Abstract
Background. Acculturation affects health, but it has never been studied with kidney disease.
Methods. We studied the association of language spoken at home, generation and birth place with kidney function among Hispanics and Chinese in the Multi-Ethnic Study of Atherosclerosis (n = 2999). Kidney function was determined by cystatin C (eGFRcys) and albumin/creatinine ratio (ACR). We evaluated mediators in models: Model 1 = age, sex, income, education; Model 2 = Model 1 + behaviors; and Model 3 = Model 1 + comorbidities.
Results. Among Hispanics, speaking mixed Spanish/English was significantly associated with lower eGFRcys (− 2.83 mL/min/1.73 m2, − 5.69–0.04) and higher ACR (RD 40%, 17–68%) compared with speaking Spanish only; this was mildly attenuated by behaviors (− 2.29, − 5.33–0.75; RD 42%, 18–72%) but not comorbidities (− 3.04, − 5.83 to − 0.23); RD 35%, 14–59%). US-born Hispanics had lower eGFRcys compared with foreign-born Hispanics [1.83 mL/min/1.73 m2 lower (0.97–1.31) for Generation 1; 1.37 mL/min/1.73 m2 lower (0.75–1.57) for Generation ≥ 2].
In contrast, Chinese who spoke any English had higher eGFRcys (2.53, 95% CI: − 1.70–6.78), but similar ACR (RD − 5%, 95% CI: − 26–23%) compared with those speaking Chinese only, but associations were not statistically significant.
Conclusion. Higher acculturation was associated with worse kidney function in Hispanics, mediated perhaps by behavioral factors but not comorbidities. Associations may be in the opposite direction among Chinese. Future studies are needed to elucidate these mechanisms.
Keywords: acculturation, cystatin C, kidney function
Introduction
Chronic kidney disease (CKD) is a major public health problem in the USA, which is reported to affect 13% of adults [9]. The impact of CKD and its complications is higher among certain racial/ethnic groups [20,28,34,43,49]. Hispanics have ~ 2-fold higher incidence of end-stage renal disease (ESRD) and Asians have a 1.3-fold higher incidence compared with non-Hispanic whites in the USA [23,34,49,50]. These observations have not been explained by differences in the prevalence of traditional CKD risk factors or differences in socioeconomic status [20,34,47]. Despite the increasing numbers of persons of Hispanic or Asian descent affected by kidney disease [49], studies of risk factors for CKD among Hispanics and Asians in the USA are limited.
One major challenge in the study of CKD risk factors within these groups is that adults who are categorized as Hispanic or Asian in epidemiological studies may actually be quite heterogenous [7,33], possibly leading to differences in disease risk. One source of variability within immigrant groups is the degree of adoption of US culture, referred to as level of acculturation. Acculturation refers to the modification of the culture, behavior, beliefs and values of individuals and groups as they borrow or adapt to another culture [4]. Different immigrant groups may acculturate to different degrees, and acculturation may also vary by gender or age [5,8,31,32,36]. Moreover, acculturation may have differing associations with disease in different groups [45]. Higher levels of acculturation have been shown to be independently associated with higher rates of traditional CKD risk factors such as diabetes, atherosclerotic heart disease and hypertension among Chinese and non-Mexican American Hispanics in the USA [13,24,30]. Evidence also suggests that the health consequences of greater acculturation are not always adverse [3]. The association of acculturation with kidney disease has not been previously studied.
We used data from the Multi-Ethnic Study of Atherosclerosis (MESA) to investigate whether acculturation is associated with kidney dysfunction and albuminuria among Hispanic and Chinese participants. We also investigated whether a potential association between acculturation and kidney dysfunction was explained by differences in traditional kidney disease risk factors or differences in behavioral factors. We hypothesized that higher levels of acculturation would be associated with decreased kidney function and increased albuminuria, and that these associations would be primarily mediated by differences in the prevalence of diabetes and hypertension.
Materials and methods
Subjects
The MESA is a large, prospective cohort sponsored by the National Heart, Lung, Blood Institute aimed to understand subclinical cardiovascular disease and its progression in a multi-ethnic population. Details on recruitment and design have been previously published [6]. The MESA cohort includes 6814 men and women aged 45–84 years at the time of recruitment. Participants were recruited from six field centers: Baltimore, MD; Chicago, IL; Forsyth County, NC; Los Angeles, CA; New York, NY; and Saint Paul, MN between July 2000 and August 2002 and were all free of cardiovascular disease at entry. Individuals were self-identified as white, African American, Hispanic or Chinese-American based upon self-report. The institutional review boards at all participating centers approved the study, and all participants gave informed consent. For these analyses, we included all participants who self-identified as Hispanics or Chinese and who either had a cystatin C measurement or an albuminuria measurement at the baseline visit (n = 2299).
Predictor variable: measures of acculturation
This study uses three proxy measures of acculturation: (i) language spoken at home, (ii) generation and (iii) place of birth to examine the association of level of acculturation with kidney dysfunction among Hispanics and Chinese. These measures were chosen because they have been shown to have high internal consistency, strong correlations with existing acculturation scales and have been reported to explain much of the variance of existing scales [10–12]. In addition, they have been widely used as proxies of acculturation in other studies [8,11,13,18,24,25,30,36]. Questionnaires were administered at the baseline MESA visit in English, Spanish and Chinese. These questionnaires collected information on sociodemographic and cultural factors. Participants were asked to identify their primary language spoken at home. For Hispanics, we categorized participants as speaking exclusively Spanish, mixed Spanish and English, or exclusively English at home. We categorized Chinese participants as either speaking exclusively Chinese or any English (combining mixed English and Chinese and English only) at home due to the low numbers of Chinese speaking English only at home.
