Abstract
Objectives
There is growing clinical and epidemiologic evidence indicating that major mood disorders form a spectrum from Major Depressive Disorder (MDD) to pure mania. The present investigation examined the prevalence and clinical correlates of MDD with sub-threshold bipolarity vs. pure MDD in the National Comorbidity Survey Replication (NCS-R).
Methods
The NCS-R is a nationally representative face-to-face household survey of the U.S. population conducted between February, 2001 and April, 2003. Lifetime history of mood disorders, symptoms and clinical indicators of severity were collected using version 3.0 of the WHO Composite International Diagnostic Interview, a fully structured lay-administered diagnostic interview.
Results
Nearly 40% of study participants with a history of major depressive disorder had a history of sub-threshold hypomania. This subgroup had a younger age of disorder onset, more episodes of depression, and higher rates of comorbidity than those without a history of hypomania, and lower levels of clinical severity than those with bipolar II disorder.
Conclusions
The findings demonstrate heterogeneity of major depressive disorder and support the validity of inclusion of sub-threshold mania in the diagnostic classification. The broadening of criteria for bipolar disorder would have important implications for research and clinical practice.
Keywords: Bipolar spectrum, Hypomania, Major Depressive Disorder, Epidemiology, National Comorbidity Survey
Introduction
Increasing evidence supports the existence of a spectrum of bipolar disorder that is far wider than is acknowledged by current diagnostic nosology. While recent lifetime prevalence estimates indicate that 1% of the U.S. population meet DSM-IV criteria for bipolar I disorder and 1.1% for bipolar II, recurrent hypomania without depression or recurrent sub-threshold hypomania (with or without depression) was found among 2.4% of respondents (1). These findings are consistent with those of other general population surveys conducted over the past two decades demonstrating the high prevalence of sub-threshold bipolar symptoms and disorder based on a range of definitions (2-6), and underscore the importance of unrecognized bipolarity in the general population.
The substantial proportion of the bipolar spectrum that is undetected has been attributed both to the narrow diagnostic criteria for bipolar II disorder as well as to the inherent difficulty in detecting milder forms of hypomania (7). This problem is potentially greatest for major depressive disorder, which may include heterogeneous conditions. Clinical studies indicate that 30-55% of those with major depression may be characterized by symptoms of hypomania (8-13), and that those with sub-threshold hypomania are less likely to respond adequately to usual treatments for major depression (14-15). Investigations of community samples demonstrate that those with major depression and sub-threshold bipolar disorder have more frequent suicide attempts (2, 16), higher rates of bipolar disorder among family members (2, 6), and increased comorbidity with anxiety, impulse control and substance use disorders (2, 4, 6), than those without sub-threshold hypomania. Some of the most compelling evidence for the validity of characterizing sub-threshold mania is the greater conversion rate to threshold-level bipolar disorder of adolescents with sub-threshold mania followed prospectively over time (7). These findings provide strong support for the clinical significance of hypomania involving fewer symptoms or lasting for a shorter duration than required by DSM-IV.
Recognition of the full spectrum of bipolar disorders is dependent on identification of the most appropriate definitions for sub-threshold manifestations. Previous descriptions by Akiskal and colleagues of the ‘soft’ bipolar spectrum have proposed broadening bipolar II criteria as well as creating a third bipolar category in order to more fully acknowledge cyclothymic and hyperthymic states, family history of bipolar disorder, temperament, and hypomanic episodes that occur during pharmacotherapy (7, 17-18). However, empirical evidence for either treatment-induced mania (19) or a latent form hypomanic temperament has not been forthcoming (20). Based on emerging evidence for a dimensional conceptualization of hypomanic symptoms, inclusion of a diagnostic specifier for “hidden” bipolarity in major depressive disorder has been proposed.
Using data from the National Comorbidity Survey Replication (NCS-R; (21), the present investigation examines the validity of distinguishing sub-threshold hypomania symptoms among those with major depression. We compare indices of clinical severity, family history, comorbidity patterns, and treatment utilization among major depressives with and without sub-threshold hypomania. Particular focus is placed on comparisons between major depression with sub-threshold hypomania, unrecognized by current nosology, and the two DSM-IV mood disorders for which clinical manifestations are most proximal: bipolar II disorder and unipolar major depressive disorder.
Methods
NCS-R Sampling and Field Procedures
The NCS-R is a nationally representative face-to-face household survey of the prevalence and correlates of a wide range of DSM-IV mental disorders that was carried out between February, 2001 and April, 2003 (21-22). The sampling frame was English speaking adults (ages 18 years and older) selected using a multi-stage clustered area probability design from the civilian household population of the continental United States. The NCS-R procedures were approved by the Human Subjects Committees of Harvard Medical School and the University of Michigan. A detailed description of procedures is presented elsewhere (22).
