Abstract
Context:
Body mass index (BMI), serum albumin, and C-reactive protein (CRP) appear to be major determinants of hospitalization.
Aim:
To determine the predictive ability of BMI, Sequential Organ Failure Assessment (SOFA score), serum albumin, and CRP to assess the duration and outcome of mechanical ventilation (MV).
Materials and Methods:
Thirty patients aged >18 years who required mechanical ventilation (MV) were enrolled for the study. They were divided into two groups; patients who improved (Group 1), patients who expired (Group 2). Group 1 was further divided into two groups: patients on MV for <5 days (Group A), and patients on MV for >5days (Group B). BMI and SOFA score were calculated, and serum albumin and CRP were estimated.
Results and Discussion:
Out of the 30 patients, 18 patients successfully improved after MV (Group 1) and 12 patients expired (Group 2). Among the 18 patients in group 1, ten patients improved within 5 days (Group A) and 8 patients after 5 days (Group B). SOFA score and CRP were significantly increased (P value 0.0003 and 0.0001, respectively) in group 2 when compared to group 1. CRP >24.2 mg/L or SOFA score >7 at the start of MV increases the probability of mortality by factor 13.08 or 3.92, respectively The above parameters did not show any statistical difference when group A was compared to group B.
Conclusion:
Simple, economic and easily accessible markers like CRP and assessment tools of critically ill patients with SOFA score are important determinants of possible outcomes of a patient from MV.
Keywords: Body mass index, C-reactive proteins, mechanical ventilation, SOFA score, serum albumin
Introduction
Endotracheal intubation and mechanical ventilation (MV) is the standard supportive therapy for acute respiratory failure (ARF).[1] Prolonged endotracheal intubation has become the standard of care in most intensive care units (ICUs) for maintenance of MV. Unfortunately, this approach is associated with significant morbidity and mortality.[2] In critically ill patients suffering from ARF, weaning from ventilatory assistance is a key survival factor.[3] Despite the efficacy of MV, there are still patients in whom positive pressure ventilation is not successful in preventing further deterioration of respiratory function.
Clinical trials and observational studies usually use scoring systems for the assessment of the severity of organ function impairment. One of most popular among them is the Sequential Organ Failure Assessment (SOFA) score.[4] SOFA is composed of scores from six organ systems (respiratory, cardiovascular, hepatic, coagulation, renal, and neurological) graded from 0 to 4 according to the degree of dysfunction/failure.
However, the prediction of MV duration is difficult and has been studied by few authors. A retrospective study done on elective cardiac surgical patients showed that vital capacity, forced expiratory volume in one second (FEV1) and arterial oxygen pressure, before surgery, predict the duration of MV.[5] Moreover, for emergent intubation, respiratory parameters cannot be measured before the tracheal intubation. Established prognostic factors such as nutritional depletion as assessed by body mass index (BMI) and serum albumin levels and overall systemic inflammation as estimated by C-reactive protein (CRP) appear to be major determinants of hospitalization and death risk whatever the end-stage respiratory disease.[6] Increased CRP levels are strongly and independently associated with respiratory impairment.[7] A higher CRP value was associated with the development of respiratory failure and subsequent intubation in patients with probable severe acute respiratory syndrome (SARS).[8] Hence, the severity of inflammatory response and impairment of organ function are the major determinants of the outcome in critically ill patients.
The predictive ability of SOFA score, BMI, CRP or serum albumin as a simple, inexpensive, and dynamic marker of critical illness in patients requiring MV has been studied by few authors. Hutter et al. study had showed that the group of patients that failed non invasive positive pressure ventilation had a mean BMI of 23 kg/m2, which is relatively under weight. However, authors have not correlated BMI with the duration and outcome of mechanical ventilation.[9] Studies done on chronic obstructive pulmonary disease have shown that patients with low BMI and nutritional depletion tend to have poor prognosis.[10–12] Also high CRP levels have been associated with development of respiratory failure and subsequent intubation in patients with probable severe acute respiratory syndrome.[7,8] Frequency of hospitalization in COPD patients have been found to be independently determined by elevated CRP.[6] It has also been shown that BMI of < 23.3 kg/m2 and CRP of >10 mg/L is an independent predictor of more than seven days duration of MV.[13] However, in this study only the patients who had improved were included in the study. We wanted to study whether these parameters can be used to predict mortality of the patients with acute respiratory distress on mechanical ventilation. Hence, this study was designed to determine the presence of a relationship between the SOFA score, BMI, CRP, serum albumin with the duration and outcome of the patients with acute respiratory distress on MV.