Generation was derived by combining information about birth place for participants and their parents and grandparents reported in the MESA questionnaire. We categorized generation as in previous acculturation studies using generation as a proxy measure of acculturation [26]. Generation 0 was defined as the participant being born outside the US (Puerto Rico included); Generation 1 if the participant was born in the USA and at least one of his/her parents were born outside the USA; Generation 2 if the participant, his/her parents and up to two grandparents were born in the USA; and Generation 3 if the participant, his/her parents and three to four grandparents were born in the USA. Generation 0 was considered least acculturated [26].
Place of birth was determined by responses participants gave in the questionnaire. We categorized participants as either US born (including Puerto Rico) or foreign born.
Outcome variables: kidney function and albuminuria
Estimated glomerular filtration rate (eGFR) was calculated using cystatin C. Cystatin C is an alternative marker of kidney function that has been shown to be less affected by age and sex than creatinine [37–39,41], may be more accurate for estimating kidney function among persons with glomerular filtration rate > 60 mL/min/1.73 m2 [35] and has stronger and more linear relationships with adverse cardiovascular outcomes and mortality compared with creatinine [42]. Cystatin C was measured from stored sera collected at the baseline MESA visit by a particle-enhanced immunonephelometric assay (Siemens). We expressed kidney function as eGFR using the equation: 76.7 × cys C − 1.19 [44].
We also studied urine albumin levels as a measure of kidney damage, using the spot urine albumin/creatinine ratio (ACR) measurement. Urine albumin and creatinine were measured by nephelometry and the Jaffe method with the ratio expressed in milligrams per gram.
Covariates
Age, sex, history of smoking, alcohol use, income and education were ascertained by a questionnaire at baseline. In addition, MESA used a questionnaire modeled after the Cross-Culture Activity Participation Study to ascertain physical activity, which is semiquantitative and assigns a MET intensity level for each activity participants responded engaging in. Physical activity data is then summarized as minutes per day and MET minutes (minutes per day × MET intensity level). One MET minute is roughly 1 kcal/min for a 60-kg person [48], which allowed a quantitative evaluation of physical activity. Diet and caloric intake were evaluated using a 127-item food frequency questionnaire [27] based upon the Insulin Resistance Atherosclerosis Study instrument. The questionnaire has been validated for different race/ethnic groups and was modified in MESA to include foods typically eaten by Chinese persons. Diabetes was defined as fasting glucose ≥ 126 mg/dL and/or use of anti-diabetic medication, a definition used by the 2003 American Diabetes Association criteria [1]. Hypertension was defined as a systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg, or current use of antihypertensive medication. Waist/hip ratio, measured as an index of body fat distribution, was calculated by measuring to the nearest 0.1 cm from the umbilicus and hips to the maximum circumference of buttocks. Body mass index (BMI) was calculated as weight (kg)/height (m) [2]. Total high-density lipoprotein (HDL) cholesterol and triglycerides were measured and low-density lipoprotein (LDL) was estimated by the Friedewald equation.
Statistical analysis
We first described the cohort characteristics by language spoken at home, separately for Hispanics and Chinese, using t-test, ANOVA or chi-square where appropriate. We used multivariable linear regression models, separate for Hispanics and Chinese, to determine whether there was an independent association of language, generation or place of birth (in separate models) with eGFR or ACR. Urinary ACR was log transformed to achieve normality. Spanish only/Chinese language only, Generation 0 and born outside the USA were used as referent categories, as these were considered least acculturated. Beta coefficients for the models with ACR were back transformed to relative differences (RD) in order to facilitate interpretation. In addition, we used three staged models with sequentially added variables in order to study potential mediators of the association between acculturation and kidney dysfunction. Model 1 included age, sex, income and education; Model 2 included variables in Model 1 plus behavioral factors: smoking (current, past, never), alcohol use (yes or no), physical activity and percent fat calories; and Model 3 included Model 1 plus traditional CKD risk factors: diabetes, hypertension, LDL, HDL, BMI and waist/hip ratio. Based on prior literature [8,32,36], we then tested for the interactions of each measure of acculturation with age (< 65 and ≥ 65 years old) and sex in Model 1 for each kidney outcome. All analyses were conducted using Stata 10 (College Station, TX, USA) [2].
Results
Characteristics of the study population
Among the 2299 participants in this study, 1496 self-identified as Hispanic and 803 as Chinese. Mean age was 62 for Hispanics and 61 for Chinese participants; mean eGFR levels were 93 and 98 mL/min/1.73 m2, respectively. Among Hispanics and Chinese, 12.5 and 12% had ACR > 30 mg/g, respectively. In addition, the distribution of the measures of acculturation varied by ethnic group. Among Hispanics, there was a wide distribution across categories of language spoken at home: 819 (55%) spoke exclusively Spanish, 238 (16%) spoke mixed Spanish and English, and 439 (29%) spoke exclusively English. In contrast, 700 (87%) of the Chinese reported speaking exclusively Chinese; only 31 Chinese participants were born in the USA.
