Abstract
Complementary and alternative medicine (CAM) therapies have been provided at hospitals along with conventional medicine in industrialized nations. Previous studies conducted in Japan revealed high proportion of Japanese had experience of using CAM, but failed to discuss how it should be provided. The present study aims to clarify the demand for CAM practice at hospitals in Japan. A questionnaire consisting of 41 questions was mailed to 10 000 adults randomly selected from the electoral roll of Mie prefecture, Japan in January 2007. The questionnaire asked the subjects about demand for CAM practice at hospitals, types of CAM therapy to be provided and associated reasons. Sociodemographic characteristics, perceived health status, experience and purpose of CAM use, and information resource for CAM were also surveyed. Completed answers were collected from 2824 (28.6%) respondents. Two thousand and nineteen (71.5%) of the respondents demanded CAM practice at hospitals with the most likely reason of “patients can receive treatment under the guidance of a physicians". The three most popular CAM therapies were Kampo, acupressure/massage/Shiatsu and acupuncture/moxibustion. The demand was positively associated with gender, ages of 40–59 years, annual household incomes of 5–7 million yen, occupation of specialist and technical workers and sales workers and poor health status. Higher demand was observed among those who used both CAM and conventional medical therapies for curative purposes. In conclusion, Japanese show a high demand for CAM practice, hoping to use CAM for curative purposes with monitoring by physicians at hospitals.
1. Introduction
With the increasing practice of complementary and alternative medicine (CAM), a bulk of studies including nationwide surveys have revealed levels of use of CAM therapy and characteristics of its users in industrialized nations [1–9]. Studies on the cost effectiveness have also presented evidence that CAM therapy can potentially contribute to a reduction in medical expenditure [10, 11]. Although dependent on social factors, a number of hospitals in industrialized nations have begun to integrate CAM practice into the conventional medical service. For example, in the USA, >37% of hospitals had introduced one or more CAM therapies in 2008 [12]. In Japan, hospitals including those allied with national universities have begun to establish departments for providing CAM practice in recent years. The practice of CAM, however, is often accompanied by challenges such as lack of licensure or education system, lack of insurance coverage and insufficient scientific evidence. Only a limited number of physicians are ready to coordinate with CAM practitioners [13].
In the west, with growing interest in integrative medicine, many research have been conducted focusing on credentialing CAM provider [14], the present situation of integration of CAM into conventional medical settings [15–18], CAM education at medical schools [19–22] and communication between physicians and CAM practitioners at hospitals [23–25]. On the contrary in Japan, most of the previous studies dealt with the popularity of CAM therapies and the backgrounds of users [7, 8], but few have discussed how and where people want them to be provided. As a wide range of legislation reformation will be required, if people want to receive CAM at hospitals along with conventional medicine, it is important to obtain information on the demand. In the present study, a population survey is conducted to assess the demand for CAM practice, reasons for the demand, types of CAM therapy to be provided and expected purposes for CAM at hospitals in Japan.
2. Methods
A total of 10 000 people, aged 20 years or above, were randomly selected from the electoral roll of all 29 cities and towns in Mie Prefecture. Sampling was conducted according to the geographic proportion of the population and in accordance with the Public Office Election Law of Japan. A questionnaire was mailed to the recipients on January 9, 2007, asking them to answer questions anonymously and to return it by January 31. It did not include any question on the clinical data that would lead to the identification of respondents. In the cover letter attached to the questionnaire, recipients were informed that the personal data including name and address were used only for sending the questionnaire, that the data indicated in the response sheets would not be used for purpose other than research, and that none of the data would not be transmitted to other parties.
Fifteen types of therapy (Table 1) were given as complementary and alternative therapies and the subjects were asked “Do you want to receive CAM therapy at hospitals?" (i.e., demand for CAM practice at hospitals). Respondents who gave “Yes" to this question were requested to answer which CAM therapy they wanted to be provided at hospitals along with conventional medicine and their reasons. The questionnaire also inquired on their experience of CAM therapy over a lifetime as well as conventional medical therapy within the last 12 months at their hospitals. Those who experienced CAM therapy (CAM users) were requested to report the purposes and information resources for the therapy. If the respondents reported they had no experience of CAM therapy or had no desire to receive it (non-CAM users), they were asked to give the reasons. Sociodemographic characteristics (age, gender, area of residence, occupation and annual household income) and perceived health status were asked in the questionnaire.
