Abstract
Intramural hematoma of duodenum (IDH) is a relatively unusual complication associated with endoscopic treatment of bleeding peptic ulcer. This unusual condition is usually seen in children following blunt trauma to the abdomen. We describe here a case of IDH occurring following endoscopic therapy for bleeding duodenal ulcer in an adult patient with end-stage renal disease. The hematomas appeared on the second day of endoscopic intervention, caused transient duodenal obstruction and resolved spontaneously with conservative treatment in a week.
Keywords: Duodenal hematoma, endotherapy, ulcer bleeding
Introduction
Peptic ulcer bleeding continues to be an important cause of non-variceal upper gastrointestinal bleeding. The endoscopic therapy is well-accepted as the first-line management tool for bleeding peptic ulcer. Endoscopic therapy for a bleeding peptic ulcer generally includes injection therapy, thermal coagulation and mechanical hemostasis. A combined therapy, in which the injection of diluted epinephrine precedes thermal coagulation, offers the best approach for successful outcomes.[1] The risk of complications with endoscopic treatment is uncommon (0.5%) and mainly includes aspiration pneumonia and gut perforation.[2] We describe here an uncommon case of intramural duodenal hematoma (IDH) which developed following endoscopic therapy of bleeding duodenal ulcer.
Case Report
This 38-year-old gentleman, known case of end-stage renal disease (ESRD) with acute hepatitis E in resolving phase, presented to our emergency OPD with complaints of multiple episodes of malena for 1 day. Patient had been on maintenance hemodialysis (HD) twice per week elsewhere and had received last HD 2 days prior to onset of peptic ulcer bleed. At presentation, he was severely anemic and hemodynamically unstable with blood pressure of 80/50 mmHg and pulse rate of 120/minute. His relevant laboratory investigation were as follows: hemoglobin 4.1 g/dl; platelet count 328×10 3/mm3; white blood cell count 8,500/mm3; INR 1.1; serum bilirubin 4.0 mg/dl (direct: 2.2 mg/dl), alanin transaminase: 41 IU/L, aspartate transaminase 47 IU/L, alkaline phosphatase 328 IU/l (normal: 32-92) IU/L), serum albumin 2.0 g/dl, blood urea 156 mg% and serum creatinin 6.5 mg/dl.
After resuscitation, an emergency esophagogastroduo -denoscopy (EGD) was done which revealed a large oozing ulcer in the anterior wall of the duodenal bulb [Figure 1]. Endoscopic treatment consisted of injection of 2 ml 0.2% adrenaline at four sites around the ulcer followed by application of tip of the heater probe directly to the bleeding site to apply tamponade and coagulation with long pulses at 15 W power setting. Hemostasis was achieved from bleeding vessel; however, minimal ooze was noted at the margin of ulcer which was controlled with APC. Patient was given intravenous infusion of a proton pump inhibitor and a transfusion of five units of packed red blood cells.
Figure 1.
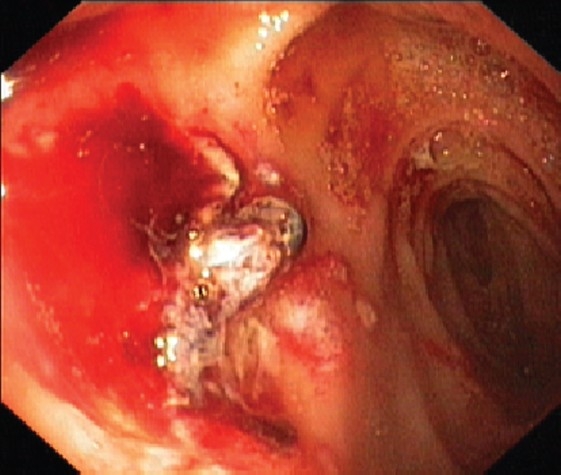
EGD on admission revealed a large ulcer in the distal portion of duodenal bulb
A day following endoscopic treatment, patient developed epigastric discomfort, recurrent bouts of vomiting along with fall in hemoglobin level from initial rise of 7.7 to 6.3 g/dl. EGD was repeated on the third day which revealed a large sub-mucosal bulge in the first part of duodenum near ulcer site causing duodenal obstruction [Figures 2a and b]. The lesion was consistent with a large IDH on CT scan of abdomen [Figure 3]. The bulk of hematoma was located at the postero-inferior wall of the duodenal bulb and its distal extension was seen up to third part of duodenum. This was not the site of injection or application of the heater probe. He was treated with bowel rest, parental nutrition and nasogastric decompression. For ESRD, patient was given twice weekly heparin-free HD with intermittent saline flushes. He became symptomatically improved over the next 7 days. On follow-up at 8 weeks, a repeat EDG revealed healed duodenal ulcer with no evidence of hematoma [Figure 4].