Materials and Methods
Type of study
Prospective follow-up study
Inclusion criteria
Thirty patients (age >18 years) admitted to the ICU of tertiary care hospital and who required mechanical ventilation were enrolled for the study. They were divided into two groups; patients who improved (Group 1), patients who expired (Group 2). Group 1 was further divided into two groups; patients on mechanical ventilator for <5 days (Group A), patients on mechanical ventilator for >5days (Group B). Approval from the institutional ethical committee was taken before commencement of the study. Written consent was taken from the patient relatives before collection of blood. Patients without neuromuscular diseases, left ventricular dysfunction, chest or abdominal trauma, hypokalemia, hypophosphatemia, hypomagnesemia, chest pain or suspected myocardial infarction, coronary bypass surgery, burn injury or any addiction, no history of exacerbation of chronic respiratory failure during the last 3 months were included in the study.
Sample size
The study was conducted for a period of two months between June 2009 and July 2009. In these two months, there were 76 admissions to the ICU. Out of these, 35 had acute respiratory distress and were intubated. Five were excluded from the study as they did not meet the inclusion criteria. Hence, thirty patients were included in the study.
Data collected from the patients record included age, sex, BMI (kg/m2), SOFA score, underlying disease, documentation of the need for MV, and duration of MV. Strict intake/output chart was maintained for all the patients to estimate their fluid balance. The ICU staffs ensured that all the patients maintained adequate fluid balance. Venous blood was collected within 24 hours after the patient was put on MV and centrifuged at 3000 rpm for 10 minutes and serum was used immediately for the estimation of serum albumin and CRP. Serum albumin was determined by bromocresol green method in Randox Daytona fully automated chemistry analyzer and CRP levels were determined by enzyme-linked immunosorbent assay.
Duration of mechanical ventilation
Duration of MV was calculated from the time the patient was intubated and connected to ventilator till the time he was disconnected from the ventilator. A combination of subjective and objective parameters were used to wean the patient from MV. The objective parameters used were: a) PaO2/FiO2 > 150-200; b) level of positive end expiratory pressure (PEEP) between 5-8 cm H2O; c) FiO2 level <50%; d) pH > 7.25; e) ability to initiate spontaneous breaths. The subjective parameters used were: a) hemodynamic stability; b) absence of active myocardial ischemia; c) absence of clinically significant vasopressor requiring hypotension; d) adequate muscular strength allowing the capability to initiate/sustain the respiratory effort.
Statistical analysis
Arithmetic mean and SD were estimated to assess the level of various parameters in the study. Differences in the outcome from MV, BMI, CRP, serum albumin, and SOFA score between the defined groups were assessed using the Mann–Whitney nonparametric test. The nonparametric Spearman ranked sign procedure was used to assess the significance of associations. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and positive or negative likelihood ratios (+ LR) for BMI, CRP, serum albumin and SOFA score in predicting the outcome of patients from MV were calculated. Also, receiver operative characteristics (ROC) curves were constructed for each of the predictive variables and the areas under the ROC curves (AUC) were compared. The analyses were facilitated with the use of the MedCalc 11.5.1.0 software packages. Stepwise logistic regression analysis was used to determine; which of the above variable was an independent risk factor for predicting the outcome of patients from MV. Differences were considered significant if the P value was <0.05. In order to test the significance of difference among the four groups based on obesity, analysis of variance was applied at 5% level of significance.
