goals for furthering human development. As part of Millennium Developing Goal (MDG) 6, the UN established a target of combating HIV/AIDS, malaria and other diseases by halting and beginning to reverse the prevalence of HIV/AIDS and other major diseases by 2015 for all national and regional populations. Monitoring HIV prevalence using national averages can mask within-country variability and thereby lead to the design and implementation of generic policies and interventions that may have limited impact at the local level.
An interesting case is Zambia, where aggregated national HIV prevalence conceals important spatial variation at the provincial level. For example, in the 2007 Zambian Demographic and Health Survey (2007 ZDHS), the national prevalence of HIV was 14.7% (unweighted data) but ranged from 9% (Northern Province) to 20% (Lusaka province). Also, between 2001 and 2007, while the national HIV prevalence changed only slightly, it increased in Western province from 13% to 17% (Central Statistical Office, 2009). Prevalence rates also vary significantly by sex and age. Women are more vulnerable to HIV infection than their male counterparts. An estimated 16.1% of females are HIV positive, compared to 12.3% of males, and prevalence in women aged 15–24 years (8.8%) is double that of men (4.4%) (Central Statistical Office, 2009).
Effective planning and delivery of HIV prevention programs depends on an understanding of where new infections are occurring and on the behaviours associated with those infections. Thailand provides an example of how comprehensive prevention strategies aimed at the main modes of transmission in the early years of the epidemic, sex work and injecting drug use (IDU), led to significant reductions in incidence by the mid 1990s (Gouws et al., 2006; WHO, 2005). Unfortunately such success stories are few, and often the response in a country does not adequately match the epidemic patterns, resulting in missed opportunities to address those risk factors that drive HIV epidemics.
Policy overview and status of HIV in Zambia since 2001
The Government of the Republic of Zambia (GRZ) has deployed a multisectoral response to HIV/AIDS by adopting one national AIDS strategic framework 2006–2010; one national coordinating body, the National HIV/AIDS/STI/TB Council (NAC) reporting to a cabinet committee on AIDS with decentralized structures; and one monitoring and evaluation system. The GRZ has integrated HIV into the development agenda with the objective: To halt and begin to reverse the spread of HIV and mitigate its impact. The response has aimed to prevent viral transmission, care for those infected and their relatives/dependents, and reduce the personal, social and economic impact of AIDS (Garbus, 2003). Prevention strategies include workplace programmes, programmes for prevention of mother-to-child transmission (PMTCT), blood safety measures, post-exposure prophylaxis (injection safety measures), and efforts to reduce stigma and discrimination.
Since 2002, the GRZ has also undertaken an ambitious antiretroviral (ARV) treatment programme. It costs as much as US$300 to buy a month’s supply of ARVs on the open market. Government-sponsored drugs cost US$9 per month after an initial payment of US$15 for testing and counselling. With an HIV prevalence rate of 14% and a population of nearly 13 million, of whom nearly 64% live below the poverty line of US$1 a day, scaling-up the provision of treatment and reducing the number of new infections remains a formidable challenge.
Nevertheless, the GRZ has made significant progress: a reduction in MTCT from 30% to 12.4%; 100% coverage by blood safety programmes; peer programmes effectively promoting delayed sexual debut; sustained change in perception through behavior change communication (BCC); effective condom promotion for casual sex and among the most at-risk groups; and an increase in HIV screening from 29.7% in 2006 to 50% in 2009. The number of screening sites in all 72 districts increased from 67 in 2005 to 307 in 2006, 678 in 2007, and 937 in 2009; 39% of persons co-infected with HIV and TB have received treatment; 15% of women and men aged 15–49 have received an HIV test in the last 12 months and know their results; and over 1,500 testing sites have been established nationwide. Also, delivery of ARVs has been impressive (15% coverage achieved in 2005, 50% in 2007, with a target of 60% in 2010) (National HIV/AIDS/STI/TB Council, 2010). In addition to MTCT and behaviour change communication programmes, the government has set up an AIDS fund to ensure that these programmes are sustained. Given this backdrop and the apparent stabilization of overall HIV prevalence1 (14.3% in 2001/2002 and 14.7% in 2007, unweighted data), our aim is to investigate spatial variation in HIV prevalence between two successive ZDHS surveys, controlling for important demographic factors.
MATERIAL AND METHODS
The Demographic and Health Survey (DHS), funded by the United States Agency for International Development (USAID), is a well-established source of reliable population level data with a substantial focus on knowledge of HIV/AIDS and sexual behaviour. The objectives, organisation, sample design, and questionnaires used in the two ZDHS surveys are described elsewhere (Central Statistical Office, 2004 and 2009). Briefly, a random probability sample of women aged 15–49 and men aged 15–59 was selected in both surveys. For the 2001/2 survey, approximately 5,000 respondents (54.6% female) were asked to give blood for syphilis and HIV testing, and the 2007 survey used a sample of 11,138 (52.5% female). Samples for HIV testing were dried blood spots on a filter paper card taken from a venous blood specimen. A three-stage testing procedure was used with 10% of the negative samples retested and discordant results tested by Western Blot. In this study, we have linked HIV status to a very limited number of demographic variables.