Table 1.
Types of CAM therapy 2019 respondents wanted to be provided at hospitals (Number with percent in parenthesis).
| Type of CAM | Number (%) |
|---|---|
| Kampo | 1391 (69.0) |
| Acupressure, massage and Shiatsu | 1157 (57.4) |
| Acupuncture and moxibustion | 815 (40.4) |
| Seitai(a) or chiropractic | 778 (38.6) |
| Psychotherapy | 544 (27.0) |
| Balneotherapy | 530 (26.3) |
| Health foods (supplement) | 477 (23.6) |
| Reflexology | 370 (18.3) |
| Aromatherapy | 237 (11.8) |
| Yoga (Ayurveda) | 235 (11.7) |
| Qigong | 222 (11.0) |
| Music therapy | 206 (10.2) |
| Hypnotherapy | 159 (7.9) |
| Meditation | 98 (4.9) |
| Thalassotherapy | 90 (4.5) |
| Others | 10 (0.5) |
(a)Seitai is a kind of manipulative technique originated in Japan, which is practiced mainly for joint adjustment.
The chi-square (χ 2) test was conducted to determine whether there was an association of the demand for CAM practice at hospitals with demographic characteristics, perceived health status and purpose for CAM use. Adjusted standardized residuals in each cell of contingency tables were examined to assess the significance of association [26]. Analysis was performed using PASW Statistics version 18.0 for Windows.
3. Results
3.1. Response Rate
A total of 2824 questionnaires were collected before January 31, with 112 undelivered. Thus, the response rate was 28.6% (2824/9888). CAM was received by 64% (1807) of the respondents over a lifetime, whereas conventional medical therapies were received by 77% (2178) within the last 12 months.
3.2. Demand for CAM at Hospitals, Its Reason and the Types of CAM Demanded
The demand for CAM practice at hospitals was reported by 71.5% (2019) of the respondents. The types of CAM therapy that the respondents wanted to be administered are listed in Table 1. The four most in-demand CAM therapies were “Kampo", “acupressure/massage/Shiatsu", “acupuncture/moxibustion" and “seitai/chiropractic". More than half of the respondents gave the reason for their choice as “patients can receive treatment under the guidance of a physician" (Table 2).
Table 2.
Reasons for the demand for CAM practice at hospitals in 2019 respondents (Number with percent in parenthesis).
| Reason | Number (%) |
|---|---|
| Patients can receive treatment under guidance of a physician | 1100 (54.5) |
| Health insurance may be used | 984 (48.8) |
| Patients can receive both CM and CAM in a single hospital | 950 (47.1) |
| Higher effect can be expected by combining CM and CAM | 858 (42.5) |
| Multiple approaches to illness can be expected | 854 (42.3) |
| Better sanitary condition can be expected | 142 (7.0) |
| Other | 30 (1.5) |
CM, conventional medicine.
3.3. Sociodemographic Indicators
Table 3 shows relationships of the demand for CAM practice at hospitals to sociodemographic characteristics and perceived health status. The demand was higher in females than in males. It varied among age groups, that is, it was higher in the 40- to 59-year-old age group, whereas it was lower in the younger (<30 years) and the older (>60 years) age groups. Those whose household income was 5–7 million yen showed a significantly higher demand, whereas those with <3 million yen had a lower demand. Higher demand was observed in “specialist and technical worker" and “sales worker" groups, whereas demand was low in “unemployed", “production process and related workers" and “agriculture, forestry and fishery workers" groups. In all the categorized groups with perceived health status, high demand for CAM practice at hospitals was observed. However, respondents who had both mental and physical problems reported significantly higher demand, whereas those who felt neither of them did have a significantly lower demand.
Table 3.