Figure 2.
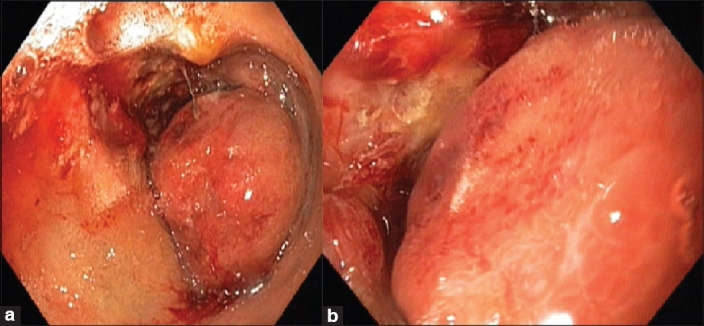
(a-b) EGD on the third hospital day showing an intramural hematoma with duodenal obstruction
Figure 3.

Contrast-enhanced abdominal CT scan showing a large hematoma at the duodenal wall
Figure 4.

EDG at 8thweek revealed healed duodenal ulcer without any evidence of hematoma
Discussion
IDH is an uncommon complication of endoscopic intervention. It usually occurs in children and young adults secondary to blunt trauma to the abdomen.[3] However, in adult this condition can occur in presence of coagulation abnormality even with minimal or endoscopic trauma. The underlying conditions, where such complication may be anticipated, are cirrhosis, ESRD, leukemia and anti-coagulation treatment.[4] As IDH has been reported in a healthy subject after endoscopic duodenal biopsy, it can occur sometime in patients without obvious risk factor.[5] In our case, the coagulation parameters as well as platelets count were within normal limits; however, platelet dysfunction because of ESRD is a known phenomenon.[6]
The mechanism of hematoma formation due to endoscopic intervention is not yet clear. The mechanism may be multifactorial where iatrogenic trauma (needle, scope, instrument, injection, etc.) as well as underlying conditions play a part. The relative fixicity of duodenum in retroperitoneum, location ahead of vertebral column and rich vascular plexus make duodenum vulnerable to this unusual complication following blunt trauma to abdomen. The prolonged procedure, repeated maneuverings of endoscope and trauma caused by injecting needle and heater probe may cause stripping of the mucosa from the underlying fixed submucosa and serosa resulting in rupture of submucosal vessels and subsequent formation hematoma in predisposed individuals. Furthermore, intermittent systemic anti-coagulation during maintenance HD might have contributed to this complication in our case. Earlier, cases with duodenal hematomas subsequent to endoscopic interventions have been reported,[7,8] including in patients with ESRD and cirrhosis.[9,10] To our knowledge, this complication has never been reported from India.
The diagnosis of duodenal hematoma is based on signs and symptoms of high gut obstruction and fall in hemoglobin without overt signs of bleeding. EDG followed by enhanced CT, which is the best imaging tool, can confirm the diagnosis. The management of this condition is usually non-operative.[11] Because of the rich blood supply of the duodenal wall, the hematoma is anticipated to be absorbed with time. Normalization of INR to <1.6 with fresh-frozen plasma and/or vitamin K is required on an individual case-by-case basis. Surgical treatment may be considered when there is no evidence of partial resolution after 7 days of conservative treatment or in cases of perforation. Another issue of management in this case was maintenance HD for ESRD. Because of high risk of bleeding complications,[12] dialytic modalities that completely preclude systemic anticoagulation, i.e. peritoneal dialysis, heparin-free HD, and HD with regional anticoagulation like citrate should be preferred. However, some data suggest that even HD does not normalize platelet abnormalities in patients with ESRD.[13] In this case, we had used heparin-free HD with intermittent saline flushes which was effective and safe.