Statistical Analysis
To account for spatial autocorrelation of HIV infection in Zambia, we applied a unified approach by exploring spatial patterns in the prevalence of HIV infection and possible nonlinear effects within a simultaneous, coherent regression framework using a geo-additive semi-parametric mixed model. The model employed a fully Bayesian approach using Markov Chain Monte Carlo (MCMC) techniques for inference and model checking (Fahrmeir and Lang, 2001; Kandala et al., 2008). The response variable is defined as yi=1 if HIV sero-positive and yi=0 otherwise. The standard measure of effect is the posterior odds ratio (OR). Although this estimation process is used less frequently in the literature, the estimated posterior odds ratios (ORs) produced can be interpreted as similar to those of ordinary logistic models. Please refer to Appendix 1 for a detailed explanation of the statistical methods.
The analysis was carried out using version 0.9 of the BayesX software package (Brezger et al., 2005), which permits Bayesian inference based on Markov chain Monte Carlo (MCMC) simulation techniques. The statistical significance of apparent associations between potential risk factors and the prevalence of HIV/AIDS was explored in chi-square and Mann–Whitney U-tests, as appropriate. Multivariate analysis was used to evaluate the significance of the posterior OR determined for the fixed, non-linear effects and spatial effects. A P-value of <0.05 was considered indicative of a statistically significant difference.
RESULTS
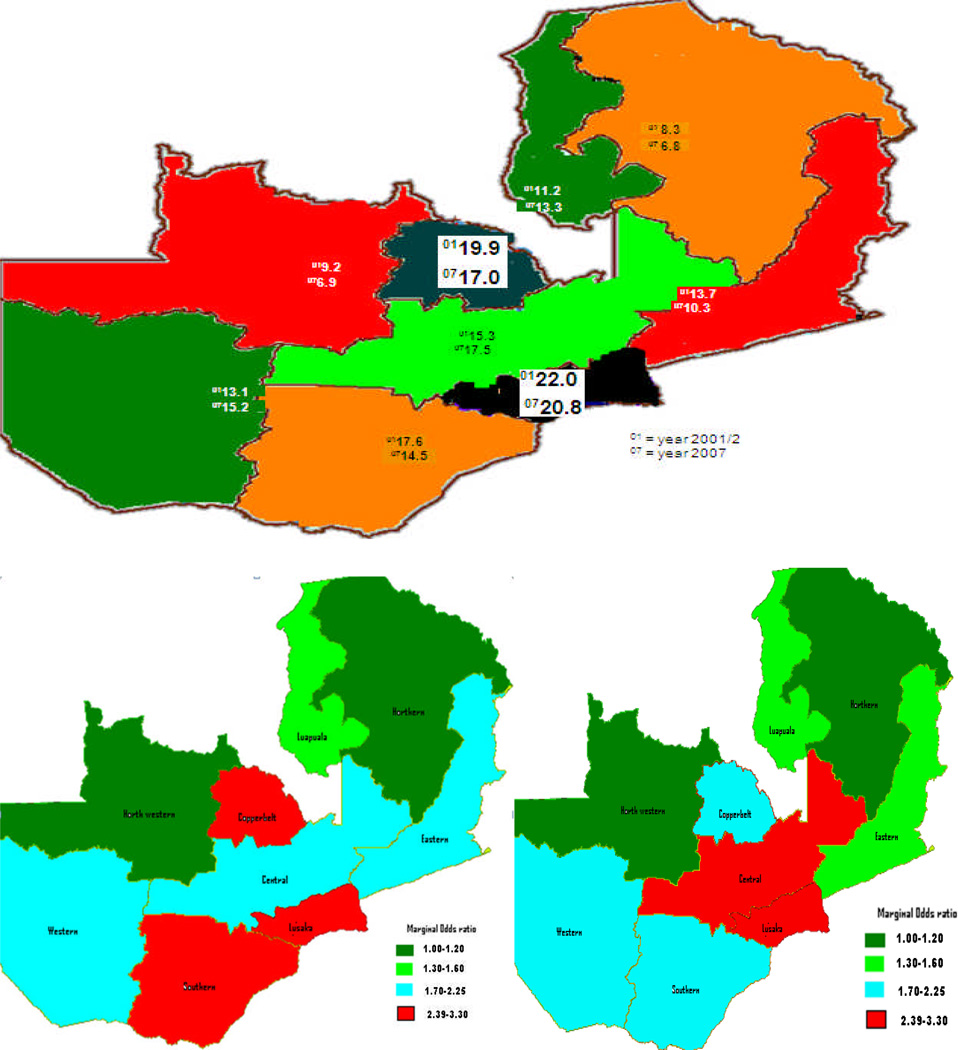
Table 1 shows the prevalence of HIV infection by age, gender, and region, unadjusted marginal odds ratios, and adjusted posterior odds ratios. The two survey populations are comparable for the selected variables in terms of the overall HIV prevalence (14.3% in 2001/2002 and 14.7% in 2007), higher prevalence among females, and lower prevalence in rural areas. The mean age for men was slightly higher than that for women in both the 2001/2 ZDHS (30.3 vs. 27.7 years) and the 2007 ZDHS (30.3 vs. 28.0 years) as expected from the sample strategy. Unadjusted marginal odds ratios indicate that in 2001/2002 the highest HIV prevalence was in Lusaka [OR & 95% CI: 3.29 (2.27, 4.76)] and Copperbelt [OR & 95% CI: 2.87 (1.99, 4.13)] provinces, followed by Southern, Central, Eastern, Western, and Luapula provinces, with the lowest prevalence in Northwestern and Northern provinces. In 2007, the highest prevalence was in Lusaka [OR & 95% CI: 2.62 (2.06, 3.32)] and Central [OR & 95% CI: 2.39 (1.85, 3.10)] provinces, followed by Western, Copperbelt, Southern, Luapula, and Eastern provinces, and the lowest prevalence was again in Northwestern and Northern provinces. Copperbelt province, a highly urbanised area, had among the highest prevalence rates in 2001/2002 but not in 2007. Surprisingly, Western province, which had a lower HIV prevalence (13.4%) in 2001/2002, had among the highest HIV prevalence rates (17.3%) in 2007.