Results
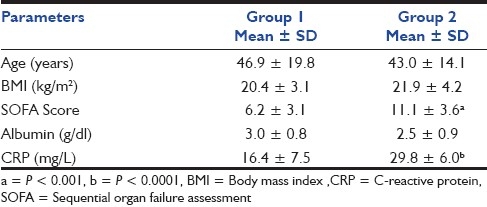
The distribution of patients in the study groups along with their mean age is shown in Table 1. Out of the 30 patients enrolled for the study, 18 patients successfully improved after mechanical ventilation support was given to them and 12 patients expired. The mean age and BMI of the patients who improved (Group 1), when compared with those who expired (Group 2), did not show any statistical significance P value 0.56 and 0.25, respectively. Serum albumin levels though decreased in group 2 when compared to group 1 was not statistically significant (P value 0.09). However, SOFA score and CRP were highly increased in group 2 when compared to group 1 (P value 0.0004 and 0.0001, respectively) [Table 2].
Table 1.
Number of patients, mean age and percentage of the patients in the three groups
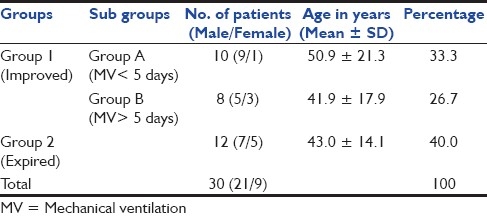
Table 2.
Mean and standard deviation of different parameters in the two groups based on their outcome from mechanical ventilation
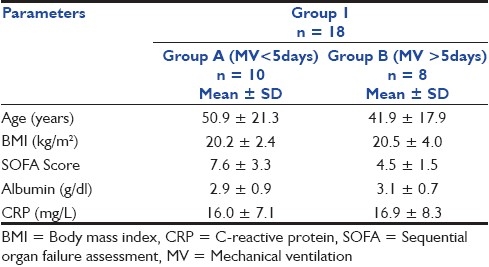
Out of the 18 patients in group 1, 10 patients improved within 5 days and 8 improved after 5 days. The mean age of the patients belonging to the two groups were comparable and did not show any statistical significance (P value >0.48). Also, mean BMI, serum albumin, CRP, and SOFA score did not show any statistical significance in the two groups [Table 3].
Table 3.
Mean and standard deviation of different parameters in the group 1 patients when they were further divided into two groups based on the duration of MV
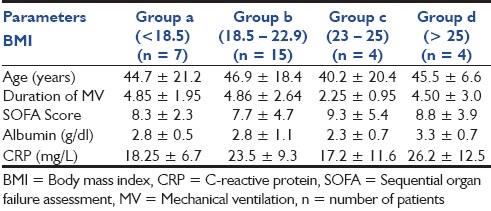
When patients were classified based on the Indian Standards of BMI,[14] 50% of the patients had normal BMI (BMI: 18.5 to 22.9), 23.3% of the patients were under weight (BMI <18.5), 13.3% of the patients were overweight (BMI 23-25), and 13.3% were obese (BMI >25). Age, duration of MV, SOFA score, and serum albumin and CRP levels did not show any statistical difference in the four groups based on the Indian standar5ds of BMI [Table 4].
Table 4.
Mean and standard deviation of different parameters in the four groups based on the indian standards of body mass index
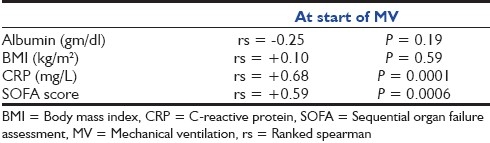
The sensitivity, specificity, PPV, NPV, positive or negative LR and area under the ROC curve (AUC) to predict the outcome of the patient from MV is shown in Table 5 and Figure 1. CRP had high specificity or PPV for predicting the outcome from MV. The SOFA score had high sensitivity or NPV for this purpose. The AUC for CRP or SOFA score was not significantly different (P > 0.05). CRP >24.2 mg/L or SOFA score >7 at the start of MV increases the probability of mortality by factor 13.08 or 3.92, respectively. By performing stepwise logistic regression analysis, it was shown that the most powerful predictor of outcome of patients from MV was SOFA score. An increase of 1 in SOFA score significantly increased the relative probability of mortality by a factor of 1.662 (95% CI, 1.1659-2.3707, P = 0.005). Also, by performing Spearman ranked correlations it was seen that CRP and SOFA score at the start of MV showed highest correlation with the mortality (rs = 0.68 and rs = 0.59, respectively). The association was negative with serum albumin concentration [Table 6].