In both race/ethnic groups, those who spoke English exclusively at home generally had higher incomes and levels of education. Hispanic participants who spoke primarily English had higher waist circumferences and BMI, though they reported higher levels of physical activity compared with those who spoke Spanish only. Hispanics who reported speaking any English or exclusively English were more likely to be current or former smokers. Among Chinese, the group speaking any English at home had higher average BMI and higher caloric intake, but a lower percentage of calories from fat (Table 1). Among Hispanics, eight participants were missing a cystatin C measure and seven were missing urine albumin measures. Among Chinese participants, only three were missing a cystatin C measure and none was missing urine albumin.
Table 1.
Characteristics of Hispanics and Chinese by language spoken at home, MESA
| Hispanics (n = 1496) |
Chinese (n = 803) |
||||
|---|---|---|---|---|---|
| Exclusively Spanish | English and Spanish | Exclusively English | Exclusively Chinese | Any English | |
| n = 819 | n = 238 | n = 439 | n = 700 | n = 103 | |
| % or mean ± SD | % or mean ± SD | ||||
| Age*,+ | 61 ± 10 | 63 ± 11 | 61 ± 10 | 63 ± 10 | 60 ± 9 |
| Male (%)* | 45 | 50 | 53 | 47 | 57 |
| Income**,++ | |||||
| <$20K | 49 | 35 | 21 | 46 | 10 |
| $20–50K | 39 | 43 | 46 | 30 | 25 |
| ≥$50K | 8 | 21 | 32 | 23 | 64 |
| Education**,++ | |||||
| < High school | 63 | 35 | 16 | 28 | 6 |
| High school graduates | 16 | 25 | 26 | 17 | 9 |
| > High school | 22 | 40 | 57 | 55 | 85 |
| BMI*,+ | 29 ± 5 | 29 ± 5 | 30 ± 6 | 24 ± 3 | 25 ± 4 |
| Waist* | 100 ± 12 | 100 ± 13 | 102 ± 14 | 87 ± 9 | 88 ± 12 |
| Waist/hip | 1 ± 0.1 | 1 ± 0.1 | 1 ± 0.1 | 1 ± 0.1 | 1 ± 0.1 |
| HDL | 47 ± 13 | 48 ± 13 | 48 ± 13 | 49 ± 13 | 50 ± 13 |
| LDL | 121 ± 34 | 117 ± 29 | 118 ± 33 | 115 ± 29 | 115 ± 31 |
| Total cholesterol | 200 ± 39 | 194 ± 34 | 197 ± 37 | 192 ± 32 | 195 ± 34 |
| Triglycerides | 158 ± 111 | 150 ± 80 | 161 ± 91 | 142 ± 84 | 148 ± 89 |
| Systolic blood pressure | 128 ± 22 | 127 ± 22 | 125 ± 21 | 125 ± 22 | 123 ± 21 |
| Diabetes | 18 | 19 | 17 | 13 | 11 |
| Hypertension | 41 | 43 | 41 | 39 | 30 |
| Smoking** | |||||
| Never | 59 | 49 | 47 | 76 | 69 |
| Former | 28 | 34 | 39 | 18 | 26 |
| Current | 12 | 16 | 14 | 6 | 5 |
| Alcohol use (%) | 317 (39%) | 129 (54%) | 259 (59%) | 202 (29%) | 48 (47%) |
| Phys. activity** | 855 ± 1339 | 1554 ± 2011 | 2113 ± 2930 | 1120 ± 1479 | 1352 ± 1752 |
| Total cal.++ | 1815 ± 907 | 1831 ± 1007 | 1730 ± 932 | 1301 ± 565 | 1555 ± 663 |
| Percent fat+ | 35 ± 7 | 36 ± 6 | 36 ± 7 | 36 ± 7 | 34 ± 6 |
| Baseline eGFRcys (mL/min/1.73 m2) | 93 ± 21 | 89 ± 21 | 92 ± 20 | 97 ± 22 | 102 ± 23 |
| Baseline ACR (mg/dL) | 35 ± 202 | 88 ± 442 | 42 ± 332 | 34 ± 181 | 21 ± 73 |
| Generation 0 | 700 (85.5%) | 97 (40.8%) | 71 (16.2%) | 695 (99.3%) | 77 (74.5%) |
| Generation 1 | 110 (13.4%) | 89 (37.4%) | 181 (41.2%) | 4 (0.6%) | 16 (15.5%) |
| Generations 2 and 3 | 3 (0.4%) | 15 (6.3%) | 74 (16.9%) | 0 | 0 |
HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Generation 0 was defined as the participant being born outside the USA (Puerto Rico included); Generation 1 if the participant was born in the USA and at least one of his/her parents were born outside the USA; Generations 2 and 3 if the participant, his/her parents and two or more of his/her grandparents were born in the USA.
P ≤ 0.05–0.001 for Hispanics.
P ≤ 0.001 for Hispanics.
P ≤ 0.05–0.001 for Chinese.
P ≤ 0.001 for Chinese.
Acculturation and kidney function among Hispanics
Compared with those who reported speaking exclusively Spanish at home, Hispanics speaking any English at home or exclusively English at home had lower eGFR, and this finding was strongest among those speaking both languages. In the group speaking mixed Spanish and English, eGFR was significantly lower compared to the Spanish only group, even after adjusting for demographic factors and socioeconomic status. Although the direction of the association remained constant, the effect size was attenuated by ~ 20% by adjustment for behavioral factors. In contrast, adjustment for traditional CKD risk factors (comorbidities) had no attenuation effect (Table 2).