Relations between sociodemographic characterisitics, perceived health status and demand for CAM practice at hospitals among all 2824 respondents.
| Do you want to receive CAM at hospitals? | Adjusted standardized residuals | P-value (χ 2 test) | ||
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Gender(a) | ||||
| Male | 850 (74.1) | 297 (25.9) | −2.9 | <.05 |
| Female | 1118 (78.9) | 299 (21.1) | 2.9 | |
| Age (years)(b) | ||||
| 20–29 | 185 (72.0) | 72 (28.0) | −2 | <.001 |
| 30–39 | 352 (80.2) | 87 (19.8) | 1.7 | |
| 40–49 | 463 (82.2) | 100 (17.8) | 3.3 | |
| 50–59 | 545 (80.6) | 131 (19.4) | 2.6 | |
| 60–69 | 343 (69.0) | 154 (31.0) | −4.7 | |
| >70 | 115 (67.6) | 55 (32.4) | −3 | |
| Annual household income (yen)(c) | ||||
| <3 million | 398 (70.3) | 168 (29.7) | −4.2 | <.001 |
| 3–5 million | 525 (77.1) | 156 (22.9) | 0.2 | |
| 5–7 million | 410 (81.8) | 91 (18.2) | 2.9 | |
| 7–10 million | 343 (76.9) | 103 (23.1) | 0 | |
| >10 million | 226 (80.7) | 54 (19.3) | 1.6 | |
| Occupation(d) | ||||
| Specialist and technical workers | 338 (81.3) | 78 (18.8) | 2.2 | <.001 |
| Administrative and managerial workers | 139 (79.4) | 36 (20.6) | 0.8 | |
| Clerical workers | 220 (81.2) | 51 (18.8) | 1.7 | |
| Production process and related workers | 164 (71.6) | 65 (28.4) | −2 | |
| Service workers | 165 (77.1) | 49 (22.9) | 0 | |
| Security workers | 14 (82.4) | 3 (17.6) | 0.5 | |
| Transport and communication workers | 36 (78.3) | 10 (21.7) | 0.2 | |
| Agriculture, forestry and fishery workers | 45 (59.2) | 31 (40.8) | −3.7 | |
| Sales workers | 100 (87.0) | 15 (13.0) | 2.6 | |
| Student | 33 (73.3) | 12 (26.7) | −0.6 | |
| Housewife/househusband | 426 (79.5) | 110 (20.5) | 1.5 | |
| Not employed | 231 (67.2) | 113 (32.8) | −4.7 | |
| Other | 90 (78.9) | 24 (21.1) | 0.5 | |
| Perceived health status | ||||
| Both mentally and physically fit | 747 (74.0) | 262 (26.0) | −2.9 | <.05 |
| Physically fit but mentally some problems | 180 (76.9) | 54 (23.1) | 0 | |
| Mentally fit but physically have some problems | 643 (77.3) | 189 (22.7) | 0.2 | |
| Both mentally and physically have problems | 438 (82.2) | 95 (17.8) | 3.2 | |
P-values indicate differences in proportion between gender, age groups, annual income groups, occupational groups and “perceived health status" groups, respectively.
(a)260 (9.2%); (b)222 (7.9%); (c)350 (12.4%); and (d)226 (8.0%) of the respondents did not answer the questions, respectively.
3.4. Purpose of CAM Use at Hospitals
The relationships between the purposes of CAM use and the demand for CAM practice at hospitals in 1807 CAM users are shown in Table 4. Those who received both CAM and conventional medical therapies for curative purposes had a higher demand for CAM practice at hospitals than those who used CAM for preventive or refreshment purposes.
Table 4.
Relations between the purpose for CAM use and demand for CAM practice at hospitals in 1807 CAM users.
| Purpose of CAM use | Do you want to receive CAM at hospitals? | Adjusted standardized residuals | P-value (χ 2 test) | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Curative purpose (also use conventional medicine) | 545 (90.5) | 57 (9.5) | 4.8 | <.001 |
| Curative purpose (only use CAM therapy) | 280 (85.6) | 47 (14.4) | 0.5 | |
| Preventive purpose | 217 (81.6) | 49 (18.4) | −1.6 | |
| Refreshment | 448 (79.7) | 114 (20.3) | −4.1 | |
P-values indicate differences in the proportions between the four groups. Of 1807 CAM users, 50 respondents did not answer the question.
3.5. Reasons for Disuse of CAM and Information Resource of CAM
The two most common reasons for disuse of 678 non-CAM users were “unclearness of the effect of CAM" and “lack of CAM therapy knowledge" (Table 5). As for information resource for CAM, 77% (1404) of CAM users depended on their family or an acquaintance for their information for CAM. Other resources are as follows: “books/magazines" (550, 29%), “TV/radio programs" (468, 25%) and “recommendation by a physician" (335, 18%).
Table 5.