The NCS-R interview was carried out in two parts. The Part I interview was administered to a nationally representative household sample of 9282 respondents ages 18 and older. The response rate was 70.9% and informed consent was obtained from all participants prior to interview. Part I included the core mental disorders assessed in the survey along with a battery of sociodemographic variables. In an effort to reduce respondent burden and control study costs, Part II was administered to 5692 of the 9282 Part I respondents, including all Part I respondents with a lifetime core disorder plus a probability subsample of other respondents. The Part II sample was weighted to adjust for differential probabilities of within-household selection, differential probabilities of selection from the Part I sample into the Part II sample based on Part I responses, and for discrepancies between the sample and the US population on sociodemographic and geographic factors assessed in the 2000 Census. The Part II sample was used for these analyses.
Mood Disorder Assessment
The NCS-R diagnoses are based on Version 3.0 of the World Health Organization's Composite International Diagnostic Interview (CIDI: 23), a fully structured, lay-administered diagnostic interview. Mood disorders (Bipolar I, Bipolar II and Unipolar depression) were diagnosed following the DSM-IV criteria, with the exception of the requirement that symptoms do not meet the criteria for a mixed episode (criterion C for mania/hypomania and criterion B for MDE). Criteria for Sub-threshold hypomania included the presence of at least one of the screening questions for mania (1). “Some people have periods lasting several days or longer when they feel much more excited and full of energy than usual. Their minds go too fast. They talk a lot. They are very restless or unable to sit still and they sometimes do things that are unusual for them, such as driving too fast or spending too much money. Have you ever had a period like this lasting several days or longer?”; OR 2. “Have you ever had a period lasting several days or longer when most of the time you were so irritable that you either started arguments, shouted at people, or hit people?”, and failure to meet the full diagnostic criteria for hypomania. If respondents endorse either of these questions, the entire mania module of the CIDI is administered and they are queried regarding 15 symptoms of mania, and those who endorse 3 or more symptoms are asked about the duration, age at onset, recurrence, frequency, severity and impairment.
For the present study, we characterized those with Major Depressive Disorder (MDD) according to the presence of the mania spectrum as follows: 1. MDD with Mania (Bipolar-I); 2. MDD with Hypomania (Bipolar-II); 3. MDD with Sub-threshold Hypomania, as defined above; and 4. MDD alone. These categories and their corresponding definitions are presented in Table 1. All diagnoses excluded cases with plausible organic causes. Clinical reappraisal interviews for Bipolar Disorders using the lifetime non-patient version of the Structured Clinical Interview for DSM-IV (SCID: 24) were administered to a probability sub-sample of 50 NCS-R respondents. CIDI cases were over-sampled and the data weighted for this over-sampling. As described in more detail elsewhere (25) CIDI-SCID concordance (Kappa̤) was good for a diagnosis of Bipolar-I/II (K=.69), with sensitivity of .87, specificity of .99, and area under the receiver operating characteristic curve of .93. CIDI-SCID concordance was higher for Bipolar-I (.88) than Bipolar-II (.50), but the McNemar test was consistently not significant (χ 21 = 0.1-0.3, p = .56-.75) indicating that CIDI prevalence estimates are unbiased in relation to SCID prevalence estimates.
Table 1. Definitions of Bipolar Spectrum Variables.
| Subgroups | DSM Disorder | Definition |
|---|---|---|
| MDD + Mania | BIPOLAR I | Bipolar I |
|
| ||
| MDD + Hypomania | BIPOLAR II | Bipolar II |
|
| ||
| MDE + Hypomania | Major Depressive Episode + Hypomania (without impairment) | |
|
| ||
| MDD + Subth Hypomania | MDE + Subthreshold hypomania | MDE diagnosis + YES to either of the two mania screening questions: Mania and Irritability |
|
| ||
| MDD Only | MDE | MDE diagnosis + NO to both of the two mania screening questions |
Age of onset, age at offset and number of episodes of manic/hypomanic episodes and major depression were assessed using retrospective self-reports at the syndrome level. Course of illness was also assessed retrospectively by asking respondents to estimate the number of years in which they had at least one episode of mania/hypomania and the number of years in which they had an episode of major depression.
Symptom severity was assessed in 12-month cases using a self-report version of the Young Mania Rating Scale (YMRS: 26) for mania/hypomania and the Quick Inventory of Depressive Symptomatology Self-Report (QIDS-SR: 27) for major depression. The Young Mania Rating Scale was based on a fully structured respondent report version developed for parent reports (28). Severity was assessed for the month in the past year when symptoms of either mania or depression were most severe. Standard Young Mania Rating Scale and Quick Inventory of Depressive Symptomatology Self-Report cutoff points were used to define episodes as severe (including original Young Mania Rating Scale and Quick Inventory of Depressive Symptomatology Self-Report ratings of very severe, with ratings in the range ≥25 on the Young Mania Rating Scale and ≥16 on the Quick Inventory of Depressive Symptomatology Self-Report), moderate (15-24 on the Young Mania Rating Scale and 11-15 on the Quick Inventory of Depressive Symptomatology Self-Report), mild (9-14 on the Young Mania Rating Scale and 6-10 on the Quick Inventory of Depressive Symptomatology Self-Report), or not clinically significant (0-8 on the Young Mania Rating Scale and 0-5 on the Quick Inventory of Depressive Symptomatology Self-Report). We did not collect data on differences in the accuracy of recall for the 12 months used in the present study compared with those of the Quick Inventory of Depressive Symptomatology Self-Report (30 days) and the Young Mania Rating Scale (7 days).