Table 2.
The association of language spoken at home with kidney function (eGFRcys) and albuminuria (ACR) among Hispanics
| Exclusively Spanish (N = 816) | Mixed Spanish and English (N = 235) | P-value | Exclusively English (N = 437) | P-value | |
|---|---|---|---|---|---|
| Kidney function by eGFRcys | |||||
| Mean difference (mL/min/1.73 m2) (95% CI) | |||||
| Demographic adjusted (Model 1) | Ref. | − 2.83 (− 5.69–0.04) | 0.05 | − 1.37 (− 3.84–1.12) | 0.28 |
| Lifestyle behavior adjusted (Model 2) | Ref. | − 2.29 (− 5.33–0.75) | 0.14 | − 1.09 (− 3.74–1.54) | 0.42 |
| Comorbidity adjusted (Model 3) | Ref. | − 3.04 (− 5.83 to − 0.23) | 0.03 | − 0.66 (− 3.09–1.78) | 0.60 |
| Albumin/creatinine ratio | |||||
| Relative difference (95% CI) | |||||
| Demographic adjusted (Model 1) | Ref. | 40% (17–68%) | < 0.001 | 10% (–6–28%) | 0.22 |
| Lifestyle behavior adjusted (Model 2) | Ref. | 42% (18–72%) | < 0.001 | 9% (− 7–29%) | 0.27 |
| Comorbidity adjusted (Model 3) | Ref. | 35% (14–59%) | < 0.001 | 3% (− 11–19%) | 0.63 |
Model 1: includes age, sex, income and education
Model 2: includes Model 1 plus smoking (current, never, past), alcohol use (yes or no), physical activity and percent fat calories
Model 3: includes Model 1 plus diabetes, hypertension, LDL, HDL, BMI and waist/hip ratio.
A similar pattern was seen with albuminuria where Hispanic participants who spoke only English and those who spoke both Spanish and English at home had significantly higher albuminuria levels compared to those who spoke Spanish only. This association was not significantly attenuated after adjustment for behavioral factors or comorbidities. Those who reported speaking English only had modestly higher levels of albuminuria, but the differences were not statistically significant.
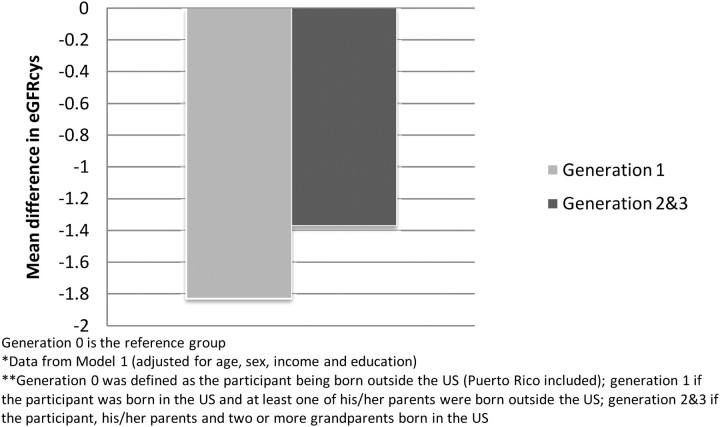
We also used generation as a proxy measure for acculturation and examined its association with kidney function and albuminuria. We observed that Hispanics who were Generation 1 and above had worse kidney function than Hispanics who were Generation 0, but the results did not reach statistical significance: eGFR was 1.83 mL/min/1.73 m2 lower (95% CI 0.97–1.31) for Generation 1 and 1.37 mL/min/1.73 m2 lower (95% CI 0.75–1.57) for Generations 2 and 3 (Figure 3). In addition, those who were Generation 1 and above had higher levels of albuminuria (RD 12%, 95% CI − 3–13%) compared to those who were Generation 0. Results were similar when we used place of birth as a proxy for acculturation; US-born Hispanics had lower eGFR (− 1.07 mL/min/1.73 m2, 95% CI − 3.31–1.19) and higher levels of albuminuria (RD 18%, 95% CI 3–36%). This association with albuminuria was moderately attenuated by adjusting for both behavioral factors and comorbidities, but significance was lost [RD 12% (− 3–30) and RD 8% (− 6–32%), respectively].
Fig. 3.
Mean differences in eGFRcys by generation among Hispanics.
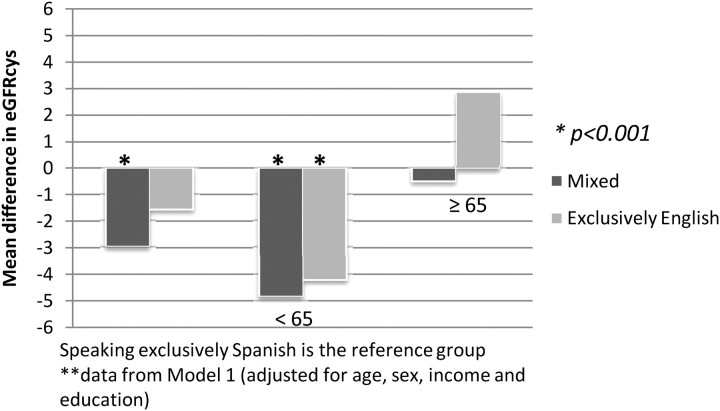
Interestingly, we found significant effect modification by age of the association between language spoken at home and kidney function in Hispanics (P for interaction = 0.009). Among those aged < 65 years, speaking English only or mixed English/Spanish was strongly and independently associated with lower eGFR. There was no observed association between acculturation and kidney dysfunction among those aged > 65 (Figure 1). We found no significant interaction with sex (P = 0.38).