Reasons for disuse of CAM therapy in 678 non-CAM users (Number with percent in parenthesis).
| Reason | Number (%) |
|---|---|
| Unclearness of effect of CAM | 370 (54.5) |
| Lack of knowledge about CAM | 289 (42.6) |
| High cost of CAM | 241 (35.5) |
| Conventional medicine alone is satisfactory | 178 (26.2) |
| Have no time to visit CAM practitioner | 136 (20.0) |
| Poor safety and sanitary condition of CAM | 70 (10.3) |
| Adverse effect of CAM | 47 (6.9) |
| Afraid of bad chemistry with CAM practitioner | 45 (6.6) |
| Have dislike of body contact | 41 (6.0) |
| Other | 55 (8.1) |
4. Discussion
It was found that over 70% of the respondents reported that they want to receive CAM therapy at hospitals. The three most in-demand CAM therapies at hospitals with conventional medicine were Kampo, acupressure/massage/Shiatsu and acupuncture/moxibustion, followed by seitai/chiropractics. Among them, Kampo is already being practiced by physicians as a part of conventional medicine in Japan. Hence, according to the classification by National Centre for Complementary and Alternative Medicine (NCCAM), it is possible that the Japanese want manipulative and body-based methods mostly to be administrated at hospitals. As shown in Table 6, under the current Japanese healthcare system, acupressure/massage/Shiatsu and acupuncture/moxibustion, both of which have a long history of practice in Japan as a part of traditional medicine, are practiced with a national license, but chiropractics and seitai lack such regulation or an education system. If those therapies need to be provided along with conventional medicine in Japan, legislative reformation is required.
Table 6.
CAM therapies under the current Japanese healthcare system.
| Type | National qualification | Health insurance coverage | Education |
|---|---|---|---|
| Kampo | No | Yes(a) | A minimum of 8-h training at medical school |
| Acupuncture and moxibustion | Yes | Limited(b) | Three years education at college or |
| Four years education at university | |||
| Acupressure, massage and Shiatsu | Yes | No | Three years education at college |
| Seitai | No | No | None |
| Chiropractic | No | No | None |
| Aromatherapy | No(c) | No | None |
| Reflexology | No | No | None |
| Yoga (Ayurveda) | No(d) | No | None |
| Qigong | No | No | None |
| Health foods | No | No | None |
| Hypnotherapy | No(d) | No | None |
| Music therapy | No(d) | No | None |
| Meditation | No | No | None |
| Psychotherapy | No(e) | No | None |
| Balneotherapy | No | No | None |
| Thalassotherapy | No | No | None |
Kampo and balneotherapy have no national licensure system, but medical doctors who have completed 5 years of special training and have passed an examination conducted by the academic society of the respective fields are certificated as medical experts in the field.
(a)One hundred and forty-eight Kampo formulae are included under physician's prescription.
(b)Limited to six diseases. Consent by physicians is required.
(c)Academic society provides society certification for medical doctors or other licensed co-medical practitioners who meet the requirement and passed written examination. There are also qualifications offered by non-academic associations for non-licensed and licensed health professionals.
(d)Applicants who meet the requirements of academic society in the field and pass the examinations are provided qualification by the society.
(e)Applicants who meet the requirements of foundation in the field and pass the examinations are provided qualification by the foundation.
Previous studies revealed that 55–62% of the patients who received CAM therapy did not report it to their physicians, suggesting that physicians should pay more attention to their patients' CAM use [4, 5, 7, 8]. In the present study, more than half of the respondents indicated the presence of a physician's guidance as the reason for demanding CAM practice at hospitals (Table 2), indicating that they placed reliance on physicians in using CAM. Thus, CAM may play a complementary role in medical care, under recognition by physicians.
Nearly half of non-CAM users answered “lack of knowledge on CAM" as the reason for not using CAM in the present study. Given the fact that over three-quarters of the CAM users obtain the information from their family or an acquaintance, CAM users also might lack sufficient information about the indications or effects of each CAM therapy. This suggests an anxiety about lack of knowledge on CAM may be associated with the expectation for an environment in which they can receive advice from physicians. Among the CAM users, those who received both CAM and conventional medical therapies for curative purposes are most likely to demand CAM practice at hospitals, whereas those who received only CAM for refreshment showed lower demand, suggesting that more people hope to see that CAM therapies are provided as a curative measure rather than as preventive one or refreshment.
