Abstract
The goal of the current study was to examine how social support and coping strategies are related in predicting emotional well-being of women with breast cancer. In achieving this goal, we examined two hypothesized models: (1) a moderation model where social support and coping strategies interact with each other in affecting psychological well-being; and (2) a mediation model where the level of social support influences choices of coping strategies between self-blame and positive reframing. In general, the data from the current study were more consistent with the mediation model than the moderation model.
Keywords: breast cancer, coping strategies, emotional well-being, mediator, moderator, social support
WOMEN with breast cancer feel diverse physical concerns as well as emotional problems such as distress, anxiety, or depression (Spiegel, 1997). As a way to reduce these problems and increase their quality of life, women with breast cancer have been found to rely on a diverse range of coping mechanisms, which are known to reduce distress (e.g. Han et al., 2008). Another line of research has demonstrated positive effects of social support on physical and psychological well-being of people suffering from chronic illness such as cancer (Helgeson & Cohen, 1996), coronary heart disease (Uchino, Cacioppo, & Kiecolt-Glaser, 1996) and diabetes (Cheng & Boey, 2000). People who have received much social support have shown lower degrees of depression and other negative moods caused by physical illness (e.g. Brown, Wallston, & Nicassio, 1989).
Although social support has been shown to improve patients’ emotional well-being, the process through which social support influences emotional well-being has not been adequately explored. Among many possible variables that can work with social support in increasing or decreasing emotional well-being, coping strategies deserve further attention. It has been suggested that the levels or quality of social support are associated with coping strategies in influencing emotional or physical well-being (e.g. Swindells et al., 1999). However, researchers have used different approaches in investigating the relationship between the two: one group of studies has treated social support and coping strategies as independent predictors for emotional well-being without being associated with each other (e.g. Lopez-Martinez, Esteve-Zarazaga, & Ramirez-Maestre, 2008), another group of studies indicated that they have an interactive effect on emotional well-being (e.g. Griffin, Friend, Kaell, & Bennett, 2001), and still another group of studies has suggested that coping strategies mediate the relationship between social support and emotional well-being (e.g. Holtzman, Newth, & DeLongis, 2004).
Because there has been a lack of consistency in explaining the inter-relationships between social support, coping strategies, and emotional well-being, the main goal of the current study was to clarify the association between coping strategies and social support in increasing or decreasing emotional well-being of women with breast cancer. In order to achieve this goal, we investigated and contrasted two models—a moderation model where coping strategies interact with perceived social support in affecting emotional well-being, and a mediation model where perceived social support influences the choice of specific coping strategies, which leads to emotional well-being. Further, we examined which of these two models can best explain the relationships among our focal variables.
Self-blame and positive reframing as coping strategies
Coping refers to ‘cognitive and behavioral efforts made to master, tolerate, or reduce external and internal demands and conflicts’ (Folkman & Lazarus, 1980, p. 223). There are many ways to categorize coping strategies. One of the most commonly used categories is active coping versus passive/avoidant coping (Carrico et al., 2006). Active coping efforts are aimed at facing a problem directly and determining possible viable solutions to reduce the effect of a given stressor. Meanwhile, passive/avoidant coping refers to behaviors that seek to escape the source of distress without confronting it (Folkman & Lazarus, 1984). Setting aside the nature of individual patients or specific external conditions, there have been consistent findings that the use of active coping strategies produce more favorable outcomes compared to passive coping strategies, such as less pain as well as depression, and better quality of life (e.g. Holmes & Stevenson, 1990). On the other hand, relying on passive/avoidant coping strategies is associated with increased depression and anxiety (e.g. Clement & Schonnesson, 1998).
Among diverse coping strategies (Carver, 1997), this study focuses on two—self-blame (e.g. ‘I have been criticizing myself’) and positive reframing (e.g. ‘I have been trying to see it in a different light, to make it seem more positive’). These two coping strategies were most relevant to this study’s theoretical contexts and expected to have opposing effects on emotional well-being. Self-blame has been categorized as a type of passive/avoidant coping strategy (e.g. Schwartz et al., 2008). Some studies confirmed this categorization of self-blame as a passive coping strategy by demonstrating that self-blame or focusing on themselves had a significantly positive association with psychological distress of surgical breast cancer patients (e.g. David, Montgomery, & Bovbjerg, 2006; Shaw, Han, Hawkins, McTavish, & Gustafson, 2008). Meanwhile, positive reframing is a type of active coping strategy, which has been also confirmed by Carver et al.’s (1993) study showing a significant negative relationship between positive reframing and emotional distress of women who were diagnosed with breast cancer.