Table 1.
Prevalence and crude marginal odds ratio of HIV/AIDS infection* by baseline characteristics (ZDHS 2001 & 2007).
| HIV DHS 2001: 3,949 | HIV DHS 2007:11,138 | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Cases | P-value** | Marginal OR & 95%CI*** |
Posterior OR & 95% CI† |
Cases | P-value** | Marginal OR & 95%CI*** |
Posterior OR & 95% CI |
| Number | 565(14.3) | 1596(14.7) | ||||||
| Gender | ||||||||
| Male | 212(11.7) | 1.00 | 649(12.6) | 1.00 | ||||
| Female | 353(16.6) | <0.001 | 1.59(1.32, 1.89) | 353(16.6) | <0.001 | 1.43(1.43, 1.59) | ||
| Place of residence | ||||||||
| Urban | 290(23.0) | 2.73(2.13, 3.28) | 934(19.8) | 2.35(2.11, 2.63) | ||||
| Rural | 275(10.2) | <0.001 | 1.00 | 662(10.8) | <0.001 | 1.00 | ||
| Age at diagnosis | ||||||||
| <24 years | 122(7.5) | See figure 3a | 299(6.9) | See figure 3a | ||||
| 25 & 35 years | 273(21.2) | 728(19.6) | ||||||
| 36 &49 years | 159(17.7) | 518(21.2) | ||||||
| 50 & 59 years | 11(8.0) | <0.001 | 51(12.6) | <0.001 | ||||
| Region of residence*** | ||||||||
| Central(4)(2) | 85(15.1) | 2.06(1.42, 2.99) | 1.22(0.97, 1.55) | 177(18.4) | 2.39(1.85, 3.10) | 1.39(1.06, 1.82) | ||
| Copperbelt(2)(4) | 99(19.8) | 2.87(1.99,4.13) | 1.02(0.74, 1.43) | 196(16.7) | 2.13(1.65, 2.74) | 0.99(0.73, 1.31) | ||
| Eastern(5)(7) | 53(13.6) | 1.83(1.21, 2.76) | 1.11(0.84, 1.43) | 180(11.8) | 1.42(1.10, 1.83) | 0.91(0.68, 1.13) | ||
| Luapula(7)(6) | 37(11.1) | 1.45(0.92, 2.27) | 0.86(0.61, 1.17) | 155(14.5) | 1.80(1.38, 2.34) | 1.03(0.83, 1.28) | ||
| Lusaka(1)(1) | 95(22.1) | 3.29(2.27, 4.76) | 1.09(0.78, 1.41) | 297(19.8) | 2.62(2.06, 3.32) | 1.29(0.99, 1.56) | ||
| Northern(9)(9) | 49(7.9) | 1.00 | 0.69(0.52, 0.87) | 104(8.6) | 1.00 | 0.61(0.46, 0.81) | ||
| North-western(8)(8) | 41(9.3) | 1.18(0.77, 1.82) | 0.81(0.60, 1.03) | 87(8.6) | 1.01(0.75, 1.35) | 0.61(0.44, 0.85) | ||
| Southern(3)(5) | 69(17.3) | 2.43(1.64, 3.59) | 1.33(1.06, 1.91) | 202(15.9) | 2.01(1.56, 2.58) | 1.25(0.90, 1.60) | ||
| Western(6)(3) | 37(13.4) | <0.001 | 1.79(1.14, 2.81) | 1.13(0.82, 1.57) | 198(17.3) | <0.001 | 2.23(1.73, 2.87) | 1.34(1.01, 1.78) |
Data are expressed as number (percentages) of cases that are HIV positive.
P-value comparison across HIV positive and negative cases using the chi-squared test for categorical variables.
Crude unadjusted marginal odds ratio (OR) obtained from the standard logistic regression model and ranked from the highest to the lowest OR. The Northern province is taken as reference because its low HIV prevalence in both surveys.
Rank of marginal OR in 2001: Lusaka(1), Copperbelt(2), Southern(3), Central(4), Eastern(5), Western(6), Luapula(7), Northwestern(8), Northern(9).
Rank of marginal OR in 2007: Lusaka(1), Central(2), Western(3), Copperbelt(4), Southern(5), Luapula(6), Eastern(7), Northwestern(8), Northern(9).
Spatially adjusted posterior odds ratio (OR) obtained from the Bayesian geo-additive regression model after controlling for nonlinear effect of age, categorical variables and the province of residence (spatial effects).
The pattern of HIV prevalence by province differed markedly between the two surveys, though there was consistently higher prevalence in Lusaka and lower prevalence in Northern Province (Figure 1). The marginal odds ratios of HIV prevalence at the provincial level shown in Figure 1 (bottom) indicate that the two provinces in which HIV prevalence is lowest and below the national prevalence in both surveys are Northern and Northwestern provinces. In 2001/2, the four provinces in which HIV prevalence rates are higher than the national average are Lusaka, Copperbelt, Central and Southern provinces. In 2007, the four provinces with HIV prevalence rates higher than the national average are Lusaka, Copperbelt, Central, and Western provinces. Copperbelt and Southern are no longer among the provinces with the highest marginal odds ratios, which in 2007 are Lusaka and Central.
Figure 1.