Role impairment in 12-month cases was assessed using the Sheehan Disability Scale (SDS: 29). As with the Young Mania Rating Scale and the Quick Inventory of Depressive Symptomatology Self-Report, the Sheehan Disability Scale asks respondents to focus on the 1 month in the past year when their mania/hypomania or major depression symptoms were most severe. Respondents rated the degree to which the condition interfered with their home management, work, social life, and personal relationships using a visual analog scale from 0 to 10 (none=0, mild=1-3, moderate=4-6, severe =7-10).
Assessment of other mental disorders, treatment, and family history
In this study, we also assessed anxiety disorders, impulse control disorders, and substance use disorders using the CIDI and based on DSM-IV criteria. Organic exclusion rules and diagnostic hierarchy rules were used in making all diagnoses. As detailed elsewhere (30-31), blinded clinical reappraisal interviews using the non-patient version of the SCID with a probability sub-sample of NCS-R respondents found generally good concordance of CIDI/DSM-IV diagnoses of anxiety, mood, and substance disorders with independent clinical assessments. Impulse-control disorder diagnoses were not validated, as the SCID clinical reappraisal interviews did not include an assessment of these disorders.
Lifetime and 12-month treatment by health care professionals (including psychiatrists, other mental health professionals, general medical providers), human services professionals, and complementary or alternative medicine providers was assessed by self-report. Information concerning mania in family members was collected in the mania section of the CIDI, and information about depression in family members was gathered only for the mother and father of the interviewed subject within the childhood section of the CIDI. Lifetime suicide attempts were assessed using the Suicidality Module of the CIDI.
Statistical Analyses
Due to the weighting and clustering used in the NCS-R design, all statistical analyses were performed using the Taylor series linearization method (32) a design-based method implemented using a software system (SUDAAN version 10; RTI International, Research Triangle Park, NC). Significance tests of sets of coefficients were performed using Wald χ2 tests based on design-corrected coefficient variance-covariance matrices. Statistical significance was evaluated using a 2-sided design based on .05-level tests. Controlling for respondent age and sex, linear regression was used to study the association between continuous outcomes (age of onset of mood disorders) and bipolar groups. Subgroup comparisons included MDD with Mania vs. Hypomania vs. Sub-threshold Hypomania, vs. MDD alone. Logistic regression analyses were used to assess the associations between dichotomous outcomes and bipolar groups while controlling for age and sex.
Results
Table 2 presents the lifetime and 12-month prevalence rates for bipolar and unipolar mood disorders. When considered together, bipolar spectrum conditions were nearly as frequent as unipolar major depression without sub-threshold hypomania. In particular, the lifetime prevalence of MDD with Sub-threshold Hypomania was 6.7%.
Table 2. Lifetime and 12-month prevalence estimates of the bipolar spectrum groups in NCS-R (n=5692).
| Lifetime Prevalence | 12-month Prevalence | |||
|---|---|---|---|---|
| % | (s.e.) | % | (s.e.) | |
| MDD + Mania | 0.7 | 0.1 | 0.3 | 0.1 |
| MDD + Hypomania | 1.6 | 0.2 | 0.8 | 0.1 |
| MDD + Subth Hypomania | 6.7 | 0.0 | 2.2 | 1.9 |
| MDD Only | 10.2 | 0.4 | 5.4 | 0.3 |
Information concerning clinical correlates of the mood disorder categories is presented in Table 3. Individuals with bipolar II disorder were more likely than those with MDD plus Sub-threshold Hypomania to have been treated for mood disorders over their lifetime as well as within the last 12 months, but no treatment differences were observed between the latter subgroup and MDD alone. Compared to MDD alone, however, those with MDD with Sub-threshold Hypomania had greater rates of comorbidity with anxiety, substance use disorders and behavioral problems. In comparison to Bipolar-II disorder, MDD with Sub-threshold Hypomania had lower comorbidity. The proportion of the Sub-threshold Hypomania with MDD group with suicide attempts (e.g., 41%) fell between those of the Bipolar-II subgroup (50%) and those with MDD alone (31%). However, these differences were not statistically significant.
Table 3. Clinical Correlates and Impact of Mood Disorder Spectrum Subgroups.