Social support
Social support refers to support received (e.g. informative, emotional, or instrumental) or the sources of the support (e.g. family or friends) that enhance recipients’ self-esteem or provide stress-related interpersonal aid (Dumont & Provost, 1999). Social support has been known to offset or moderate the impact of stress caused by illness (e.g. Aro, Hanninen, & Paronene, 1989). Specifically for breast cancer patients, social support has been found to reduce stress associated with a cancer diagnosis (e.g. Israel & Schurman, 1990), bring positive changes in their lives (e.g. Bozo, Gundogdu, & Buyukasik-Colak, 2009), and improve emotional well-being (e.g. Dunkel-Schetter, 1984; Holland & Holahan, 2003).
Social support and coping strategies
As mentioned above, previous studies on the relationship between social support and coping strategies have not been consistent. One way to look at how social support and coping strategies might work in combination is to look at an interactive effect between these two factors on emotional well-being. In this model, the selection of specific coping strategies might not be driven by the levels or quality of social support, but coping strategies may moderate the relationship between social support and emotional well-being. This perspective assumes that coping strategies are considered as a style or type of inherent trait that are not induced or affected by external factors (e.g. social support) (Lazarus, 1993). There are a few studies that have looked at the interactive effect of social support and coping strategies on physical or emotional well-being of patients. One study by Griffin and colleagues (2001) showed rheumatoid arthritis patients who cope by venting their emotions exhibited poorer physical well-being when they did not perceive healthy or positive social support from close others. Another study by Noh and Kaspar (2003) suggested that the use of emotion-focused coping reduced depression if people were supported by their ethnic community members, while emotional coping exacerbated depression when ethnic community support was not available.
While the two studies referred to above selected the level of social support as a moderator, the current study treats social support as an independent variable and coping strategies as moderators. Still, those previous studies and the current study share the same assumption that there is no causal relationship between social support and coping strategies. Considering that positive reframing has been known to reduce emotional distress while self-blame tends to intensify it, we expect that the positive effect of social support on psychological well-being would be more pronounced among people who use positive framing more and those who use self-blame less.
H1: The association between perceived social support and emotional well-being is moderated by their choice of coping strategies in the way that the positive effect of social support on psychological well-being will be more pronounced for those using positive reframing more and those using self-blame less.
On the other hand, the current study examined another possibility that the relationship between social support and emotional well-being can be mediated by different coping strategies selected by individuals (e.g. Holland & Holahan, 2003), that is, perceived social support would influence people to rely on different types of coping strategies, and the different coping strategies chosen by them would affect their emotional well-being differently. This perspective assumes that perceived social support affects people’s choice or use of specific coping strategies, which can either boost up or reduce the impact of social support on emotional well-being. Here, coping is considered as a process or state that can be affected over time by external factors (e.g. social support) (Lazarus, 1993).
There have been a small group of studies indicating the existence of indirect effects between social support and emotional well-being through the use of specific coping strategies (e.g. Holtzman et al., 2004). A possible rationale behind this argument is that social support can work as coping assistance (O’Brien & DeLongis, 1997; Thoits, 1986). For example, a high level of social support turned out to improve emotional well-being of patients with cardiac disease both directly and indirectly through encouraging the use of positive reassessment of their physical conditions (Holohan, Moos, Holohan, & Brennan, 1995). Park, Edmondson, Fenster, and Blank (2008) also have shown that cancer survivors who perceive high levels of social support tend to choose active coping strategies and have more positive changes in their health behaviors. In the context of breast cancer, Holland and Holahan (2003) found that breast cancer patients who perceived high levels of social support made greater use of positive reappraisal, and planned problem-solving as their coping strategies, which eventually led to higher levels of emotional well-being. Concurring with these studies’ assumption that perceived social support would affect their choice of specific coping strategies, the current study predicts that the relationship between social support and emotional well-being will be mediated by their choice of an active coping strategy (i.e. positive reframing) or a passive coping strategy (i.e. self-blame).
H2: The more social support people perceive: (a) the more they will use positive reframing as a coping strategy; and (b) the less they will use self-blame as a coping strategy.