The combined practice of CAM therapy and conventional medicine is defined as integrative medicine by NCCAM as “integrative medicine combines conventional and CAM treatments for which there is evidence of safety and effectiveness [27]". Besides scientific evidence, the practice of integrative medicine would require a wide range of legislation reforms such as a licensure system for CAM, education curricula in medical schools and insurance systems in accordance with the medical systems of each nation. The present survey demonstrated that many Japanese wanted CAM therapies such as Kampo and manipulative and body-based methods to be integrated into medical service at hospitals. However, the current healthcare system in Japan offers only a minimum of 8-h training for Kampo or acupuncture in a 6-year education program in medical schools, which is far from sufficient; less education is provided to physicians for other types of CAM. With little knowledge on indication or possible adverse effects, physicians are not ready to use CAM or to coordinate with CAM practitioners. Another fundamental barrier to integrating CAM into conventional medical service is the current public health insurance system, which prohibits a patient to have reimbursed both for conventional medical treatment and CAM therapy, if the patient receives those therapies at a hospital under the same diagnosis. Thus, reforms in public health insurance system, as well as educational program are important when CAM therapies are integrated.
Higher demand for CAM practice at hospitals was observed in females, the groups of those aged 40–59 years, in annual household incomes of 5–7 million yen, and in specialist and technical workers and sales workers. Those who reported both mental and physical problems showed higher demand. These results, together with the observation of lower demand among those aged >60 years, those with their annual income over 7 million yen and those engaged in administrative and management works, suggest that people from middle classes and those engaged in intellectual occupation but not in administrative position, were the most likely users of CAM provided at hospitals.
The present study demonstrated high demand for CAM practice at hospitals in Japan. However, this does not mean that all CAM therapies are to be included in the medical service at hospitals, however. For better integration of CAM with conventional medicine at hospitals, further surveys should be conducted to make clear which CAM therapies are to be administered and which are to be provided independent of conventional medical service at hospitals. The background on the demand for CAM practice at hospitals and the implications for future study are summarized in Figure 1.
Figure 1.
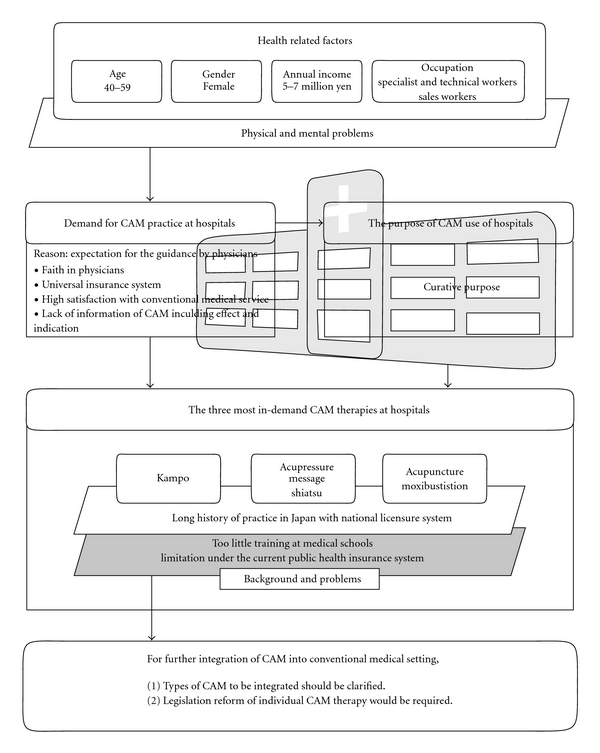
Background on the demand for CAM therapy at hospitals in Japan and implications for future study.
Finally, the present survey has the following limitations. First, the study was conducted by carrying out a postal survey and the response rate was relatively low compared with other surveys conducted in western nations. There was no information on the non-respondents. Also, recipients who were hospitalized might not have answered the questionnaire. Second, the respondents were not asked about the seriousness of their illness. Third, geographical characteristics of the sampling population should be considered. Mie prefecture is a relatively rural state located south of Kyoto and Nagoya, with a population of 1 867 696 (the population of adults aged 20 years or above is 1 503 662) [28], and the low prevalence of CAM therapies such as reflexology and yoga, which are relatively new to the Japanese population, may have influenced the respondents' CAM knowledge.