| MDD + Mania | MDD + Hypomania | MDD + Subth Hypomania | MDD Only | MDD + Hypomania vs. MDD + Subth Hypomania | MDD + Subth Hypomania vs. MDD Only | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | s.e. | % | s.e. | % | s.e. | % | s.e. | OR (95% C.I.) | OR (95% C.I.) | |
| Treatment for Mood Disorders | ||||||||||
| Lifetime | 86.2 | 3.3 | 81.2 | 3.9 | 64.9 | 2.4 | 64.8 | 1.8 | 2.4 (1.4-4.0)* | 1.0 (0.8-1.4) |
| Last 12 months | 67.7 | 8.8 | 46.3 | 5.4 | 38.8 | 3.9 | 38.3 | 2.3 | 1.7 (1.2-2.4)* | 1.2 (0.9-1.5) |
| Comorbidity disorders (Lifetime) | ||||||||||
| Anxiety | 87.1 | 4.8 | 82.6 | 3.3 | 72.2 | 2.8 | 52.6 | 1.7 | 1.9 (1.2-3.0)* | 2.3 (1.8-3.0)* |
| Substance Use | 63.9 | 4.6 | 41.8 | 3.7 | 35.3 | 2.3 | 18.0 | 1.5 | 1.4 (1.0-2.0)* | 2.3 (1.7-3.1)* |
| Behavioral Problem | 69.0 | 5.5 | 50.4 | 5.1 | 41.1 | 2.1 | 19.2 | 1.0 | 1.7 (1.1-2.6)* | 2.3 (1.8-2.9)* |
| Suicide Attempts (Lifetime) | 66.1 | 7.1 | 50.2 | 6.7 | 40.7 | 3.3 | 31.2 | 3.2 | 1.5 (0.9-2.7) | 1.4 (1.0-2.1)* |
| Sheehan Disability Scale: Role impairment (12 month) | ||||||||||
| Severe (%) | 94.3 | 3.8 | 91.9 | 3.8 | 67.1 | 4.0 | 61.5 | 2.3 | 5.6 (2.0-16.2)*a | 1.3 (0.9-1.9)b |
| Moderate (%) | 5.7 | 3.8 | 7.0 | 3.6 | 24.7 | 3.7 | 27.6 | 2.2 | ||
| Mild (%) | NA | NA | 1.1 | 1.2 | 6.2 | 1.8 | 7.8 | 1.3 | ||
| None (%) | NA | NA | NA | NA | 2.0 | 1.1 | 3.1 | 0.8 | ||
Severe group versus all others
p<0.05
Examination of clinical correlates within the bipolar spectrum (Table 4) demonstrates that bipolar II is associated with a five-fold risk of having a severe score on the Young Mania Rating Scale compared to MDD with Sub-threshold Hypomania, but no difference was observed when the categories of moderate and severe were collapsed. Individuals with MDD with Sub-threshold Hypomania also were less likely to have been treated for manic symptoms over their lifetime or within the past 12 months. No difference was found between these two conditions for family history of mania.
Table 4. Clinical Correlates of Mania by Mood Disorder Spectrum Subgroups.
| MDD + Mania | MDD + Hypomania | MDD + Subth Hypomania | MDD Only | MDD + Hypomania vs. MDD + Subth Hypomania | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| % | s.e. | % | s.e. | % | s.e. | % | s.e. | OR (95% C.I.) | |||
| Treatment for mania | |||||||||||
| Lifetime | 64.1 | 5.2 | 59.7 | 4.1 | 5.6 | 1.3 | NA | NA | 25.8 (13.3-50.1)* | ||
| Last 12 months | 44.8 | 10.1 | 36 | 5.0 | 12.5 | 3.3 | NA | NA | 4.0 (1.7-9.3)* | ||
| Young Mania Rating Scales (12 month) | |||||||||||
| Severe | 84.8 | 7.4 | 53.3 | 8.0 | 19.8 | 8.0 | NA | NA | 5.0 (1.4-18.2)*a | ||
| Moderate | 12.4 | 7.0 | 27.8 | 7.4 | 62.2 | 9.7 | NA | NA | |||
| Mild | 2.8 | 2.8 | 13.7 | 5.0 | 6.6 | 4.8 | NA | NA | |||
| None | 0.0 | 0.0 | 5.2 | 3.1 | 11.4 | 7.6 | NA | NA | |||
| Mania in family members | 70.4 | 5.6 | 67.8 | 3.9 | 76 | 5.8 | NA | NA | 0.7 (0.3-1.4) | ||
Severe group versus all others
p<0.05
Clinical correlates related to depression are presented in Table 5. Individuals with bipolar II disorder had significantly more severe depressive symptoms and more episodes of depression than MDD with Sub-threshold Hypomania, and were more likely to have been treated for depression over their lifetime. MDD with Sub-threshold Hypomania did not differ from MDD concerning the severity of depressive symptoms, treatment of depression, of family history of depression. However, those with MDD with Sub-threshold Hypomania had significantly more episodes of depression than those with MDD alone.
Table 5. Clinical Correlates of Depression by Mood Disorder Spectrum Subgroups.