H3: The association between perceived social support and emotional well-being is mediated by their choice of positive reframing or self-blame as their coping strategies.
In testing the mediation model, the current study also investigated which indirect path is stronger than the other—the indirect effect through self-blame or the indirect effect through positive reframing (Research Question 1).
Methods
Sample
The data analyzed in the current study consisted of 231 underserved women (i.e. income being at or below 250 percent of poverty; for a single woman < $21,475/year, family of four < $44,125/year) with breast cancer. Recruitment took place between May 2001 and April 2003 from rural Wisconsin and Detroit, Michigan. These participants were part of a larger eHealth intervention evaluating the Comprehensive Health Enhancement Support System (CHESS) ‘Living with Breast Cancer’ program, an Internet-based information and support system designed to help people facing a health crisis. Prior to the start of the intervention, participants filled out a baseline survey that assessed patients’ coping strategies (including self-blame, positive reframing), their perceived level of social support, and quality of life outcomes, along with demographic and disease-related characteristics. The hypotheses proposed above were tested by analyzing data collected as part of this baseline survey.
Study participants had a mean age of 51 years and diverse educational backgrounds, with 42.4 percent having a high school education or less, 29.9 percent having attended some college, 24.2 percent were college graduates, and 3.5 percent attended graduate school. A total of 27.3 percent lived alone and 70.1 percent were classified as early stage of cancer (0–2) and 29.9 percent classified as late stage of cancer (3–4). In addition, 62.3 percent were Caucasian women, 35.9 percent African American, and 1.7 percent other minorities.
Measures
Besides basic demographic information, participants answered our primary measures at pretest. These measures have been widely tested and demonstrated in terms of reliability, validity, and responsiveness to clinical change (Gustafson et al., 2005). For all measures, scale scores are calculated as averages across scale items.
Emotional well-being
A six-item emotional well-being subscale of the Functional Assessment of Cancer Therapy-Breast (FACT-B) (M = 2.45, SD = 1.00) asked, on a five-point scale ranging from 0 = not at all to 4 = very much, how often participants had felt, for example, sad, or nervous (Gustafson et al., 2005). These items were reversed before computing an emotional well-being scale (Cronbach’s α = .86).
Social support
Social support (M = 2.95, SD = .86), which was developed from previous studies (Gustafson et al., 2005), was created using six items (Cronbach’s α = .87) that asked respondents, on a five-point scale ranging from 0 = not at all to 4 = very much, for example, if there are people they could count on for emotional support, or if there are people they could rely on when they need help doing something.
Positive reframing
Positive reframing (M = 2.88, SD =.94) was created using two items (Cronbach’s α = .70) that asked respondents, on a four-point scale ranging from 1 = I haven’t been doing this at all to 4 = I’ve been doing this a lot, if they have been trying to see breast cancer in a different light, and if they have been looking for something good in what is happening. Positive reframing was a coping strategy measured with the Brief Cope (Carver, 1997), a shorter version of the original 60-item COPE scale developed by Carver et al. (1993), which has strong evidence for its validity and reliability.
Self-blame
A two-item self-blame scale (M = 1.81, SD = .89) was also adopted from the Brief Cope scale (Carver, 1997). Respondents are asked, on a four-point scale ranging from 1 = I haven’t been doing this at all to 4 = I’ve been doing this a lot, if they have been criticizing themselves, and if they have been blaming themselves for things that happened (Cronbach’s α = .80).
Control variables
In order to verify control variables, first of all, bivariate correlation analysis was run with five demographic variables and four focal variables mentioned above. While age and education level were coded as ratio and ordinal scales respectively, race (1 = Caucasian, 0 = non-Caucasian), living status (1 = living alone, 0 = not living alone), cancer stage (1 = early stage, 0 = later stage) were coded as dichotomous variables. Age, race, and cancer stage turned out to be significantly related to at least one of the four focal variables. To reduce confounding effects, these three variables and education were controlled when testing the moderation and mediational models.
Results
Zero-order correlations
Highly significant and positive correlations were found between social support and emotional well-being (r = .34, p < .001), between positive reframing and emotional well-being (r = .34, p < .001), and between positive reframing and social support (r = .29, p < .001). There were significant but negative correlations between self-blame and emotional well-being (r = –.49, p < .001) and between self-blame and social support (r = –.40, p < .001). No significant correlation was found between the two coping strategies (r = –.09, p = .17).