Despite those limitations, however, sampling population of our survey is not considered to be more likely to include people in favor of CAM. In our survey, 23.7% (669/2824) of the respondents reported lifetime experience of acupuncture treatment, which is quite similar with the data shown in Ishizaki et al.'s nationwide surveys conducted annually from 2003 through 2006 (26.7, 19.4, 24.4 and 25.4, resp.) [9]. Our study showed the lifetime utilization of Kampo is 37.5% (1058/2824), which is also close to the figure shown in the Okabe's survey (∼40%) conducted at four major general hospitals in Tokyo [29].
5. Conclusion
In Mie prefecture, Japan, there is a high demand for CAM practice, especially Kampo and manipulative methods, along with conventional medicine as a curative measure with monitoring of physicians at hospitals. These findings should be confirmed through nationwide survey and can be utilized for better integration of CAM into conventional medical setting in Japan.
Funding
This work was financially supported by the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Acknowledgments
The authors thank Kazuo Miyagawa of the Mie Prefectural Office and Hiroyuki Nakahata of the Hyakugo Economic Research Institute for reviewing the questionnaire and providing valuable advice. The Ministry of Education, Culture, Sports, Science and Technology of Japan.
References
- 1.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. Journal of the American Medical Association. 1998;280(18):1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 2.Ernst E, White A. The BBC survey of complementary medicine use in the UK. Complementary Therapies in Medicine. 2000;8(1):32–36. [PubMed] [Google Scholar]
- 3.Thomas KJ, Nicholl JP, Coleman P. Use and expenditure on complementary medicine in England: a population based survey. Complementary Therapies in Medicine. 2001;9(1):2–11. doi: 10.1054/ctim.2000.0407. [DOI] [PubMed] [Google Scholar]
- 4.Thomas K, Coleman P. Use of complementary or alternative medicine in a general population in Great Britain. Results from the National Omnibus survey. Journal of Public Health. 2004;26(2):152–157. doi: 10.1093/pubmed/fdh139. [DOI] [PubMed] [Google Scholar]
- 5.Xue CCL, Zhang AL, Lin V, Da Costa C, Story DF. Complementary and alternative medicine use in Australia: a national population-based survey. Journal of Alternative and Complementary Medicine. 2007;13(6):643–650. doi: 10.1089/acm.2006.6355. [DOI] [PubMed] [Google Scholar]
- 6.Ock SM, Choi JY, Cha YS, et al. The use of complementary and alternative medicine in a general population in South Korea: results from a national survey in 2006. Journal of Korean Medical Science. 2009;24(1):1–6. doi: 10.3346/jkms.2009.24.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamashita H, Tsukayama H, Sugishita C. Popularity of complementary and alternative medicine in Japan: a telephone survey. Complementary Therapies in Medicine. 2002;10(2):84–93. doi: 10.1054/ctim.2002.0519. [DOI] [PubMed] [Google Scholar]
- 8.Hori S, Mihaylov I, Vasconcelos JC, McCoubrie M. Patterns of complementary and alternative medicine use amongst outpatients in Tokyo, Japan. BMC Complementary and Alternative Medicine. 2008;8, article no. 14 doi: 10.1186/1472-6882-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ishizaki N, Yano T, Kawakita K. Public status and prevalence of acupuncture in Japan. Evidence-Based Complementary and Alternative Medicine. 2008;7(4):493–500. doi: 10.1093/ecam/nen037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sawazaki K, Sakuraba H, Masudai F, Ishii C, Yokoyama K. Use of complementary and alternative medicines among factory workers: investigation of workers in manufacturing. Sangyo Eiseigaku Zasshi. 2005;47:254–258. doi: 10.1539/sangyoeisei.47.254. [DOI] [PubMed] [Google Scholar]
- 11.Sawazaki K, Mukaino Y, Kinoshita F, et al. Acupuncture can reduce perceived pain, mood disturbances and medical expenses related to low back pain among factory employees. Industrial Health. 2008;46(4):336–340. doi: 10.2486/indhealth.46.336. [DOI] [PubMed] [Google Scholar]
- 12.Hospital Connect Search. 2009, http://www.hospitalconnect.com.