Table 5.
Predictive ability of BMI, CRP, albumin, and SOFA score for outcome of the patients from MV
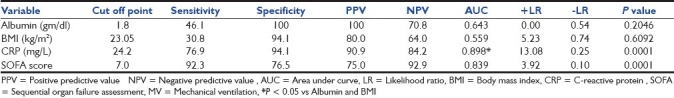
Figure 1.
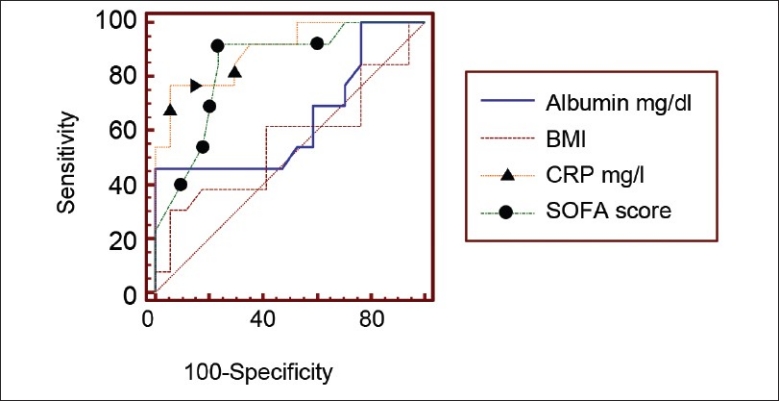
Receiver operator characteristic curves for each of the predictive variables
Table 6.
Association of SOFA score, BMI, CRP, and serum albumin with the outcome of patients from MV (Spearman ranked correlations)
Discussion
The severity of inflammatory response and impairment of organ function are the major determinants of the outcome in critically ill patients.[15,16] With an increase in the number of overweight and obese patients admitted to the ICU, morbidity and mortality have become a concern for the ICU physicians. In our study, CRP showed a significant relationship with the outcome of patient from MV. The level of CRP, which is a marker of inflammation, is known to increase in conditions in which the body is under stress. Their levels were more or less the same in patients who improved after being on mechanical ventilation regardless of the duration they required for improvement as shown in Table 3. On the other hand, patients in group 2 who had very high levels of CRP could not survive even after being on mechanical ventilation as shown in Table 2. However, BMI did not have significant relation with either the duration of MV or the outcome of patient from MV. The serum albumin was comparatively higher in patients who responded to mechanical ventilation successfully than those who expired. However, it was not statistically significant as indicated in Table 2. Patients who had a lower SOFA score had better chances of weaning indicating that overall Systemic Organ Failure may lead to death even after prolonged ventilation. So calculation of SOFA score is helpful in predicting the outcome of the patient on mechanical ventilator. Similarly, patients who have a higher SOFA score could not survive [Table 2] indicating that SOFA score can act as a good predictor of outcome from MV.
Several studies have shown that the two major determinants of outcome in patients with end-stage respiratory disease were BMI and CRP.[6,9,17] It has been shown that the patients who failed noninvasive positive pressure ventilation had a mean BMI of 23 kg/m2 , which is relatively underweight. Also, for each 1-point increase in BMI, there was a 29% decrease in the risk of endotracheal intubation and MV. Lower muscle mass makes it more likely that a patient will become dependent on MV and less likely that a patient will have effective cough. In addition to this, it has been shown that critically ill patients in overweight and obese categories have a better survival and discharge functional status.[18] However, in our study when the patients were classified into four groups based on their BMI there was no significant difference in their duration of mechanical ventilation, serum albumin and CRPs as shown in Table 4. This could probably be due to the small sample size involved in the study group. The serum albumin concentration in COPD patients with acute respiratory failure who require MV was associated with survival and successful weaning.[19] The albumin and blood glucose are possible indexes of the metabolic status of trauma patient, which could be essential in deciding the need for ventilator and weanable status of the patients who are mechanically ventilated for extended periods of time.[20] However, in our study serum albumin levels did not show any significant association with duration as well as outcome of the patient on MV.