Prevalence of HIV in Zambia by province and marginal odds ratios of HIV prevalence (bottom) 2001/2-2007 DHS
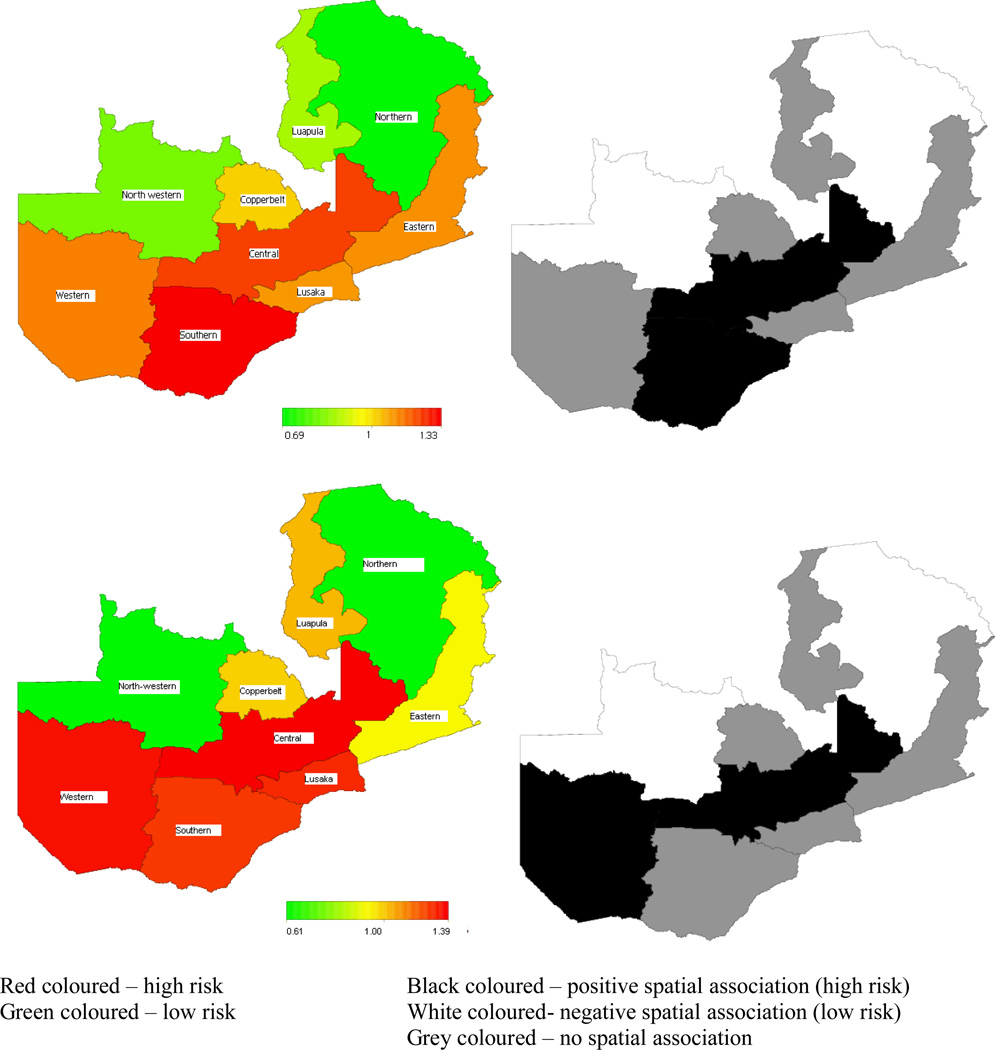
In multivariable Bayesian geo-additive regression analyses, gender (female) [OR & 95% Credible Region (CR): 1.59(1.32, 1.89) in 2001 and OR & 95% CR: 1.43(1.43, 1.59) in 2007] and urban residence [OR & 95% CR: 2.73(2.13, 3.28) in 2001 and OR & 95% CR: 2.35(2.11, 2.63) in 2007] were consistently associated with higher HIV status in both samples. Moreover, age at HIV diagnosis (as a continuous variable) and province of residence (as a spatial variable) remained significant risk factors in both surveys. Overall, results of the 2001/2 ZDHS (Figure 2) show that after accounting for spatial auto-correlation in the data, the provinces with the highest HIV prevalence included Central and Southern, while Lusaka and Copperbelt no longer ranked among the highest prevalence regions as suggested by the marginal OR (Figure 1). Six years later (Figure 2 bottom), after accounting for spatial auto-correlation, the highest risk provinces included Central and Western but not Lusaka.
Figure 2.