In conclusion, IDH can occur uncommonly following a commonly performed endoscopic procedure. The diagnosis is suspected by clinical feature and is confirmed by endoscopic and imaging findings. The conservative treatment usually leads to resolution of hematoma with time.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Endo M, Higuchi M, Chiba T, Suzuki K, Inoue Y. Present state of endoscopic hemostasis for nonvariceal upper gastrointestinal bleeding. Dig Endosc. 2010;22:S31–4. doi: 10.1111/j.1443-1661.2010.00976.x. [DOI] [PubMed] [Google Scholar]
- 2.Laine L, McQuaid K. Endoscopic therapy for bleeding ulcers: An evidence-based approach based on meta-analyses of randomized controlled trials. Clin Gastroenterol Hepatol. 2009;7:33–47. doi: 10.1016/j.cgh.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 3.Voss M, Bass DH. Traumatic duodenal haematoma in children. Injury. 1994;25:227–30. doi: 10.1016/0020-1383(94)90067-1. [DOI] [PubMed] [Google Scholar]
- 4.Karjoo M, Luisiri A, Silberstein M, Kane RE. Duodenal hematoma and acute pancreatitis after gastrointestinal endoscopy. Gastrointest Endosc. 1994;40:493–5. doi: 10.1016/s0016-5107(94)70219-5. [DOI] [PubMed] [Google Scholar]
- 5.Zinelis SA, Hershenson LM, Ennis MF, Boller M, Ismail-Beigi F. Intramural duodenal hematoma following upper gastrointestinal endoscopic biopsy. Dig Dis Sci. 1989;34:289–91. doi: 10.1007/BF01536064. [DOI] [PubMed] [Google Scholar]
- 6.Kaw D, Malhotra D. Platelet dysfunction and end-stage renal disease. Semin Dial. 2006;19:317–22. doi: 10.1111/j.1525-139X.2006.00179.x. [DOI] [PubMed] [Google Scholar]
- 7.Jalihal A, Chong VH. Duodenal perforations and haematoma: Complications of endoscopic therapy. ANZ J Surg. 2009;79:767–8. doi: 10.1111/j.1445-2197.2009.05078.x. [DOI] [PubMed] [Google Scholar]
- 8.Yen HH, Chen YY. Duodenal intramural hematoma and delayed perforation: Rare but fatal complication of endoscopic therapy for a bleeding duodenal ulcer. Endoscopy. 2009;41:E119. doi: 10.1055/s-0029-1214655. [DOI] [PubMed] [Google Scholar]
- 9.Sugai K, Kajiwara E, Mochizuki Y, Noma E, Nakashima J, Uchimura K, et al. Intramural duodenal hematoma after endoscopic therapy for a bleeding duodenal ulcer in a patient with liver cirrhosis. Intern Med. 2005;44:954–7. doi: 10.2169/internalmedicine.44.954. [DOI] [PubMed] [Google Scholar]
- 10.Chung S, Park CW, Chung HW, Shin SJ, Chang YS. Intramural duodenal hematoma and hemoperitoneum after endoscopic treatment in a patient with chronic renal failure on hemodialysis: A report. Cases J. 2009;2:9083. doi: 10.1186/1757-1626-2-9083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Degiannis E, Boffard K. Duodenal injuries. Br J Surg. 2000;87:1473–9. doi: 10.1046/j.1365-2168.2000.01594.x. [DOI] [PubMed] [Google Scholar]
- 12.Cheung J, Yu A, LaBossiere J, Zhu Q, Fedorak RN. Peptic ulcer bleeding outcomes adversely affected by end-stage renal disease. Gastrointest Endosc. 2010;71:44–9. doi: 10.1016/j.gie.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Chalasani N, Cotsonis G, Wilcox CM. Upper gastrointestinal bleeding in patients with chronic renal failure: Role of vascular ectasia. Am J Gastroenterol. 1996;91:2329–32. [PubMed] [Google Scholar]