Fig. 1.
Mean differences in kidney function among Hispanics, stratified by age.
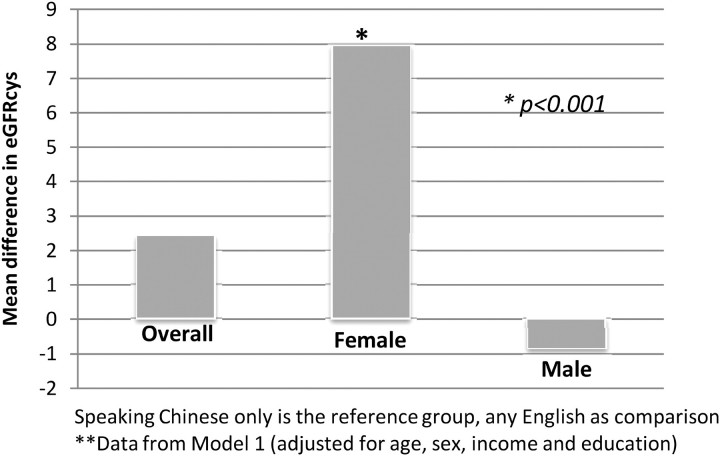
The association of acculturation and kidney dysfunction among Chinese
In contrast to the findings among Hispanics, speaking any English at home was associated with better kidney function among the Chinese, but the findings were not statistically significant. However, the point estimate was consistent in all models and similar in magnitude to the association observed when mixed language Hispanics were compared to English language Hispanics (Table 3). Chinese who reported speaking any English had slightly lower levels of albuminuria, but these findings were not statistically significant. We could not evaluate generation or place of birth in the Chinese because nearly all were either Generation 0 or 1 and born outside the USA. We found a significant interaction with gender in the Chinese (P = 0.04) but not with age (P = 0.80). The use of any English language at home was associated with a significantly higher eGFR among Chinese women, whereas no association was observed among Chinese men (Figure 2). This association was not attenuated after adjustment for behavioral factors and only slightly by comorbidities.
Table 3.
The association of language spoken at home with kidney function (eGFRcys) and albuminuria (ACR) among Chinese
| Exclusively Chinese (N = 700) | Any English (N = 103) | P-value | |
|---|---|---|---|
| Kidney function by eGFRcys | |||
| Mean difference (mL/min/1.73 m2) (95% CI) | |||
| Demographic adjusted (Model 1) | Ref. | 2.53 (− 1.70–6.78) | 0.24 |
| Lifestyle behavior adjusted (Model 2) | Ref. | 2.48 (− 1.87–6.83) | 0.25 |
| Comorbidity adjusted (Model 3) | Ref. | 2.14 (− 2.02–6.31) | 0.31 |
| Albumin/creatinine ratio | |||
| Relative difference (95% CI) | |||
| Demographic adjusted (Model 1) | Ref. | − 5% (− 26–23%) | 0.73 |
| Lifestyle behavior adjusted (Model 2) | Ref. | − 2% (− 15–26%) | 0.89 |
| Comorbidity adjusted (Model 3) | Ref. | − 3% (− 24–25%) | 0.86 |
Model 1: includes age, sex, income and education
Model 2: includes Model 1 plus smoking (current, never, past), alcohol use (yes or no), physical activity and percent fat calories
Model 3: includes Model 1 plus diabetes, hypertension, LDL, HDL, BMI and waist/hip ratio.
Fig. 2.
Mean differences in eGFRcys among Chinese, statified by gender.
Discussion
Using proxy measures of acculturation, we found an association between acculturation and kidney function by eGFR and albuminuria among Hispanics and Chinese. Interestingly, the direction of the association differed by race/ethnic group. Particularly when measured by language spoken at home, higher levels of acculturation were associated with worse kidney function and higher albuminuria among Hispanics, whereas the direction of the association with kidney function was the opposite among Chinese, although it was not statistically significant. Among demographic subgroups, language appeared to have the strongest associations with kidney function among younger Hispanics and among Chinese women. Adjustment for behavioral factors attenuated the association between acculturation and kidney disease among Hispanics, but adjustment for traditional kidney disease risk factors had little effect.
The observed differences in the association of acculturation and kidney function by race/ethnicity illustrate the complexity of studying acculturation effects on health and disease. The acculturation process itself may differ for Hispanics and Chinese immigrants, and it may have differing positive and negative effects on health across racial/ethnic groups [5,15,31,36,45]. For example, Hispanics who are more acculturated may adopt adverse behaviors related to diet or smoking that may impact health [19,29], whereas Chinese may in fact stop smoking or increase physical activity, as has been previously reported [3,8].