Total residual spatial provincial effects (left) and 80% posterior probability map (right) of the risk of HIV infection in Zambia (ZDHS 2001 and 2007)
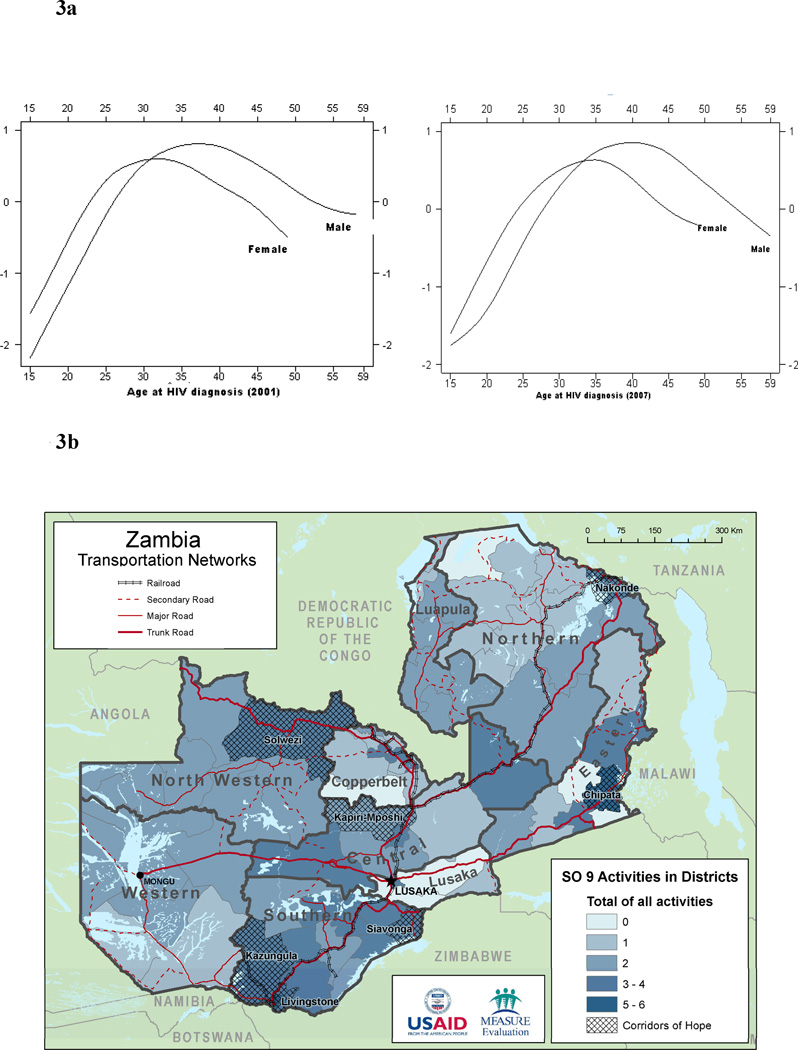
Figure 3 shows an inverse U-shape association and a bell shaped non-linear relationship between the probability of HIV infection and age at HIV diagnosis. In 2001/2, the probability of infection at age 15 differs by sex, with men starting at lowest probability, but in 2007 this gap appears to have decreased, with men approaching the same probability as women. At all other ages, the two surveys show agreement in the pattern of the probability of infection. A watershed is present between 30–34 years of age, when both men and women have the highest observed probability of HIV infection. Before age 30, this probability rises quickly as age increases. Beyond age 34 there is a declining probability of infection, although the variation in probability increases rapidly at the same time as age continues to increase.
Figure 3.
a Estimated nonlinear association of the risk of HIV/AIDS and age at the time of HIV/AIDS diagnosis, ZDHS2001 and 2007.
b. Major Zambia transport corridors and number of USAID Strategic Objective 9 Activities by District,* with Corridors of Hope Implementation Districts Highlighted.
*Data Source: USAID | Zambia Multi-sector HIV/AIDS activities. Available: http://www.usaid.gov/zm/maps/so_9activities.pdf.
DISCUSSION
Our novel and most important findings are illustrated in the contrast between Figures 1 and 2. We observed a pronounced change in the odd ratios in Lusaka and Copperbelt for the 2001/2 ZDHS and Lusaka and Central for the 2007 ZDHS following adjustment of the geographical location (spatial auto-correlation) arising from the population mobility (migration), and the younger age structure of the urban population‥ Also, Western province, which was among the lowest prevalence areas in 2001/2002, changed to one of the highest prevalence areas in 2007. And Southern province, which was among the highest prevalence areas in 2001/2002, changed to one of the lowest prevalence areas in 2007. Copperbelt was no longer among the provinces with the highest marginal odds ratios in both surveys.
We also observed a rapid increase in sero-prevalence among men aged 15. This finding is unlikely due to earlier sexual debut: respondents aged 15–19 reporting sex before age 15 declined from 27% to 16% between the 2001/2 and 2007 ZDHS (Central Statistical Office, 2004 and 2009). A more likely explanation is riskier intercourse among males. The percentage of adolescent men aged 15–19 reporting using a condom with their most recent sexual partner declined from 35% in 2000 to 31% in 2009, and only 38% reported that they could get condoms on their own (Central Statistical Office, 2010).
That the highest probability of being HIV-infected was observed among respondents residing in Western and Central provinces could be explained in part by the mobility of the Zambian population along transportation routes, acknowledged by the World Bank and other leading institutions as a major vector in the spread of HIV (World Bank, 2008; World Bank, 2009). Truck drivers, seasonal workers and commercial sex workers all comingle along these routes, often moving from less developed/urbanized areas to more developed regions with greater economic opportunities. With an unemployment rate exceeding 50% and 68% of Zambians living in poverty, many young women have little choice but to become commercial sex-workers, with HIV rates documented at 65% (UNAIDS/WHO, 2008; Biennial Report to UNGASS, 2010). Often they are denied the kinds of prevention services available to non-sex workers (Graham, 2009). By contrast, the rapid decrease in prevalence rates in Southern province could possibly reflect the heavy concentration of USAID Strategic Objective 9 (SO9) funding and activities in Southern province, particularly along the major transport route between Livingstone and Lusaka (USAID Zambia S09 Activities, 2010) (Figure 3b bottom).