Moderation model
The moderation model was tested by a hierarchical multiple regression analysis. Four control variables (i.e. age, race, education, and cancer stage) were entered in the first block, followed by main effect variables (second block), and interaction terms (third block). In order to reduce multicollinearity that could be augmented by creating interaction terms, social support and two coping strategy variables were centered before computing the interaction terms. The main effects of self-blame and positive reframing coping strategies were significant. In accordance with previous literature, self-blame is negatively related to emotional well-being (β = −.40, p < .001), while positive reframing is positively related to emotional well-being (β = .16, p = .002). The interaction between social support and positive reframing was barely significant (β = −.11, p = .049), but the overall R-square change of the interaction term block was not significant (see Table 1).
Table 1.
Hierarchical regression analysis for social support and coping strategies predicting emotional well-being of women with cancer (N = 231)
| Variables | β | t-value |
|---|---|---|
| Step 1 | ||
| Age | .14* | 2.66 |
| Race | .03 | .57 |
| Cancer stage | −.09 | −1.63 |
| Education | .08 | 1.53 |
| Step 2 | ||
| Social support | .23** | 3.73 |
| Self-blame | −.40** | −6.69 |
| Positive reframing | .16** | 3.10 |
| Step 3 | ||
| Social support × Self-blame | −.05 | −.64 |
| Social support × Positive reframing | −.11* | −2.00 |
Notes: F (8, 217) = 18.58, p < .001, adjusted R2 = .39. ΔR2 of control variable block (Step 1) = .05, ΔF(3, 222) = 4.04**; ΔR2 of main effect block (Step 2) = .34, ΔF(3, 219) = 41.51**; ΔR2 of the interaction term block (Step 3) = .01, ΔF (2, 217) = 2.01
p < .05;
p < .01
Mediation model
In order to test the overall fit of the hypothesized mediation model, structural equation modeling (SEM) (EQS 6.1, Bentler, 2006) was used. SEM allows us to test all components of the mediation model simultaneously. As a way to control age, race, education, and cancer stage in the mediation model, residual values of all four focal variables were obtained through regressing them with the four control variables. These residuals of four focal variables, thus, are variances that are not explained by the four covariates. The mediation path model using residuals of the four focal variables showed a good fit with the data: χ2 (1, N = 231) = .10, p = .75, CFI = 1.00, NFI = 1.00, RMSEA = .00 (CI = .00, .12). As predicted by Hypotheses 2a and 2b, the path from social support to positive reframing was significantly positive, and the path from social support to self-blame was significantly negative. The fact that there was a significant total indirect effect through both positive reframing and self-blame (β = .20, p < .001) supports Hypothesis 3 (see Fig. 1).
Figure 1.
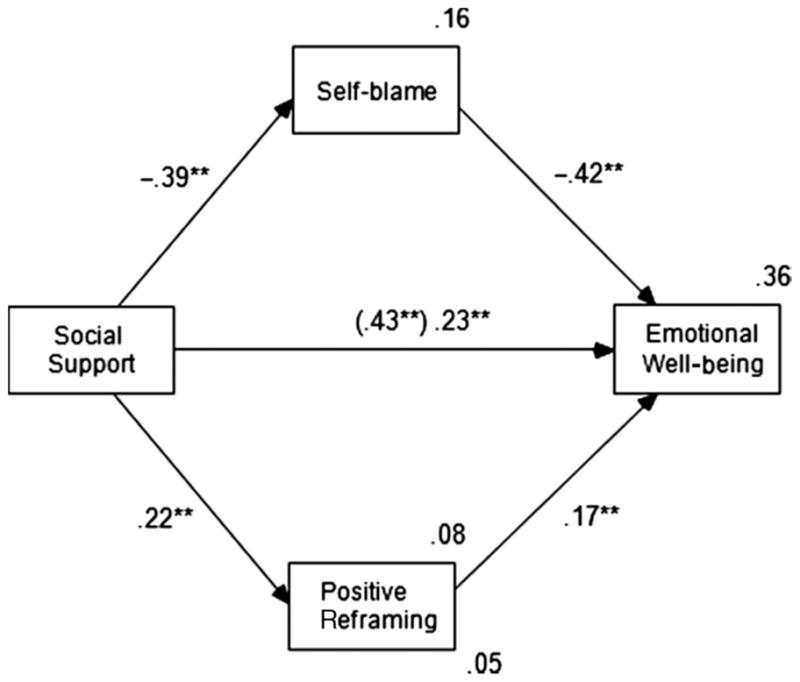
The results of path model analysis for the mediation model.