| MDD + Mania | MDD + Hypomania | MDD + Subth Hypomania | MDD Only | MDD + Hypomania vs. MDD + Subth Hypomania | MDD + Subth Hypomania vs. MDD Only | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | s.e. | % | s.e. | % | s.e. | % | s.e. | OR (95% C.I.) | OR (95% C.I.) | |
| Treatment for depression | ||||||||||
| Lifetime | 86.2 | 3.3 | 77.4 | 4.5 | 64.9 | 2.4 | 64.8 | 1.8 | 1.8 (1.1-3.1)* | 1.1 (0.8-1.4) |
| Last 12 months | 63.3 | 9.1 | 42.8 | 5.4 | 36.1 | 4.0 | 38.3 | 2.3 | 1.3 (0.8-2.3) | 0.9 (0.6-1.4) |
| Number of episodes of depression | ||||||||||
| ≥5 | 72.0 | 4.9 | 60.2 | 5.4 | 39.6 | 1.9 | 25.6 | 1.6 | 2.3 (1.5-3.7)*a | 1.9 (1.5-2.4)*b |
| 2-5 | 23.3 | 3.9 | 25.1 | 3.5 | 41.3 | 2.2 | 39.3 | 2.0 | ||
| ≤1 | 4.7 | 2.2 | 14.7 | 3.3 | 19.1 | 1.7 | 35.1 | 1.8 | ||
| Quick Inventory of Depressive Symptoms (12 month) | ||||||||||
| Severe | 72.4 | 10.0 | 73.8 | 7.5 | 54.1 | 3.5 | 51.7 | 2.1 | 2.4 (1.1-5.5)*c | 1.1 (0.8-1.6)d |
| Moderate | 20.5 | 9.5 | 26.2 | 7.5 | 36.6 | 3.4 | 36.9 | 2.0 | ||
| Mild | 7.1 | 5.1 | 0.0 | 0.0 | 8.6 | 1.8 | 9.3 | 1.5 | ||
| None | 0.0 | 0.0 | 0.0 | 0.0 | 0.7 | 0.7 | 2.1 | 0.8 | ||
| Depression in family members | 31.6 | 6.6 | 28.3 | 4.7 | 20.0 | 1.7 | 16.8 | 1.5 | 1.7 (1.0-2.8)* | 1.1 (0.8-1.5) |
Subjects with more than 5 episodes versus all others
Severe group versus all others
p<0.05
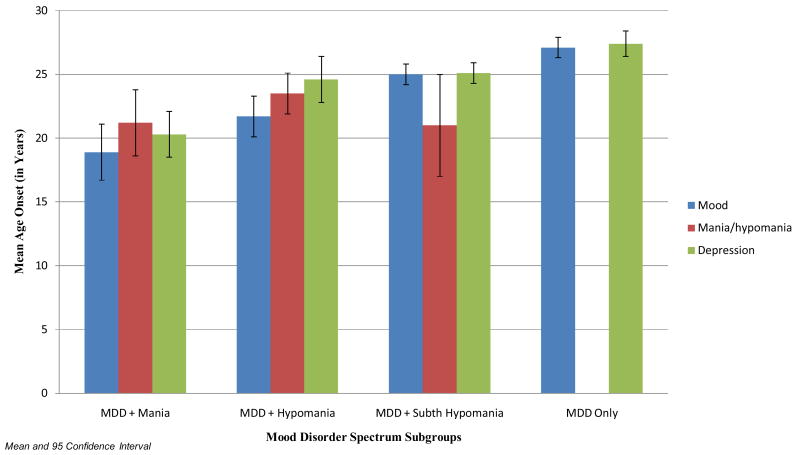
Figure 1 shows the mean age of onset for mood disorder, mania/hypomania, and depression by bipolar spectrum groups. MDD with Sub-threshold Hypomania has an earlier age of onset for mood disorder than MDD alone, and, in turn, a later age of onset than MDD with Hypomania (BP-II). No differences were found between MDD with Hypomania (BP-II) and MDD with Sub-threshold Hypomania for the age of onset of mania/hypomania and age onset of depression. MDD with Sub-threshold Hypomania had a younger age of first onset for depression than MDD alone.
Figure 1. Mean Age Onset of Mania/Hypomania and Depression by Mood Disorder Spectrum Subgroups.
Discussion
Converging evidence from clinical and epidemiologic studies suggests that the current diagnostic criteria for bipolar II disorder fail to include milder but clinically significant bipolar syndromes, and that a significant percentage of these conditions are diagnosed by default as unipolar major depression (6, 16). Using data from a nationally-representative sample, the present investigation examined the validity of characterizing sub-threshold bipolarity as a source of heterogeneity in major depressive disorder (6). Its principal aims were to estimate the prevalence of these categories of the bipolar spectrum and to compare the clinical characteristics of major depression with Sub-threshold Hypomania to other bipolar disorders as well as to MDD alone.
Application of the present categories revealed considerable diversity in the clinical manifestations of mood disorders and indicate that bipolar spectrum disorders are almost as frequent as ‘pure’ unipolar depression. However, the question of perhaps greatest importance to mood disorder research and clinical practice concerns the appropriateness of diagnosing major depression in individuals who also have Sub-threshold Hypomania. This subtype of mood disorder corresponds to 39% of all cases of unipolar major depression in the general population, and it was not found to differ from depression alone in terms of lifetime or 12-month treatment for mood disorders. While these findings are consistent with past research demonstrating that Sub-threshold Hypomania is often subsumed under the category of unipolar depression (8-9, 11-13, 16, 18), important differences were nonetheless observed in the clinical characteristics of these categories. Individuals with MDD and Sub-threshold Hypomania had a younger age of disorder onset, greater rates of comorbidity, more episodes of depression and a trend towards more suicide attempts compared to individuals with MDD alone. Considered jointly with reported differences in response to pharmacotherapy between these forms of mood disorder (15, 33), the present findings underscore the heterogeneity of major depression and support the notion that a critical reappraisal of diagnostic criteria for mood disorders is warranted.