As a President’s Emergency Plan for AIDS Relief (PEPFAR) focus country, Zambia has benefited from high levels of external funding, rising from US$6 in 2003 to US$10 per capita in 2006. During this period, the proportion of external funding rose from 70% to 74%, with PEPFAR the largest funder (50%), followed by the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM) (16%) and the World Bank MAP program (Multi-Country HIV/AIDS Program for Africa), which ended in 2008 (Global HIV/AIDS Initiatives Network, 2009). GFATM has allocated Zambia USD 42.5 million to counter HIV/AIDS. This major influx of donor funding has supported a variety of programmes during this period, but it is difficult if not impossible to precisely inventory these activities. The USAID Zambia Mission publically details the specific HIV/AIDS Multi-sector Response activities funded through PEPFAR listed in Table 2 (USAID Zambia Mission, 2010). Funding for these combined activities was roughly USD 100 million, or nearly one sixth of the US government total of USD 620 million for the period 2003 to 2008, which constituted approximately 60% of all donors funding to Zambia (USAID Zambia S09 Activities, 2010). Of the USD 270 million approved by PEPFAR for Zambia in fiscal year 2009, approximately 28% was earmarked for prevention activities (U.S. State Department, 2010).
Table 2.
| Program | Years | USD (million) | Location | Services |
|---|---|---|---|---|
| Reaching HIV/AIDS Affected People with Integrated Development and Support (RAPIDS) | 2004–2006 | 57.5 | 53 districts throughout Zambia | Home- and community-based care for people living with AIDS, care and support for OVCs, youth livelihood and promotion of abstinence among youth, and household resilience and improved food security for those affected by HIV/AIDS |
| Support to the HIV/AIDS Response in Zambia (SHARe) | 2004–2010 | 21.0 | 61 districts throughout Zambia | Expands access to HIV prevention, treatment and services through workplace programs; strengthen the capacity of coordinating bodies and faith-based, community-based and other local organizations, to plan, implement, monitor and evaluate HIV/AIDS activities; and strengthen the policy and regulatory environment to protect PLWHA and those affected by HIV/AIDS |
| BizAIDS | 2005–2008 | 1.6 | Small businesses throughout Zambia | Trains participating businesses in HIV/AIDS prevention, mitigation, and care and support; provides information to business owners and their employees on how they can protect themselves from contracting HIV, plan their business in light of HIV/AIDS, and on how they can access legal services to deal with the challenges brought by HIV/AIDS in the business operations; promotes HIV CT among owners and employees of micro and small businesses; and trains local trainers through the District Business Associations |
| Scaling Up Community Care to Enhance Social Safety Nets (SUCCESS) "RETURN TO LIFE" | 2006–2008 | 9.8 | 30 districts throughout Zambia | Palliative care focus. Strengthens services offered and logistical support to faith-based hospices and is fostering linkages with other USG funded programs for support to OVCs and for ART |
| AFRICA KIDSAFE (AKS) | 2004–2007 | 1.7 | Urban regions throughout Zambia, began in Lusaka, Livingstone, and Copperbelt Provinces | Consolidates and expands a safety net of NGOs and CBOs that work with communities and families to effectively meet the immediate and long-term needs of street and at-risk children throughout Zambia |
| The Zambian Corridors of Hope HIV/AIDS Prevention Initiative (COH II) | 2006–2009 | 11.0 | Livingstone, Kazungula, Chipata, Katete, Kapiri Mposhi, Chirundu, and Ndola | Comprehensive HIV/AIDS prevention project concentrated on seven of the highest HIV prevalence border and transport corridor areas in Zambia, delivered by 3 Zambian NGOs. Collaboration with the District Health Management Teams, District AIDS Task Forces, and other service delivery teams. Targets residents of border and corridor communities and high-risk populations and includes counseling and testing (CT) services, STI screening and treatment, condom social marketing, interpersonal counseling for behavior change, outreach work, and youth prevention activities for in- and out-of-school youth |
In addition to the programs listed in this table, USAID Zambia coordinates numerous centrally-funded providing care and support to Orphans and Vulnerable Children (OVC): World Concern, Opportunity International, CRS CHAMP, Christian Aid, FHI FABRICS, Hope Worldwide, Hope for African Children Initiative, and PCI BELONG. In addition, five New Partnership Initiatives have begun implementation: Kara Counseling, Nazarene Compassionate Ministries, Luapula Foundation, Catholic Missions Medical Board, and Mothers2Mothers (USAID Zambia Mission, 2010).
The USAID program most relevant to the spread of HIV along transport corridors, the 3-year (2006–2009), USD 11 million Corridors of Hope II (COH II) program, has neglected the major east-west corridor between Lusaka and Mongu at the western terminus of the major road into Western province (see map, Figure 3b). This program became fully implemented in 2007 in seven Zambian high-prevalence border and transport districts: Livingstone, Kazungula, Chipata, Kapiri Mposhi, Nakonde, Solwezi, and Siavonga (Chirundu) (COH II Program, 2008). In 2009 the Corridors of Hope III (COH III) program was proposed to continue and potentially expand the activities of CHO II, with three basic elements focusing on prevention of sexual transmission—condoms and other prevention, abstinence-based (AB) activities, and counselling and testing (CT) services. Funded at close to USD 25 million over five years and potentially adding additional sites in years 3–5, COH III will continue to provide services in the same seven districts as COH II (COH III Program, 2009). Our findings suggest that this program should be expanded into transport towns along the east-west corridor into Western province.