- 13.Jain N, Astin JA. Barriers to acceptance: an exploratory study of complementary/alternative medicine disuse. Journal of Alternative and Complementary Medicine. 2001;7(6):689–696. doi: 10.1089/10755530152755243. [DOI] [PubMed] [Google Scholar]
- 14.Eisenberg DM, Cohen MH, Hrbek A, Grayzel J, Van Rompay MI, Cooper RA. Credentialing complementary and alternative medical providers. Annals of Internal Medicine. 2002;137(12):965–973. doi: 10.7326/0003-4819-137-12-200212170-00010. [DOI] [PubMed] [Google Scholar]
- 15.Scherwitz L, Stewart W, McHenry P, Wood C, Robertson L, Cantwell M. An integrative medicine clinic in a community hospital. American Journal of Public Health. 2003;93(4):549–552. doi: 10.2105/ajph.93.4.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vohra S, Feldman K, Johnston B, Waters K, Boon H. Integrating complementary and alternative medicine into academic medical centers: experience and perceptions of nine leading centers in North America. BMC Health Services Research. 2005;5, article no. 78 doi: 10.1186/1472-6963-5-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen MH, Sandler L, Hrbek A, Davis RB, Eisenberg DM. Policies pertaining to complementary and alternative medical therapies in a random sample of 39 academic health centers. Alternative Therapies in Health and Medicine. 2005;11(1):36–40. [PubMed] [Google Scholar]
- 18.Song MY, John M, Dobs AS. Clinicians' attitudes and usage of complementary and alternative integrative medicine: a survey at the Johns Hopkins Medical Institute. Journal of Alternative and Complementary Medicine. 2007;13:305–306. doi: 10.1089/acm.2006.5340. [DOI] [PubMed] [Google Scholar]
- 19.Wetzel MS, Kaptchuk TJ, Haramati A, Eisenberg DM. Complementary and alternative medical therapies: implications for medical education. Annals of Internal Medicine. 2003;138(3):191–196. doi: 10.7326/0003-4819-138-3-200302040-00011. [DOI] [PubMed] [Google Scholar]
- 20.Hewson MG, Copeland HL, Mascha E, Arrigain S, Topol E, Fox JEB. Integrative medicine: implementation and evaluation of a professional development program using experiential learning and conceptual change teaching approaches. Patient Education and Counseling. 2006;62(1):5–12. doi: 10.1016/j.pec.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 21.Witt CM, Brinkhaus B, Willich S. Teaching complementary and alternative medicine in a reform curriculum. Forschende Komplementarmedizin. 2006;13(6):342–348. doi: 10.1159/000097437. [DOI] [PubMed] [Google Scholar]
- 22.Elder WG, Hustedde C, Rakel D, Joyce J. CAM curriculum activities to enhance professionalism training in medical schools. Complementary Health Practice Review. 2008;13:127–133. doi: 10.1177/1533210107313917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frenkel M, Ben-Arye E, Geva H, Klein A. Educating CAM practitioners about integrative medicine: an approach to overcoming the communication gap with conventional health care practitioners. Journal of Alternative and Complementary Medicine. 2007;13(3):387–391. doi: 10.1089/acm.2006.6293. [DOI] [PubMed] [Google Scholar]
- 24.Klimenko E, Julliard K. Communication between CAM and mainstream medicine: delphi panel perspectives. Complementary Therapies in Clinical Practice. 2007;13:46–52. doi: 10.1016/j.ctcp.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 25.Soklaridis S, Kelner M, Love RL, Cassidy JD. Integrative health care in a hospital setting: communication patterns between CAM and biomedical practitioners. Journal of Interprofessional Care. 2009;23:655–667. doi: 10.3109/13561820902886287. [DOI] [PubMed] [Google Scholar]
- 26.Haberman SJ. The analysis of residuals in cross-classified tables. Biometrics. 1973;29:205–220. [Google Scholar]
- 27.NCCAM. 2009, http://nccam.nih.gov/news/camstats/2007/camsurvey_fs1.htm.
- 28.Mie Prefecture. 2009, http://www.pref.mie.jp/DATABOX/library/jinkou/index.htm.
- 29.Okabe T. Survey in general hospital: special session 2. The role of Kampo medicine for Japanese population- Kampo prevalence survey. (Abstract of the 60th annual meeting of the Japan Society of Oriental Medicine) Kampo Medicine. 2009;60(supplement):120–121. [Google Scholar]