The negative impact of higher acculturation on kidney function in Hispanics is consistent with prior data [14,24,26,30]. The finding that this outcome appeared to be more pronounced among those who reported speaking both English and Spanish is noteworthy. One possible mechanism to explain this observation is that Hispanics who speak predominantly English may have acquired adverse health behaviors, but have better access to the healthcare system and higher health literacy, thus attenuating some of the adverse effects of acculturation in this group. When we examined potential mediators of the association between language and kidney disease, we found that lifestyle behaviors moderately attenuated the association, whereas traditional CKD risk factors like diabetes and hypertension did not. This finding is consistent with studies that found acculturation to have a negative effect on health behaviors in this population [16,17,21,29]. The mechanism to explain the fact that different health behaviors rather than traditional CKD risk factors attenuated the effects of acculturation with eGFR should be explored further. It is possible that changes in behavior may lead to increased inflammation, oxidative stress and/or obesity before the onset of clinical diabetes, hypertension or CKD (eGFR < 60 mL/min/1.73 m2 [2]). These factors have been associated with kidney dysfunction [22, 40]. We also found a significant effect modification by age on the association of language spoken at home and kidney function among Hispanics, where the effects of acculturation were strongest among younger Hispanics. This may be explained by reports that younger Hispanics appear to have higher rates of obesity, poorer nutritional habits and lower rates of physical activity compared to their White counterparts [5]. It may also be that the effects of age on kidney function overwhelm any measurable effect of acculturation, older participants have lived in the USA longer, so that language is a poorer measure of acculturation, or that older participants migrated at an older age and were less likely to acculturate, resulting in a more narrow range of exposure to host country influences. Future studies should focus on investigating social and biological pathways that mediate the associations between adverse health habits and kidney disease.
In contrast to Hispanics, we observed that acculturation may be associated with better kidney function. This has also been observed in other studies [5]. The positive association between acculturation and kidney function was significant primarily in Chinese women. Chinese women have been reported to adopt the healthy habits, such as increased physical activity [3] and healthier diet, of the US earlier and smoke less than their male counterparts [32]. In addition to differences in the adoption of adverse health habits, Chinese immigrants tend to have higher incomes and levels of education than Hispanic immigrants in the USA, which may lead to better access to healthcare. Other important factors such as spirituality and social cohesion may also shield immigrant groups from adverse effects of other components of acculturation [15,46], factors present in Hispanics but perhaps overwhelmed by adverse acculturation influences in other realms.
To our knowledge, this is the first study to examine the relationship between acculturation and kidney function ‘within’ race/ethnic groups. Strengths of the study include the use of MESA, which is a large, multi-ethnic, diverse cohort. In addition, cystatin C is a measure of kidney function that has been shown to be less biased than creatinine, particularly in a general population study such as this one. This study also examined the two largest immigrant groups in the USA, yielding results that could be helpful in clinical practice and for health interventions for these populations. However, our study is limited by the use of proxies for acculturation rather than a validated scale. Although some of our findings did not reach statistical significance, these were consistent using several different measures of acculturation. In addition, we used eGFR as measure of kidney function, and equations have not been accurately validated in all major race/ethnic groups. Due to the cross-sectional nature, we cannot address the direction of the association, although it seems implausible that decreased kidney function could affect language status. A major limitation is that we were limited in power by sample size and the narrow distribution of measures of acculturation in the Chinese, which may have biased our results toward the null. Moreover, residual, unmeasured confounding may be present. However, our findings support the concept that race/ethnic groups are not homogenous, and that race is a multi-dimensional construct involving genetic ancestry, cultural heritage and the unique acculturation process of each ethnic group in the USA.
In summary, we found that acculturation was associated with kidney function, but that this association differed in direction by race/ethnicity. For Hispanics, those who spoke mixed Spanish and English had the worst kidney health based on eGFR and albuminuria, and this association was stronger among the young Hispanics. Among Chinese, higher acculturation was associated with better kidney function, and this finding was strongest among the women. Our findings demonstrate that within-group differences are important to consider when examining the health of different ethnic/racial groups in the USA. Often these groups may be considered homogenous, but there are many factors that influence their health. Further studies should examine potential mediators to explain the association between acculturation and kidney function. This is of great public health importance as these ethnic/racial groups are likely to encompass a growing proportion of the CKD population in the USA.
Acknowledgments
This research was supported by contracts N01-HC-95159 from the National Heart, Lung, and Blood Institute. The authors thank the other investigators, the staff and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Conflict of interest statement. None declared.