Border migration from Angola into Western province is another possible explanation for the increase in Western province rates, but Angola has the lowest HIV prevalence rate (2.5%) in continental southern Africa, while countries to the south (Namibia, 15%; Botswana, 24%; and Zimbabwe, 15%) have higher rates (UNAIDS/WHO, 2010). The Trans-Caprivi highway links landlocked Botswana, Zambia and Zimbabwe with the deepwater port of Walvis Bay in Namibia, and is thus a very active transport zone/border crossing for truckers. The Caprivi region of Namibia along this route has the highest prevalence of HIV in Namibia, estimated at over 40% (Afrol News, 2006). Also, declining prevalence in Southern province could be attributed to increased AIDS-related mortality, but provincial-level aids-specific mortality data are not available to test this hypothesis.
Also, the primary drivers of the Zambian epidemic are not necessarily the high-risk populations noted above, although they certainly contribute a disproportionate share of the cases via multiple, concurrent, geographically-dispersed sexual partnerships. By far, the largest source of new infections (over 70% of the total) is casual heterosexual sex (National HIV/AIDS/STI/TB Council, 2010). The greatest prevention impact would therefore be expected for programmes broadly targeting this much larger risk group.
A major limitation of the findings was discussed previously (Kandala et al., 2008; Garcia-Calleja et. al., 2006). Residual spatial distributions of risk of HIV infection might be influenced by model variable selection. Urban/rural location and province are both chosen as explanatory factors in the geo-additive regression model. However, it is possible that place of residence (urban/rural location) shared the effect of geographic distribution of the regions (provinces), especially in Lusaka and Copperbelt, as these areas are highly urbanized and almost one-half of the country’s population is concentrated in these few urban zones. It is worth investigating this issue further if one has several factors included in HIV/AIDS studies. It was not possible to confirm or disprove the above statement in our study since we had only a limited set of variables (province, urban/rural residence and gender).
It is worth mentioning some of the advantages of the approach described above over more conventional approaches like regression models with fixed or random province effects; or standard 2-level multilevel modelling with unstructured spatial effects. Most studies of HIV/AIDS prevalence astonishingly neglect the geographic location, spatial autocorrelation, and nonlinear effects of covariates, which in our view is likely to result in misleading conclusions regarding the prevalence of the disease. Additionally, and more importantly, the impact of this neglect is an underestimation of standard errors of the fixed effects which in turn inflates the apparent significance of the estimates. Our analysis included this correlation structure and accounted for the dependence of neighbouring provinces in the model. Since ZDHS data are based on a random sample within communities, the structured component introduced here allows us to ‘borrow strength’ from neighbouring clusters in order to cope with the sample variation of province effect and obtain estimates for areas that may have had inadequate sample sizes or be unsampled. This gives more reliable estimates of the fixed effect standard errors. A failure to take into account the posterior uncertainty in the spatial location (province) would overestimate the precision of the prediction of HIV prevalence in regions with inadequate sample size. Controlling for important risk factors such as geographical location (spatial auto-correlation) arising from the population mobility (migration), age structure of the population, and gender gave estimates of prevalence that are statistically robust.
CONCLUSION
Findings from the two consecutive surveys corroborate the Zambian government’s efforts to slow HIV prevalence and achieve MDG 6. However, it is possible that these efforts are variable across provinces, and this variability is reflected in the progress made in reducing HIV prevalence by province in our study. Northern and Northwestern provinces consistently remain the lowest HIV risk areas and Central province is consistently a highest-risk area throughout the six year review. However, Southern province went from the highest risk area in 2001/2002 to among the lowest risk areas in 2007, while Western province went from among the lowest risk areas in 2001/2002 to among the highest risk areas in 2007, a novel finding which warrants further investigation. The HIV/AIDS prevalence maps generated here could be useful for intervention policies to achieve MDG 6 in Zambia.
Finally, given the cross-sectional nature of our data, it is very difficult to ascertain the actual impact of HIV programmes in Zambia. Data on HIV incidence rates would have been preferable, since HIV prevalence can increase if people live longer because of effective ARV programmes, and given the problems associated with coverage and accessibility of ARV programmes across all provinces, further introducing an added and unpredictable variability. Despite these limitations, these analyses might be repeated in other countries in which HIV/AIDS is hyper-endemic and with at least two DHS surveys with reliable provincial-level HIV prevalence estimates. More nuanced spatial analyses can lend insights into the mechanisms of viral spread within countries and can help to geographically target prevention activities tailored to the suggested mechanisms, and thus more rapidly contain the epidemic.
ACKNOWLEDGEMENT
We thank Macro International for providing us the two rounds of the DHS data from Zambia and Becky Wilkes of CPC Spatial Analysis unit of Measure Evaluation for generating map in Figure 3.
Footnotes
The 2007 ZDHS report indicates a national prevalence of 14.3% using weighted data. Similarly, the 2001 DHS report indicates a national prevalence of 15.6% using weighted data. We report unweighted data, but our hierarchical Bayesian modelling takes into account the sampling design in order to account for the imbalanced distribution of the data.
CONTRIBUTIONS:
N-B Kandala: Conception and design. Literature review. Data analysis and interpretation. Drafting the article. Critical revisions for important intellectual content. Approval of final article for submission.
P Brodish: Literature review. Interpretation of results. Drafting the article. Critical revisions for important intellectual content. Approval of final article for submission.
B Buckner: Interpretation of results. Critical revisions for important intellectual content.
S Foster: Interpretation of results. Critical revisions for important intellectual content.
N Madise: Interpretation of results. Critical revisions for important intellectual content.