A strong and independent association of increased CRP and respiratory failure were shown in several studies.[7,8] The relationship between CRP and prognosis is also well recognized in chronic respiratory failure. Also the circulating blood levels of several inflammatory cytokines and acute phase proteins were higher in patients with stable chronic obstructive pulmonary disease.[21] Hornarmand et al showed that both BMI and CRP when compared with the SOFA score, can be used in estimating the risk of prolonged MV and concluded that BMI <23.3 kg/m 2 or CRP >10 mg/L at the time of discontinuation of MV were independent predictors of more than seven days duration of MV. Also, an increase of 1 in CRP-2 or BMI-2 significantly increased the relative probability of >7 days of MV by a factor 1.454 or 1.201, respectively.[13] These data confirm the association of systemic inflammation with respiratory failure. However, in our study CRP >24.2 mg/L or SOFA score >7 at the start of MV showed an increased probability of mortality by factor 13.08 or 3.92 respectively. More severe the organ injury, as implicated by the SOFA score calculation, higher the CRP levels. Also, elevated concentrations of serum CRP correlated well with mortality as shown in Table 6. There is an increasing body of evidence supporting the critical role of the vascular endothelium in the pathogenesis of multiple organ failure in critically ill patients.[22,23] CRP can act directly on endothelial cells, inducing the production of inflammatory cytokines. These data show that measuring serum CRP level during the period of MV acts as a marker for predicting risk of organ failure and subsequent outcome of the patient from mechanical ventilation.
Limitation of the study
Small sample size is the limitation of the study. Therefore, large-scale, multi-centric, prospective epidemiologic studies must be conducted to confirm and validate the findings of this preliminary study.
Conclusions
Simple, economic and easily accessible markers like CRP and assessment tools of critically ill patients with SOFA score are important determinants of possible outcomes of a patient from MV.
Acknowledgments
The study was done as a part of ICMR-STS 2010
Footnotes
Source of Support: Indian Council for Medical Research, New Delhi, India.
Conflict of Interest: None declared.
References
- 1.Bott J, Carroll MP, Conway JH, Keilty SE, Ward EM, Brown AM, et al. Randomised controlled trial of nasal ventilation in acute ventilatory failure due to chronic obstructive airways disease. Lancet. 1993;341:1555–7. doi: 10.1016/0140-6736(93)90696-e. [DOI] [PubMed] [Google Scholar]
- 2.Stauffer JL, Fayter NA, Graves B, Cromb M, Lynch JC, Goebel P. Survival following mechanical ventilation for acute respiratory failure in adult men. Chest. 1993;104:1222–9. doi: 10.1378/chest.104.4.1222. [DOI] [PubMed] [Google Scholar]
- 3.Schlossmacher P, Hasselmann M, Meyer N, Kara F, Delabranche X, Kummerlen C, et al. The prognostic value of nutritional and inflammatory indices in critically ill patients with acute respiratory failure. Clin Chem Lab Med. 2002;40:1339–43. doi: 10.1515/CCLM.2002.231. [DOI] [PubMed] [Google Scholar]
- 4.Plummer AL, Gracey DR. Consensus conference on artificial airways in patients receiving mechanical ventilation. Chest. 1989;96:178–80. doi: 10.1378/chest.96.1.178. [DOI] [PubMed] [Google Scholar]
- 5.Durand M, Combes P, Eisele JH, Contet A, Blin D, Girardet P. Pulmonary function tests predict outcome after cardiac surgery. Acta Anaesth Belg. 1993;44:17–23. [PubMed] [Google Scholar]
- 6.Cano NJ, Pichard C, Roth H, Court-Fortuné I, Cynober L, Gérard-Boncompain M, et al. C-reactive protein and body mass index predict outcome in end-stage respiratory failure. Chest. 2004;126:540–6. doi: 10.1378/chest.126.2.540. [DOI] [PubMed] [Google Scholar]