We used a multiple mediation analysis (Preacher & Hayes, 2008) for testing the significance of the indirect effects and contrasting the strengths of indirect effects through two mediators. For this analysis, the SPSS macro program developed and updated by Preacher and Hayes (2008) was used. Using this program was necessary, because EQS 6.1 only provides the size and significance of the total indirect effects through multiple mediators (i.e. the sum of all indirect effects), but does not allow for testing the significance of individual indirect effects separately or directly comparing the strengths of individual indirect effects.
The indirect effect of social support on emotional well-being mediated by self-blame showed a positive sign and was statistically significant (b = .16, Z = 4.79, p < .001). The indirect effect of social support on emotional well-being mediated by positive reframing also exhibited a positive sign and was statistically significant (b = .04, Z = 2.32, p = .02). The fact that the direct effect of social support on emotional well-being when controlling for coping strategies became smaller (β = .23, p < .001) compared to the direct effect of social support on emotional well-being without controlling for coping strategies (β = .43, p < .001) provides evidence for partial mediation through two coping strategies (Baron & Kenny, 1986). In order to answer Research Question 1, the pairwise contrast of the two indirect effects was used. The analysis result revealed that the specific indirect effect through self-blame was significantly greater than the indirect effect through positive reframing (b = .12, Z = 3.29, p = .001).
Discussion
The goal of the current study was to examine how social support and coping strategies are related in predicting emotional well-being of women with breast cancer through a joint examination of two hypothesized models regarding their association—moderation and mediation models. In general, the data from the current study were more consistent with the mediation model than the moderation model. Thus, breast cancer patients’ perception on how much social support they receive from others may influence their choice of specific coping strategies between active (i.e. positive reframing) and passive (i.e. self-blame) coping, which in turn may influence their emotional well-being. Of course, we should be cautious in unabashedly interpreting the direction of causality given our use of cross-sectional data.
Still, the findings of the current study are consistent with a group of studies indicating that social support can function as coping assistance (e.g. O’Brien & DeLongis, 1997; Thoits, 1986) in the sense that active participation of significant others can influence breast cancer patients’ efforts to manage their physical as well as emotional conditions. As suggested by Thoits (1986), significant others can suggest ways of managing physical or emotional distress caused by breast cancer, or even can participate directly in breast cancer patients’ efforts. As a result, social support can help bolster self-esteem of individuals as well as the sense of control over their situations (Brown & Harris, 1978). A strong sense of control and confidence would strengthen breast cancer patients’ own coping efforts by leading them to rely on active coping strategies (e.g. positive reframing) rather than passive/avoidance coping strategies (e.g. self-blame).
These findings have some theoretical implications for the effectiveness of social support interventions in breast cancer by expanding the role of social support in improving emotional well-being. There have been many studies looking at the direct effect of social support on breast cancer patients’ emotional well-being. The perception of adequate social support has been associated with lower levels of depression (Finch, Okun, Pool, & Ruehlman, 1999), better social adjustment (Dunkel-Schetter, 1984), and higher self-esteem (Feather & Wainstock, 1989). However, this study expands the role of social support by showing that perceived social support not only directly increases emotional well-being, but also may indirectly influence emotional well-being by affecting the choice of specific coping strategies. In that sense, the association between social support and patients’ well-being can be summarized as ‘the rich get richer’ model: the more and better social support one has, the higher chance the patient has for improving her psychological well-being through higher likelihood of selecting active coping strategies, having more confidence, and more control over her situation. Furthermore, those who have many supportive others might choose more active coping strategies, because they feel that they have more to live for.
The indirect effect of social support on emotional well-being through self-blame was significantly stronger than the indirect effect through positive reframing. This indicates that self-blame may play a significant role in diminishing people’s emotional well-being when they do not perceive a high level of social support from others, much more than positive framing does in boosting their emotional well-being when they perceive a high level of social support. Considering that lower levels of social support are associated with women with breast cancer using self-blame as their coping strategy, it may be difficult for them to maintain positive perspectives—and avoid negative ones—about their physical condition without much social support.