References
- 1.Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2003;26:S5–S20. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- 2.Stata Reference Manual Release 10. College Station: Stata Press; 2007. [Google Scholar]
- 3.Abraido-Lanza AF, Chao MT, Florez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Soc Sci Med. 2005;61:1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abraido-Lanza AF, White K, Vasquez E. Immigrant populations and health. In: Anderson N, editor. Encyclopedia of Health and Behavior. Newbury Park: Sage; 2004. [Google Scholar]
- 5.Allen ML, Elliott MN, Morales LS, et al. Adolescent participation in preventive health behaviors, physical activity, and nutrition: differences across immigrant generations for Asians and Latinos compared with Whites. Am J Public Health. 2007;97:337–343. doi: 10.2105/AJPH.2005.076810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 7.Burchard EG, Ziv E, Coyle N, et al. The importance of race and ethnic background in biomedical research and clinical practice. N Engl J Med. 2003;348:1170–1175. doi: 10.1056/NEJMsb025007. [DOI] [PubMed] [Google Scholar]
- 8.Choi S, Rankin S, Stewart A, et al. Effects of acculturation on smoking behavior in Asian Americans: a meta-analysis. J Cardiovasc Nurs. 2008;23:67–73. doi: 10.1097/01.JCN.0000305057.96247.f2. [DOI] [PubMed] [Google Scholar]
- 9.Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. Jama. 2007;298:2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 10.Coronado GD, Thompson B, McLerran D, et al. A short acculturation scale for Mexican-American populations. Ethn Dis. 2005;15:53–62. [PubMed] [Google Scholar]
- 11.Cruz TH, Marshall SW, Bowling JM, et al. The validity of a proxy acculturation scale among US Hispanics. Hisp J Behav Sci. 2008;30:425. [Google Scholar]
- 12.Devo RA, Diehl AK, Hazuda H, et al. A simple language-based acculturation scale for Mexican Americans: validation and application to health care research. Am J Public Health. 1985;75:51–55. doi: 10.2105/ajph.75.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diez Roux AV, Detrano R, Jackson S, et al. Acculturation and socioeconomic position as predictors of coronary calcification in a multiethnic sample. Circulation. 2005;112:1557–1565. doi: 10.1161/CIRCULATIONAHA.104.530147. [DOI] [PubMed] [Google Scholar]
- 14.Diez Roux AV, Detrano R, Jackson SA, et al. Acculturation and socioeconomic position as predictors of coronary calcification in a multiethnic sample. Circulation. 2008;112:1557–1565. doi: 10.1161/CIRCULATIONAHA.104.530147. [DOI] [PubMed] [Google Scholar]
- 15.Dressler WW. Hypertension in the African American community: social, cultural, and psychological factors. Semin Nephrol. 1996;16:71–82. [PubMed] [Google Scholar]
- 16.Ebin VJ, Sneed CD, Morisky DE, et al. Acculturation and interrelationships between problem and health-promoting behaviors among Latino adolescents. J Adolesc Health. 2001;28:62–72. doi: 10.1016/s1054-139x(00)00162-2. [DOI] [PubMed] [Google Scholar]
- 17.Gil AG, Wagner EF, Vega WA. Acculturation, familialism, and alcohol use among Latino adolescent males. J Community Psychol. 2000;28:443–458. [Google Scholar]
- 18.Gomez SL, Kelsey JL, Glaser SL, et al. Immigration and acculturation in relation to health and health-related risk factors among specific Asian subgroups in a health maintenance organization. Am J Public Health. 2004;94:1977–1984. doi: 10.2105/ajph.94.11.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gordon-Larsen P, Harris KM, Ward DS, et al. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Soc Sci Med. 2003;57:2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- 20.Hall YN, Hsu CY, Iribarren C, et al. The conundrum of increased burden of end-stage renal disease in Asians. Kidney Int. 2005;68:2310–2316. doi: 10.1111/j.1523-1755.2005.00691.x. [DOI] [PubMed] [Google Scholar]
- 21.Harris KM. Washington, DC: National Academy Press; 1999. The health status and risk behaviors of adolescents in immigrant families. [Google Scholar]
- 22.Hsu CY, Iribarren C, McCulloch CE, et al. Risk factors for end-stage renal disease: 25-year follow-up. Arch Intern Med. 2009;169:342–350. doi: 10.1001/archinternmed.2008.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hsu CY, Lin F, Vittinghoff E, et al. Racial differences in the progression from chronic renal insufficiency to end-stage renal disease in the United States. J Am Soc Nephrol. 2003;14:2902–2907. doi: 10.1097/01.asn.0000091586.46532.b4. [DOI] [PubMed] [Google Scholar]
- 24.Kandula NR, Diez Roux AV, Chan C, et al. Association of acculturation levels and prevalence of diabetes mellitus in the Multi-ethnic Study of Atherosclerosis (MESA) Diabetes Care. 2008;31:1621–1628. doi: 10.2337/dc07-2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lauderdale DS, Rathouz PJ. Body mass index in a US national sample of Asian Americans: effects of nativity, years since immigration and socioeconomic status. Int J Obes Relat Metab Disord. 2000;24:1188–1194. doi: 10.1038/sj.ijo.0801365. [DOI] [PubMed] [Google Scholar]
- 26.Lutsey PL, Diez Roux AV, Jacobs DR, Jr, et al. Associations of acculturation and socioeconomic status with subclinical cardiovascular disease in the Multi-Ethnic Study of Atherosclerosis. Am J Public Health. 2008;98:1963–1970. doi: 10.2105/AJPH.2007.123844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lutsey PL, Jacobs DR, Jr, Kori S, et al. Whole grain intake and its cross-sectional association with obesity, insulin resistance, inflammation, diabetes and subclinical CVD: the MESA Study. Br J Nutr. 2007;98:397–405. doi: 10.1017/S0007114507700715. [DOI] [PubMed] [Google Scholar]