Differences were also observed for markers of clinical severity or history when comparing individuals with MDD and Sub-threshold Hypomania to those meeting criteria for bipolar II disorder. However, these findings reflect the greater general severity in bipolar II disorder rather than differences in the basic expression of depressive or hypomanic syndromes. Perhaps the most convincing evidence for inclusion of the concept of sub-threshold hypomania is the finding that a family history of mania is equally common among those with sub-threshold hypomania as with threshold mania. Although the family history was based on report by the respondents, it is unlikely that there would be differential bias by the various mania/hypomania subgroups. As these differences are quantitative in nature, they are consistent with conceptualization of depression with sub-threshold hypomania as a milder manifestation of bipolar disorder as described nearly a century ago (34) and whose pertinence has been reemphasized since the introduction of modern diagnostic systems (8, 35). The inclusion of Sub-threshold Hypomania among those with MDD in the diagnosis of bipolar disorders would have a far reaching impact on a number of scientific disciplines, ranging from descriptive and analytic epidemiology to genetic research, whose progress depends on validity of mood disorder phenotypes. Most importantly, such an expansion of the bipolar concept would likely lead to important changes in the treatment of patients who are undiagnosed or misdiagnosed despite elevated morbidity and mortality rates (36-37).
The present findings also have important clinical implications for the evaluation of mood disorders. If there is a substantial group of major depressives who manifest hidden bipolarity, it would be critical to include careful evaluation of a history of hypomania symptoms and family history of mania. In fact, based on the convergence of findings across international samples as well as emerging evidence from clinical studies, a diagnostic specifier for sub-threshold bipolarity in the diagnostic category of major depression has been proposed (6). Despite the widespread clinical belief that antidepressants may trigger bipolar symptoms in susceptible individuals, empirical evidence for this is lacking (19). However, addition of a mood stabilizer after response to antidepressant treatment may be beneficial in those who manifest sub-threshold bipolarity (38).
The present results provide the first comparisons of the prevalence and clinical correlates of BP- II disorder, MDD with Sub-threshold Hypomania, and MDD alone in a nationally-representative U.S. sample. These findings confirm those of a population-based study of young adults which also revealed that nearly 40% of those with major depression may manifest bipolar disorder. Concerning limitations of this study that should be considered in interpreting the findings, the use of the fully structured, lay-administered CIDI precluded the collection of information on the full spectrum of expression of bipolar disorder proposed in recent studies (7, 16, 39). Although we could not modify the thresholds for some of the diagnostic criteria for mania and depression, our definition of sub-threshold bipolar disorder is still more restrictive than the definitions proposed by clinical researchers. Therefore, our prevalence estimate of sub-threshold bipolar disorder is likely to underestimate bipolar spectrum disorder in the population. Although the clinical reappraisal study found good concordance of CIDI diagnoses with blinded clinical diagnoses based on the SCID, concordance was lower for Bipolar-II and sub-threshold bipolar disorder than for Bipolar Disorder-I (25). The less flexible nature of the CIDI in comparison to clinical interviews could have also led to overestimation of comorbidity and potentially influence clinical severity markers. Differences between the 1-year recall period of the symptom scales used in the present study and those for which the scales were standardized diminish the comparability of the present findings with those of previous clinical samples. In addition, the prevalence of mania in family members was not assessed in all groups. Finally, although the prevalence of bipolar disorder would be expected to increase if diagnostic criteria were expanded to include MDD with Sub-threshold Mania, there would not be an increase in the overall prevalence of mood disorders because there would be a concomitant decrease in the rates of major depression. This risk should be examined critically but weighed against prospective evidence that youth with Major Depressive episodes plus Sub-threshold Mania have a high probability of conversion to bipolar-I disorder (6) and that milder manifestations of the bipolar spectrum can be distinguished from major depression in severity, course, and comorbidity.
Acknowledgments
The National Comorbidity Survey Replication (NCS-R) was supported by grant U01-MH60220 from the National Institute of Mental Health (NIMH) with supplemental support from the National Institute of Drug Abuse (NIDA), The Substance Abuse and Mental Health Services Administration; grant 044708 from The Robert Wood Johnson Foundation and the John W. Alden Trust. Manuscript preparation was supported by the Intramural Research Program of the National Institutes of Health, National Institute of Mental Health (Ms. Cui and Drs. Cravchik, Rothen, and Merikangas), and an ATIP award from the French National Center for Scientific Research (Dr. Swendsen),. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or US Government.
Footnotes
Financial Disclosure and conflict of interest: Dr Kessler has been a consultant for GlaxoSmith-Kline Inc., Kaiser Permanente, Pfizer Inc., Sanofi-Aventis, Shire Pharmaceuticals and Wyeth-Ayest; has served on advisory boards for Eli Lilly & Company and Wyeth-Ayerst; and has had research support for his epidemiological studies from Bristol-Myers Squibb, Eli Lilly & Company, GlaxoSmithKline, Johnson & Johnson Pharmaceuticals, Ortho-McNeal Pharaceuticals Inc., Pfizer Inc., and Sanofi-Aventis. Prof Dr. Angst has served on the advisory board for Eli Lilly & Company, Janssen Cilag and Sanofi Aventis, and has served on the speakers' bureau for Eli Lilly & Company and AstraZeneca.