The current study had some limitations. Although each path of the hypothesized mediation model is theoretically warranted, the direction of causality cannot be guaranteed because of our using cross-sectional data. As suggested by Kline (2005), an alternative model was tested to rule out other plausible causality models: emotional well-being became an endogenous variable, while social support became an output. This model might also make some theoretical sense in that breast cancer patients who are emotionally healthy may choose positive reframing rather than self-blame, which, in turn, would impact their attitudes, activeness, or reliance on social support. The alternative model also showed a good fit with the data, χ2 (1, N = 231) = .05, p = .50, CFI = 1.00, NFI = 1.00, RMSEA =.00 (CI = .00, .15). Thus, longitudinal studies are required to replicate the directionality of the hypothesized model.
Concerning social support, the current study focused on participants’ general perception on how much social support they are receiving from others and did not consider, for example, specific types of social support (e.g. instrumental/emotional). Future studies should examine how different ways of measuring social support can affect the choice of coping strategy as this will provide more granular insights about the phenomena examined in this article.
Another limitation is that our sample consisted of relatively younger women with newly diagnosed breast cancer. Generalizability of our findings might thus be limited in populations of older women with breast cancer or women who had been aware of their breast cancer for a while. Generalizability might also be limited by the fact that our sample was an underserved population and our recruitment sites were limited to rural and urban areas in the Midwest of the United States of America.
Taken together, the findings of the current study have important practical implications for women with breast cancer: social support should be considered as one of the most important factors for the effective interventions among cancer patients. Encouraging breast cancer patients to affiliate with others who can provide social support does improve their emotional well-being. Although receiving good medical treatments might be an essential factor for curing breast cancer, social support can play a crucial role in augmenting the effect of the treatments through helping patients maintain positive perspective about themselves and their conditions. Some breast cancer patients might be reluctant to share their sensitive health information with others for fear of disapproval or rejection (Coyne, 1976), and therefore social support might not always be sought. Even in such a scenario, breast cancer patients may still achieve quality of life benefits by receiving empathic understanding and support from similar others (Buck & Parke, 1972).
Acknowledgments
The study was funded by grants from the National Cancer Institute and the John and Mary Markle Foundation (RFP No. NO2–CO–01040–75). The authors would like to thank the women who agreed to participate in our study.
Biographies
JUNGHYUN KIM (PhD, Michigan State University) is an Assistant Professor in the School of Communication Studies at the Kent State University. Her research interests include the effects of new media on psychological well-being, and computer-mediated communication.
JEONG YEOB HAN (PhD, University of Wisconsin) is an Assistant Professor in the Department of Telecommunications and a faculty member with the Center for Health and Risk Communication (CHRC) and the Institute for Behavioral Research (IBR) at the University of Georgia. He is also a research consultant to the National Cancer Institute-funded Center of Excellence in Cancer Communication Research at the University of Wisconsin-Madison.
BRET R. SHAW (PhD, University of Wisconsin) is an Assistant Professor with the Department of Life Sciences Communication and a researcher with the National Cancer Institute-funded Center of Excellence in Cancer Communication Research at the University of Wisconsin-Madison.
FIONA M. MCTAVISH (MS, University of Wisconsin) is the Deputy Director of the Center for Health Enhancement Systems Studies (CHESS) at the University of Wisconsin-Madison.
DAVID H. GUSTAFSON (PhD, University of Michigan) is a Research Professor in the College of Engineering and Director of the National Cancer Institute’s Center of Excellence in Cancer Communication at the University of Wisconsin-Madison.
Footnotes
COMPETING INTEREST: None declared.
Contributor Information
JUNGHYUN KIM, Kent State University, USA.
JEONG YEOB HAN, University of Georgia, USA.
BRET SHAW, University of Wisconsin-Madison, USA.
FIONA MCTAVISH, University of Wisconsin-Madison, USA.
DAVID GUSTAFSON, University of Wisconsin-Madison, USA.