- 28.McClellan W, Warnock DG, McClure L, et al. Racial differences in the prevalence of chronic kidney disease among participants in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Cohort Study. J Am Soc Nephrol. 2006;17:1710–1715. doi: 10.1681/ASN.2005111200. [DOI] [PubMed] [Google Scholar]
- 29.Montez JK, Eschbach K. Country of birth and language are uniquely associated with intakes of fat, fiber, and fruits and vegetables among Mexican-American women in the United States. J Am Diet Assoc. 2008;108:473–480. doi: 10.1016/j.jada.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 30.Moran A, Diez Roux AV, Jackson SA, et al. Acculturation is associated with hypertension in a multiethnic sample. Am J Hypertens. 2007;20:354–363. doi: 10.1016/j.amjhyper.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 31.Palinkas LA, Pickwell SM. Acculturation as a risk factor for chronic disease among Cambodian refugees in the United States. Soc Sci Med. 1995;40:1643–1653. doi: 10.1016/0277-9536(94)00344-s. [DOI] [PubMed] [Google Scholar]
- 32.Parikh NS, Fahs MC, Shelley D, et al. Health behaviors of older Chinese adults living in New York City. J Community Health. 2009;34:6–15. doi: 10.1007/s10900-008-9125-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peralta CA, Li Y, Wassel C, et al. Differences in albuminuria between Hispanics and Whites: an evaluation by genetic ancestry and country of origin: The Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Genet. 2010;3:240–247. doi: 10.1161/CIRCGENETICS.109.914499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peralta CA, Shlipak MG, Fan D, et al. Risks for end-stage renal disease, cardiovascular events, and death in Hispanic versus non-Hispanic white adults with chronic kidney disease. J Am Soc Nephrol. 2006;17:2892–2899. doi: 10.1681/ASN.2005101122. [DOI] [PubMed] [Google Scholar]
- 35.Rule AD, Bergstralh EJ, Slezak JM, et al. Glomerular filtration rate estimated by cystatin C among different clinical presentations. Kidney Int. 2006;69:399–405. doi: 10.1038/sj.ki.5000073. [DOI] [PubMed] [Google Scholar]
- 36.Salant T, Lauderdale DS. Measuring culture: a critical review of acculturation and health in Asian immigrant populations. Soc Sci Med. 2003;57:71–90. doi: 10.1016/s0277-9536(02)00300-3. [DOI] [PubMed] [Google Scholar]
- 37.Sarnak M, Katz R, Fried L, et al. Cystatin C and aging success. Arch Intern Med. 2008;168:147–153. doi: 10.1001/archinternmed.2007.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shlipak M, Katz R, Cushman M, et al. Cystatin-C and inflammatory markers in the ambulatory elderly. Am J Med. 2005;118:1416. doi: 10.1016/j.amjmed.2005.07.060. [DOI] [PubMed] [Google Scholar]
- 39.Shlipak M, Katz R, Kestenbaum B, et al. Rate of kidney function decline in older adults—a comparison using creatinine and cystatin C. Am J Nephrol. 2009;30:171–178. doi: 10.1159/000212381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shlipak MG, Fried LF, Crump C, et al. Elevations of inflammatory and procoagulant biomarkers in elderly persons with renal insufficiency. Circulation. 2003;107:87–92. doi: 10.1161/01.cir.0000042700.48769.59. [DOI] [PubMed] [Google Scholar]
- 41.Shlipak MG, Katz R, Kestenbaum B, et al. Rapid decline of kidney function increases cardiovascular risk in the elderly. J Am Soc Nephrol. 2009;20:2625–2630. doi: 10.1681/ASN.2009050546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shlipak MG, Sarnak M, Katz R, et al. Cystatin-C and risk for mortality and cardiovascular disease in elderly adults. N Engl J Med. 2005;352:2049–2060. doi: 10.1056/NEJMoa043161. [DOI] [PubMed] [Google Scholar]
- 43.Stehman-Breen CO, Gillen D, Steffes M, et al. Racial differences in early-onset renal disease among young adults: the coronary artery risk development in young adults (CARDIA) study. J Am Soc Nephrol. 2003;14:2352–2357. doi: 10.1097/01.asn.0000083392.11042.14. [DOI] [PubMed] [Google Scholar]
- 44.Stevens LA, Coresh J, Schmid CH, et al. Estimating GFR using serum cystatin C alone and in combination with serum creatinine: a pooled analysis of 3,418 individuals with CKD. Am J Kidney Dis. 2008;51:395–406. doi: 10.1053/j.ajkd.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stewart AL, Napoles-Springer AM. Advancing health disparities research: can we afford to ignore measurement issues? Med Care. 2003;41:1207–1220. doi: 10.1097/01.MLR.0000093420.27745.48. [DOI] [PubMed] [Google Scholar]
- 46.Tang TN, Dion KL. Gender and acculturation in relation to traditionalism: perceptions of self and parents among Chinese students. Sex Roles. 1999;41:17–29. [Google Scholar]
- 47.Tarver-Carr ME, Powe NR, Eberhardt MS, et al. Excess risk of chronic kidney disease among African-American versus white subjects in the United States: a population-based study of potential explanatory factors. J Am Soc Nephrol. 2002;13:2363–2370. doi: 10.1097/01.asn.0000026493.18542.6a. [DOI] [PubMed] [Google Scholar]
- 48.Taylor HL, Jacobs DR, Jr, Schucker B, et al. A questionnaire for the assessment of leisure time physical activities. J Chronic Dis. 1978;31:741–755. doi: 10.1016/0021-9681(78)90058-9. [DOI] [PubMed] [Google Scholar]
- 49.USRDS . Renal Data System (USRDS) Annual Data Report. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2008. [Google Scholar]
- 50.Xue JL, Eggers PW, Agodoa LY, et al. Longitudinal study of racial and ethnic differences in developing end-stage renal disease among aged medicare beneficiaries. J Am Soc Nephrol. 2007;18:1299–306. doi: 10.1681/ASN.2006050524. [DOI] [PubMed] [Google Scholar]