References
- 1.Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. [erratum appears in Arch Gen Psychiatry. 2007 Sep;64(9):1039] Archives of General Psychiatry. 2007;64(5):543–52. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Angst J, Gamma A, Benazzi F, Ajdacic V, Eich D, Rossler W. Toward a re-definition of sub-threshold bipolarity: Epidemiology and proposed criteria for bipolar-II, minor bipolar disorders and hypomania. Journal of Affective Disorders. [Journal; Peer Reviewed Journal] 2003 Jan;73(1-2):133–46. doi: 10.1016/s0165-0327(02)00322-1. [DOI] [PubMed] [Google Scholar]
- 3.Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry. 1995 Apr;34(4):454–63. [PubMed] [Google Scholar]
- 4.Merikangas KR, Herrell R, Swendsen J, Rossler W, Ajdacic-Gross V, Angst J. Specificity of bipolar spectrum conditions in the comorbidity of mood and substance use disorders: results from the Zurich cohort study. Arch Gen Psychiatry. 2008 Jan;65(1):47–52. doi: 10.1001/archgenpsychiatry.2007.18. [DOI] [PubMed] [Google Scholar]
- 5.Szadoczky E, Papp Z, Vitrai J, Rihmer Z, Furedi J. The prevalence of major depressive and bipolar disorders in Hungary. Results from a national epidemiologic survey. J Affect Disord. 1998 Sep;50(2-3):153–62. doi: 10.1016/s0165-0327(98)00056-1. [DOI] [PubMed] [Google Scholar]
- 6.Zimmermann P, Bruckl T, Nocon A, Pfister H, Lieb R, Wittchen HU, et al. Heterogeneity of DSM-IV major depressive disorder as a consequence of sub-threshold bipolarity. Arch Gen Psychiatry. 2009 Dec;66(12):1341–52. doi: 10.1001/archgenpsychiatry.2009.158. [DOI] [PubMed] [Google Scholar]
- 7.Akiskal HS, Bourgeois ML, Angst J, Post R, Moller H, Hirschfeld R. Re-evaluating the prevalence of and diagnostic composition within the broad clinical spectrum of bipolar disorders. Journal of Affective Disorders. 2000;59 1:S5–S30. doi: 10.1016/s0165-0327(00)00203-2. [DOI] [PubMed] [Google Scholar]
- 8.Akiskal HS, Mallya G. Criteria for the “soft” bipolar spectrum: treatment implications. Psychopharmacol Bull. 1987;23(1):68–73. [PubMed] [Google Scholar]
- 9.Benazzi F. Antidepressant-associated hypomania in outpatient depression: a 203-case study in private practice. J Affect Disord. 1997 Oct;46(1):73–7. doi: 10.1016/s0165-0327(97)00082-7. [DOI] [PubMed] [Google Scholar]
- 10.Cassano GB, Savino M, Perugi G, Musetti L, Akiskal HS. Major depressive episode: unipolar and bipolar II. Encephale. 1992 Jan;(Spec No 1):18. 15–8. [PubMed] [Google Scholar]
- 11.Hantouche EG, Akiskal HS, Lancrenon S, Allilaire JF, Sechter D, Azorin JM, et al. Systematic clinical methodology for validating bipolar-II disorder: data in mid-stream from a French national multi-site study (EPIDEP) J Affect Disord. 1998 Sep;50(2-3):163–73. doi: 10.1016/s0165-0327(98)00112-8. [DOI] [PubMed] [Google Scholar]
- 12.Koukopoulos A, Reginaldi D, Laddomada P, Floris G, Serra G, Tondo L. Course of the manic-depressive cycle and changes caused by treatment. Pharmakopsychiatre. 1980;13:156–67. doi: 10.1055/s-2007-1019628. [DOI] [PubMed] [Google Scholar]
- 13.Manning JS, Haykal RF, Connor PD, Akiskal HS. On the nature of depressive and anxious states in a family practice setting: the high prevalence of bipolar II and related disorders in a cohort followed longitudinally. Compr Psychiatry. 1997 Mar-Apr;38(2):102–8. doi: 10.1016/s0010-440x(97)90089-4. [DOI] [PubMed] [Google Scholar]
- 14.Seemüller F, Severus E, Möller HJ, Riedel M. Letter to the editor: Antidepressants and suicidality in younger adults – is bipolar illness the missing link? Acta Psychiatrica Scandinavica. 2009;119:166–7. doi: 10.1111/j.1600-0447.2008.01328.x. [DOI] [PubMed] [Google Scholar]
- 15.Keck PE, Jr, Kessler RC, Ross R. Clinical and economic effects of unrecognized or inadequately treated bipolar disorder. Journal of Psychiatric Practice. [Journal; Peer Reviewed Journal] 2008 May;14(Suppl 2):31–8. doi: 10.1097/01.pra.0000320124.91799.2a. [DOI] [PubMed] [Google Scholar]
- 16.Judd LL, Akiskal HS. The prevalence and disability of bipolar spectrum disorders in the US population: Re-analysis of the ECA database taking into account sub-threshold cases. Journal of Affective Disorders. [Journal; Peer Reviewed Journal] 2003 Jan;73(1-2):123–31. doi: 10.1016/s0165-0327(02)00332-4. [DOI] [PubMed] [Google Scholar]
- 17.Akiskal HS. The bipolar spectrum: new concepts in classification and diagnosis. In: Grinspoon L, editor. Psychiatry Update: The American Psychiatric Association Annual Review. Washington, DC: American Psychiatry Press; 1983. pp. 271–92. [Google Scholar]