References
- Aro H, Hanninen V, Paronene O. Social support, life events and psychosomatic symptoms among 14–16 year old adolescents. Social Science and Medicine. 1989;19:1051–1056. doi: 10.1016/0277-9536(89)90015-4. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality & Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bentler PM. EQS 6 structural equations program manual. Encino, CA: Multivariate Software; 2006. [Google Scholar]
- Bozo O, Gundogdu E, Buyukasik-Colak C. The moderating role of different sources of perceived social support on the dispositional optimism: Posttraumatic growth relationship in postoperative breast cancer patients. Journal of Health Psychology. 2009;14:1009–1020. doi: 10.1177/1359105309342295. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris T. The social origins of depression. New York: Free Press; 1978. [DOI] [PubMed] [Google Scholar]
- Brown G, Wallston K, Nicassio P. Pain coping strategies and depression in rheumatoid arthritis. Journal of Consulting and Clinical Psychology. 1989;57:652–657. doi: 10.1037//0022-006x.57.5.652. [DOI] [PubMed] [Google Scholar]
- Buck RW, Parke RD. Behavioral and physiological response to the presence of a friendly or neutral person in two types of stressful situations. Journal of Personality and Social Psychology. 1972;24:143–153. doi: 10.1037/h0033370. [DOI] [PubMed] [Google Scholar]
- Carrico AW, Antoni MH, Durán RE, Ironson G, Feredo F, Klimas N, Schneiderman N. Reductions in depressed mood and denial coping during cognitive behavioral stress management with HIV-positive gay men treated with HAART. Annals of Behavioral Medicine. 2006;31:155–164. doi: 10.1207/s15324796abm3102_7. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Carver CS, Pozo C, Harris SD, Noriega V, Scheier ME, Robinson DS, et al. How coping mediates the effect of optimism on distress: A study of women with early stage breast cancer. Journal of Personality and Social Psychology. 1993;65:375–390. doi: 10.1037//0022-3514.65.2.375. [DOI] [PubMed] [Google Scholar]
- Cheng TYL, Boey KW. Coping, social support, and depressive symptoms of older adults with type II Diabetes Mellitus. Clinical Gerontologist. 2000;22:15–30. [Google Scholar]
- Clement U, Schoennesson LN. Subjective HIV attribution theories, coping, and psychological functioning among homosexual men with HIV. AIDS Care. 1998;10:355–363. doi: 10.1080/713612416. [DOI] [PubMed] [Google Scholar]
- Coyne JC. Depression and the response of others. Journal of Abnormal Psychology. 1976;85:186–193. doi: 10.1037//0021-843x.85.2.186. [DOI] [PubMed] [Google Scholar]
- David D, Montgomery G, Bovbjerg D. Relations between coping responses and optimism–pessimism in predicting anticipatory psychological distress in surgical breast cancer patients. Personality and Individual Differences. 2006;40:203–213. doi: 10.1016/j.paid.2005.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumont M, Provost MA. Resilience in adolescents: Protective role of social support, coping strategies, self-esteem, and social activities on experience of stress and depression. Journal of Youth and Adolescence. 1999;28:343–363. [Google Scholar]
- Dunkel-Schetter C. Social support and cancer: Findings based on patient interviews and their implications. Journal of Social Issues. 1984;40:77–98. [Google Scholar]
- Feather BL, Wainstock JM. Perception of postmastectomy patients. Part 1. The relationships between social support and network providers. Cancer Nursing. 1989;2:293–300. [PubMed] [Google Scholar]
- Finch JF, Okun MA, Pool GJ, Ruehlman LS. A comparison of the influence of conflictual and supportive social interactions on psychological distress. Journal of Personality. 1999;67:581–621. doi: 10.1111/1467-6494.00066. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. Journal of Health and Social Behavior. 1980;21:219–239. [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. If it changes it must be a process: A study of emotion and coping during three stages of a college examination. Journal of Personality and Social Psychology. 1984;48:150–170. doi: 10.1037//0022-3514.48.1.150. [DOI] [PubMed] [Google Scholar]
- Griffin KW, Friend R, Kaell AT, Bennett RS. Distress and disease status among patients with rheumatoid arthritis: Roles of coping styles and perceived responses from support providers. Annals of Behavioral Medicine. 2001;23:133–138. doi: 10.1207/S15324796ABM2302_8. [DOI] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Stengle W, Ballard D, Hawkins R, Shaw B, et al. Use and impact of eHealth system by low-income women with breast cancer. Journal of Health Communication. 2005;10:194–218. doi: 10.1080/10810730500263257. [DOI] [PubMed] [Google Scholar]