- 7.Kony S, Zureik M, Driss F, Neukirch C, Leynaert B, Neukirch F. Association of bronchial hyperresponsiveness and lung function with C-reactive protein (CRP): A population based study. Thorax. 2004;59:892–6. doi: 10.1136/thx.2003.015768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu CY, Huang LJ, Lai CH, Chen HP, Chen TL, Fung CP, et al. Clinical characteristics, management and prognostic factors in patients with probable severe acute respiratory syndrome (SARS) in a SARS center in Taiwan. J Chin Med Assoc. 2005;68:110–7. doi: 10.1016/S1726-4901(09)70231-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hutter DA, Holland BK, Ashtyani H. The effect of body mass index on outcomes of patients receiving noninvasive positive-pressure ventilation in acute respiratory failure. Respir Care. 2004;49:1320–5. [PubMed] [Google Scholar]
- 10.Chailleux E, Fauroux B, Binet F, Dautzenberg B, Polu JM. Predictors of survival in patients receiving domiciliary oxygen therapy or mechanical ventilation.A 10-year analysis of ANTADIR observatory. Chest. 1996;109:741–9. doi: 10.1378/chest.109.3.741. [DOI] [PubMed] [Google Scholar]
- 11.Gray-Donald K, Gibbons L, Shapiro SH, Macklem PT, Martin JG. Nutritional status and mortality in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1996;153:961–6. doi: 10.1164/ajrccm.153.3.8630580. [DOI] [PubMed] [Google Scholar]
- 12.Chailleux E, Laaban JP, Veale D. Prognostic value of nutritional depletion in patients with COPD treated by long-term oxygen therapy: Data from the ANTADIR observatory. Chest. 2003;123:1460–6. doi: 10.1378/chest.123.5.1460. [DOI] [PubMed] [Google Scholar]
- 13.Honarmand A, Safavi M. Do C-reactive protein and body mass index predict duration of mechanical ventilation in critically ill trauma patients? Ulus Travma Acil Cerrahi Derg. 2008;14:284–91. [PubMed] [Google Scholar]
- 14.Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, et al. Consensus Statement for Diagnosis of Obesity, Abdominal Obesity and the Metabolic Syndrome for Asian Indians and Recommendations for Physical Activity, Medical and Surgical Management. J Assoc Physicians India. 2009;57:163–70. [PubMed] [Google Scholar]
- 15.Angus DC, Wax RS. Epidemiology of sepsis: An update. Crit Care Med. 2001;29:S109–16. doi: 10.1097/00003246-200107001-00035. [DOI] [PubMed] [Google Scholar]
- 16.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 17.Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:1005–12. doi: 10.1056/NEJMoa021322. [DOI] [PubMed] [Google Scholar]
- 18.Tremblay A, Bandi V. Impact of body mass index on outcomes following critical care. Chest. 2003;123:1202–7. doi: 10.1378/chest.123.4.1202. [DOI] [PubMed] [Google Scholar]
- 19.Menzies R, Gibbons W, Goldberg P. Determinants of weaning and survival among patients with COPD who require mechanical ventilation for acute respiratory failure. Chest. 1989;95:398–405. doi: 10.1378/chest.95.2.398. [DOI] [PubMed] [Google Scholar]
- 20.Safavi M, Honarmand A. The impact of admission hyperglycemia or hypoalbuminemia on need ventilator, time ventilated, mortality and morbidity in critically ill trauma patients. Ulus Travma Acil Cerrahi Derg. 2009;15:120–9. [PubMed] [Google Scholar]
- 21.Malo O, Sauleda J, Busquets X, Miralles C, Noguera A. Systemic inflammation during exacerbations of chronic obstructive pulmonary disease. Arch Bronconeumol. 2002;38:172–6. [PubMed] [Google Scholar]
- 22.Levi M, ten Cate H, van der Poll T. Endothelium: Interface between coagulation and inflammation. Crit Care Med. 2002;30:S220–4. doi: 10.1097/00003246-200205001-00008. [DOI] [PubMed] [Google Scholar]
- 23.WC The role of the endothelium in severe sepsis and multiple organ dysfunction syndrome. Blood. 2003;101:3765–77. doi: 10.1182/blood-2002-06-1887. [DOI] [PubMed] [Google Scholar]