- 18.Cassano GB, Akiskal HS, Savino M, Musetti L, Perugi G. Proposed subtypes of bipolar II and related disorders: with hypomanic episodes (or cyclothymia) and with hyperthymic temperament. J Affect Disord. 1992 Oct;26(2):127–40. doi: 10.1016/0165-0327(92)90044-7. [DOI] [PubMed] [Google Scholar]
- 19.Licht RW, Gijsman H, Nolen WA, Angst J. Are antidepressants safe in the treatment of bipolar depression? A critical evaluation of their potential risk to induce switch into mania or cycle acceleration. Acta Psychiatr Scand. 2008 Nov;118(5):337–46. doi: 10.1111/j.1600-0447.2008.01237.x. [DOI] [PubMed] [Google Scholar]
- 20.Meyer TD, Keller F. Is there evidence for a latent class called ‘hypomanic temperament’? J Affect Disord. 2003 Aug;75(3):259–67. doi: 10.1016/s0165-0327(02)00051-4. [DOI] [PubMed] [Google Scholar]
- 21.Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res. 2004;13(2):60–8. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, et al. The US National Comorbidity Survey Replication (NCS-R): Design and field procedures. International Journal of Methods in Psychiatric Research. [Journal; Peer Reviewed Journal] 2004;13(2):69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. [Journal; Peer Reviewed Journal] 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 25.Kessler RC, Akiskal HS, Angst J, Guyer M, Hirschfeld RMA, Merikangas KR, et al. Validity of the assessment of bipolar spectrum disorders in the WHO CIDI 3.0. Journal of Affective Disorders. [Journal; Peer Reviewed Journal] 2006 Dec;96(3):259–69. doi: 10.1016/j.jad.2006.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. British Journal of Psychiatry. [Journal; Peer Reviewed Journal] 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 27.Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry. [Journal; Peer Reviewed Journal] 2003 Sep;54(5):573–83. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 28.Gracious BL, Youngstrom EA, Findling RL, Calabrese JR. Discriminative validity of a parent version of the Young Mania Rating Scale. Journal of the American Academy of Child & Adolescent Psychiatry. [Journal; Peer Reviewed Journal] 2002 Nov;41(11):1350–9. doi: 10.1097/00004583-200211000-00017. [DOI] [PubMed] [Google Scholar]
- 29.Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. International Journal of Psychiatry in Medicine. [Journal; Peer Reviewed Journal] 1997;27(2):93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- 30.Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, et al. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMH-CIDI) International Journal of Methods in Psychiatric Research. [Journal; Peer Reviewed Journal] 2004;13(2):122–39. doi: 10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. [Journal; Peer Reviewed Journal] 2005 Jun;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 32.Wolter K. Introduction to Variance Estimation. New York, NY: Springer-Verlag; 1985. [Google Scholar]
- 33.Angst J. The bipolar spectrum. British Journal of Psychiatry. 2007;190:189–91. doi: 10.1192/bjp.bp.106.030957. [DOI] [PubMed] [Google Scholar]
- 34.Kraepelin E. Manic-depressive insanity and significance of hypomanic switches in unipolar melancholic paranoia. Edinburgh: ES Livingstone; 1899/1921. [Google Scholar]
- 35.Angst J, Frey R, Lohmeyer B, Zerbin-Rudin E. Bipolar manic-depressive psychoses: results of a genetic investigation. Hum Genet. 1980;55(2):237–54. doi: 10.1007/BF00291773. [DOI] [PubMed] [Google Scholar]
- 36.Hirschfeld RM, Keller MB, Panico S, Arons BS, Barlow D, Davidoff F, et al. The National Depressive and Manic-Depressive Association consensus statement on the undertreatment of depression. JAMA. 1997 Jan 22-29;277(4):333–40. [PubMed] [Google Scholar]
- 37.Lish JD, Dime-Meenan S, Whybrow PC, Price RA, Hirschfeld RM. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord. 1994 Aug;31(4):281–94. doi: 10.1016/0165-0327(94)90104-x. [DOI] [PubMed] [Google Scholar]
- 38.Licht RW, Vestergaard P, Brodersen A. Long-term outcome of patients with bipolar disorder commenced on lithium prophylaxis during hospitalization: a complete 15-year register-based follow-up. Bipolar Disord. 2008 Feb;10(1):79–86. doi: 10.1111/j.1399-5618.2008.00499.x. [DOI] [PubMed] [Google Scholar]
- 39.Akiskal HS, Benazzi F. Optimizing the detection of bipolar II disorder in outpatient private practice: toward a systematization of clinical diagnostic wisdom. Journal of Clinical Psychiatry. 2005;66(7):914–21. doi: 10.4088/jcp.v66n0715. [DOI] [PubMed] [Google Scholar]