- Han JY, Shaw BR, Hawkins RP, Pingree S, McTavish F, Gustafson DH. Expressing positive emotions within online support groups by women with breast cancer. Journal of Health Psychology. 2008;13:1002–1007. doi: 10.1177/1359105308097963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Cohen S. Social support and adjustment to cancer: Reconciling descriptive, correlational, and intervention research. Health Psychology. 1996;15:135–148. doi: 10.1037//0278-6133.15.2.135. [DOI] [PubMed] [Google Scholar]
- Holland KD, Holahan CK. The relation of social support and coping to positive adaptation to breast cancer. Psychology and Health. 2003;18:15–29. [Google Scholar]
- Holmes J, Stevenson C. Differential effects of avoidant and attentional coping strategies on adaptation to chronic and recent-onset pain. Health Psychology. 1990;9:577–584. doi: 10.1037//0278-6133.9.5.577. [DOI] [PubMed] [Google Scholar]
- Holohan CJ, Moos RH, Holohan CK, Brennan PL. Social support, coping, and depressive symptoms in a late-middle-aged sample of patients reporting cardiac illness. Health Psychology. 1995;14:152–163. doi: 10.1037//0278-6133.14.2.152. [DOI] [PubMed] [Google Scholar]
- Holtzman S, Newth S, DeLongis A. The role of social support in coping with daily pain among patients with rheumatoid arthritis. Journal of Health Psychology. 2004;9:677–695. doi: 10.1177/1359105304045381. [DOI] [PubMed] [Google Scholar]
- Israel BA, Schurman SJ. Social support, control, and the stress process. In: Glanz K, Lewis FM, Rimer B, editors. Health behavior and health education: Theory, research, and practice. San Francisco, CA: Jossey-Bass; 1990. pp. 187–215. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2. New York: Guilford; 2005. [Google Scholar]
- Lazarus R. Coping theory and research: Past, present, and future. Psychosomatic Medicine. 1993;55:234–247. doi: 10.1097/00006842-199305000-00002. [DOI] [PubMed] [Google Scholar]
- Lopez-Martinez A, Esteve-Zarazaga R, Ramirez-Maestre C. Perceived social support and coping responses are independent variables explaining pain adjustment among chronic pain patients. Journal of Pain. 2008;9:373–379. doi: 10.1016/j.jpain.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Noh S, Kaspar V. Perceived discrimination and depression: Moderating effects of coping, acculturation, and ethnic support. American Journal of Public Health. 2003;93:232–238. doi: 10.2105/ajph.93.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien TB, DeLongis A. Coping with chronic stress: An interpersonal perspective. In: Gottlieb BH, editor. Coping with chronic stress. New York: Plenum Publishing Corporation; 1997. pp. 161–190. [Google Scholar]
- Park C, Edmondson D, Fenster J, Blank T. Positive and negative health behavior changes in cancer survivors: A stress and coping perspective. Journal of Health Psychology. 2008;13:1198–1206. doi: 10.1177/1359105308095978. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Schwartz R, Hogben M, Liddon N, Augenbraun M, Mccormack W, Rubin S, Wilson T. Coping with a diagnosis of C Trachomatis or N Gonorrhoeae: Psychosocial and behavioral correlates. Journal of Health Psychology. 2008;13:921–929. doi: 10.1177/1359105308095066. [DOI] [PubMed] [Google Scholar]
- Shaw B, Han J, Hawkins R, McTavish F, David H. Communicating about self and others within an online support group for women with breast cancer and subsequent outcomes. Journal of Health Psychology. 2008;13:930–939. doi: 10.1177/1359105308095067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel D. Psychosocial aspects of breast cancer treatment. Seminars in Oncology. 1997;24:36–47. [PubMed] [Google Scholar]
- Swindells S, Mohr J, Justis JC, Berman S, Squier C, Wagener MM, et al. Quality of life in patients with human immunodeficiency virus infection: Impact of social support, coping style and hopelessness. International Journal of STDs and AIDS. 1999;10:383–391. [PubMed] [Google Scholar]
- Thoits PA. Social support as coping assistance. Journal of Consulting and Clinical Psychology. 1986;54:416–423. doi: 10.1037//0022-006x.54.4.416. [DOI] [PubMed] [Google Scholar]
- Uchino BN, Cacioppo JT, Kiecolt-Glaser KG. The relationships between social support and physiological processes: A review with emphasis on underlying mechanisms and implications for health. Psychological Bulletin. 1996;119:488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]