REFERENCES
- 1.Gouws E, White PJ, Stover J, Brown T. Short term estimates of adult HIV incidence by mode of transmission: Kenya and Thailand as examples. Sex Transm Infect. 2006;2006:82. doi: 10.1136/sti.2006.020164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. External review of the health sector response to HIV/AIDS in Thailand. India: WHO; 2005. Ministry of Public Health Thailand, World Health Organization Regional Office for South-East Asia. 2005. Link to report. [Google Scholar]
- 3.Central Statistical Office [Zambia], Central Board of Health [Zambia], and ORC Macro. Zambia Demographic and Health Survey 2001–2. Calverton, Maryland. USA: Central Statistical Office, Central Board of Health and ORC Macro; 2003. [Google Scholar]
- 4.Central Statistical Office (CSO), Ministry of Health (MOH), Tropical Diseases Research Centre (TDRC), University of Zambia, and Macro International Inc. Zambia Demographic and Health Survey 2007. Calverton, Maryland, USA: CSO and Macro International Inc.; 2009. [Google Scholar]
- 5.Kandala N-B, Ji C, Cappuccio PF, Stones RW. The epidemiology of HIV infection in Zambia, AIDS Care. 2008;20(7):812–819. doi: 10.1080/09540120701742292. [DOI] [PubMed] [Google Scholar]
- 6.Garbus L. HIV/AIDS in Zambia. University of California San Francisco: AIDS Policy Research Center; 2003. [Google Scholar]
- 7.National HIV/AIDS/STI/TB Council. Policy Overview and Status of the AIDS Epidemic in Zambia. 2010 (Lecture by NAC Director General)
- 8.Global HIV/AIDS Initiatives Network. [Accessed June 1, 2010];Funding and Scale-up of HIV/AIDS Services in Zambia, Policy Brief Global HIV/AIDS Initiatives Network, October 2009. 2009 Available: http://www.ghinet.org/downloads/Zambia_policybrief_scalingup.pdf.
- 9. [Accessed June 1, 2010];USAID Zambia Mission. 2010 Available: http://www.usaid.gov/zm/hiv/hiv.htm.
- 10.Inter Press Service (IPS) Health Zambia. [Accessed June 1, 2010];People Living With HIV/AIDS Find Drugs Elusive. 2003 Available: http://ipsnews.net/news.asp?idnews=21086.
- 11.Fahrmeir L, Lang S. Bayesian Inference for Generalized Additive Mixed Models Based on Markov Random Field Priors. Applied Statistics (JRSS C) 2001;50:201–220. [Google Scholar]
- 12.Central Statistical Office (CSO), Ministry of Health (MOH), University of Zambia, and MEASURE Evaluation. Zambia Sexual Behavior Survey 2009. Lusaka, Zambia: CSO and MEASURE Evaluation; 2010. [Google Scholar]
- 13.UNAIDS/WHO. Epidemiological Fact Sheet on HIV and AIDS, Zambia 2008 Update. New York, NY; Geneva, Switzerland: UNAIDS/WHO; 2010. p. 18. [Google Scholar]
- 14.Biennial Report to UNGASS. Distribution of new infections. Zambia Country Report: Monitoring the Declaration of Commitment on HIV and AIDS and the Universal Access, Biennial Report to UNGASS, 2010. 2010:29.
- 15.Graham AC. Making Prevention Work: Lessons from Zambia on Reshaping the U.S. Response to the Global HIV/AIDS Epidemic. SIECUS: Sexuality Information and Education Council of the United States. 2009 [Google Scholar]
- 16.U.S. State Department. [Accessed June 1, 2010.];Office of U.S. Global AIDS Coordinator and the Bureau of Public Affairs, U.S. State Department. 2010 Available: http://www.pepfar.gov/about/122668.htm.
- 17.COH III Program. PEPFAR Country Operational Plans - Fiscal Years 2007–2009. Zambia: 2009. p. 554. [Google Scholar]
- 18.World Bank. The World Bank’s commitment to HIV/AIDS in Africa: our agenda for action, 2007–2011. 2008
- 19.World Bank. Implementation completion and results report (IDA-H0170) on a grant in the amount of SDR 33.7 million (US$ 42 million equivalent) to the Republic of Zambia for the Zambia National Response to HIV/AIDS (ZANARA) project in support of the second phase of the multi-country AIDS program for Africa. 2009 Report No: ICR0000922.
- 20.COH II Program FHI. Corridors of Hope II. 2010 Available: http://www.fhi.org/en/CountryProfiles/Zambia/res_COHII_project.htm Also, Available: http://www.rti.org/brochures/zambia_hiv_coh2.pdf.
- 21.Zambian Ministry of Health report. Zambia HIV Prevention, Response and Modes of Transmission Analysis. 2009
- 22.Garcia-Calleja JM, Gouws E, Ghys PD. National population based HIV prevalence surveys in sub-Saharan Africa: results and implications for HIV and AIDS estimates. Sex Transm Infect. 2006;82 Suppl III:iii64–iii70. doi: 10.1136/sti.2006.019901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Afrol News. [May 30, 2006];Curbing HIV/AIDS along a transport corridor. 2006 Available: http://www.afrol.com/articles/19544.
- 24.USAID Zambia S09 Activities. [Accessed June 1, 2010];2010 Available: http://www.usaid.gov/zm/maps/so_9activities.pdf.
- 25.Kammann EE, Wand MP. Geoadditive models. J R Stat Soc C. 2003;52:1–18. [Google Scholar]
- 26.Eilers PHC, Marx BD. Flexible smoothing with B-splines and penalties (with discussion) Stat Sci 89. 1996:89–121. [Google Scholar]
- 27.Spiegelhalter D, Best N, Carlin B, Van der Line A. Bayesian measures of models complexity and fit. J R Stat Soc Ser B 64. 2002:1–34. [Google Scholar]